Abstract
Objective
The modest efficacy of psychological interventions for youth depression, including evidence-based psychotherapies (EBPs), suggests a question: Do the therapy components match the coping strategies youths find helpful when dealing with depressed mood? Answering this question may help strengthen treatments.
Method
We asked 105 middle schoolers across a range of depression symptom levels to identify the coping strategies they used when they felt sad (habitual responses), and those that made them feel better (perceived-effective responses). Habitual and perceived-effective responses were coded for resemblance to EBPs, and each youth’s habitual responses were coded for their match to the youth’s perceived-effective responses.
Results
Most perceived-effective responses (92.6%) matched EBP components (most frequent: Behavioral Activation); however, 65.0% of the EBP components did not match any youth’s habitual or perceived-effective responses. Youths at higher depression symptom levels were significantly more likely than low-symptom youths to report (a) habitual responses that did not match EBP components, (b) habitual responses that did not match their own perceived-effective responses, and (c) perceiving no effective response.
Conclusions
The higher their depression symptom level, the less likely youths were to use strategies identified by researchers and perceived by themselves as effective, and the less likely they were to identify any perceived-effective coping strategy. The findings suggest a need to (a) determine which EBP components do in fact enhance youth coping, (b) design the most effective ways to help youths master those effective components, and (c) facilitate more frequent use of those strategies the youths already find effective.
Keywords: children, adolescents, depression, coping, evidence-based psychotherapies
Depression has been identified as the third most disabling disease and the most disabling mental disorder in the world (World Health Organization, 2008). The effects of depression on children and adolescents (herein, collectively, “youths”) are serious and often long-lasting (Rice, Lifford, Thomas, & Thapar, 2007). Unfortunately, the efficacy of depression interventions for youths is rather modest. The largest meta-analysis of randomized controlled trials (RCTs) of psychotherapy for youth depression to date, most of which tested behavioral or cognitive treatments, revealed a small to medium treatment effect (d = 0.34), significantly smaller than that for other youth problems (Weisz, McCarty, & Valeri, 2006). These results are consistent with those of meta-analyses of prevention programs for youth depression (Merry et al., 2011, d = 0.20 with no intervention controls; Stice, Shaw, Bohon, Marti, & Rohde, 2009, r = .15, equivalent to d = .30). Based on the mean effect sizes obtained, the probability that a randomly selected youth in an intervention condition would have a better outcome than a randomly selected youth in a control condition is barely above chance (55% – 59%, see McGraw & Wong, 1992). In light of increasing rates of depression starting in the middle school years (Merikangas et al., 2010), the high probability of recurrence (Costello et al., 2002), and the apparent risks of antidepressant use for youths (Hetrick, McKenzie, Cox, Simmons, & Merry, 2012), the modest effects of existing interventions for youth depression suggest the potential value of using new strategies to examine these interventions and generate ideas for strengthening them.
Most of the strategies for building and refining youth depression interventions to date have relied mainly on the perspective of adults—primarily theorists, researchers, and therapists (see Weisz & Kazdin, 2010)—and these have generated useful ideas. In the present study, we used a complementary approach that draws from the perspective of youths themselves: assessing the degree of congruence between what youths reported about their own experiences dealing with depressed mood, and the contents of youth depression interventions that show substantial evidence of efficacy, that is, interventions classified as evidence-based psychotherapies (EBPs). Youth depression EBPs are largely programs designed to build specific coping skills. Examples include the cognitive behavioral therapy (CBT) protocol, Adolescent Coping with Depression Course (Clarke, Lewinsohn, & Hops, 1990); the interpersonal therapy (IPT) protocol, Interpersonal Therapy-Adolescent Skills Training (Young, Mufson, Davies, 2006); and types of behavior therapy (BT) such as relaxation training (e.g., Kahn, Kehle, Jenson, & Clark, 1990). Some coping skills may involve taking action to bring existing conditions into line with one’s wishes and goals, as in primary control coping, and others may involve altering oneself (e.g., one’s expectations and interpretations) to adjust to those conditions, thereby controlling their personal psychological impact, as in secondary control coping (Compas, Connor-Smith, Saltzman, Thomsen, & Wadsworth, 2001; Rothbaum, Weisz, & Synder, 1982). EBPs for youth depression often teach youths primary and secondary control coping skills, in both cases with the aim of improving mood (e.g., Bearman, & Weisz, 2009).
We thought it would be useful to assess the extent to which the coping skills found in EBPs correspond to the coping approaches young people commonly use when they experience depressed mood, and particularly to the coping approaches young people find effective in alleviating depressed mood. We reasoned that close matches between EBP contents and what youths themselves practice and find effective might suggest EBP components that deserve special emphasis, and that any mismatches might suggest possible adjustments that could refine and strengthen EBPs for youth depression. With this in mind, we asked middle schoolers to describe how they responded when they experienced depressed mood. We asked them to identify (a) what they usually did when feeling sad, and (b) what they perceive makes them feel better; herein, we refer to these coping responses as habitual responses and perceived-effective responses respectively. We coded these habitual and perceived-effective responses for whether they matched components of EBPs for youth depression, and we coded each youth’s habitual responses for whether they matched any of that youth’s perceived-effective responses. To probe for any differences between youths who had been more vs. less successful in addressing depression, we sampled youths across a range of depression symptomatology. By applying this approach to this sample, we were able to investigate several questions about coping and depression symptoms.
First, we examined the extent to which youths’ coping responses corresponded with EBP components to determine whether current EBPs have done a good job of capturing strategies youths habitually use, and those the youths themselves find effective. We also identified which specific EBP components corresponded with youths’ habitual responses, and which did not—those that did could be considered to reflect “common practice” in youth coping, and those that did not may reflect coping strategies least likely to be deployed without therapy. The latter might thus be candidates for special emphasis in treatment or prevention programs, to thus be added to the skill set youths can use to ameliorate their depression. We also identified which EBP components corresponded with youths’ perceived-effective responses, and which did not, to generate hypotheses about ways to simplify or streamline EBPs. One criticism of some EBPs is that they use a “kitchen sink” approach, piling on multiple components (e.g., behavioral activation, relaxation, cognitive work), when slimmer treatments might be as effective, more efficient, and more disseminable. EBP components not perceived as effective in everyday use could be candidates for elimination, if further empirical support is obtained from dismantling studies.
Second, we investigated whether level of depression symptoms was associated with the extent to which (a) youths’ habitual responses matched components of EBPs for depression, (b) youths’ habitual responses matched responses youths perceived as effective, and (c) youths perceived any coping response as effective. Given the strong focus of EBPs on teaching youths coping skills to improve their mood, we predicted that level of depression symptoms would be negatively associated with degree of match between habitual responses and depression EBPs. Because theory and research links depression to deficits in emotion regulation (Joormann & D’Avanzato, 2010; Nolen-Hoeksema, 2012), it is plausible that youths with more depression symptoms may have trouble habitually using the coping strategies that they themselves find effective, and identifying perceived-effective coping strategies in the first place. Therefore, we predicted that level of depression symptoms would be negatively associated with degree of match between habitual responses and perceived-effective responses, and with the ability to identify perceived-effective responses.
