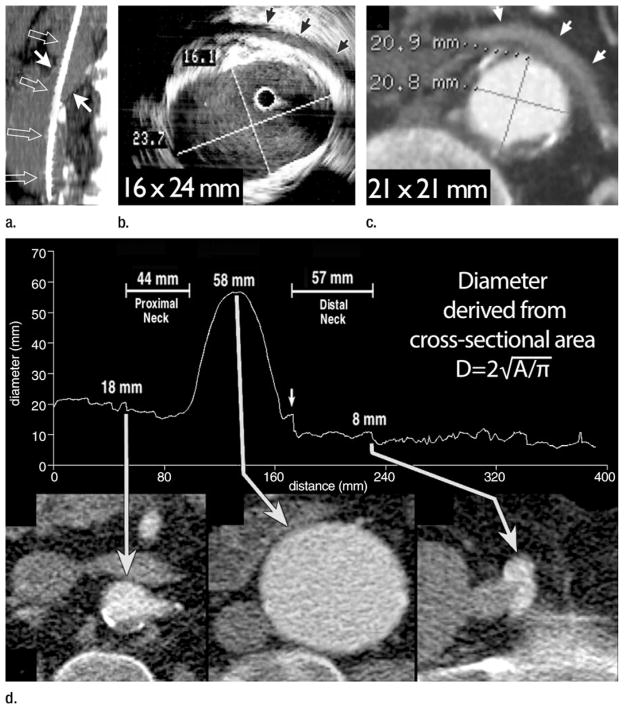
Figure 8.
(a) Sagittal 1.5-cm-thick MIP through an abdominal aortic aneurysm (AAA) depicts an oblique course of intravascular US catheter (open arrows) through the proximal aneurysm neck (solid arrows). A mean intravascular US catheter obliquity of 21.1° ± 2.6 relative to median axis of proximal neck lumen explains the tendency of intravascular US to depict greater eccentricity and maximal transverse diameter of the AAA neck relative to orthogonal CT sections. (b) Intravascular US and (c) double oblique CT reformation orthogonal to median axis of the lumen at level of the anticipated proximal fixation site for a stent-graft. Arrows = left renal vein. Aortic eccentricity is 0.68 for intravascular US and 1.00 for CT. Although intravascular US catheter obliquity may be the cause of some major axis overestimation, US artifacts substantially hinder confident wall identification. Note the distance between perceived anterior wall of the aorta and left renal vein on US image. CT image demonstrates that the majority of these high-level echoes are artifacts. (d) Following automated extraction of the median centerline of the aorto-right iliac lumen, oblique reformations are generated every millimeter along length of the centerline. The average diameter derived from cross-sectional area is plotted relative to longitudinal position along the centerline. CT sections correspond to the positions indicated by arrows on the plot. A small localized peak in the curve indicates origin of right and inferior-most renal artery (left arrow). Diameter immediately distal to this peak is 18 mm, corresponding to proximal stent-graft fixation site. Middle long arrow indicates maximum aneurysm diameter, which is 58 mm. Transition from aorta to right common iliac artery is apparent from an abrupt transition in cross-sectional area (short arrow). Further reduction in diameter indicates the origin of the right external iliac artery, which is 8 mm at its origin (right long arrow). In addition to providing measurements of diameter, distance along the path is readily ascertained, providing information on aortic segment lengths. (Part d reprinted, with permission, from reference 66.)