Abstract
Treatment of unprotected left main (ULM) in-stent restenosis (ISR) in patients with prior drug eluting stent implantation is challenging. Treatment usually involves complex stenting procedures or bypass grafting. Drug coated balloon (DCB) is relatively new concept which is usually used in treatment of ISR. In a patient of ULM ISR, use of DCBs is a safe, economic and a technically simple option with relatively good outcomes. We report use of simultaneous kissing balloon dilatation with novel sirolimus coated balloons (SCBs) via radial artery to treat ULM ISR.
Keywords: Drug coated balloon (DCB), unprotected left main (ULM), in-stent restenosis (ISR)
Introduction
Management of in-stent restenosis (ISR) in unprotected left main (ULM) bifurcation lesions is very challenging situations, as repeat stent implantation is seldom possible (1). A non-implantable drug coated balloon (DCB) is a treatment option without need for further complex stenting. DCBs are well-established and useful in various clinical indications such as ISR, small vessel and bifurcation lesions. Paclitaxel coated balloon uses cytotoxic paclitaxel drug with various drug carrier like shellac, urea, iopromide and BHTC with improving their performance. Sirolimus is clinically well acceptable cytostatic drug but difficult to adhere on balloon surface. Because of these technical difficulties experience with sirolimus coated balloon (SCB) is limited. ‘Magic Touch’ (Concept Medical Inc., USA) is SCB coated with phospholipid encapsulated sirolimus nanocarriers of dose 1.27 µg/mm2 which has shown long term drug retention in vivo (2,3) and approved in India.
In this report, we describe treatment of ULM bifurcation ISR by simultaneous kissing balloon technique with of two SCB.
Case report
A 68-year-old male presented to our hospital with symptoms of class II angina. He had a known history of coronary artery disease. Two years ago, the patient underwent coronary artery bypass surgery (CABG) with a venous graft to obtuse marginal (OM) and to left anterior descending artery (LAD). One year ago the patient had recurrent angina due to occlusion of both LAD and LM grafts. Cardiac catheterization demonstrated significant bifurcation stenosis of the distal left main coronary artery (LMCA) with proximal stenosis left circumflex artery (LCx) and LAD. The patient underwent bifurcation T-stenting with a small protrusion technique using two everolimus eluting stents (3.50 mm × 24 mm stent LMCA to LAD, and 3.50 mm × 23 mm stent in LCx).
The patient was admitted to our hospital with and repeat angiography showed significant focal ISR in LCx (Figure 1A) and LAD (Figure 1B). In view of the recurrent symptoms and ISR, we planned for re-intervention. The procedure was done through right radial artery access with a 6 F extra backup guide catheter. Both LAD and LCx were wired using Sion blue coronary guide-wires. After sequential semi-compliant balloon dilatation, the ISR segment in the LCx stent was pre-dilated using a 3.50 mm × 10 mm non-compliant balloon (Figure 2A). Post LCx stent dilatation, we noticed some carinal shift to the LAD. Hence the ostial LAD was also pre-dilated with a 3.50 mm × 10 mm non-compliant balloon (Figure 2B) followed by non-compliant kissing balloon dilatation. Post procedure NC balloon dilatation flow is shown in Figure 3. Repeat DES was not considered a good option. Therefore we decided to perform DCB dilatation. Two SCBs (3.50 mm × 15 mm in LAD and a 3.00 mm × 15 mm in LCx) were deployed with prolonged simultaneous kissing balloon technique (Figure 4A). Post-procedure flow was good with no residual stenosis (Figure 4B). Patient was continued on dual antiplatelet therapy and discharged three days after re-intervention. At 6 months, the patient was presented for a routine follow-up appointment with treadmill testing. He was asymptomatic and stress testing was negative with good left ventricular systolic functions.
Figure 1.
