Abstract
Objective
To examine individual and interpersonal processes of coping and emotional distress in a sample of mothers and fathers of children with recently diagnosed cancer.
Method
A sample of 317 mothers and 166 fathers of 334 children were recruited near the time of the child’s cancer diagnosis or relapse (M = 1.4 months, SD = 1.2). Mothers and fathers completed standardized measures of coping and depressive symptoms.
Results
Analyses of individual coping responses revealed that, for both mothers and fathers, primary control coping (e.g., problem solving, emotional modulation) and secondary control coping (e.g., acceptance, cognitive reappraisal) were associated with lower depressive symptoms. Interpersonal analyses of coping and distress indicated that mothers’ and fathers’ coping as well as depressive symptoms were significantly correlated. Actor–partner interdependence model analyses indicated that mothers’ coping was associated with fathers’ depressive symptoms. Significant interactions also suggested that mothers’ secondary control coping may have a compensatory effect against fathers’ use of disengagement coping, both for themselves and their husbands.
Conclusion
Mothers’ and fathers’ adaptation to a child’s cancer diagnosis and treatment are characterized by both individual and interpersonal processes, with secondary control coping playing a central role in both of these processes. Implications for interventions to enhance effective coping for parents of children with cancer are highlighted.
Keywords: parents, child cancer, coping, emotional distress
The diagnosis and treatment of cancer in a child are significant sources of stress for mothers and fathers, affecting the parents of over 12,000 children in the U.S. annually (Jemal, Siegel, Xu, & Ward, 2010). Parents are faced with a range of different stressors, with the greatest threat being the potential death of their child. This high level of stress can be associated with acute and prolonged symptoms of emotional distress, including depressive symptoms, in a subgroup of parents (Kazak, Boeving, Alderfer, Hwang, & Reilly, 2005; Pai et al., 2007). Therefore, it is important to understand the ways that parents cope with a child’s cancer in order to inform interventions that may facilitate more adaptive coping for these parents This includes possible interpersonal processes of coping and adjustment by which there may be bidirectional effects of distress and coping strategies between partners within a couple.
Parents of children with cancer encounter multiple sources of stress, including the emotional challenges of caring for their child, disruptions in daily routines, financial challenges due to income loss and medical expenses, and challenges communicating with medical professionals and their child about complex aspects of the disease and treatment (Rodriguez et al., 2012). Research has indicated that although many parents do not report significant levels of distress, a significant subgroup of parents may be at risk for emotional distress, including depressive symptoms (e.g., Iobst et al., 2009; Kazak et al., 2005; Norberg, Lindblad, & Boman, 2005). Although studies generally have shown a decline in parents’ depressive symptoms and other forms of emotional distress over several years following a child’s cancer diagnosis, mean levels of distress are significantly higher than normative levels near the time of diagnosis (Maurice-Stam, Oort, Last, & Grootenhuis, 2008; Pai et al., 2007).
Given the variability in levels of depressive symptoms and other forms of emotional distress among parents of children with cancer, it is important to identify patterns of coping that may be associated with higher versus lower levels of symptoms and distress. Researchers have examined the relationships between coping and parental distress among parents of pediatric cancer patients (e.g., Maurice-Stam et al., 2008; Bennett Murphy, Flowers, McNamara, & Young-Saleme, 2008; Norberg et al., 2005). However, it is difficult to synthesize findings because of heterogeneity in measures of coping, types of coping strategies assessed, time since the child’s diagnosis, and sample characteristics. A review by Clarke, McCarthy, Downie, Ashley, and Anderson (2009) noted that eight studies of parents coping with a child’s cancer all used different measures and different subtypes of coping, mirroring problems in the field of research on coping in general (Skinner, Edge, Altman, & Sherwood, 2003).
The majority of studies of parents’ coping with their child’s cancer have not examined the association of coping and emotional distress between partners. Although some studies (e.g., Bennett Murphy et al., 2008; Patistea, 2005) have compared the ways that mothers and fathers cope with a child’s cancer, these studies analyzed mean-level differences between mothers and fathers rather than associations between coping and partners’ emotional distress for mothers and fathers. Two studies that reported analyses of couples (Dahlquist et al., 1993; Hoekstra-Weebers, Jaspers, Kamps, & Klip, 1998) found that parents’ discrepant use of coping strategies may be related to their distress, but the association between coping and partners’ depressive symptoms is still unclear.
It is plausible that partners’ coping may have either interference or compensatory effects on one another’s emotional distress (Aldao & Nolen-Hoeksema, 2012). Drawing on dyadic models of coping (e.g., Berg & Upchurch, 2007), interference effects may occur when one partner’s use of maladaptive coping strategies undermines the effects of the other partner’s use of potentially beneficial coping strategies for themselves and their partner (Kraemer, Stanton, Meyerowitz, Rowland, & Ganz, 2011). In contrast, compensatory effects may be reflected when one’s own, or a partner’s, use of potentially beneficial types of coping serves as a buffer against personal or one’s partner’s use of maladaptive types of coping.
The current study was guided by a control-based model of coping with stress in which the level of actual and perceived controllability of illness-related stress is central for understanding the ways that children and their parents cope with chronic illness (Compas, Jaser, Dunn, & Rodriguez, 2012). Drawing on Weisz and colleagues’ model of perceived control (Rudolph, Dennig, & Weisz, 1995; Weisz, McCabe, & Dennig, 1994), three types of coping can be distinguished: primary control coping, secondary control coping, and disengagement coping (Compas, Connor-Smith, Saltzman, Thomsen, & Wadsworth, 2001; Compas et al., 2012). Primary control coping includes strategies intended to directly change the source of stress (e.g., problem solving) or one’s emotional reactions to the stressor (e.g., emotional expression, emotional modulation). Secondary control coping encompasses efforts to adapt to stress, including cognitive reappraisal, positive thinking, acceptance, and distraction. Disengagement coping includes efforts to orient away from the source of stress or one’s reactions to it (e.g., avoidance, denial, wishful thinking). Secondary control coping has been found to be most adaptive for coping with uncontrollable stress, whereas primary control is better suited for controllable stressors (Compas et al., 2012). These three factors of coping, as measured by the Responses to Stress Questionnaire (RSQ; Connor-Smith, Compas, Wadsworth, Thomsen, & Saltzman, 2000), have been supported by confirmatory factor analyses with adult samples of women coping with breast cancer (Compas et al., 2006) and parents coping with economic stress (Wadsworth, Raviv, Compas, & Connor-Smith, 2005). This control-based model may be particularly suited to understanding coping in parents of children with cancer because they face stressors that vary considerably in their degree of controllability.