Third, we assessed whether depression symptom level was associated with the extent to which (a) youths’ perceived-effective responses matched components of EBPs for depression, and (b) youths’ habitual and perceived-effective responses matched specific EBP components. Although prior literature offered no clear basis for predictions, it could be useful to understand whether high-symptom youths are any less likely than their low-symptom peers to perceive coping strategies resembling EBP components as effective. Additionally, identifying specific EBP components that differentiate high- and low-symptom youths may shed light on potentially useful therapy content that depressed youths may require special support to master. Thus, we planned a priori to conduct analyses to answer these research questions even in the absence of specific predictions.
Finally, we explored whether youths suggested new coping strategies that are not evident in current EBPs. Current youth depression treatment approaches have been derived largely from the adult treatment literature (David-Ferdon & Kaslow, 2008). Coping strategies youths perceive as effective, but that are not components of current EBPs, might suggest new ideas about treatment components that are potentially beneficial and more developmentally appropriate.
We focused on middle schoolers because depression rates begin to surge in early adolescence, with the median age of mood disorder onset among youths documented at 13 years (Merikangas et al., 2010). In addition this period marks the often stressful transition from childhood to adolescence, involving significant changes in biology, cognitive abilities, and social environments. Thus researchers (e.g., Silk et al., 2007) have highlighted middle school as a particularly rich period for studying stress, coping, resilience, and depression. Furthermore, middle schoolers were thought to have adequate introspective ability, verbal fluency, and experience with depression symptoms to provide meaningful responses in the study measures. We also examined the association between gender and coping, and the interaction between gender and depression on coping, because gender may moderate the relation between depression and coping. Early adolescence is the point at which girls’ depression symptoms begin to accelerate beyond those of boys (Ge, Lorenz, Conger, Elder, & Simons, 1994); this has been attributed in part to gender differences in adolescents’ use of coping strategies (Nolen-Hoeksema, 2012). Thus we tested the main effect of depression symptoms on coping adjusting for gender, and the interactive effect of depression symptoms and gender on coping.
Method
The study complied fully with the internal review board of Judge Baker Children’s Center, Boston, MA.
Sampling Strategy
All 6th and 7th grade students from two Boston area middle schools were invited to participate in the study, with informed caregiver consent and youth assent obtained. In an initial screening, 292 youths completed the Children’s Depression Inventory (CDI; Kovacs, 2003). To obtain a sample with varying depression symptomatology, youths with higher CDI scores were oversampled. All 55 youths who scored 9 or higher, and a randomly selected subsample of 50 youths who scored below 9, completed additional measures described below. We limited the subsample of less symptomatic youths to 50, with the goal of achieving a full sample CDI mean of approximately 9, which corresponds to the 46th–61st percentile across CDI normative samples (Kovacs, 2003). This approach resulted in good variability in CDI scores around a mean of 8.5 (SD = 7.0, range = 0–34).
Participants
Participants were 105 youths aged 11 to 13 years (M = 11.7, SD = 0.65); 52.4% female; and 60.0% European American, 14.3% multi-ethnic, 11.4% African or African American, 7.6% Hispanic or Latin American, 1.9% Asian or Asian American, 3.8% other, and 1.0% not reporting their ethnicity (see Appendix for ethnic breakdown by CDI score). Most (69.5%) were from intact two-parent families, 27.6% had divorced or separated parents, and 2.9% lived with adults other than their parents. Depression symptom level was not significantly associated with any of these demographic characteristics.
Measures
Depression symptom composite
We used a continuous variable composite of three depression symptom measures for all analyses to maximize precision and optimize measurement reliability.
The first measure was the CDI, a widely used measure of depression symptoms for youths aged 7 to 17 years that is supported by substantial reliability and validity data (e.g., Kovacs, 2003). The CDI comprises 27 items that each pose three graded alternatives, one of which is chosen (e.g., “I am sad once in a while.” “I am sad many times.” “I am sad all the time.”). The present study used a 26-item version that excluded a suicide ideation-intent item due to school officials’ concerns about suggesting suicide to children who might otherwise not have considered it. The total scale score (Cronbach’s α = .88) was used to compute the depression symptom composite. No data were missing on this measure.
The second measure was the DSM-oriented Affective Problems scale from the Youth Self-Report (YSR; Achenbach, Dumenci, & Rescorla, 2003). A self-report measure of emotional and behavioral problems for ages 11 to 18 years that is supported by extensive normative and psychometric data (e.g., Achenbach & Rescorla, 2001), the YSR comprises 118 items rated on a three-point Likert scale. We used versions of the CDI and YSR Affective Problems scale that excluded two items on suicidal or self-harm behavior and suicidal ideation due to similar concerns as described above for the excluded CDI item. The DSM-oriented Affective Problems scale score (Cronbach’s α = .74), computed by summing 11 items (excluding the 2 deleted items) corresponding to the symptoms of major depression, was used to compute the depression symptom composite. One response was missing from two items, and two responses were missing from one item.
The third measure was the depression module of the Diagnostic Interview Schedule for Children, Version 4 (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). The DISC-IV is a structured diagnostic interview comprising yes/no questions designed for administration by lay interviewers to generate DSM-IV-TR (American Psychiatric Association, 2000) diagnoses. We summed up the “yes” responses on the 13 unique symptoms of major depressive disorder, dysthymic disorder standard criteria, and dysthymic disorder with alternative research criterion B (see American Psychiatric Association, 2000, p. 774–775) to generate a DISC depression symptom score (Cronbach’s α = .87). No data were missing on this measure.
The three depression symptom measures were highly intercorrelated: CDI–YSR r = .76, CDI–DISC r = .61, and YSR–DISC r = .58. These high intercorrelations, together with the high internal consistency of each measure and minimal missing data, support creating a depression symptom composite measure via unit weighting. Thus we standardized each measure and took the mean of the three measures, resulting in a centered depression symptom composite measure (M = 0.00, SD = 0.88, Cronbach’s α = .85).
Structured interview
Research assistants interviewed the youths individually, asking them to identify events that made them “feel down, or sad, or gloomy.” To assess habitual responses, research assistants asked: “When these bad things happen, and you feel down, sad, or gloomy, what do you usually do? Tell me three things that you are most likely to do when you feel really bad.” To assess perceived-effective responses, research assistants asked “When you are feeling down, sad, or gloomy, have you figured out some things you can do that will make you feel better?” Youths who said yes were asked, “What are the top three things you do that make you feel better when something bad has happened?” Youths’ responses were written down verbatim.
Coding of Coping Responses
Match between youth responses and EBP components
We coded coping responses for whether they matched components of CBT, IPT, and BT—the treatments designated as “well-established” or “probably efficacious” EBPs for youth depression in David-Ferdon and Kaslow’s (2008) systematic review. Among specific treatment protocols identified by David-Ferdon and Kaslow (p. 80, p. 85) as having outperformed control groups, we selected all three IPT and all three BT protocols; because there were numerous CBT protocols, we selected four that had outperformed control groups in two RCTs. We were inclusive in selecting treatment protocols in order to construct codes that were representative of each treatment orientation. We created 87 fine-grained codes grouped under 20 EBP components with reference to the treatment protocols and by consensus among the three of us. For example, the EBP component, Relaxation, has five codes: deep breathing exercises, progressive muscle relaxation, positive imagery, relaxation through other specific means (e.g., listening to music to relax), and relaxation through vague/unspecified means (e.g., trying to keep calm). Table 1 describes the 20 components. Details of the selection of EBP components and coding procedures are provided in the Appendix.
Table 1.
