Abstract
Background
Pancreatic cancer is increasingly common and poised to become the second leading cause of cancer deaths by the year 2020. Surgical resection is only chance for cure yet significant disparities in resection rates exist by insurance status. The 2006 Massachusetts health care reform serves as natural experiment to evaluate the unknown impact of health insurance expansion on treatment of pancreatic cancer.
Study Design
Using the Agency for Healthcare Research and Quality State Inpatient Databases, this cohort study examines non-elderly, adult patients with no insurance, private coverage, or government-subsidized insurance plans who were admitted with pancreatic cancer in Massachusetts and three control states. Primary outcome was change in pancreatic resection rates. Difference-in-difference models were used to show impact of Massachusetts health care reform on resection rates for pancreatic cancer, controlling for confounding factors and secular trends.
Results
Prior to the Massachusetts reform, government-subsidized and self-pay patients (GSSP) had significantly lower rates of resection than privately-insured patients. The 2006 Massachusetts health reform was associated with a 15% increased rate of admission with pancreatic cancer (P=0.043) and a 67% increased rate of surgical resection (P=0.043) compared to control states. Measured disparities in likelihood of resection by insurance status decreased in Massachusetts while remaining unchanged in control states.
Conclusions
The 2006 Massachusetts health care reform was associated with increased resection rates for pancreatic cancer compared to control states. Our findings provide hopeful evidence that increased insurance coverage may help improve equity in pancreatic cancer treatment. Additional studies are needed to evaluate the longevity of these findings and generalizability in other states.
Introduction
The incidence of pancreatic cancer is increasing, making it currently the fourth leading cause of cancer mortality in the United States with projections of it becoming the second leading cause by the year 2020.1,2 The overall five-year survival continues to be less than 5% and surgical resection remains the only chance for long-term survival.3 Unfortunately, the majority of patients present with metastatic or locally advanced disease. For patients with locally advanced cancers, multimodality therapy has allowed for an improvement in survival for even the most challenging cases.4,5 While only 15% of patients present with resectable pancreatic cancer, 40–60% of these patients fail to undergo potentially curative resection.6,7 Studies evaluating geographic and historic variability have shown areas with higher resection rates to be associated with improved overall survival.7,8
Significant disparities in the treatment of pancreatic cancer have been documented across the country. Lack of private insurance coverage has been linked to lower likelihood of presenting with resectable pancreatic cancer and decreased likelihood of undergoing surgery.9 Socioeconomic status, including insurance coverage, is also associated with decreased receipt of care of pancreatic cancer in compliance with standard treatment guidelines.10 Further analyses suggest that gaps in treatment and overall survival for cancer diagnoses may be enhanced if access to health care is improved.11
The 2006 Massachusetts health care reform provides a unique natural experiment to evaluate the impact of health insurance expansion on disparities in pancreatic cancer. Nearly all provisions within the law were aimed at increasing access to insurance coverage through mechanisms that included the expansion of Medicaid, creation of a new subsidized insurance program for those ineligible for Medicaid, and expanding young adult eligibility on parental plans until age 26.12 The law also provided the basic framework for the Patient Protection and Affordable Care Act, which has the potential of adding insurance coverage to more than 16-million Americans.13 Since implementation of the 2006 Reform, Massachusetts has seen increased insurance coverage to about 96% of its residents. However, questions remain as to whether increased insurance coverage will translate into increased access to or quality of care for patients with pancreatic cancer.
Prior studies have identified multiple drivers of disparities in diagnosis, treatment, and outcomes of pancreatic cancer. Uninsured patients are significantly less likely to be referred for surgical resection and are less likely to be evaluated at high-volume centers.14 As centralization of pancreatic cancer treatment has increased over past decades, questions have been raised as to how patients with already limited access to care may be impacted. To that end, the question remains whether increased coverage across a population will translate into increased receipt of surgery for patients with pancreatic cancer. We hypothesized that increased insurance coverage in Massachusetts would be associated with increased resection rates for pancreatic cancer. The primary aim of this study is to examine changes in surgical resection rates for patients with pancreatic cancer before and after the Massachusetts health reform in 2006. Our secondary aim was to evaluate changes in site-of-care during admission for pancreatic cancer.