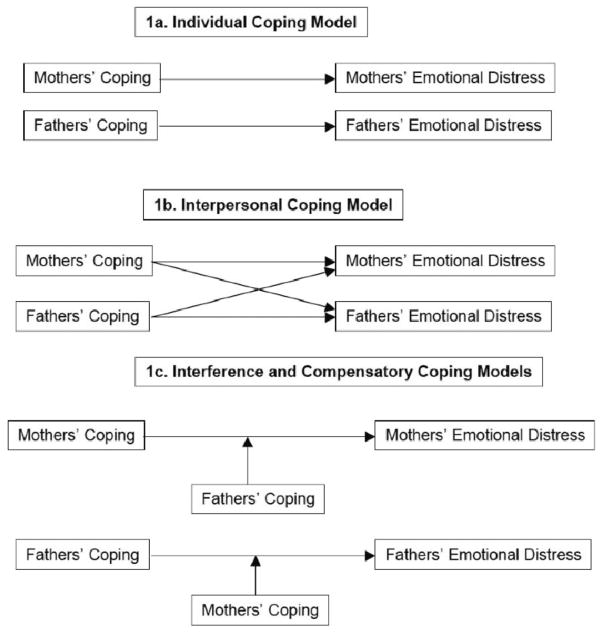
Applying this model in a sample of parents within the initial months after their child’s cancer diagnosis, we examined the association between coping and emotional distress in individual and interpersonal analyses (see Figure 1). First, we hypothesized that, at the individual level for mothers and fathers, primary and secondary control would be associated with lower depressive symptoms, whereas disengagement coping would be related to higher levels of symptoms (see Figure 1a). Second, we hypothesized that there would be moderate concordance within dyads for both coping strategies and levels of depressive symptoms. Third, we hypothesized that mothers’ and fathers’ coping would be significantly related to their spouses’ depressive symptoms. Specifically, we expected that primary and secondary control coping in one parent would be related to lower distress for their partner, while disengagement coping would be associated with higher partner depressive symptoms (see Figure 1b). Finally, we conducted exploratory analyses of potential interpersonal interference effects of disengagement coping and potential compensatory effects of secondary control coping in relation to a partner’s use of disengagement coping by testing the interactions of secondary control and disengagement coping between mothers and fathers (see Figure 1c). We chose secondary control coping because it may be especially well-suited to coping with uncontrollable aspects of a child’s cancer diagnosis and treatment, whereas disengagement coping has been associated with greater depressive symptoms.
Figure 1.
Hypothesized models of individual, interpersonal, interference, and compensatory relations of coping and emotional distress for mothers and fathers.
Method
Participants
Participants were 317 mothers and 166 fathers of 334 children with cancer. All participants were included in the individual analyses of mothers’ and fathers’ coping and distress. Within this group of mothers and fathers, there were 151 couples (i.e., data were available from both mother and father), and these couples were included in the interpersonal analyses of coping and distress. Participants were recruited from pediatric cancer registries at two hospitals in the Midwestern and Southern United States. Eligibility criteria included mothers and fathers whose child (a) was age 5–17 years old; (b) had a new cancer diagnosis or relapse/recurrence of cancer within the previous 2 months; (c) was actively receiving treatment through the oncology division; and (d) had no preexisting developmental disability.
Families of children with new diagnoses comprised 89% (n = 297) of the sample (see Table 1); there were no significant differences in enrollment based on the child’s first-time diagnosis versus relapse status. Mean age was 37.5 years for mothers and 39.5 years for fathers; participants’ children were on average 10.5 years old (SD = 3.9). Mean level of education was 16.0 years for both mothers and fathers. The majority of the sample was White (84.9% of mothers and 89.8% of fathers); 9.8% of mothers and 7.2% of fathers were African American, and the remainder of parents were from other racial groups. Annual family income ranged from less than $25,000 to more than $100,000. Seventy-five percent of participating mothers and 93% of participating fathers were currently married. The specific relationship to the child with cancer included biological parents (96.2% mothers and 85.6% fathers), step-parents (1.6% step-mothers and 10.4% step-fathers), or adoptive parents (2.2% mothers and 4% fathers). Same-sex couples were eligible for participation, however, all participating dyads were heterosexual couples.
Table 1.
Mothers’ and Fathers’ Demographic Characteristics, Psychological Distress, and Coping
| Variables | Mothers (N = 317)
|
Fathers (N = 166)
|
||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age (years) | 37.5 | 7.1 | 39.5 | 7.7 |
| Years of education | 13.9 | 2.2 | 14.1 | 2.6 |
|
| ||||
|
n
|
%
|
n
|
%
|
|
| Racea | ||||
| White | 269 | 84.9 | 149 | 89.8 |
| African American | 31 | 9.8 | 12 | 7.2 |
| Asian American | 3 | 0.9 | 1 | 0.6 |
| American Indian/Native Alaskan | 1 | 0.3 | 0 | 0 |
| Other | 12 | 3.8 | 4 | 2.4 |
| Annual family incomeb | ||||
| ≤ $25,000 | 87 | 28.2 | 34 | 20.5 |
| $25,001–$50,000 | 88 | 28.6 | 41 | 24.7 |
| $50,001–$75,000 | 48 | 15.6 | 35 | 21.1 |
| $75,001–$100,000 | 36 | 11.7 | 25 | 15.1 |
| ≥ $100,000 | 49 | 15.9 | 31 | 18.7 |
| Marital statusc | ||||
| Married/living with someone | 237 | 75.2 | 154 | 92.8 |
| Single, divorced, separated, or widowed | 78 | 24.7 | 12 | 7.2 |
|
| ||||
|
M
|
SD
|
M
|
SD
|
|
| Psychological distress | ||||
| BDI-II coping | 15.2 | 10.5 | 11.0 | 9.3 |
| Primary control | .20 | .04 | .19 | .04 |
| Secondary control | .26 | .05 | .27 | .05 |
| Disengagement | .13 | .03 | .14 | .03 |
Note. BDI-II = Beck Depression Inventory–II.
Information on race was not provided by one participant.
Annual family income data were not available for nine families.
Information on marital status was not provided by 2 participants.
Some parents participated alone either because they were not currently in a romantic relationship or they had a current partner/significant other but their partner was unwilling or unable to participate. There were no significant differences between mothers and fathers who were part of a dyad or who were participating alone in the study with regard to time since their child’s diagnosis, fathers’ education, or mothers’ or fathers’ age or race. Mothers who were part of a dyad had significantly higher levels of education (M = 17.1 years) than mothers who participated alone (M = 15.4 years), t(310) = −3.8, p < .01. Mothers who had a partner who participated in the study (M = 13.2) were significantly lower in depressive symptoms on the Beck Depression Inventory–II (BDI-II) than those who did not have a partner (M = 16.4) who participated, t(305) = 2.59, p = .010. Similarly, fathers who had a partner who participated (M = 10.1) were lower on the BDI-II than those who did not have a participating partner (M = 13.8), t(150) = 2.14, p = .036.
Measures
Demographic and medical data
Parents provided data on age, race, ethnicity, years of education, annual family income, and marital status. Parents also gave permission for research staff to review the child’s medical records for information on diagnosis or relapse status.