Evidence-Based Psychotherapy (EBP) Components Endorsed by Youths, EBP Components Not Endorsed by Youths, and Not-EBP-Component Codes Endorsed by Youths
| EBP Components Endorsed by Youths | Percentage of Youths Endorsing |
EBP | |||
|---|---|---|---|---|---|
| Habitual | Perceived- Effective |
CBT | BT | IPT | |
| 1. Behavioral Activation: engaging in activities that are enjoyable, use up energy, or involve friends/family, success, creativity, religion/spirituality, or helping others | 59.6 | 70.9 | ✓ | ||
| 2. Increasing Social Support: talking with others, getting advice, information, understanding, and comfort from others, acquiring/strengthening relationships | 23.8 | 30.0 | ✓ | ✓ | ✓ |
| 3. Problem Solving: e.g., identifying the problem, generating solutions and weighing their pros and cons, taking action, evaluating the outcome, anticipating or preventing future problems, and social problem solving including assertiveness, negotiation, empathy, communication analysis, active listening, warm or nonblaming responses | 17.3 | 18.4 | ✓ | ✓ | ✓ |
| 4. Distraction: thinking about something else, doing something to occupy oneself | 11.5 | 11.7 | ✓ | ||
| 5. Cognitive Strategies: e.g., evaluating the accuracy or helpfulness of thoughts, generating realistic or positive alternatives, thinking about the good sides of a bad situation, thought interruption, setting aside worry time, identifying negative thoughts and their link to feelings and behavior | 10.6 | 5.8 | ✓ | ✓ | |
| 6. Practice or Perseverance: practicing to build skills or to do better at something, homework, role plays, keep trying, try again next time | 8.7 | 3.9 | ✓ | ✓ | ✓ |
| 7. Relaxation: deep breathing, progressive muscle relaxation, positive imagery | 4.8 | 1.9 | ✓ | ✓ | |
| EBP Components Not Endorsed by Youths | EBP | ||
|---|---|---|---|
| CBT | BT | IPT | |
| 8. Goal Setting: e.g., identifying goals and barriers to goals, breaking goals into smaller steps, planning to achieve goal, charting progress, evaluating outcomes | ✓ | ✓ | ✓ |
| 9. Modeling: using others as a guide for how to act | ✓ | ✓ | ✓ |
| 10. Self-Monitoring: collecting information on one's feelings, behaviors, and events | ✓ | ✓ | ✓ |
| 11. Psychoeducation: learning about depression and how negative feelings may arise | ✓ | ✓ | ✓ |
| 12. Reinforcement: making a plan to reward self for working harder or doing better | ✓ | ✓ | |
| 13. Identifying Stress-Related Situations: identifying situations that make one feel tense or uncomfortable | ✓ | ✓ | |
| 14. Understanding Affect: labeling emotions, understanding situations leading to positive or negative feelings | ✓ | ✓ | |
| 15. Understanding and Finding Meaning in Loss and Change: mourning death or relationship loss, assessing losses and gains from change, identifying new demands | ✓ | ✓ | |
| 16. Personalizing Treatment: identifying best- fit skills for oneself | ✓ | ✓ | |
| 17. Building a Positive Sense of Self: recognizing strengths, broadening self-definition | ✓ | ||
| 18. Understanding Relationships and their Link to Affect: identifying important relationships, recognizing that they influence mood | ✓ | ||
| 19. Expressing Affect to Others : verbal communication of feelings to others in a purposeful, intentional, and constructive way | ✓ | ||
| 20. Limited Sick Role: acknowledging that when depressed, one can't do things as well as before, but will gradually increase activities and responsibilities | ✓ | ||
| Not-EBP-Component Codes Endorsed by Youths | Percentage of Youths Endorsing |
|
|---|---|---|
| Habitual | Perceived- Effective |
|
| A. Separating Self Physically or Mentally From the Stressor | ||
| 1. Being alone | 10.6 | 2.9 |
| 2. Going to one’s room without description of activity in the room | 7.7 | 2.9 |
| 3. Staying away from people or things that are upsetting or remind one of the problem | 5.8 | 1.9 |
| 4. Trying not to think about it or to forget about it | 2.9 | 1.0 |
| 5. Going upstairs | 0 | 1.0 |
| 6. Ignoring the situation, avoiding it | 1.9 | 0 |
| B. Refraining from Activity | ||
| 7. Lying around or sleeping a lot | 3.8 | 4.9 |
| 8. Sitting, doing nothing, slouching, rocking | 2.9 | 1.0 |
| 9. Not talking to others, keeping quiet | 2.9 | 0 |
| C. Noncommunicative expression of feelings | ||
| 10. Crying | 10.6 | 1.0 |
| 11. Punching a pillow | 1.0 | 1.0 |
| 12. Writing feelings down on paper and ripping the paper up | 0 | 1.0 |
| 13. Yelling | 2.9 | 0 |
| 14. Yelling for mother and telling on sister | 1.0 | 0 |
| 15. Throwing things on the floor | 1.0 | 0 |
| 16. Stomping | 1.0 | 0 |
| D. Other Not-EBP-Component Codes | ||
| 17. Feeling angry | 1.9 | 0 |
| 18. Feeling frustrated, annoyed, grouchy, upset | 3.8 | 0 |
| 19. Getting into arguments | 1.0 | 0 |
| 20. Doing something the other person does not like | 1.0 | 0 |
| 21. Hitting the person | 1.0 | 0 |
| 22. Getting back at the person | 1.0 | 0 |
| 23. Giving brother a wedgie | 1.0 | 0 |
| 24. Accepting problem and carrying on with life | 1.0 | 0 |
| 25. Keeping feelings under control and then letting them out at an appropriate time | 1.0 | 0 |
| 26. Keeping feelings to self | 1.0 | 0 |
| 27. “Same as usual” | 1.0 | 0 |
| 28. Thinking about negative things | 1.0 | 0 |
Note. CBT = cognitive-behavioral therapy; BT = behavioral therapy; IPT = interpersonal therapy.
Match between habitual and perceived-effective responses
To facilitate coding the match between youths’ habitual and perceived-effective responses, we created 28 additional fine-grained codes for responses coded as “not an EBP component” by logical grouping of similar responses together, with reference to items in the Responses to Stress Questionnaire (RSQ; Connor-Smith, Compas, Wadsworth, Thomsen, & Saltzman, 2000). Table 1 shows the 28 codes. We determined whether each habitual response had a fine-grained code (EBP or Not-EBP component) that matched the code of any of the youth’s perceived-effective responses using SPSS Statistics Version 20.
Coding procedures and reliability
The coders were a doctoral student and two research assistants at the Master’s and Bachelor’s level. Coders chose one code that most closely resembled each coping response while blind to the status of each response as habitual vs. perceived-effective (to preclude bias—e.g., coding more perceived-effective responses than habitual responses as matching EBP components). The coders coded a randomly selected 15% of responses for training and practice purposes, discussing coding decisions when in doubt. Then they independently coded another randomly selected 20% of the responses and showed very good interrater reliability (κ = 0.86 for EBP-component codes, κ = 0.83 for not Not-EBP-component codes). The doctoral student had been involved in creating the coding manual from review of the literature, thus she had the most relevant exposure and experience, and was designated the master coder. When the coders’ responses were not identical for the reliability items, the master coder’s coding was used, and interrater reliability was computed by comparison to her codes. The master coder coded all the remaining responses.