Methods
Study Design & Data
This cohort study used the Hospital Cost and Utilization Project State Inpatient Databases (SID) for Massachusetts, New Jersey, New York, and Florida between January 1, 2001 and December, 31 2011. The SID are administrative databases capturing approximately 98% of all discharges from all hospitals across respective states each year. Data are collected and maintained by public-private partnerships, supported by the Agency of Healthcare Research and Quality (AHRQ). Control states were selected based on completeness of data and similar availability of surgical services.15
We included all inpatient admissions of non-disabled, non-elderly, adult patients with pancreatic cancer and no insurance coverage, private or Medicaid insurance coverage, or the newly created Commonwealth Care insurance (only in Massachusetts after reform). Admission with pancreatic cancer was determined via ICD-9 diagnosis codes (ICD-9-CM 15.7, 15.7x). Patients without insurance coverage, Medicaid, or Commonwealth Care coverage were grouped together and are subsequently referred to in this manuscript as government-subsidized/self-pay (GSSP). This cohort represents the primary population impacted by the 2006 health reform in Massachusetts that predominantly led to increased enrollment in either Medicaid or Commonwealth Care coverage.16 Patients with Medicare coverage were excluded from this analysis as no significant changes to Medicare eligibility or enrollment occurred as a part of the Massachusetts law. Patients aged less than 18 years or greater than 65 years were also excluded as coverage for these individuals were not directly affected by the insurance expansion.
Outcome Measures
The primary outcome was surgical resection for pancreatic cancer. Surgical resection was defined using ICD-9 procedure codes (ICD-9-CM 52.5x, 52.6, 52.7). We also identified patients who underwent palliative procedures including gastroenterostomy (ICD-9-CM 44.32, 44.38, 44.39, 46.39), biliary bypass (ICD-9-CM 51.36, 51.37, 51.39), endoscopic stents (ICD-9-CM 51.87, 52.93), or percutaneous procedures on biliary track (ICD-9-CM 51.980). Patients undergoing any surgery included those who underwent pancreatectomy (see above), palliative procedures (see above), or exploratory laparotomy/laparoscopy (ICD-9-CM 54.11, 54.21, 54.23, 54.29).
To evaluate trends in site-of-care, a separate variable was created to identify high-volume pancreatic surgery centers. Considerable debate remains regarding what absolute number of annual pancreatectomies per hospital constitutes a high volume and subsequently associated higher quality hospital. As the present study was not intended to evaluate volume/outcomes relationships, we used methodology consistent with prior studies to classify individual hospitals as high-volume.12,17–20 Hospital volume was identified by calculating the number of annual pancreatic resections per SID-assigned unique hospital identification number. Hospitals with volumes in the top quartile were deemed high-volume. This volume ultimately amounted to 12 cases per hospital per year and is similar to previous thresholds classifying high-volume pancreatectomy centers.12,17,18 Additional sensitivity analyses with alternative thresholds for high-volume hospitals used in previous studies (18 and 25 pancreatic resections per year) did not significantly alter results.19,20
Risk Adjustments
Multivariable models examining changes in rates of pancreatectomy controlled for age, sex, patient race, comorbidities using the Elixhauser Comorbidity Index21, and secular trends. Models examining disparities in probability of undergoing pancreatectomy before and after reform included additional adjustment for metastatic disease, receipt of chemotherapy, receipt of radiation therapy, and admission to a high pancreatectomy-volume hospital. Admission with metastatic disease was defined using concurrent ICD-9 diagnosis codes (ICD-9-CM 19.6x, 19.7x, 19.8x, 19.90). Similarly, concurrent procedural codes were used to determined receipt of chemotherapy (ICD-9-CM 99.25) or radiation therapy (ICD-9-CM 92.29). Secular trends were defined on a quarterly basis using a continuous time variable starting at the first quarter of 2001 and ending with the fourth quarter of 2010.
The primary independent variables included intervention group (Massachusetts vs. Control States), insurance coverage (GSSP vs. Private coverage), and pre- or post-reform time of discharge. The pre-reform period was defined as any admission before the third quarter of 2006, the time the legislation was passed, and post-reform was defined as any discharge after the fourth quarter of 2007. The time period between 2006 quarter three and 2008 quarter one were excluded as this was the period of implementation spanning initial signing of legislation and full implementation of the individual mandate requiring all residents to carry insurance. Previous studies have also shown the most significant uptake in insurance coverage occurred after this mandate went into effect in January 2008.22 Sensitivity analyses including all discharges between 2006 and 2008 did not change our results.