Coping
Parents completed the Pediatric Cancer version of the RSQ (RSQ-PC; Connor-Smith et al., 2000; Miller et al., 2009; Rodriguez et al., 2012) that is designed to assess coping responses to stressors related to having a child with cancer. The RSQ includes 57 items on which participants indicate with a 4-point scale how they react to and how much they use various coping methods, ranging from 0 (not at all) to 4 (a lot), in response to 11 stressors related to their child’s cancer, including daily/role functioning (e.g., paying bills and family expenses), cancer communication (e.g., talking with my child about cancer), and cancer caregiving (e.g., seeing the effects of my child’s treatment).
Factor analyses of the RSQ have identified five factors: primary control engagement coping (e.g., problem solving, emotional expression, emotional modulation), secondary control engagement coping (e.g., cognitive restructuring, positive thinking, acceptance, distraction), and disengagement coping (e.g., avoidance, denial, wishful thinking); two additional scales that reflect involuntary stress responses were not used in the current analyses. The RSQ has been shown to have good psychometric properties with adults (Compas et al., 2006; Wadsworth et al., 2005). Internal consistencies (α) for the current sample for each of the factors of interest ranged from .75–.79 for mothers and from .74–.76 for fathers. Proportion scores were created by dividing the total score for each factor by the total score for the RSQ (Connor-Smith et al., 2000; Osowiecki & Compas, 1999) and were used in the current analyses to control for response bias (i.e., to control for “yea” saying in endorsing high levels of all forms of coping).
Depressive symptoms
Mothers’ and fathers’ depressive symptoms as assessed on the BDI-II (Steer, Ranieri, Beck, & Clark, 1993) were examined in the current study because (a) depressive symptoms have been the focus of previous studies of parents of children with cancer (see Pai et al., 2007, for a review), (b) the BDI-II provides cutoff scores for levels of elevated symptoms, and (c) depressive symptoms reflect one aspect of broader nonspecific emotional distress. The BDI-II is a well-standardized measure of depressive symptoms in nonpsychiatric samples and demonstrates good psychometric properties (Steer et al., 1993). The measure has 21 items on which participants rate symptoms using a 4-point scale ranging from 0 (no change/not at all) to 3 (substantial change/severely). Scores on the BDI-II can range from minimal (0–13) to mild (14–19), moderate (20–28), and severe (29–63; Beck, Steer, & Brown, 1996). Internal consistency reliabilities (α) in the current sample were .93 for both mothers and fathers.
Procedure
Parents at the two research sites were approached in outpatient hematology/oncology clinics or inpatient rooms by a member of the research team. Eighty-seven percent of families who were approached agreed to participate. On average, parents consented to participate in the study 1.4 months (SD = 1.2) after their child’s diagnosis or relapse, and returned questionnaires 2.4 months after their child’s diagnosis (SD = 2.1). Variation in the time at which parents were first approached by the research team occurred based on the timing of communication of the diagnosis from the medical team to the research team, parents’ availability to hear about the study, and parents’ needing time to consider the study before consenting. After providing informed consent during a visit to the hospital, parents were given questionnaire packets that they completed in the hospital, outpatient clinic, or home; they returned at a subsequent visit. When only one parent was present and another parent or caregiver was involved, consent forms and questionnaires were sent home for the other caregiver to consider. Initial contact was most often made with mothers, who were encouraged to describe the study to their husbands/partners; research assistants were available to speak with partners about the study and to enroll them in the study. Families were compensated $50 when at least one parent completed the measures. Institutional review boards at both sites approved the study protocol.
Statistical Analyses
Statistical analyses were conducted using SPSS (19th ed.) and Mplus (Version 7.11). Pearson correlations and linear multiple regression analyses were conducted separately for mothers and fathers to assess individual associations of coping with depressive symptoms. We examined potential covariates and found that maternal/paternal age, education, income, and race were associated with coping and/or depressive symptoms and were included as covariates in the regression analyses. Child diagnosis type and maternal/paternal ethnicity were also examined, but did not correlate with coping/depressive symptoms and therefore were not included in the regression analyses. Correlations were used to test bivariate interpersonal associations of coping and depressive symptoms between mothers and fathers. A series of actor–partner interdependence models (APIMs; Kenny, Kashy, & Cook, 2006) were fit using maximum likelihood path analysis. This approach accounts for nonindependence between members of a couple. We used a path modeling approach in which data from each member of a couple were treated as separate variables, in order to predict individuals’ depressive symptoms as a function of both their own coping (actor effect) and their partners’ coping (partner effect).
Interactions between secondary control coping and disengagement coping were also included in an APIM to examine possible interference and compensatory effects in the interpersonal analyses. All coping variables were centered by subtracting the sample mean from each individual score and both the centered variables and their products were included in the analyses. Post hoc probing was conducted for significant interactions to determine whether simple slopes differed significantly from zero, and predicted associations were plotted separately at high and low values (i.e., ± 1 SD) of the moderator (Aiken & West, 1991; Holmbeck, 2002). The individual regression analyses were based on subsample values of 302 mothers and 162 fathers; the interpersonal analyses are based on 150 mother–father dyads; APIM analyses were based on 108 dyads, due primarily to missingness on the covariates. Mothers’ and fathers’ age, level of education, race, and family income were included in all regression and APIM analyses. With a subsample of 108, we were able to detect bivariate correlations of .26 or greater (p < .05, β = .80), and the 95% confidence interval (CI) for R2 in regression analyses with n equal to 108 ranged from .049–.220.
Results
Descriptive Statistics
Mothers’ mean BDI-II score (M = 15.2, SD = 10.5) fell in the mild range (Beck et al., 1996) while fathers’ mean score was in the minimal range for depressive symptoms (M = 11.0, SD = 9.3); 29% of mothers and 13% of fathers reported moderate-to-severe levels of depressive symptoms (total scores ≥ 20). Mothers reported using significantly more primary control coping than fathers, t(466) = −2.48, p = .014, and fathers reported using significantly more disengagement coping than mothers, t(463) = 2.41, p = 016.
Individual Analyses
Individual correlations
Bivariate correlations of mothers’ and fathers’ coping and their own depressive symptoms are presented in Table 2. As hypothesized, mothers’ primary and secondary control coping were significantly associated with lower levels of depressive symptoms. Mother’s disengagement coping was significantly associated with greater levels of depressive symptoms. Correlations among fathers’ self-reports indicated a similar pattern, in which primary and secondary control coping were significantly and negatively associated with reports of depressive symptoms. Fathers’ disengagement coping was significantly and positively associated with depressive symptoms.
Table 2.