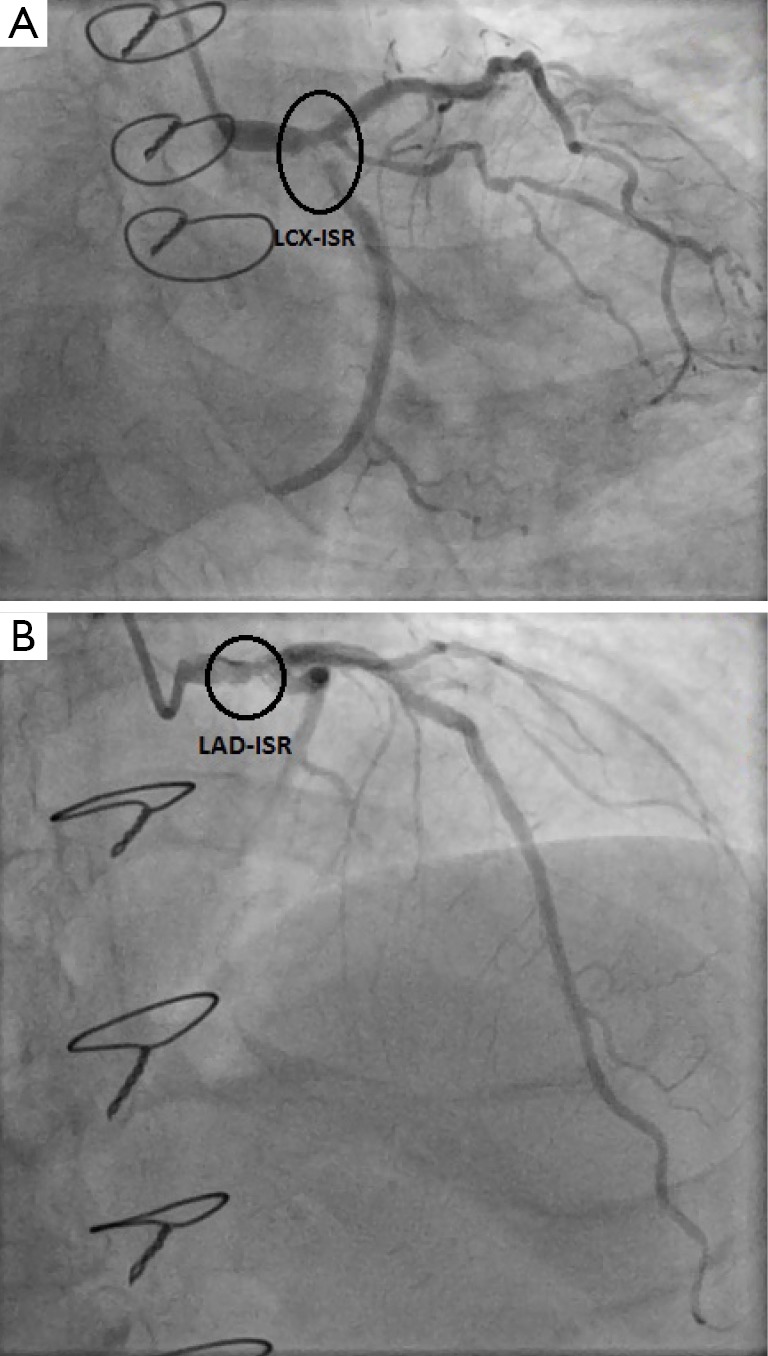
(A) In-stent restenosis in LCx; (B) in-stent restenosis in LAD. LCx, left circumflex artery; LAD, left anterior descending.
Figure 2.