Data-Analytic Plan
We first examined the correspondence between the youths’ coping responses and EBP components and identified those EBP components the youths did or did not perceive as effective, regardless of depression symptom level. Second, we tested the three study hypotheses—that youths’ depression symptom levels would be negatively associated with the extent to which (a) their habitual responses matched EBP components, (b) their habitual responses matched their perceived-effective responses, and (c) they were able to identify perceived-effective responses. Third, we conducted planned a priori analyses of research questions for which we did not have specific predictions: whether depression symptom level was associated with the extent to which (a) youths’ perceived-effective responses matched EBP components, and (b) youths’ habitual and perceived-effective responses matched specific EBP components. Analyses were conducted using SAS Version 9.3 PROC LOGISTIC. Finally, we qualitatively examined youths’ perceived-effective responses that did not match EBP components and discussed their potential as therapeutic strategies for depressed youths.
Results
Correspondence between Youth Coping and Evidence-Based Psychotherapies
Table 1 shows the extent of match between youth coping responses and EBP components. A striking feature of the table is that across all youths in the study, only seven of the 20 EBP components were identified as habitual or perceived-effective responses. Behavioral Activation was the most frequently endorsed, followed by Increasing Social Support, Problem Solving, Distraction, Cognitive Strategies, Practice or Perseverance, and Relaxation. All seven are CBT components, four are also IPT-A components, and four are also BT components. Youths endorsed each EBP component at similar rates in their habitual and perceived-effective responses. By contrast, 13 of the components included by treatment developers as part of the EBPs were not identified as either habitual or perceived-effective responses by a single youth in the sample. Notably, four of these never-identified components—goal-setting; modeling the behavior of others; self-monitoring one’s thoughts, feelings, and behavior; and psychoeducation—are found in all three EBPs for youth depression. Six additional components not endorsed by any youth are core elements of CBT, which is by far the most widely practiced and thoroughly researched of the three EBPs.
Analyses Testing Three Study Hypotheses
Coping variables
Tests of the three hypotheses involved three coping variables.
Proportion of habitual responses matching EBP components: computed by dividing the number of habitual responses matching EBP components by the total number of habitual responses reported by each youth. For example, youths who reported a total of three habitual responses, of which one matched an EBP component, would have 1/3 of responses matching an EBP component. Proportion outcomes account for the variation in total number of habitual or perceived-effective responses reported and have been recommended over frequency outcomes (see Connor-Smith et al., 2000). Although there are five possible proportions (1, 2/3, 1/2, 1/3, 0), we collapsed the middle three to increase cell frequencies, thereby generating an ordinal variable with three levels—all (1), some (2/3, 1/2, 1/3), and none (0).
Proportion of habitual responses matching perceived-effective responses: computed by dividing the number of habitual responses that matched one of the youth’s own perceived-effective responses by the total number of habitual responses the youth reported. We generated a three-level ordinal variable using the same approach as for the previous variable.
Total number of perceived-effective responses (i.e., 0, 1, 2, 3); we collapsed the middle two, generating an ordinal variable with three levels—zero, one/two, and three.
Hypothesis-testing procedures
To test our three hypotheses, we conducted logistic regression analyses with depression symptoms as the main predictor and the three coping variables as outcomes, with gender and the Depression Symptoms × Gender interaction as additional predictors (for reasons noted previously). We considered depression symptoms rather than coping as the predictor because youths were sampled on the basis of their depression symptom levels, and the ordinal nature of the coping variables makes logistic regression the most appropriate approach. Each three-level outcome may be modeled with two binary logistic regression models using the same set of predictors. For example, Model 1 tests whether the odds of youths reporting all habitual responses matching EBP components differ significantly across depression symptom levels; Model 2 tests whether the odds of youths reporting at least some habitual responses matching EBP components differ significantly across depression symptom levels. If the two odds ratios yielded by the two models are not significantly different, then they can be summarized with one odds ratio estimated by a single ordinal logistic regression model—this is the proportional odds assumption (Agresti, 2007). If this assumption was violated (as indicated by a significant result on the score test of the proportional odds assumption), we fitted two binary logistic regression models for each combination of predictors and outcome. If the proportional odds assumption was met, we fitted one ordinal logistic regression model for each predictor–outcome combination. We first used the Wald test to estimate significance levels of predictors in all models, then we used the likelihood ratio (LR) test to ascertain the significance levels in the final model (see Agresti, 2007). We also tested the assumption that continuous predictors are linearly related to the log odds of the outcome using the Box-Tidwell approach (Hosmer & Lemeshow, 2000). Finally, we used the Hosmer-Lemeshow goodness-of-fit test to assess binary logistic regression models with the continuous depression symptom predictor (this test is unsuitable for models with only categorical predictors or with ordinal outcomes; Agresti, 2007). Because the validity of the ordinal models depends on the validity of the two binary models that could model each ordinal outcome, and because global goodness-of-fit tests are not available for ordinal logistic regression models, we tested the linearity assumption and goodness-of-fit tests for the two binary models that could model each ordinal outcome using the approaches described above (see Bender & Grouven, 1997).