Individual and Interpersonal Correlations Among Mothers’ and Fathers’ Coping and Psychological Distress
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Mothers’ primary control coping | — | ||||||
| 2. Mothers’ secondary control coping | .35*** | — | |||||
| 3. Mothers’ disengagement coping | −.59*** | −.56*** | — | ||||
| 4. Mothers’ BDI-II | −.51*** | −.63*** | .39*** | — | |||
| 5. Fathers’ primary control coping | .31*** | .17** | −.19* | −.21* | — | ||
| 6. Fathers’ secondary control coping | .30*** | .31*** | −.26*** | −.31** | .31*** | — | |
| 7. Fathers’ disengagement coping | −.36*** | −.19* | .32*** | .24** | −.51*** | −.43*** | — |
| 8. Fathers’ BDI-II | −.17** | −.24** | .05 | .30** | −.47*** | −.64*** | .27*** |
Note. For individual correlations, n equals 311 mothers and n equals 165 fathers. For interpersonal correlations, n equals 151 mothers and n equals 151 fathers. Mean correlation of mothers’ coping and fathers’ distress was r equals .16. Mean correlation of fathers’ coping and mothers’ distress was r equals .19. BDI-II = Beck Depression Inventory–II.
p < .05.
p < .01.
p < .001.
Individual regression analyses
Linear multiple regression analyses were conducted to examine associations of all three types of coping entered together in models predicting depressive symptoms separately for mothers and fathers (see Table 3). In analyses of mothers’ coping, the model predicting mothers’ own depressive symptoms was significant (total model R2 = .51; p < .001); primary control, secondary control, and disengagement coping were all significant when entered together. A similar pattern was found for fathers’ coping predicting fathers’ own depressive symptoms. The overall model was significant (total model R2 = .52; p < .001), and primary control, secondary control, and disengagement coping were all significant when entered together. When the covariates were included in the models, the effects for primary and secondary control coping remained significant for mothers and fathers and disengagement was no longer significant.
Table 3.
Hierarchical Regression Coefficients for Individual Analyses: Predicting Mothers’ and Fathers’ Depressive Symptoms From Their Own Coping
| Predictor variable | Mothers’ BDI-II
|
Fathers’ BDI-II
|
||
|---|---|---|---|---|
| B (SE) | β | B (SE) | β | |
| Step 1 | ||||
| Primary control | −107.15 (13.23)*** | −.40 | −88.60 (14.82)*** | −.38 |
| Secondary control | −112.162 (9.47)*** | −.57 | −107.77 (10.89)*** | −.60 |
| Disengagement | −60.14 (21.65)** | −.16 | −67.48 (24.67)** | −.18 |
| Step 2 | ||||
| Primary control | −92.66 (15.75)*** | −.35 | −72.13 (18.13)*** | −.32 |
| Secondary control | −109.49 (10.80)*** | −.57 | −102.95 (13.95)*** | −.58 |
| Disengagement | −49.94 (25.69)† | −.13 | −38.85 (30.42) | −.11 |
| Age | −.03 (0.08) | −.02 | −.02 (.09) | −.02 |
| Education | −.01 (.01) | –−.05 | .08 (.19) | .04 |
| Family income | −.01 (.004) | −.08 | .001 (.01) | .01 |
| Race (1) | −2.10 (1.72) | −.06 | −3.71 (2.34) | −.11 |
| Race (2) | 1.78 (2.13) | −.04 | −6.02 (4.10) | −.10 |
Note. To analyze the effects of race, which is a nominal variable with more than two categories, we created two dummy codes in which Race (1) controlled for differences due to African American versus White and Race (2) controlled for differences due to Other races versus White. BDI-II = Beck Depression Inventory–II.
p = .052.
p < .05.
p < .01.
p < .001.
In light of the positive bivariate correlations between disengagement coping and depressive symptoms for mothers and fathers, the negative standardized slopes in the regression analyses indicated a possible suppressor effect. Analyses were conducted to probe this possible suppressor effect of primary and secondary control coping on the association between disengagement coping and depressive symptoms for mothers and fathers (MacKinnon, Krull, & Lockwood, 2000). The total indirect effect through the suppressors (i.e., the sum of the indirect effects of disengagement coping on depressive symptoms through each suppressor) was .54 for mothers, 95% CI [.48, .63], and .45 for fathers, 95% CI [.32, .59]. Thus, there is evidence that primary and secondary control coping act as suppressors in the association between disengagement coping and depressive symptoms. However, when the covariates were included, the effect for disengagement coping was no longer significant for fathers or mothers.
Interpersonal Analyses
Interpersonal correlations
Bivariate correlations of coping and depressive symptoms between mothers and fathers are presented in Table 2. Mothers’ and fathers’ use of primary control, secondary control, and disengagement coping strategies were significantly associated with their partners’ corresponding type of coping and mothers’ and fathers’ depressive symptoms were positively related. Correlations (r) ranged from .30–.32 (all medium in magnitude).
Correlational analyses of mothers’ and fathers’ coping with their partners’ levels of psychological distress are also presented in Table 2. All three of the correlations of fathers’ coping with mothers’ distress were significant. Specifically, fathers’ primary and secondary control coping were significantly and negatively correlated with mothers’ depressive symptoms, and fathers’ disengagement coping was significantly and positively related to mothers’ depressive symptoms. Mothers’ primary and secondary control coping negatively correlated with fathers’ depressive symptoms, whereas mothers’ reports of disengagement coping did not correlate with fathers’ depressive symptoms.
Interpersonal regression analyses
We examined the simple effects of mothers’ and fathers’ coping on their partners’ emotional distress (see Table 4). Because of the large number of possible combinations of mothers’ and fathers’ coping, we focused our interpersonal regression analyses on secondary control coping and disengagement coping because they showed the most consistent pattern of significant correlations in the individual and interpersonal correlations of mothers’ and fathers’ coping and distress. We tested an APIM model with mothers’ and fathers’ BDI-II scores as the dependent variables. In the first step of each equation, we examined the main effects of mothers’ and fathers’ own secondary control and disengagement coping and their partners’ secondary control disengagement coping; in the second step, family income and mothers’ and fathers’ age, race, and education were added (see Table 4). In the first step of the equation predicting mothers’ depressive symptoms, only mothers’ secondary control coping was a significant predictor. When the covariates were added to the equation, mothers’ secondary control coping remained the only significant predictor. In the second regression equation, we tested predictors of fathers’ depressive symptoms on BDI-II score. In the first step, fathers’ secondary control coping but not disengagement coping was a significant predictor, and mothers’ secondary control coping and disengagement coping were significant predictors of fathers’ depressive symptoms. When the covariates were added to the equation, fathers’ secondary control coping and mothers’ disengagement coping remained significant predictors of fathers’ depressive symptoms.
Table 4.