Statistical Analyses
We used difference-in-differences models to evaluate the differential change in outcomes in MA after reform relative to concurrent trends in control states.23–25 These models identify differential changes in outcomes in groups exposed to a policy change as compared to the control group not exposed to the policy change. To evaluate for a differential change in outcomes for all patients in MA after reform relative to control states, we used an interaction term between MA and the post-reform indicator variable. The subsequent coefficient (the difference-in-differences estimator) represents the independent change in the outcome associated with the 2006 intervention for all patients. Given the rarity of pancreatic cancer and low incidence of subsequent pancreatectomy, Poisson models were used to estimate the incident rate ratio of pancreatectomy, palliative procedures, or any surgical procedure for pancreatic cancer. The total population of non-elderly adults with private or GSSP insurance coverage in Massachusetts and control states was determined using available resources from the United States Census Bureau and The Commonwealth of Massachusetts.13,26
To look specifically at changes in outcomes by insurance coverage, we created a three-term interaction variable between MA, post-reform, and GSSP. This “triple-difference” estimator represents the independent impact of the 2006 Massachusetts reform on patients with GSSP coverage in Massachusetts, adjusting for changes in control states as well as secular trends within Massachusetts. In Poisson models, these coefficients represent the increased rate ratio of pancreatectomy attributable to the insurance expansion. Changes in probability of admission to a high-volume hospital after reform were evaluated using linear regression models, controlling for patient level demographic and comorbidity status, presence of metastasis, receipt of chemotherapy, radiation, or surgery as well secular trends. The “difference-in-difference” estimator used in these linear models represents the percentage-point change in probability of admission to high-volume hospital.
Disparities in probability of undergoing pancreatectomy if admitted with pancreatic cancer were established using logistic regression models. For these models we also controlled for patient level demographic and clinical factors, receipt of care at high verse low volume hospital, clustering at the individual hospital level, and secular trends. Disparities in probability of admission to high volume hospital controlled for patient level demographic and clinical factors, receipt of chemotherapy, radiation, or surgery, secular trends, and clustering at the hospital level.
This study was deemed exempt from IRB review. Data were analyzed using Stata version 13 (College Station, Texas). Results were considered significant if P ≤ 0.05.
Results
Our entire cohort included 6,086 admissions of patients with pancreatic cancer in Massachusetts and 41,074 admissions in control states (Table 1). Patients in Massachusetts were more likely to be of white race, have private insurance coverage, or be admitted to a not-for-profit urban hospital of greater than 300 beds. Patient ages, sex, comorbidities, probability of admission with metastatic disease, and percentage care at high-volume pancreatic surgery centers were similar between Massachusetts and control states.
Table 1.
Overall Demographic Characteristics
| Massachusetts n=6,086 | Control States n=41,074 | p Value | |
|---|---|---|---|
| Age, y, mean (std) | 55.0 (7.3) | 54.9 (7.4) | 0.114 |
| Female, n (%) | 2,811 (46.2) | 18,470 (45.0) | 0.027 |
| Race, n (%) | < 0.001 | ||
| White | 5,068 (85.4) | 27,088 (67.3) | |
| Black | 373 (6.3) | 6,066 (15.1) | |
| Hispanic | 280 (4.7) | 4,400 (10.9) | |
| Other | 213 (3.6) | 2,685 (6.7) | |
| Elixhauser Index, mean (std) | 2.2 (1.5) | 2.3 (1.5) | < 0.001 |
| Private insurance, n (%) | 4,979 (83.7) | 30,292 (73.8) | < 0.001 |
| Hospital type, n (%) | < 0.001 | ||
| Private | 227 (3.7) | 3,051 (7.4) | |
| NFP, rural | 111 (1.8) | 762 (1.9) | |
| NFP, urban, <300 beds | 1,648 (27.1) | 8,357 (20.4) | |
| NFP, urban, 300+ beds | 4,100 (67.4) | 28,885 (70.4) | |
| High volume hospital | 4,274 (70.2) | 28,659 (69.7) | 0.689 |
| Metastatic disease n (%) | 3,709 (60.9) | 23,478 (57.2) | < 0.001 |
| Pancreatectomy n (%) | 785 (12.9) | 3,798 (9.3) | < 0.001 |
Examining admission for all patients in Massachusetts relative to control states, there was no differential change in admissions with pancreatic cancer relative to control states (IRR 1.01, 95% CI [0.96 to 1.07], P=0.689). However, the Massachusetts health reform was independently associated with a 15% increased rate of admission with pancreatic cancer (IRR 1.15, 95% CI [1.00 to 1.31], P=0.043) for GSSP patients in Massachusetts relative to control states, adjusting for confounding patient-level factors and secular trends.