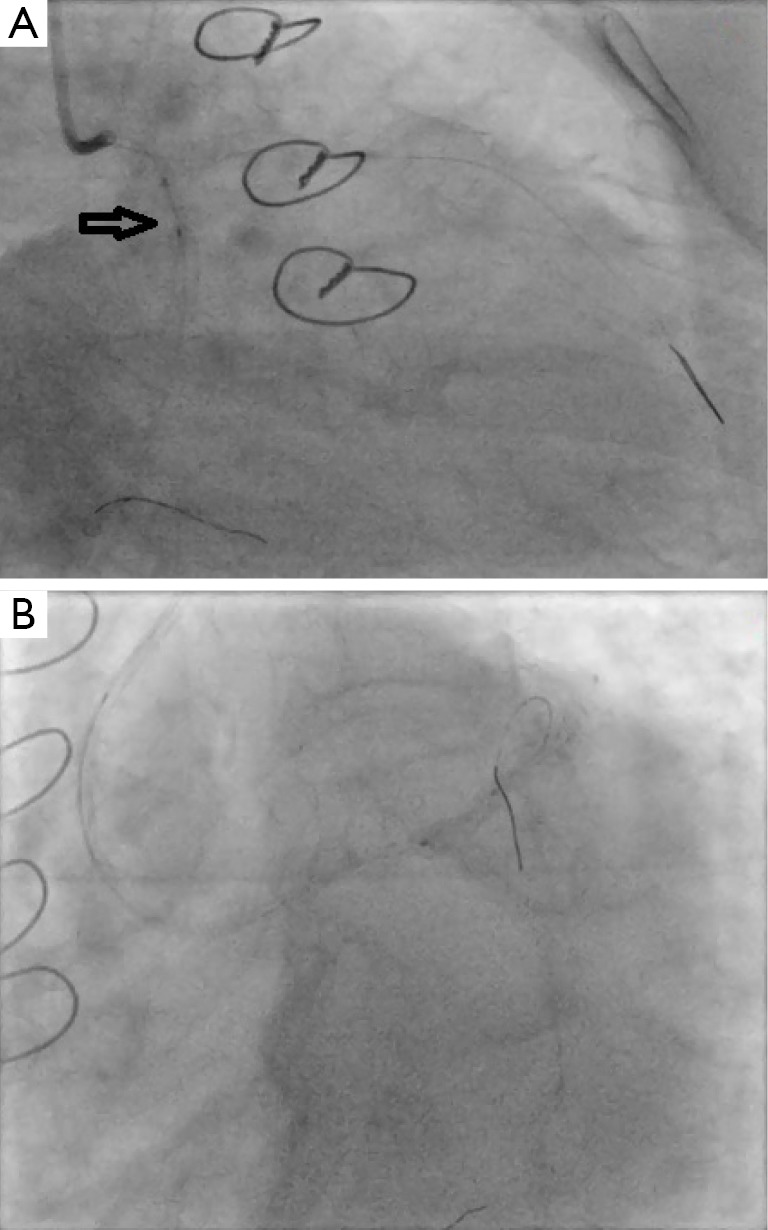
(A) LCx non-compliant balloon dilatation; (B) LAD non-compliant balloon dilatation. LCx, left circumflex artery; LAD, left anterior descending.
Figure 3.
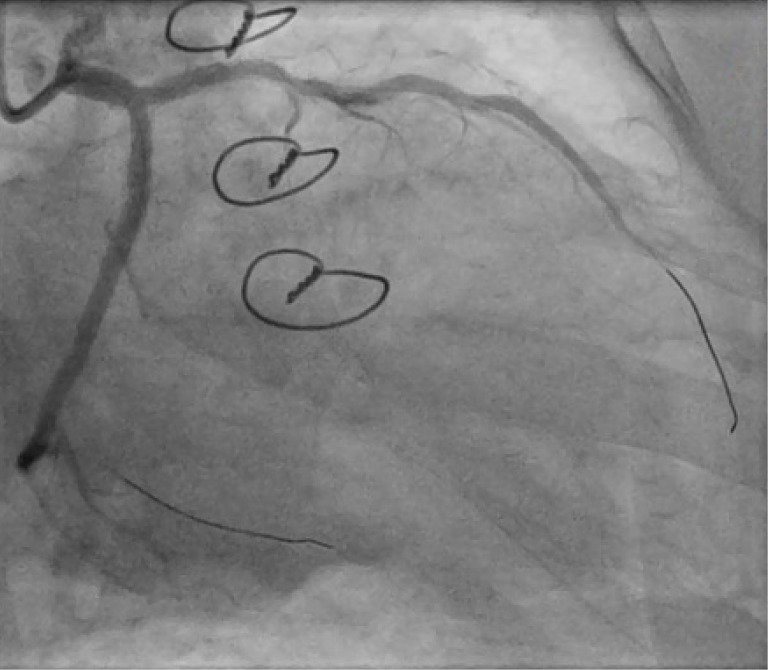
Post non-compliant balloon dilatation in LCx and LAD. LCx, left circumflex artery; LAD, left anterior descending.