Hierarchical Regression Coefficients for Interpersonal Analyses: Predicting Mothers’ and Fathers’ Depressive Symptoms From Their Partner’s Coping While Controlling for Own Coping
| Predictor variable | Mothers’ BDI-II
|
Fathers’ BDI-II
|
||
|---|---|---|---|---|
| B (SE) | β | B (SE) | β | |
| Step 1 | ||||
| Mothers’ secondary control | −121.02 (13.44)*** | −.66 | −26.50 (13.36)* | −.15 |
| Mothers’ disengagement | −7.68 (25.24) | −.02 | −69.83 (25.18)** | −.21 |
| Fathers’ secondary control | −12.57 (12.45) | −.07 | −114.16 (12.38)*** | −.64 |
| Fathers’ disengagement | 37.93 (26.95) | .10 | 21.29 (26.65) | .06 |
| Step 2 | (R2 = .58***) | (R2 = .43***) | ||
| Mothers’ secondary control | −123.34 (15.02)*** | −.69 | −20.75 (15.14) | .17 |
| Mothers’ disengagement | −3.06 (29.00) | −.01 | −58.85 (29.12)* | .20 |
| Fathers’ secondary control | −4.00 (15.06) | −.02 | −107.29 (15.13)*** | −.63 |
| Fathers’ disengagement | 9.19 (30.50) | −.02 | −1.24 (30.61) | −.004 |
| Family income | .001 (.01) | .02 | −.001 (.01) | −.02 |
| Mothers’ age | .41 (.15)** | .28 | .05 (.15) | .04 |
| Mothers’ education | −.01 (.01) | −.04 | −.01 (.01) | −.10 |
| Mothers’ race (1) | 20.09 (7.12)** | .52 | 9.84 (7.15) | .30 |
| Mothers’ race (2) | −3.22 (3.79) | −.07 | −1.03 (3.88) | −.03 |
| Fathers’ age | −.34 (.13)* | −.26 | −.07 (.13) | −.06 |
| Fathers’ education | −.32 (.19) | −.13 | .01 (.20) | .003 |
| Fathers’ race (1) | −20.11 (6.74)** | −.55 | −11.07 (6.76) | −.35 |
| Fathers’ race (2) | 6.58 (4.54) | .02 | −1.17 (5.16) | −.02 |
Note. To analyze the effects of race, which is a nominal variable with more than two categories, we created two dummy codes in which Race (1) controlled for differences due to African American versus White and Race (2) controlled for differences due to Other races versus White. BDI-II = Beck Depression Inventory–II.
p < .05.
p < .01.
p < .001.
Interference and compensatory analyses
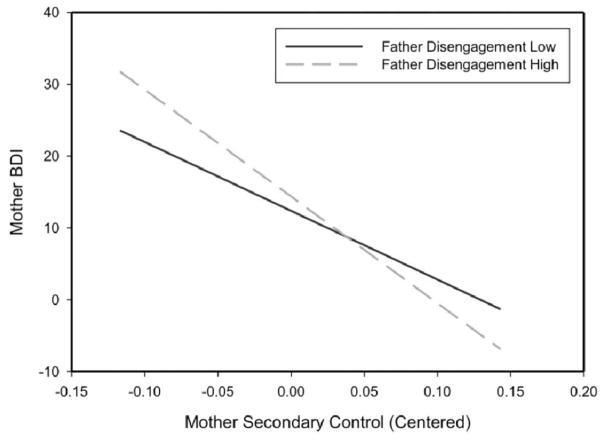
In a final set of APIM analyses, we examined possible interference and compensatory models of coping by including interactions for mothers’ or fathers’ secondary control coping with their partners’ disengagement coping and for mothers’ or fathers’ disengagement coping with their partners’ secondary control coping (see Table 5). In the first step of the equation predicting mothers’ depressive symptoms, mothers’ secondary control coping was significant and the interaction between mothers’ secondary control coping and fathers’ disengagement coping was also significant. We estimated the simple slope of mothers’ depressive symptoms regressed on mothers’ secondary control coping when fathers’ disengagement coping fell 1 SD above and 1 SD below the mean (see Figure 2). The association between mothers’ depressive symptoms and secondary control coping when fathers reported higher levels of disengagement coping was significant, and the association when fathers reported lower levels of disengagement coping was also significant. When the covariates were added to the equation predicting mothers’ depressive symptoms, only mothers’ secondary control coping remained significant, and the interaction between mothers’ secondary control coping and fathers’ disengagement coping was no longer significant.
Table 5.
Hierarchical Regression Coefficients for Interference/Compensatory Analyses: Predicting Mothers’ and Fathers’ Depressive Symptoms From the Interaction Between Their Own and Their Partners’ Coping
| Predictor variable | Mothers’ BDI-II
|
Fathers’ BDI-II
|
||
|---|---|---|---|---|
| B (SE) | β | B (SE) | β | |
| Step 1 | ||||
| Mothers’ secondary control | −122.190 (13.09)*** | −.66 | −27.36 (13.16)* | −.15 |
| Mothers’ disengagement | −9.90 (24.69) | −.03 | −65.96 (24.89)** | −.20 |
| Fathers’ secondary control | −14.33 (12.25) | −.08 | −111.23 (12.31)*** | −.62 |
| Fathers’ disengagement | 39.21 (26.24) | .10 | 21.36 (26.22) | .06 |
| Mothers’ secondary control × Fathers’ disengagement | −1043.71 (502.36)* | −.13 | −1037.66 (503.88)* | −.14 |
| Fathers’ secondary control × Mothers’ disengagement | −363.65 (436.16) | −.05 | 730.32 (438.55) | .11 |
| Step 2 | (R2 = .60***) | (R2 = .45***) | ||
| Mothers’ secondary control | −125.53 (14.85)*** | −.70 | −24.06 (14.99) | −.16 |
| Mothers’ disengagement | −4.40 (28.64) | −.01 | −63.21 (28.77)* | −.21 |
| Fathers’ secondary control | −4.27 (14.90) | −.02 | −105.50 (14.97)*** | −.62 |
| Fathers’ disengagement | 12.89 (30.07) | .03 | 1.37 (30.16) | .004 |
| Mothers’ secondary control × Fathers’ disengagement | −858.58 (587.70) | −.11 | −1137.86 (593.76)† | −.18 |
| Fathers’ secondary control × Mothers’ disengagement | −103.09 (598.00) | −.01 | 646.55 (606.93) | .10 |
| Family income | .002 (.01) | .02 | −.001 (.01) | −.02 |
| Mothers’ age | .38 (.15)* | .26 | .03 (.15) | .02 |
| Mothers’ education | −.003 (.01) | −.26 | −.01 (.01) | −.08 |
| Mothers’ race (1) | 18.24 (7.09)* | .47 | 8.99 (7.11) | .27 |
| Mothers’ race (2) | −3.40 (3.76) | −.07 | −1.83 (3.85) | −.07 |
| Fathers’ age | −.328 (.13)* | −.25 | −.08 (.13) | −.07 |
| Fathers’ education | −.27 (.16) | −.11 | .03 (.20) | .02 |
| Fathers’ race (1) | −18.93 (6.66)** | −.52 | −10.24 (6.78) | −.33 |
| Fathers’ race (2) | .002 (.01) | .10 | −1.87 (5.09) | −.03 |
Note. To analyze the effects of race, which is a nominal variable with more than two categories, we created two dummy codes in which Race (1) controlled for differences due to African American versus White and Race (2) controlled for differences due to Other races versus White. BDI-II = Beck Depression Inventory–II.
p = .055.
p < .05.
p < .01.
p < .001.