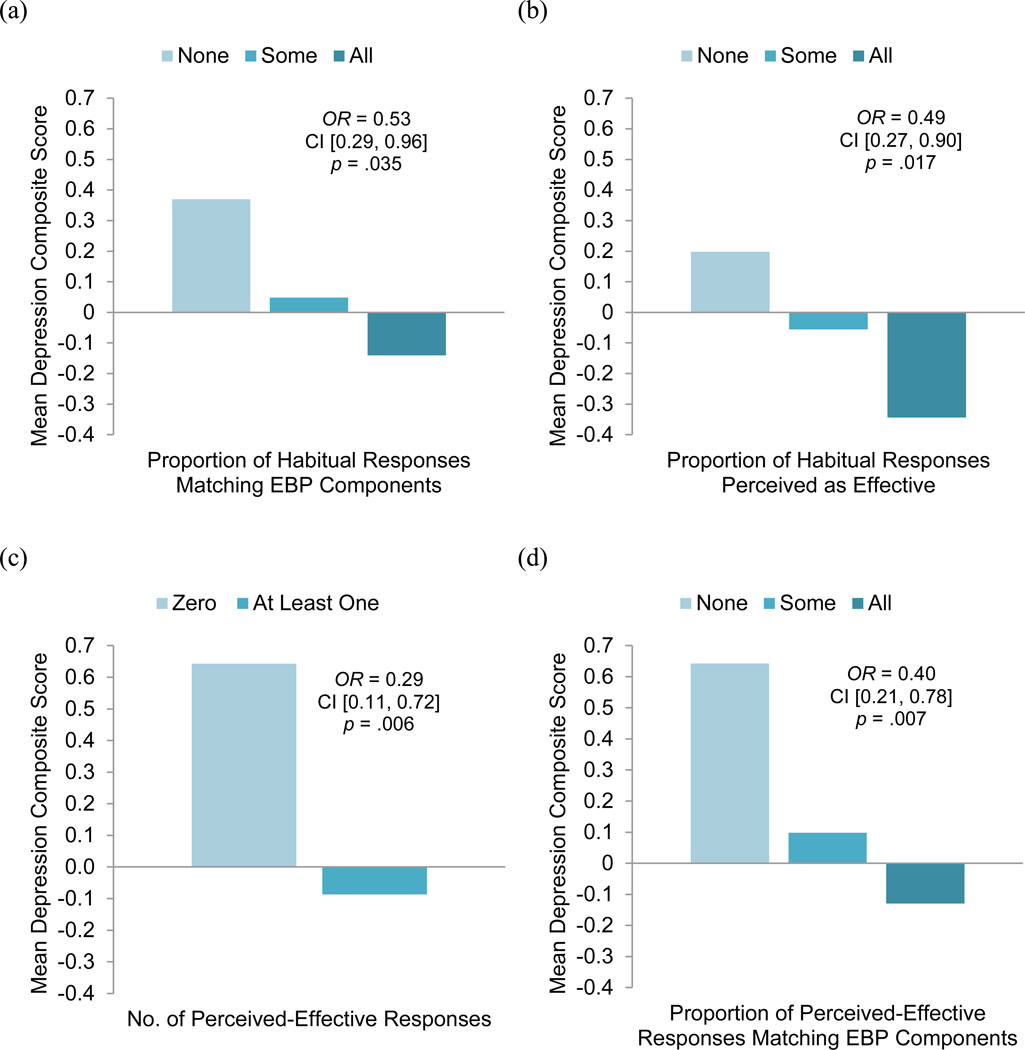
Test of hypothesis 1: Level of depression symptoms will be negatively associated with degree of match between habitual responses and EBP components
Analyses involving habitual responses included 104 youths (1 youth did not answer the relevant questions), of whom 49.0% reported All habitual responses, 36.5% reported Some, and 13.5% reported None matching EBP components. Table 2a shows the taxonomy of models that display the fitted relationship between youths’ depression symptoms, gender, and the proportion of habitual responses matching EBP components. The proportional odds and linearity assumptions were met and adequate fit was found in all models. Depression symptoms was a significant predictor of the log odds of reporting a higher proportion of habitual responses matching EBP components when controlling for gender (b = −0.46, p = .035); it was not a significant predictor when not controlling for gender (b = −0.40, p = .057). Gender was a significant predictor when controlling for depression symptoms (b = 0.78, p = .043); it was not a significant predictor when not controlling for gender (b = 0.68, p = .071). Because the Depression × Gender interaction was not significant, we did not include it in our final model. Figure 1a shows an odds ratio of less than 1 for depression symptoms in the final model, indicating that youths with higher levels of depression symptoms had greater odds of reporting a lower proportion of their habitual responses matching EBP components. Specifically, the fitted odds that a youth scoring at the 75th percentile on depression symptoms would report a lower proportion of habitual responses that match EBP components is 1.89 (inverse of OR, 0.53; 95% CI [0.29, 0.96]) times the fitted odds for a youth scoring at the 25th percentile,1 controlling for gender. In addition, an odds ratio of more than 1 for gender indicates that boys had greater odds than girls of reporting a higher proportion of habitual responses matching EBP components. The fitted odds of boys reporting a greater proportion of habitual responses matching EBP components was 2.18 (95% CI [1.02, 4.64]) times that of girls, controlling for depression symptoms. As predicted, youths with higher depression symptom levels were less likely to report habitual responses that matched EBP components. This association did not differ by gender, though boys were more likely than girls to report habitual responses matching EBP components,
Table 2.
Taxonomies of Nested Logistic Regression Models that Display the Fitted Relationship Between Youths’ Level of Depression Symptoms, Gender, and (a) the Proportion (All, Some, None) of Habitual Coping ResponsesMatching Evidence-Based Psychotherapy (EBP) Components (n = 104), (b) the Proportion of Habitual Coping Responses Matching Youths’ Identified Perceived-Effective Responses (n = 103), and (c) the Number (Three and At Least One) of Perceived-Effective Coping Responses Reported (n = 103)
| Models | |||||
|---|---|---|---|---|---|
| Parameter | M0 | MD | MG | MDG | MD×G |
| (a) Matching EBP Componentsa | |||||
| Intercept 2 | −0.05 | −0.35 | −0.41 | −0.39 | |
| Intercept 1 | 1.82*** | 1.51*** | 1.51*** | 1.53*** | |
| Depression Symptoms | −0.40† | −0.46* | −0.28 | ||
| Genderb | 0.68† | 0.78* | 0.79* | ||
| Depression Symptoms × Gender | −0.35 | ||||
| −2LL | 207.29 | 203.65 | 204.03 | 199.58 | 198.92 |
| NagelkerkeR2 | 0.000 | 0.040 | 0.036 | 0.083 | 0.090 |
| (b) Matching Youths’ Perceived-Effective Responsesa | |||||
| Intercept 2 | −1.53*** | −1.81*** | −1.88*** | −1.88*** | |
| Intercept 1 | 0.23 | −0.07 | −0.07 | −0.08 | |
| Depression Symptoms | −0.50* | −0.52* | −0.59† | ||
| Genderb | 0.63† | 0.68† | 0.68† | ||
| Depression Symptoms × Gender | 0.14 | ||||
| −2LL | 214.17 | 208.81 | 211.32 | 205.62 | 205.52 |
| NagelkerkeR2 | 0.000 | 0.058 | 0.031 | 0.091 | 0.092 |
| (c) No. of Perceived-Effective Responsesc | |||||
| Three Perceived-Effective Responses | |||||
| Intercept | 0.62** | 0.69* | 0.69* | 0.71* | |
| Depression Symptoms | −0.14 | −0.14 | −0.38 | ||
| Genderb | −0.15 | −0.14 | −0.16 | ||
| Depression Symptoms × Gender | 0.49 | ||||
| −2LL | 133.31 | 132.97 | 133.18 | 132.84 | 131.74 |
| NagelkerkeR2 | 0.000 | 0.005 | 0.002 | 0.006 | 0.021 |
| At Least One Perceived-Effective Response | |||||
| Intercept | 2.17*** | 1.75*** | 1.95*** | 1.92*** | |
| Depression Symptoms | −0.89** | −0.91** | −0.83† | ||
| Genderb | 0.43 | 0.52 | 0.62 | ||
| Depression Symptoms × Gender | −0.19 | ||||
| −2LL | 78.10 | 70.73 | 77.60 | 70.06 | 69.99 |
| NagelkerkeR2 | 0.000 | 0.130 | 0.009 | 0.141 | 0.143 |
Note. M0 = null model with no predictors; MD = model with depression symptoms as the only predictor; MG = model with gender as the only predictor; MDG = model with depression symptoms and gender as predictors; MD×G = model with depression symptoms, gender, and their interaction as predictors. Significance levels were based on the Wald test. Regression coefficients for the predictors with p< .10 are in shown in boldface.
The proportional odds assumption was met, thus three-level ordinal outcomes were used in analyses; the models predict youths reporting a higher proportion of habitual responses matching EBP components or perceived- effective responses.
Gender was coded as 0 for girls and 1 for boys.
The proportional odds assumption was not met, thus two binary outcomes were used.
p < .10;
p < .05;
p <.01,
p <.001.
Figure 1.
Youths with a higher depression score had greater odds of reporting (a) a lower proportion of habitual responses matching evidence-based psychotherapy (EBP) components, (b) a lower proportion of habitual responses perceived as effective, (c) zero perceived-effective response, and (d) a lower proportion of perceived-effective responses matching EBP component. Significance levels were based on the likelihood ratio (LR) test; df = 1 in all LR tests.