Figure 4.
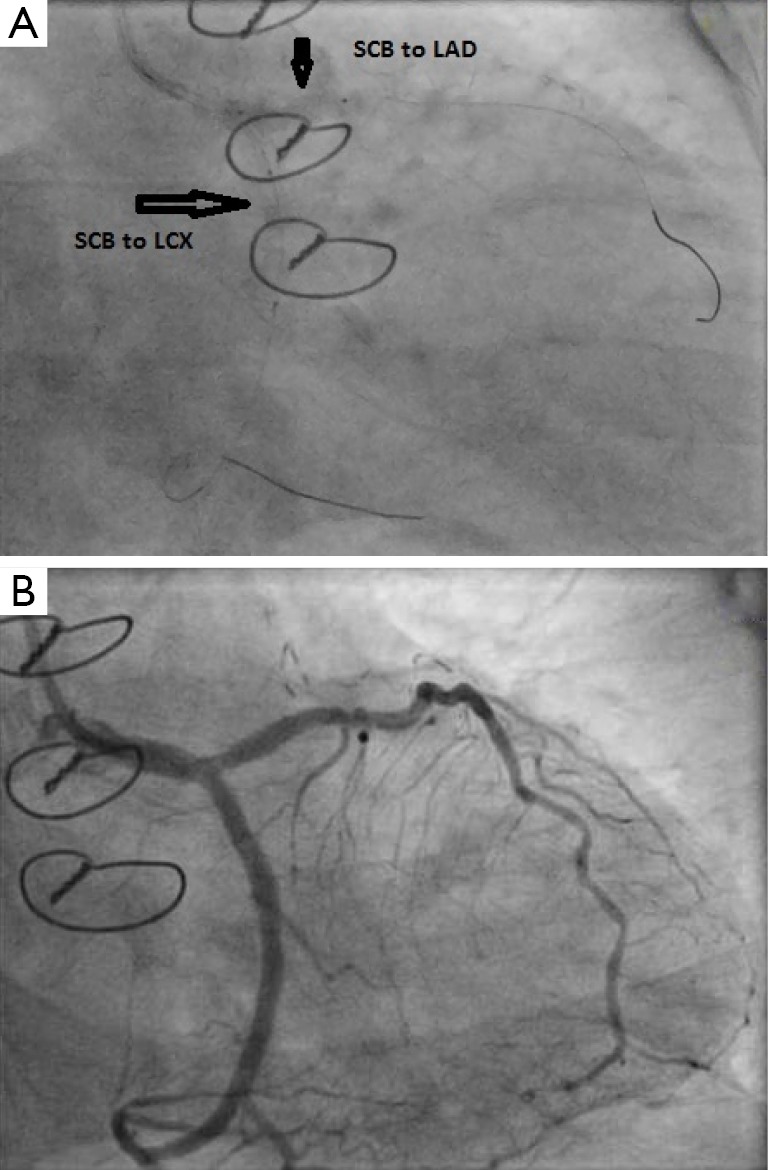
(A) Kissing two magic touch SCB; (B) final flow. SCB, sirolimus coated balloon.