Figure 2.
Interaction of mothers’ secondary control coping and fathers’ disengagement coping as predictors of mothers’ depressive symptoms. BDI = Beck Depression Inventory–II.
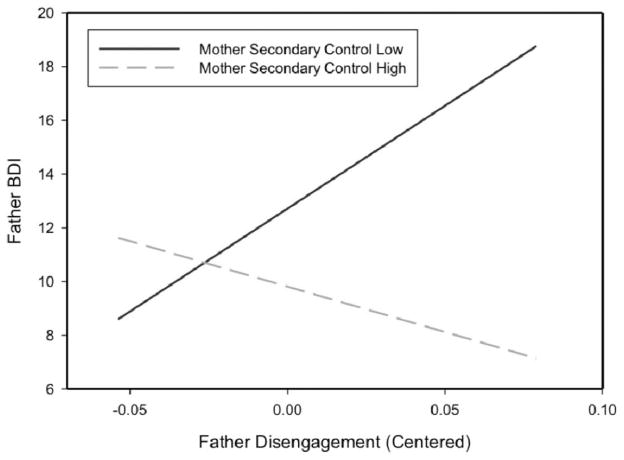
In the first step of the equation predicting fathers’ depressive symptoms, fathers’ secondary control coping and mothers’ secondary control and disengagement coping, and the interaction between fathers’ disengagement and mothers’ secondary control coping were all significant predictors. We estimated the simple slope of fathers’ depressive symptoms regressed on fathers’ disengagement coping when mothers’ secondary control coping fell 1 SD above and 1 SD below the mean (see Figure 3). The association between fathers’ distress and disengagement coping when mothers reported higher levels of secondary control coping strategies was not significant, but the association was significant when mothers reported lower levels of secondary control coping. When the covariates were added to the equation in the second step predicting fathers’ depressive symptoms, fathers’ secondary control coping and mothers disengagement coping remained significant and the interaction between fathers’ disengagement coping and mothers’ secondary control coping was no longer significant.
Figure 3.
Interaction of mothers’ secondary control coping and fathers’ disengagement coping as predictors of fathers’ depressive symptoms. BDI = Beck Depression Inventory–II.
Discussion
The current study examined both individual and interpersonal processes of coping in a sample of mothers and fathers of children with cancer soon after diagnosis. The findings provide evidence that primary and secondary control coping are associated with lower depressive symptoms for both mothers and fathers. Further, the findings provide new information about interpersonal processes of coping and distress between mothers and fathers. There are both main and interactive effects of mothers’ and fathers’ coping on one another’s distress, suggesting that parental coping can be best understood as both an individual and an interpersonal process.
At the individual level, mothers’ and fathers’ own use of primary control, secondary control, and disengagement coping were all significantly related to depressive symptoms. When entered together in the separate individual regression models for mothers and fathers that included all three types of coping, primary and secondary control and disengagement coping accounted for significant and unique variance in predicting depressive symptoms. The strong associations of both primary and secondary control coping with fewer depressive symptoms suggest that parents may be faced with both controllable and uncontrollable sources of stress related to their child’s cancer that are responsive to both of these types of coping. For example, parents are able to seek out information, discuss treatment options with medical staff, and take steps to help their families deal with stress, all of which lend themselves to primary control coping efforts. But parents also experience significant stress that is beyond their control, which requires more accommodative coping responses, such as reappraising the situation and accepting aspects of their child’s disease and treatment. It is noteworthy that the significant effects for disengagement coping in the individual regression models reflect suppressor effects. That is, for mothers and for fathers, disengagement coping correlated with higher levels of depressive symptoms in the correlations, but was related to lower depressive symptoms when included in the regression analyses along with primary and secondary control coping. This may suggest that disengagement coping may be associated with lower depressive symptoms when it is accompanied by the use of primary and secondary control coping, but this pattern warrants further attention in subsequent research. The findings for primary and secondary control coping remained significant even after controlling for several covariates (i.e., family income and parents’ age, education, and race), suggesting that these findings are relatively robust.
These findings are consistent with those of previous studies that have highlighted general patterns of coping strategies that are related to either positive or negative adjustment among parents of children with cancer. For example, studies have found lower emotional distress is associated with coping strategies that involve focusing on and engaging with the problem (e.g., Bennett Murphy et al., 2008; Norberg et al., 2005). There is some evidence that positive cognitive appraisal and optimism are also related to better adjustment among parents (e.g., Maurice-Stam et al., 2008). Conversely, prior findings indicated that various forms of avoidance and disengagement (e.g., denial, passivity) are associated with greater emotional distress (Greening & Stoppelbein, 2007; Maurice-Stam et al., 2008; Bennett Murphy et al., 2008). The role of disengagement coping in the context of the use of engagement forms of coping is in need of future research.
Although important, the analyses of the individual-level associations between coping and distress present only a partial picture of the process of adaptation to the stress of a child’s cancer for mothers and fathers. Consistent with dyadic models of coping (Berg & Upchurch, 2007), the current study provides evidence of the importance of interpersonal processes at several levels. Similar to findings from prior students (see Clarke et al., 2009, for a review), we found that mothers reported more primary control coping and fathers reported more disengagement coping. Further, the correlations between mothers’ and fathers’ reports of primary control, secondary control, and disengagement coping were all statistically significant (range: .31–.32), reflecting a medium effect size (Cohen, 1992). This pattern suggests that, intentionally or unintentionally, mothers and fathers may coordinate their coping efforts in beneficial ways. It is also noteworthy that mothers’ and fathers’ reports of primary and secondary control coping were significantly and negatively correlated with their partners’ use of disengagement coping (r range: −.19 to −.36). The significant positive correlations between partners’ reports of disengagement coping and their depressive symptoms suggest that some couples may be characterized by more maladaptive ways of coping and associated higher levels of distress.
Additionally, in the bivariate correlations, mothers’ depressive symptoms correlated significantly with all three types of fathers’ coping. Fathers’ depressive symptoms correlated with their partners’ use of primary control and secondary control coping, but not with mothers’ disengagement coping. Specifically, mothers’ and fathers’ use of secondary control coping correlated with lower distress for themselves and for their partners, whereas disengagement coping was related to more distress individually and interpersonally.