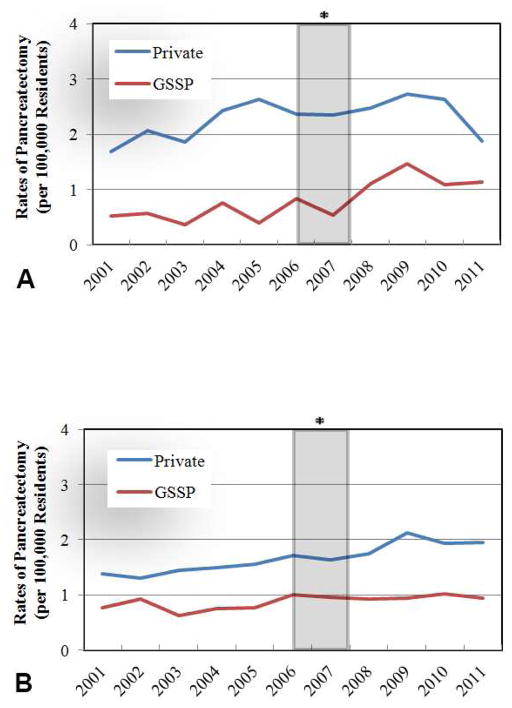
Patients with GSSP coverage had lower rates of resection than privately insured patients in both Massachusetts and control states throughout the study period (Figure 1a-b). Examining collective trends for all patients Massachusetts and control states regardless of insurance coverage, there was no differential change in resection rates (IRR 0.96, 95% CI [0.82 to 1.12], P=0.587), palliative procedures (IRR 1.02, 95% CI [0.93 to 1.12], P=0.683), or any surgical procedure (IRR 1.04, 95% CI [0.94 to 1.16], P=0.457) for all patients in Massachusetts relative to all patients in control states. There were also no differential change in the probability of presenting with metastatic disease after reform for all patients in Massachusetts compared to control states (IRR 1.0, 95% CI [0.93 to 1.07], P=0.931).
Figure 1.
Rates of pancreatic resection for pancreatic cancer by insurance coverage in A) Massachusetts and B) control states
* 2006 Insurance Expansion
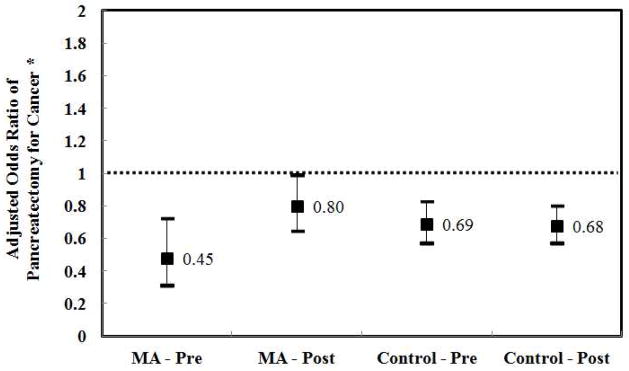
Analyzing the specific impact on GSSP patients, however, the 2006 insurance expansion was independently associated with a 67% increased rate of pancreatectomy (IRR 1.67, 95% CI [1.01 to 2.76], P=0.043) for GSSP patients in Massachusetts relative to control states (Table 2). Prior to reform, GSSP-insured patients had significantly lower odds of undergoing resection when admitted with pancreatic cancer in both Massachusetts (O.R. 0.45, 95% CI [0.31 to 0.73], P=0.001) and control states (O.R. 0.69, 95% CI [0.58 to 0.83], P<0.001) (Figure 2). After reform, the measured disparity decreased in Massachusetts (O.R. 0.80, 95% CI [0.65 to 0.9], P=0.042) while remaining unchanged in control states (O.R. 0.68, 95% CI [0.57 to 0.80], p<0.001). Sensitivity analysis showed no differential trend in pancreatectomy rates for GSSP patients in Massachusetts and control states before insurance expansion (+0.01 cases per 100,000, 95% CI [−0.07 to 0.09], P=0.835). Similarly, there was no differential change in pre-reform rates of surgery between GSSP patients and privately-insured patients in Massachusetts (−0.04 cases per 100,000, 95% CI [−0.11 to 0.02], P=0.189).
Table 2.
Impact of Insurance Expansion on Surgery for Pancreatic Cancer
| Massachusetts (Cases per 100,000 residents) | Control States (Cases per 100,000 residents) | Difference-in-Difference | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Diff | Pre | Post | Diff | Unadjusted Rate Change | IRR | p Value | |
| Pancreatic resection | 0.60 | 1.22 | +0.62 | 0.81 | 0.96 | +0.15 | +0.47 | +1.67 | 0.043 |
| Palliative surgery | 0.93 | 1.62 | +0.69 | 1.30 | 1.42 | +0.12 | +0.57 | +1.56 | 0.001 |
| Any surgery | 1.68 | 3.07 | +1.39 | 2.28 | 2.54 | +0.26 | +1.13 | +1.53 | 0.006 |
IRR, Pancreatectomy (Incident) Rate Ratio, controlling for age, sex, comorbidities, race, and secular trends in entire cohort; Diff, difference; Pre, pre-reform; Post, post-reform
Figure 2.