Discussion
Treatment of ISR is a challenging condition with numerous treatment options, and stenting is technically difficult. Heterogeneous drug distribution in the stented segment of current DESs likely contributes to focal restenosis. Simultaneous DCB dilatation in main and side branch is an attractive concept in LMCA-ISR, because it avoids additional metal polymer implantation and provides homogeneous drug deposition to the vessel wall.
Previously reported cases of drug-eluting balloon treatment have used paclitaxel eluting balloons (4,5). Compared to paclitaxel, sirolimus drug eluting balloons have superior safety margin (6), less inflammatory response (7) and lower late lumen loss (8). However, in-tissue absorption of paclitaxel is higher than sirolimus allowing delivery with shorter exposure duration. Currently, the only commercially available SCB is the ‘Magic Touch’. Encapsulated sirolimus nanocarriers adherent to the balloon surface facilitate transfer to the vessels wall upon expansion, and travel to deeper layer of artery. The device has shown its efficacy in various clinical indications (9). Considering uniqueness and better safety profile of sirolimus, SCB could be an attractive future option in repeat percutaneous coronary intervention.
Conclusions
The use of novel SCBs for the treatment of LMCA ISR appears to be a promising approach. However, the experience is limited to case reports and clinical trials are necessary to confirm these anecdotal observations.
Acknowledgements
None.
Footnotes
Conflicts of Interest: Manish Doshi is the owner of Concept Medical Inc., India; Prakash Sojitra is an employee of Concept Medical Inc., India. The other authors have no conflicts of interest to declare.
References
- 1.Colombo A, Moses JW, Morice MC, et al. Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation 2004;109:1244-9. [DOI] [PubMed] [Google Scholar]
- 2.Lemos PA, Farooq V, Takimura CK, et al. Emerging technologies: polymer-free phospholipid encapsulated sirolimus nanocarriers for the controlled release of drug from a stent-plus-balloon or a stand-alone balloon catheter. EuroIntervention 2013;9:148-56. [DOI] [PubMed] [Google Scholar]
- 3.Sojitra P, Yazdani SK, Otsuka F, et al. A Novel Nano Particle Sirolimus Delivery Via Coated Balloon. J Am Coll Cardio 2013;6:S40. [Google Scholar]
- 4.Ielasi A, Anzuini A. Kissing drug-eluting balloons for the treatment of unprotected distal left main bifurcation drug-eluting stent restenosis. Cardiovasc Revasc Med 2012;13:347-9. [DOI] [PubMed] [Google Scholar]
- 5.Sgueglia GA, Todaro D, Stipo A, et al. Simultaneous inflation of two drug-eluting balloons for the treatment of coronary bifurcation restenosis: a concept series. J Invasive Cardiol 2011;23:474-6. [PubMed] [Google Scholar]
- 6.Wang HJ, Lu TL, Huang H, et al. Paclitaxel induces thrombomodulin downregulation in human aortic endothelial cells. Tex Heart Inst J 2011;38:20-6. [PMC free article] [PubMed] [Google Scholar]
- 7.Parry TJ, Brosius R, Thyagarajan R, et al. Drug-eluting stents: sirolimus and paclitaxel differentially affect cultured cells and injured arteries. Eur J Pharmacol 2005;524:19-29. [DOI] [PubMed] [Google Scholar]
- 8.Agostoni P, Cosgrave J, Biondi-Zoccai GG, et al. Angiographic analysis of pattern of late luminal loss in sirolimus- and paclitaxel-eluting stents. Am J Cardiol 2007;99:593-8. [DOI] [PubMed] [Google Scholar]
- 9.Parikh K. A real-world Outcome of sirolimus coated balloon in coronary artery disease. EuroPCR 2015, Paris, 21 May 2015. Available online: http://www.pcronline.com/EuroPCR/EuroPCR-2015/Cardiovascular-innovation-pipeline-Stents-and-devices