Test of hypothesis 2: Level of depression symptoms will be negatively associated with degree of match between youths’ habitual responses and their perceived-effective responses
Analyses bearing on hypothesis 2 included 103 youths (2 youths did not answer the relevant questions), of whom 18.4% reported All habitual responses, 36.9% reported Some, and 44.7% reported None matching their own perceived-effective responses. Table 2b shows the taxonomy of models that display the fitted relationship between youths’ depression symptoms, gender, and the proportion of habitual responses matching youths’ self-identified perceived-effective responses. The proportional odds and linearity assumptions were met and adequate fit was found in all models. Depression symptoms was a significant predictor of the log odds of reporting a higher proportion of habitual responses matching their perceived-effective responses (b = −0.50, p = .021); it remained significant when controlling for gender (b = −0.52, p = .017). Gender was not a significant predictor whether controlling for depression symptoms or not. Because the Depression × Gender interaction was not significant, we did not include it in our final model. In the final model (Figure 1b), the fitted odds that a youth scoring at the 75th percentile on depression symptoms would report a lower proportion of habitual responses that match EBP components is 2.05 (inverse of OR, 0.49; 95% CI [0.27, 0.90]) times the fitted odds for a youth scoring at the 25th percentile, controlling for gender. As predicted, youths with higher depression symptom levels were less likely to report habitual responses that matched their own perceived-effective responses; this association did not differ by gender.
Test of hypothesis 3: Level of depression symptoms will be negatively associated with ability to identify perceived-effective responses
Analyses involving perceived-effective responses included 103 youths (2 youths did not answer the relevant questions), of whom 65.0% reported three, 22.3% reported one/two, and 12.7% reported 0 perceived-effective responses. The proportional odds assumption was not met in the models with depression symptoms entered as a predictor; this indicates that the odd ratios across depression symptom levels differ significantly between reporting at least one and reporting three perceived-effective responses. We constructed two taxonomies of binary logistic regression models to test whether the odds of reporting three perceived-effective responses, and at least one perceived-effective response, differs significantly across depression symptom levels and gender (see Table 2c). The linearity assumption was met and adequate fit was found in all binary models. Depression symptoms was not a significant predictor when the outcome was three perceived-effective responses. However, depression symptoms was a significant predictor when the outcome was at least one perceived-effective response (b = −0.89, p = .007), and it remained significant when controlling for gender (b = −0.91, p = .006). Gender was not a significant predictor for either outcome. Because the Depression × Gender interaction was not significant for either outcome as well, we did not include it in the final models. In the final model (Figure 1c), the fitted odds that a youth scoring at the 75th percentile on depression symptoms would report no perceived-effective response is 3.51 (inverse of OR, 0.29; 95% CI [0.11, 0.72]) times the fitted odds for a youth scoring at the 25th percentile, controlling for gender. As predicted, youths with higher depression symptom levels were less able to identify perceived-effective responses; this association did not differ by gender.
Planned Analyses to Answer Research Questions Without Specific Predictions
Next, we examined whether depression symptoms were associated with (a) the extent to which youths’ perceived-effective responses matched any EBP component, and (b) the extent to which the youths’ habitual and perceived-effective responses matched specific EBP components. As noted previously, we also tested whether gender was a predictor of these two outcomes. In addition, we tested assumptions and checked model fit using the procedures described previously.
(a) Association of depression symptoms and gender with the proportion of perceived-effective responses matching EBP components
We computed the proportion of perceived-effective responses matching EBP components by dividing the number of perceived-effective responses matching EBP components by the total number of perceived-effective responses reported by each youth. Then we generated a three-level ordinal variable using the same approach used for the proportion coping variables computed for tests of hypotheses 1 and 2. Analyses involving perceived-effective responses included 103 youths (1 youth did not answer the relevant questions), of whom 70.9% reported All habitual responses, 16.5% reported Some, and 12.6% reported None matching EBP components. Interestingly, nearly all (92.6%) perceived-effective responses were coded as matching EBP components, and all youths who reported any perceived-effective response had at least some perceived-effective responses that resembled EBP components. We conducted ordinal logistic regression analysis with proportion of perceived-effective responses matching EBP components as the outcome, and depression symptoms and gender entered simultaneously as predictors. The proportional odds and linearity assumptions were met and adequate fit was found. Depression symptoms was a significant predictor of the log odds of reporting a higher proportion (all vs. some/none, and all/some vs. none) of perceived-effective responses matching EBP components (b = −0.66, p = .007), and it remained significant when controlling for gender (b = −0.66, p = .007). Gender was not a significant predictor. Figure 1d shows that the fitted odds that a youth scoring at the 75th percentile on depression symptoms would report a lower proportion of perceived-effective responses that match EBP components is 2.50 (inverse of OR, 0.40; 95% CI [0.21, 0.78]) times the fitted odds for a youth scoring at the 25th percentile, controlling for gender. Thus youths with higher depression symptom levels were less likely to report perceived-effective responses that matched EBP components, and this association did not differ by gender.
(b) Association of depression symptoms and gender with the proportion of coping responses matching specific EBP components
Because relatively few coping responses matched each specific EBP component, we did not compute the proportion of each youth’s habitual and perceived-effective responses matching each EBP component. Instead, we used binary outcomes—youth report of at least some (vs. none) of their coping responses matching each EBP component. Depression symptoms and gender were entered simultaneously as predictors. Analyses were not conducted for outcomes with low expected cell frequencies (i.e., under five)—namely, habitual responses and perceived-effective responses matching Relaxation and Practice or Perseverance, and perceived-effective responses matching Cognitive Restructuring. Depression symptom level was not a significant predictor for any EBP component, but gender was a highly significant predictor of youths’ habitual responses (b = −1.25, p = .012) and perceived-effective responses (b = −1.27, p = .004) matching Increasing Social Support, controlling for depression symptoms. The fitted odds of girls reporting at least some habitual responses (OR = 0.29, 95% CI [0.10, 0.80]) and at least some perceived-effective responses (OR = 0.28, 95% CI [0.11, 0.69] matching Increasing Social Support, were respectively 3.48 times and 3.55 times that of boys. Adequate fit was found for these two models. In other words, girls were more likely than boys to cope habitually by seeking support from others, and more likely to perceive this as an effective coping strategy.
Identifying Perceived-effective Responses that Did Not Match EBPs
Finally, we examined the perceived-effective responses that did not match EBP components for ideas that might suggest new directions for intervention. Of 244 perceived-effective responses provided, only 18 (7.4%) did not match EBP components. These 18 responses appear to fall under three broad clusters: (a) separating oneself physically or mentally from the stressor, (b) refraining from activity, and (c) noncommunicative expression of one’s feelings (see Table 1 for the types of coping responses that come under each broad cluster).
Discussion
We interviewed middle schoolers about coping strategies they used habitually and those they found effective. Their responses revealed significant areas of match and mismatch with youth depression EBPs. On the plus side, a large majority of perceived-effective responses matched EBP components. This suggests that most of the responses youths perceived as effective have been incorporated within the EBPs, and thus that there may be general agreement between youths and treatment developers on what works to improve mood. On the other hand, 13 of the 20 EBP components were not identified by a single youth as either habitual or perceived-effective. This suggests the possibility that not all of the components deemed important enough by treatment developers to be included within EBPs actually contribute to therapeutic benefit, and that a reduction in the array of skills taught could make current treatments more efficient, easier for youths to assimilate, and potentially more effective. Alternatively, the mismatch between youth responses and EBT components may indicate gaps in youth coping skills that, if addressed through therapy, could be beneficial to depressed youths. Dismantling research, testing the effects of separate EBP components, could help to clarify which of these interpretations is more valid.