Impact of government-subsidized/self-pay insurance status on odds of pancreatectomy for pancreatic cancer, before and after insurance expansion
*Adjusted for patient age, sex, race, comorbidities, receipt of chemotherapy or radiation, admission to high-volume hospital, clustering within hospitals, and secular trends. Reference group is privately-insured patients. MA, Massachusetts; Control, control states; Pre, pre-reform; Post, post-reform
Examining secondary outcomes, the Massachusetts insurance expansion was associated with 56% increased rates of GSSP patients undergoing palliative procedures (IRR 1.56, 95% CI [1.19 to 2.04], P=0.001) and a 53% increased rates of undergoing any surgical procedure (IRR 1.53, 95% CI [1.13 to 2.07], P=0.006) compared to control states and secular trends. There was no differential change in the rates of presenting with metastatic disease for GSSP patients in Massachusetts compared to control states (IRR 1.09, 95% CI [0.91 to 1.29], P=0.349).
Before insurance expansion, GSSP patients had a significantly lower odds of admission to high-volume hospitals as compared to privately-insured patients in both Massachusetts (OR 0.62, 95% CI [0.38 to 1.03], P=0.064) and control states (OR 0.72, 95% CI [0.58 to 0.89], P=0.001). Although there was a considerable increase in the percentage of GSSP patients admitted to high-volume pancreatectomy centers across both cohorts, there was no differential change in the probability of admission to high-volume hospital for GSSP patients in Massachusetts compared to control states (0.03 percentage-point decrease, 95% CI [−10.21 to 10.15], P=0.996). After reform, GSSP patients continued to have a lower probability of admission to high-volume hospital as compared to privately insured patients in both Massachusetts (OR 0.61, 95% CI [0.38 to 0.98], P=0.041) and in control states (OR 0.69, 95% CI [0.55 to 0.86], P=0.001).
We also looked at where patients received pancreatectomy for cancer. Greater than 93 percent of all patients in Massachusetts had their operation performed at a high-volume pancreatic center before and after reform. There was no significant difference in the probability of the operation being performed at a high-volume center between GSSP and privately-insured patients in Massachusetts before (OR 0.69, 95% CI [0.23 to 2.10], P=0.513) or after (OR 4.10, 95% CI [0.62 to 27.35], P=0.145). However, GSSP patients in control states had lower probability of having an operation at a high-volume center compared to privately-insured patients before (OR 0.70, 95% CI [0.44 to 1.09], P=0.114) and after (OR 0.48, 95% CI [0.32 to 0.72], P<0.001) insurance expansion in Massachusetts. Difference-in-difference analysis revealed no significant change in the probability of having an operation at a high-volume center for GSSP patients in Massachusetts after reform compared to control states (2.34 percentage-point decrease, 95% CI [−18.31 to 13.59], P=0.772).
Discussion
The incidence of pancreatic cancer continues to rise and the prognosis is not improving. Surgical resection remains the only chance for long-term survival and previous studies show that areas of higher resection rates also have higher survival. Yet it has been repeatedly demonstrated that uninsured and underinsured patients have lower rates of operations and lower survival rates.27,28 In this study, we present data suggesting that the 2006 Massachusetts insurance coverage expansion was associated with a 15% increased rate of admissions and a 67% increased rate of surgical resection for pancreatic cancer for GSSP patients in Massachusetts relative to control states. Secondary analysis found a corresponding 56% increased rate of palliative procedure and a 53% increased rate of any surgical intervention for GSSP in Massachusetts after reform compared to control states.
Dissecting the drivers of disparities in the treatment of pancreatic cancer and identifying solutions has remained elusive. Underinsured patients are more likely to present with advanced disease not amenable to resection. Unfortunately, they are also less likely to be referred for surgical evaluation regardless of resectability. Even if patients with pancreatic cancer are referred, they are less likely to be referred to high-volume pancreatic centers which are concurrently associated with improved delivery of recommended care.29,30 Previous studies have looked to insurance coverage or financial concerns as a driver of socioeconomic disparities in cancer.8,31 To our knowledge, this is the first study to demonstrate that increasing insurance coverage through population-wide health care reform might be associated with increased rates of pancreatic resection for cancer.