We further examined more complex interpersonal associations of coping and distress in a series of APIM analyses focused on mothers’ and fathers’ secondary control and disengagement coping. In general, mothers’ levels of depressive symptoms were not associated with fathers’ coping in the multivariate analyses, with the exception of an interaction between her use of secondary control coping and his use of disengagement coping. Specifically, mothers’ use of secondary control coping may reflect a compensatory effect by buffering them from their partners’ disengagement coping. That is, fathers’ disengagement coping was related to higher levels of mothers’ depressive symptoms for mothers who reported low levels of secondary control coping, but not for mothers who were high in secondary control coping. Mothers’ secondary control coping also appeared to serve a compensatory effect by buffering fathers from their own use of disengagement coping. That is, fathers’ disengagement coping correlated with higher depressive symptoms when their partners were low in secondary control coping, but did not correlate with their depressive symptoms when their partners were high in secondary control coping. However, these interactions were no longer significant when the covariates (i.e., family income, parents’ age, education, and race) were included, suggesting that these effects are qualified in relation to the whole sample of mothers and fathers in this study.
In general, more evidence was found for interpersonal effects of coping in analyses of fathers’ distress than for mothers’ distress. There was a significant association between mothers’ secondary control coping and fathers’ depressive symptoms even after accounting for fathers’ secondary control and disengagement coping, mothers’ disengagement coping, and their interactions. This suggests that fathers may experience a beneficial effect of mothers’ use of secondary control coping strategies including acceptance, cognitive reappraisal, positive thinking, and positive forms of distraction.
This study had several strengths that increase the potential significance of the findings. First, the study was guided by a clear conceptual model of coping and used well-validated measures of coping and depressive symptoms. Second, analyses were based on a large sample of mothers and fathers, including a large sample of couples. Third, the sample was relatively homogeneous with regard to time since their child’s diagnosis, providing an opportunity to gain a picture of coping and distress in mothers and fathers in the initial weeks and months after diagnosis and during treatment when levels of parents’ emotional distress may be relatively high. Fourth, high rates of recruitment and enrollment of parents were achieved at two sites.
The current study also had several weaknesses that need to be addressed in future research. Most importantly, the findings are all cross-sectional and need to be examined further in prospective longitudinal analyses that will provide a better test of the direction of the individual and interpersonal associations between coping and emotional distress. A second limitation is that the individual analyses of coping and distress are, like other studies, based on parents’ self-reports of both constructs. This creates a problem of shared method variance that may inflate the levels of association between coping and distress in the individual-level analyses. Third, parents’ coping with stressors related to their child’s cancer was assessed; however, the ways that parents may be coping with other sources of stress in their lives was not examined and these other coping efforts may have had an effect on parents’ depressive symptoms. Fourth, variations in relationship quality and status (beyond marital status) may be important to examine in future studies of parents of children with cancer. Fifth, the sample in the current study was somewhat homogeneous with regard to socioeconomic status, race, and ethnicity, and future research is needed with more diverse samples.
These limitations notwithstanding, the findings suggest some avenues for future research on interventions to enhance coping skills in parents of children with cancer. Interventions for parents of children with cancer have focused on teaching problem-solving skills that represent one type of primary control coping (e.g., Askins et al., 2009; Sahler et al., 2005). Problem-solving interventions have also included other skills (e.g., relaxation, reframing, distraction) that are similar to secondary control coping skills (Nezu, Nezu, & D’Zurilla, 2013). The current findings, if supported by longitudinal analyses, suggest that parents would benefit from interventions that strengthen a wide set of coping skills, including both primary control and, importantly, secondary control coping skills. Further, the current study suggests that, when possible, interventions might best target mothers and fathers together because there may be both individual and interpersonal benefits of enhancing parents’ use of secondary control coping skills.
Acknowledgments
Supported by the National Cancer Institute (Grant R01CA118332), a gift from Patricia and Rodes Hart, and The Research Institute at Nationwide Children’s Hospital (intramural funding).
Contributor Information
Bruce E. Compas, Vanderbilt University
Heather Bemis, Vanderbilt University.
Cynthia A. Gerhardt, Nationwide Children’s Hospital, Columbus, Ohio, and The Ohio State University
Madeleine J. Dunn, Vanderbilt University
Erin M. Rodriguez, Vanderbilt University
Leandra Desjardins, Vanderbilt University.
Kristopher J. Preacher, Vanderbilt University
Samantha Manring, Nationwide Children’s Hospital, Columbus, Ohio, and The Ohio State University.
Kathryn Vannatta, Nationwide Children’s Hospital, Columbus, Ohio, and The Ohio State University.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Aldao A, Nolen-Hoeksema S. When are adaptive strategies most predictive of psychopathology? Journal of Abnormal Psychology. 2012;121:276–281. doi: 10.1037/a0023598. http://dx.doi.org/10.1037/a0023598. [DOI] [PubMed] [Google Scholar]
- Askins MA, Sahler OJZ, Sherman SA, Fairclough DL, Butler RW, Katz ER, Phipps S. Report from a multi-institutional randomized clinical trial examining computer-assisted problem-solving skills training for English- and Spanish-speaking mothers of children with newly diagnosed cancer. Journal of Pediatric Psychology. 2009;34:551–563. doi: 10.1093/jpepsy/jsn124. http://dx.doi.org/10.1093/jpepsy/jsn124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory manual. 2. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Bennett Murphy LM, Flowers S, McNamara KA, Young-Saleme T. Fathers of children with cancer: Involvement, coping, and adjustment. Journal of Pediatric Health Care. 2008;22:182–189. doi: 10.1016/j.pedhc.2007.06.003. http://dx.doi.org/10.1016/j.pedhc.2007.06.003. [DOI] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. http://dx.doi.org/10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Clarke NE, McCarthy MC, Downie P, Ashley DM, Anderson VA. Gender differences in the psychosocial experience of parents of children with cancer: A review of the literature. Psycho-Oncology. 2009;18:907–915. doi: 10.1002/pon.1515. http://dx.doi.org/10.1002/pon.1515. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. http://dx.doi.org/10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Compas BE, Beckjord E, Agocha B, Sherman ML, Langrock A, Grossman CI, Luecken L. Measurement of coping and stress responses in women with breast cancer. Psycho-Oncology. 2006;15:1038–1054. doi: 10.1002/pon.999. http://dx.doi.org/10.1002/pon.999. [DOI] [PubMed] [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127:87–127. http://dx.doi.org/10.1037/0033-2909.127.1.87. [PubMed] [Google Scholar]