As predicted, depression symptoms had a main effect on all three coping outcomes examined. Youths with more depression symptoms, compared to youths with fewer symptoms, were less likely to report using habitual responses that matched EBP components, and to report using habitual responses that matched even their own perceived-effective responses. That is, the higher the symptom level, the less likely youths were to use not only strategies identified by treatment researchers but also the strategies they themselves identified as perceived-effective. This suggests that youths with elevated depression symptoms may know of some useful strategies but fail to use the strategies frequently or successfully. This is consistent with research indicating that depressed adults have difficulty implementing strategies that are effective for nondepressed adults (see Joormann & D’Avanzato, 2010). Our analysis of responses perceived as effective showed an even more striking pattern: The odds of reporting no perceived-effective response was 3.5 times greater for the average high-symptom youth than for the average low-symptom youth in our sample. In other words, the higher the youths’ symptom level, the less likely they were to perceive any coping response as effective.
Boys were much more likely than girls to have habitual responses that matched EBP components. To understand this gender effect, we examined boys’ and girls’ habitual responses that did not match EBP components. Girls reported crying, experiencing a negative emotion (e.g., anger, annoyance), being alone, and going to their rooms more than boys; this contributed to girls having a lower proportion of habitual responses matching EBP components. This fits research showing that girls are more likely to cope with stressful situations by focusing on their own distress (not an EBP component), whereas boys have a greater tendency to distract themselves from their distress and engage in activities (EBP components; Broderick, 1998; Nolen-Hoeksema, 2012). In addition, girls were much more likely to report habitual and perceived-effective responses matching Increasing Social Support. Evidence indicates that girls and women identify more strongly with their interpersonal roles than do boys and men, and are more emotionally impacted by others’ experiences; however, research has focused on how this increases girls’ and women’s vulnerability to depression via increased interpersonal stress and co-rumination (Nolen-Hoeksema, 2012; Nolen-Hoeksema & Hilt, 2009). Our finding that girls habitually seek social support and find it an effective strategy suggests that this interpersonal orientation might facilitate their use of relationships as resources for improving their mood.
Finally, a modest percentage of the perceived-effective responses youths identified did not match EBP components. Some of these responses involved separating oneself from stressors or avoiding activity. These responses might be viewed as disengagement coping, which has been associated with higher depression levels (Connor-Smith et al., 2000). On the other hand, these responses may be adaptive if they limit youths’ exposure to stress or involve suppressing their sad thoughts indirectly. Evidence indicates that indirect approaches such as focused distraction, thought postponement, or nonjudgmental awareness of the thought (as in acceptance- and mindfulness-based therapies) are superior to direct suppression (Wegner, 2011). In fact, separating self from the stressor resembles a couples therapy approach in which partners take a “time-out” from each other in order to care for themselves—an approach designed to increase acceptance of partners’ negative behavior (Christensen & Jacobson, 1998). Among the responses involving noncommunicative expression of feelings, written disclosure may be a promising coping strategy to incorporate into current EBPs. In two RCTs, adolescents randomly assigned to write about intense emotional experiences weekly or fortnightly reported greater decreases in depression symptoms (Stice, Burton, Bearman, & Rohde, 2006), in negative affect, and in days absent from school (Horn, Pössel, & Hautzinger, 2011) compared to no-intervention controls.
Limitations and Strengths
One limitation of the study is its cross-sectional design, which could not test causal models. We could not determine, for example, whether depression symptoms made it difficult for the youths to generate or use coping strategies they or treatment developers deemed effective, or the youths’ lack of perceived-effective strategies led to their depression symptoms, or both. We also could not discern why, if youths with higher levels of depression symptoms could identify perceived-effective coping responses, they still experienced depression symptoms. Were they not using perceived-effective coping responses as often as other youths, or perhaps not implementing them as successfully? Future research may address such questions, and the additional questions of whether youths’ coping responses varied as a function of the severity of the youths’ stressors, or of the youths’ stress levels in response to the stressors.
Another limitation is that the coping interview relies on retrospective self-report, which can be influenced by memory limitations (Compas et al., 2001). It is not possible to verify that what youths report doing is actually what they usually do. It is possible that high-symptom youths may be susceptible to memory biases for negative information (see Gotlib & Joormann, 2010), which could account for difficulty in identifying perceived-effective responses. We conducted supplemental analyses to explore this possibility and did not find evidence that memory bias was driving the finding that high-symptom youths had greater odds of identifying no perceived-effective responses (see Appendix).2 Note, however, that regardless of whether high-symptom youths lacked perceived-effective coping responses, or had difficulty recalling strategies previously perceived as effective, the clinical implications would be similar; in both cases, the youths would be unlikely to use strategies that could repair their mood when they are feeling sad.
Other limitations can be noted briefly. Our use of a subsample of youths for this study may have limited our power to detect significant associations between variables, especially interactions. When youths responded that they had not figured out things they could do to make themselves feel better, we accepted their answer. We did not press further by asking, again, what they could do to feel better, in part because doing so might have suggested that we didn’t believe them, and in part because we thought answers given in response to interviewer pressure might not have been valid. However, it is possible that such interviewer pressure might have yielded more responses.
A strength of the coping interview is the open-ended nature of the questions, which avoids the risk of constraining youths’ responses; we did not assume that youths would report responses that fit neatly into EBP components or coping categories, and this approach generated a different picture of what youths considered helpful than what the EBPs might have suggested. Although unconstrained responses may lack the pre-structured framework of a standard questionnaire, we created standardized coding rules that generated high interrater reliability.
Clinical Implications
Our findings are consistent with the current focus of EBPs on teaching adaptive coping. The great majority of youths’ perceived-effective responses matched EBP components, suggesting that the EBPs capture most of what youths find helpful. Consistent with this idea, more symptomatic youths were less likely to use those EBP component-like strategies habitually. That said, our findings were also notable for the large number of EBP components (13 of 20) that were not identified by a single youth in our sample; this suggests the possibility of excess baggage in some treatments. Given the high percentage of youths who fail to complete the typically-lengthy standard EBP protocols (see, e.g., Weisz & Kazdin, 2010) and the finding that shorter depression prevention programs have larger effects than longer ones (Stice et al., 2009), there may be value in efforts to identify EBP components that contribute little and might thus be reduced or eliminated—leading to more streamlined and efficient treatment. Second, it may be fruitful for EBP therapists not only to teach youths new coping strategies, but also to help them identify effective strategies that are already in their repertoire and find ways to bolster the use of those strategies when depression symptoms surface. Third, some youths may need help in identifying at least one effective coping response, and practicing it until they can implement it successfully, as higher depression symptoms were associated with lower odds of identifying even one response they found effective. Fourth, girls may benefit from coaching in how to seek social support appropriately, as girls in our sample were more likely than boys to use this coping strategy habitually and to perceive it as effective. Finally, written disclosure of emotions may be considered for further testing in RCTs and, possibly, for inclusion in youth depression interventions.
More broadly, our findings suggest that there may be value in soliciting youth perspectives, as a complement to the adult perspectives (e.g., from theorists, researchers, and clinicians) that have most often shaped the development of youth interventions. Learning what youths perceive as effective based on their own life experience may help generate hypotheses about ways to streamline and strengthen interventions that are designed to help them.
Supplementary Material
Acknowledgments
This study was supported by grants from the National Institute of Mental Health (MH068806) and the Norlien Foundation awarded to John R. Weisz; the Harvard University Stimson Memorial Fund for Research awarded to Mei Yi Ng; and a grant from the National Institute of Mental Health (K23MH093491) awarded to Dikla Eckshtain. We are grateful to Angie Morssal, Heather Phipps, Carin Eisenstein, Kristen Jones, and other research assistants for their valuable help with this study, and to the children, families and schools who have participated in and supported our research. John R. Weisz receives royalties for some of the published work cited in this paper.