Our findings suggest increased admission and resection rates, but no differential change in admissions to high-volume centers or probability of having surgery at high-volume hospital. As such, these data might represent an increase in the discovery of early stage pancreatic cancer. Patients may be presenting to clinicians with symptoms earlier given new insurance coverage and thus be more amenable to surgical resection.32,33 Previous studies have demonstrated an association between reimbursement for and receipt of other cancer screening tests.34 It is therefore possible that providers are increasing utilization of diagnostic testing such as computed tomography scans and tumor marker studies when patient present with subtle early signs such as abdominal pain, hyperbilirubinemia, or pancreatitis. While there was no change in the rates of patient presentation with metastatic disease, our use of an administrative dataset prevents our ability to definitively determine whether or not patients were indeed presenting with earlier stage or resectable pancreatic lesion. Yet given previous studies suggesting a strong association between regions with higher resection rates and overall survival with pancreatic cancer, our findings provide optimistic evidence that insurance expansion can be linked with increased resection rates for pancreatic cancer.
The increase in resection rates for GSSP patients could be a result of increased referral to high-volume centers or surgeons more likely to proceed with resection. While our difference-indifference analysis showed no differential change in admissions to high-volume centers, this analysis is limited by small sample size in Massachusetts and high utilization of high-volume centers for all patients in Massachusetts even prior to reform. With greater than 90% of all pancreatectomy surgeries being performed at high-volume centers in Massachusetts prior to reform, it is therefore not surprising that no significant increase was seen after insurance expansion. Finally, without oncologic data, we can not entirely exclude the possibility of inappropriate surgical resections. Additional evaluation of data with more clinical and oncologic granularity will help determine whether there is indeed an increased diagnosis of early stage, operable pancreatic cancer and that the increased rates of resection are indeed for appropriate surgical candidates. Furthermore, long-term outcomes of these patients who are resected remain unknown.
Although there was an increased rate of resection for GSSP patients in Massachusetts, a statistically significant gap still exists in resection rates compared to privately-insured patients. The decreased disparity in odds of resection is certainly encouraging, especially given the concurrent increased rate of admission. Massachusetts did have a higher disparity in resection rates prior to reform relative to control states. This could reflect limitations in sample size or differences in the healthcare environment between cohorts. Disparities in the diagnosis and treatment of cancer are multifactorial and additional efforts will be needed to dissect out other intervenable, population-specific drivers in disparities. Ongoing education of both patients and providers is needed to combat against the traditionally nihilistic attitude towards this malignancy and its poor prognosis. As centralization of pancreatic cancer treatment continues to localize care within fewer select centers, additional efforts at improving navigability of complex health care systems is also needed. While additional studies will be needed to evaluate the generalizability of Massachusetts’ experience elsewhere in the country, our data suggest that expanding insurance coverage across a population may play an important role in moving towards more equitable care.
The study is bound by a number of key limitations that must be considered when contextualizing findings. First, we used administrative datasets that have the potential for coding errors. However, our data is consistent with prior publications which have used the AHRQ-maintained HCUP databases to evaluate trends in pancreatic cancer.19,35,36 We are also, perhaps most significantly, limited by lack of clinical granularity, oncologic variables, and long-term survival data that may be available in more cancer-specific registries. The SID only capture inpatient hospitalizations and thus we are unable to determine the true denominator of all patients diagnosed with pancreatic cancer who may not be admitted to a hospital during this period. Additional studies with population-level data on all patients diagnosed with pancreatic cancer may provide more detailed information on stage-specific treatment. However, the present study focuses on changes in resection rates over time. It is unlikely that there would be a significant change in the overall incidence of pancreatic cancer in populations that would directionally confound our results. Nonetheless, the inability to include all patients with pancreatic cancer, independent of admission to hospital, does introduce a limitation to the present analysis.
Our primary outcome for this study was pancreatic resection for cancer. Given that this is a very definite event that would be captured by coding and that all patients undergoing resection are admitted to an inpatient hospital, we are unlikely to have significant errors in coding for this outcome. While challenging to state a clear improvement in early diagnosis or long-term survival, our findings at least provide optimistic evidence for the improvement in care for GSSP patients previously identified to be receiving inequitable care for pancreatic cancer.
We cannot fully exclude other ecologic changes that could have impacted changes in care provided in Massachusetts over this time period. To our knowledge, there were no other large policy shifts that occurred in the state that could have resulted in our findings. Similarly, our findings from Massachusetts may not be generalizable to other states or regions. Therefore it will be critical to evaluate the impact of similar insurance expansions (or lack thereof) in other states as a part of the Affordable Care Act. Yet these preliminary findings from Massachusetts provide hopeful data that expansion of insurance across a population may be associated with improved care for pancreatic cancer.