- Compas BE, Jaser SS, Dunn MJ, Rodriguez EM. Coping with chronic illness in childhood and adolescence. Annual Review of Clinical Psychology. 2012;8:455–480. doi: 10.1146/annurev-clinpsy-032511-143108. http://dx.doi.org/10.1146/annurev-clinpsy-032511-143108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68:976–992. http://dx.doi.org/10.1037/0022-006X.68.6.976. [PubMed] [Google Scholar]
- Dahlquist LM, Czyzewski DI, Copeland KG, Jones CL, Taub E, Vaughan JK. Parents of children newly diagnosed with cancer: Anxiety, coping, and marital distress. Journal of Pediatric Psychology. 1993;18:365–376. doi: 10.1093/jpepsy/18.3.365. http://dx.doi.org/10.1093/jpepsy/18.3.365. [DOI] [PubMed] [Google Scholar]
- Greening L, Stoppelbein L. Brief report: Pediatric cancer, parental coping style, and risk for depressive, posttraumatic stress, and anxiety symptoms. Journal of Pediatric Psychology. 2007;32:1272–1277. doi: 10.1093/jpepsy/jsm057. http://dx.doi.org/10.1093/jpepsy/jsm057. [DOI] [PubMed] [Google Scholar]
- Hoekstra-Weebers JE, Jaspers JPC, Kamps WA, Klip EC. Gender differences in psychological adaptation and coping in parents of pediatric cancer patients. Psycho-Oncology. 1998;7:26–36. doi: 10.1002/(SICI)1099-1611(199801/02)7:1<26::AID-PON315>3.0.CO;2-0. http://dx.doi.org/10.1002/(SICI)1099-1611(199801/02)7:1<26::AID-PON315>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. http://dx.doi.org/10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Iobst EA, Alderfer MA, Sahler OJZ, Askins MA, Fairclough DL, Katz ER, Noll RB. Problem solving and maternal distress at the time of a child’s diagnosis of cancer in two-parent versus lone-parent households. Journal of Pediatric Psychology. 2009;34:817–821. doi: 10.1093/jpepsy/jsn140. http://dx.doi.org/10.1093/jpepsy/jsn140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA: A Cancer Journal for Clinicians. 2010;60:277–300. doi: 10.3322/caac.20073. http://dx.doi.org/10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Boeving CA, Alderfer MA, Hwang WT, Reilly A. Posttraumatic stress symptoms during treatment in parents of children with cancer. Journal of Clinical Oncology. 2005;23:7405–7410. doi: 10.1200/JCO.2005.09.110. http://dx.doi.org/10.1200/JCO.2005.09.110. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York, NY: Guilford Press; 2006. [Google Scholar]
- Kraemer LM, Stanton AL, Meyerowitz BE, Rowland JH, Ganz PA. A longitudinal examination of couples’ coping strategies as predictors of adjustment to breast cancer. Journal of Family Psychology. 2011;25:963–972. doi: 10.1037/a0025551. http://dx.doi.org/10.1037/a0025551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding, and suppression effect. Prevention Science. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurice-Stam H, Oort FJ, Last BF, Grootenhuis MA. Emotional functioning of parents of children with cancer: The first five years of continuous remission after the end of treatment. Psycho-Oncology. 2008;17:448–459. doi: 10.1002/pon.1260. http://dx.doi.org/10.1002/pon.1260. [DOI] [PubMed] [Google Scholar]
- Miller KS, Vannatta K, Compas BE, Vasey M, McGoron KD, Salley CG, Gerhardt CA. The role of coping and temperament in the adjustment of children with cancer. Journal of Pediatric Psychology. 2009;34:1135–1143. doi: 10.1093/jpepsy/jsp037. http://dx.doi.org/10.1093/jpepsy/jsp037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nezu AM, Nezu CM, D’Zurilla TJ. Problem-solving therapy: A treatment manual. New York, NY: Springer; 2013. [Google Scholar]
- Norberg AL, Lindblad F, Boman KK. Coping strategies in parents of children with cancer. Social Science & Medicine. 2005;60:965–975. doi: 10.1016/j.socscimed.2004.06.030. http://dx.doi.org/10.1016/j.socscimed.2004.06.030. [DOI] [PubMed] [Google Scholar]
- Osowiecki DM, Compas BE. A prospective study of coping, perceived control and psychological adjustment to breast cancer. Cognitive Therapy and Research. 1999;23:169–180. http://dx.doi.org/10.1023/A:1018779228432. [Google Scholar]
- Pai ALH, Greenley RN, Lewandowski A, Drotar D, Youngstrom E, Peterson CC. A meta-analytic review of the influence of pediatric cancer on parent and family functioning. Journal of Family Psychology. 2007;21:407– 415. doi: 10.1037/0893-3200.21.3.407. http://dx.doi.org/10.1037/0893-3200.21.3.407. [DOI] [PubMed] [Google Scholar]
- Patistea E. Description and adequacy of parental coping behaviours in childhood leukaemia. International Journal of Nursing Studies. 2005;42:283–296. doi: 10.1016/j.ijnurstu.2004.06.010. http://dx.doi.org/10.1016/j.ijnurstu.2004.06.010. [DOI] [PubMed] [Google Scholar]
- Rodriguez EM, Dunn MJ, Zuckerman T, Vannatta K, Gerhardt CA, Compas BE. Cancer-related sources of stress for children with cancer and their parents. Journal of Pediatric Psychology. 2012;37:185–197. doi: 10.1093/jpepsy/jsr054. http://dx.doi.org/10.1093/jpepsy/jsr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD, Dennig MD, Weisz JR. Determinants and consequences of children’s coping in the medical setting: Conceptualization, review, and critique. Psychological Bulletin. 1995;118:328–357. doi: 10.1037/0033-2909.118.3.328. http://dx.doi.org/10.1037/0033-2909.118.3.328. [DOI] [PubMed] [Google Scholar]
- Sahler OJZ, Fairclough DL, Phipps S, Mulhern RK, Dolgin MJ, Noll RB, Butler RW. Using problem-solving skills training to reduce negative affectivity in mothers of children with newly diagnosed cancer: Report of a multisite randomized trial. Journal of Consulting and Clinical Psychology. 2005;73:272–283. doi: 10.1037/0022-006X.73.2.272. http://dx.doi.org/10.1037/0022-006X.73.2.272. [DOI] [PubMed] [Google Scholar]
- Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychological Bulletin. 2003;129:216–269. doi: 10.1037/0033-2909.129.2.216. http://dx.doi.org/10.1037/0033-2909.129.2.216. [DOI] [PubMed] [Google Scholar]
- Steer RA, Ranieri WF, Beck AT, Clark DA. Further evidence for the validity of the Beck Anxiety Inventory with psychiatric outpatients. Journal of Anxiety Disorders. 1993;7:195–205. http://dx.doi.org/10.1016/0887-6185(93)90002-3. [Google Scholar]
- Wadsworth ME, Raviv T, Compas BE, Connor-Smith J. Parent and adolescent responses to poverty-related stress: Tests of mediated and moderated coping models. Journal of Child and Family Studies. 2005;14:283–298. http://dx.doi.org/10.1007/s10826-005-5056-2. [Google Scholar]
- Weisz JR, McCabe MA, Dennig MD. Primary and secondary control among children undergoing medical procedures: Adjustment as a function of coping style. Journal of Consulting and Clinical Psychology. 1994;62:324–332. doi: 10.1037//0022-006x.62.2.324. http://dx.doi.org/10.1037/0022-006X.62.2.324. [DOI] [PubMed] [Google Scholar]