Footnotes
Although it is more common to base odds ratios on an increase of a one unit or one standard deviation in a continuous predictor, we based our odds ratios on an increase of an interquartile range in depression symptoms because it is more meaningful to compare the average high-symptom youth (scoring at the 75th percentile) to the average low-symptom youth (scoring at the 25th percentile), than to compare two youths who are one unit or one standard deviation apart in depression symptoms (see Babyak, 2009).
We thank an anonymous reviewer for suggesting these analyses.
Otherwise, none of the authors reports any conflict of interest.
Contributor Information
Mei Yi Ng, Harvard University.
Dikla Eckshtain, Massachusetts General Hospital and Harvard Medical School.
John R. Weisz, Harvard University
References
- Achenbach TM, Dumenci L, Rescorla LA. DSM-oriented and empirically based approaches to constructing scales from the same item pools. Journal of Clinical Child and Adolescent Psychology. 2003;32:328–340. doi: 10.1207/S15374424JCCP3203_02. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Center for Children, Youth and Families; 2001. [Google Scholar]
- Agresti A. An introduction to categorical data analysis. 2nd ed. Hoboken, NJ: Wiley & Sons.; 2007. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders—fourth edition, text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Babyak MA. Rescaling continuous predictors in regression models. Statistical tips from the editors of Psychosomatic Medicine [Web log post] 2009 Sep 24; Retrieved from http://stattips.blogspot.com/2009/08/rescaling-continuous-predictors-in.html.
- Bearman SK, Weisz JR. Primary and secondary control enhancement training (PASCET): Applying the deployment-focused model of treatment development and testing. In: Essau CA, editor. Treatments for adolescent depression: Theory and practice. New York, NY: Oxford University Press; 2009. pp. 97–121. [Google Scholar]
- Bender R, Grouven U. Ordinal logistic regression in medical research. Journal of the Royal College of Physicians of London. 1997;31:546–551. [PMC free article] [PubMed] [Google Scholar]
- Broderick PC. Early adolescent gender differences in the use of ruminative and distracting coping strategies. The Journal of Early Adolescence. 1998;18:173–191. [Google Scholar]
- Christensen A, Jacobson NS. Acceptance and change in couple therapy: A therapist's guide to transforming relationships. New York: Norton; 1998. [Google Scholar]
- Clarke GN, Lewinsohn PM, Hops H. [Retrieved March 28, 2010];Adolescent coping with depression course. 1990 from http://www.kpchr.org/acwd/acwd.html. [Google Scholar]
- Compas BE, Connor-Smith J, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127:87–127. [PubMed] [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68:976–992. [PubMed] [Google Scholar]
- Costello EJ, Pine DS, Hammen C, March JS, Plotsky PM, Weissman MM, Leckman JF. Development and natural history of mood disorder. Biological Psychiatry. 2002;52:529–542. doi: 10.1016/s0006-3223(02)01372-0. [DOI] [PubMed] [Google Scholar]
- David-Ferdon C, Kaslow NJ. Evidence-based psychosocial treatments for child and adolescent depression. Journal of Clinical Child and Adolescent Psychology. 2008;37:62–104. doi: 10.1080/15374410701817865. [DOI] [PubMed] [Google Scholar]
- Ge X, Lorenz FO, Conger RD, Elder GH, Jr, Simons RL. Trajectories of stressful life events and depressive symptoms during adolescence. Developmental Psychology. 1994;30:467–483. [Google Scholar]
- Gotlib IH, Joormann J. Cognition and depression: Current status and future directions. Annual Review of Clinical Psychology. 2010;6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetrick SE, McKenzie JE, Cox GR, Simmons MB, Merry SN. Newer generation antidepressants for depressive disorders in children and adolescents. Cochrane Database of Systematic Reviews, Issue. 2012;11 doi: 10.1002/14651858.CD004851.pub3. Art. No.: CD004851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn AB, Pössel P, Hautzinger M. Promoting adaptive emotion regulation and coping in adolescence: A school-based prevention programme. Journal of Health Psychology. 2011;16:258–273. doi: 10.1177/1359105310372814. [DOI] [PubMed] [Google Scholar]
- Hosmer D, Lemeshow S. Applied logistic regression. 2nd ed. New York, NY: John Wiley & Sons.; 2000. [Google Scholar]
- Joormann J, D’Avanzato C. Emotion regulation in depression: Examining the role of cognitive processes. Cognition and Emotion. 2010;24:913–939. [Google Scholar]
- Kahn J, Kehle T, Jenson W, Clark E. Comparison of cognitive-behavioral, relaxation, and self-modeling interventions for depression among middle-school students. School Psychology Review. 1990;19:196–211. [Google Scholar]
- Kovacs M. Children’s Depression Inventory (CDI): Technical manual update. North Tonawanda, NY: Multi-Health Systems; 2003. [Google Scholar]
- McGraw KO, Wong SP. A common language effect size statistic. Psychological Bulletin. 1992;111:361–365. [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merry SN, Hetrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, McDowell H. Psychological and educational interventions for preventing depression in children and adolescents. Cochrane Database of Systematic Reviews. 2011;2011(12) doi: 10.1002/14651858.CD003380.pub3. Art. No.: CD003380. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Emotion regulation and psychopathology: The role of gender. Annual Review of Clinical Psychology. 2012;8:161–187. doi: 10.1146/annurev-clinpsy-032511-143109. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Hilt LM. Gender differences in depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression in adolescents. New York, NY: Guilford; 2009. pp. 386–404. [Google Scholar]
- Rice F, Lifford KJ, Thomas HV, Thapar A. Mental health and functional outcomes of maternal and adolescent reports of adolescent depressive symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1162–1170. doi: 10.1097/chi.0b013e3180cc255f. [DOI] [PubMed] [Google Scholar]
- Rothbaum F, Weisz JR, Snyder SS. Changing the world and changing the self: A two-process model of perceived control. Journal of Personality and Social Psychology. 1982;42:5–37. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Silk JS, Vanderbilt-Adriance E, Shaw DS, Forbes EE, Whalen DJ, Ryan ND, Dahl RE. Resilience among children and adolescents at risk for depression: Mediation and moderation across social and neurobiological context. Development and Psychopathology. 2007;19:841–865. doi: 10.1017/S0954579407000417. [DOI] [PubMed] [Google Scholar]
- Stice E, Burton E, Bearman SK, Rohde P. Randomized trial of a brief depression prevention program: An elusive search for a psychosocial placebo control condition. Behaviour Research and Therapy. 2006;45:863–876. doi: 10.1016/j.brat.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice S, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegner DM. Setting free the bears: Escape from thought suppression. American Psychologist. 2011;66:671–680. doi: 10.1037/a0024985. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolescents. 2nd ed. New York, NY: Guilford Press; 2010. [Google Scholar]
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. The Global Burden of Disease: 2004 Update. Geneva, Switzerland: World Health Organization Press; 2008. [Google Scholar]
- Young JF, Mufson L, Davies M. Efficacy of Interpersonal Psychotherapy Adolescents Skills Training: An indicated preventive intervention for depression. Journal of Child Psychology and Psychiatry. 2006;47:1254–1262. doi: 10.1111/j.1469-7610.2006.01667.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.