Conclusion
Government-subsidized and self-pay patients have been previously shown to have lower resection rates for pancreatic cancer. Here we report that the 2006 Massachusetts insurance expansion was associated with an increased rate of resection, palliative procedures, or any surgical intervention for pancreatic cancer as compared to three control states. Despite improvements, disparities in the rate of surgery still persist in Massachusetts and control states. Ongoing evaluation of the impact of insurance expansion on equity in pancreatic cancer treatment is needed within Massachusetts and across the United States as other states increase access to care as a part of the Affordable Care Act.
Acknowledgments
Support: Dr Song was supported by a grant from the National Institute on Aging (F30-AG039175).
The authors would like to acknowledge the National Bureau of Economic Research (Cambridge, MA) through whom data were made available. Furthermore, databases are maintained through HCUP Data Partners including the Massachusetts Center for Health Information and Analysis, the Florida Agency for Health Care Administration, and the New Jersey Department of Health, and the New York State Department of Health.
Footnotes
Disclosure Information: Nothing to disclose.
Disclosures outside the scope of this work: Dr Warshaw is a paid consultant to Novo Nordisk.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer Statitistics, 2008. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid liver and pancreas cancers in the United States. Cancer Res. 2014;74:2913–2921. doi: 10.1158/0008-5472.CAN-14-0155. [DOI] [PubMed] [Google Scholar]
- 3.Konstantinidis IT, Dursun A, Zheng H, et al. Metastatic tumors int he pancreas in the modern era. J Am Coll Surg. 2010;211:749–753. doi: 10.1016/j.jamcollsurg.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferrone CR, Marchegiani G, Hong TS, et al. Radiologic and surgical implications of neoadjuvant treatment with FOLFIRINOX for locally advanced and borderline resectable pancreatic cancer. Ann Surg. 2015;261:12–17. doi: 10.1097/SLA.0000000000000867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Truty MJ, Thomas RM, Katz MH, et al. Multimodality therapy offers a chance for cure in patients with pancreatic adenocarcinoma deemed unresectable at first operative exploration. J Am Coll Surg. 2012;215:41–52. doi: 10.1016/j.jamcollsurg.2012.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Billimoria KY, Bentrem DJ, Ko CY, et al. National failure to operate on early stage pancreatic cancer. Ann Surg. 2007;246:173–180. doi: 10.1097/SLA.0b013e3180691579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDowell BD, Chapman CG, Smith BJ, et al. Pancreatectomy predicts improved survival for pancreatic adenocarcinoma: Results of an instrumental variable analysis. Ann Surg. 2015;261:740–745. doi: 10.1097/SLA.0000000000000796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riall TS, Nealon WH, Goodwin JS, et al. Pancreatic cancer int he general population: Improvements in survival over the last decaded. J Gastrointest Surg. 2006;10:1212–1224. doi: 10.1016/j.gassur.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Abraham A, Al-Refaie WB, Parsons HM, et al. Disparities in pancreas cancer care. Ann Surg Oncol. 2013;20:2078–2087. doi: 10.1245/s10434-012-2843-z. [DOI] [PubMed] [Google Scholar]
- 10.Visser BC, Ma Y, Zak Y, et al. Failure to comply with NCCN guidelines for the management of pancreatic cancer compromises outcomes. HPB. 2012;14:539–547. doi: 10.1111/j.1477-2574.2012.00496.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zell JA, Rhee JM, Ziogas A, et al. Race, socioeconomic status, treatment, and survival time among pancreatic cancer cases in California. Cancer Epidemiol Biomarkers Prev. 2007;16:546–552. doi: 10.1158/1055-9965.EPI-06-0893. [DOI] [PubMed] [Google Scholar]
- 12.Constitution of the Commonwealth of Massachusetts. The General Court of Massachusetts; Apr 12, 2006. [Accessed on Feb 17, 2013]. Chapter 58 of the Acts of 2006, An Act Providing Access to Affordable, Quality, Accountable Health Care. at: http://www.malegislature.gov/Laws/SessionLaws/Acts/2006/Chapter58. [Google Scholar]
- 13.Long S. What is the evidence on Health Reform in Massachusetts and How Might the Lessons from Massachusetts Apply to National Health Reform? Urban Institute; Jun, 2010. [Accessed on 1 January 2013]. at: http://www.urban.org/uploadedpdf/412118-massachusetts-national-health-reform.pdf. [Google Scholar]
- 14.Al-Fefaie WB, Muluneh B, Zhong W, et al. Who receives their complex cancer surgery at low-volume hospitals? J Am Coll Surg. 2012;214:81–87. doi: 10.1016/j.jamcollsurg.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Dartmouth Atlas of Health Care. [Accessed on 11 October 2012]; at: http://www.dartmouthatlas.org/
- 16.Health Insurance Coverage in Massachusetts: Results from the 2008–2010 Massachusetts Health Insurance Surveys. Division of Health Care Finance and Policy; Boston, MA: 2010. [Accessed on 20 April 2015]. at: http://archives.lib.state.ma.us/bitstream/handle/2452/109940/ocn725895012.pdf?sequence=1&isAllowed=y. [Google Scholar]
- 17.Birkmeyer JD, Sun Y, Wong SL, Stukel TA. Hospital volume and late survival after cancer surgery. Ann Surg. 2007;245:777–783. doi: 10.1097/01.sla.0000252402.33814.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu JH, Zingmond DS, McGory ML, et al. Disparities in the utilization of high-volume hospitals for complex surgery. JAMA. 2006;296:1973–1980. doi: 10.1001/jama.296.16.1973. [DOI] [PubMed] [Google Scholar]
- 19.McPhee JT, Hill JS, Whalen GF, et al. Perioperative mortality for pancreatectomy: A national perspective. Ann Surg. 2007;246:246–253. doi: 10.1097/01.sla.0000259993.17350.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fong Y, Gonen M, Rubin D, et al. Long-term survival is superior after resection for cancer in high-volume centers. Ann Surg. 2005;242:540–547. doi: 10.1097/01.sla.0000184190.20289.4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Chandra A, Gruber J, McKnight R. The importance of the individual mandate—Evidence from Massachusetts. N Eng J Med. 2011;364:293–295. doi: 10.1056/NEJMp1013067. [DOI] [PubMed] [Google Scholar]
- 23.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: Massachusetts Institute of Technology; 2002. [Google Scholar]
- 24.Donald SG, Lang K. Inference with difference-in-differences and other panel data. Rev Econ Stat. 2007;89:221–233. [Google Scholar]
- 25.Athey S, Imbens GW. Identification and inference in nonlinear difference-in-differences models. Econometrica. 2006;74:431–497. [Google Scholar]
- 26. [Accessed at on 1/11/213];US Census Bureau Historic Tables. http://www.census.gov/hhes/www/hlthins/data/historical/HIB_tables.html.
- 27.Halpern MT, Ward EM, Pavluck AL, et al. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: A retrospective analysis. Lancet Oncol. 2008;9:222–231. doi: 10.1016/S1470-2045(08)70032-9. [DOI] [PubMed] [Google Scholar]
- 28.Krzyzanowska MK, Weeks JC, Earle CC. Treatment of locally advanced pancreatic cancer in the real world: Population-based practices and effectiveness. J Clin Oncol. 2003;21:3409–3414. doi: 10.1200/JCO.2003.03.007. [DOI] [PubMed] [Google Scholar]
- 29.Chang DC, Zhang Y, Mukherjee D, et al. Variations in referral patterns to high-volume centers for pancreatic cancer. J Am Coll Surg. 2009;209:720–726. doi: 10.1016/j.jamcollsurg.2009.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Visser BC, Mia Y, Zak Y, et al. Failure to comply with NCCN guidelines for the management of pancreatic cancer compromises outcomes. HPB. 2012;14:539–547. doi: 10.1111/j.1477-2574.2012.00496.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ward E, Halpern M, Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 32.Loehrer AP, Hawkins AT, Auchincloss HG, et al. Impacted of expanded insurance coverage on racial disparities in vascular disease: Insights from Massachusetts. Ann Surg. 2015 doi: 10.1097/SLA.0000000000001310. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Loehrer AP, Song Z, Auchincloss HG, Hutter MM. Influence of health insurance expansion on disparities in the treatment of acute cholecystitis. Ann Surg. 2015;262:139–145. doi: 10.1097/SLA.0000000000000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Halpern MT, Romaire MA, Haber SG, et al. Impact of state-specific Medicaid reimbursement and eligibility policies on receipt of cancer screening. Cancer. 2014;120:3016–3024. doi: 10.1002/cncr.28704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Finlayson E, Fan Z, Birkmeyer JD. Outcomes in octogenarians undergoing high-risk cancer operation: A national study. J Am Coll Surg. 2007;205:729–734. doi: 10.1016/j.jamcollsurg.2007.06.307. [DOI] [PubMed] [Google Scholar]
- 36.Kotwall CA, Maxwell JG, Brinker CC, et al. National estimates of mortality rates for radical pancreaticoduodenectomy in 25,000 patients. Ann Surg Oncol. 2002;9:847–854. doi: 10.1007/BF02557520. [DOI] [PubMed] [Google Scholar]