Abstract
Alcohol septal ablation (ASA) in hypertrophic obstructive cardiomyopathy reduces left ventricular outflow tract gradients. A third of patients do not respond; inaccurate localisation of the iatrogenic infarct can be responsible. Transthoracic echocardiography (TTE) using myocardial contrast can be difficult in the laboratory environment. Intra-cardiac echocardiography (ICE) provides high-quality images. We aimed to assess ICE against TTE in ASA. The ability of ICE and TTE to assess three key domains (mitral valve (MV) anatomy and systolic anterior motion, visualisation of target septum, adjacent structures) was evaluated in 20 consecutive patients undergoing ASA. Two independent experts scored paired TTE and ICE images off line for each domain in both groups. The ability to see myocardial contrast following septal arterial injection was also assessed by the cardiologist performing ASA. In patients undergoing ASA, ICE was superior in viewing MV anatomy (P=0.02). TTE was superior in assessing adjacent structures (P=0.002). There was no difference in assessing target septum. Myocardial contrast: ICE did not clearly identify the area of contrast in 17/19 patients due to dense acoustic shadowing (8/19) and inadequate opacification of the myocardium (6/19). ICE only clearly localised contrast in 2/19 cases. ICE does not visualise myocardial contrast well and therefore cannot be used to guide ASA. TTE was substantially better at viewing myocardial contrast. There was no significant difference between ICE and TTE in the overall ability to comment on cardiac anatomy relevant to ASA.
Keywords: hypertrophic obstructive cardiomyopathy, alcohol septal ablation, non-surgical septal reduction therapy
Introduction
Hypertrophic cardiomyopathy (HCM) is an inherited disease, characterised by otherwise unexplained hypertrophy of the myocardium. It has an estimated phenotypic prevalence of one in 500 (1). It is a highly heterogeneous disease with variable penetrance and different patterns of hypertrophy. The prevalence of left ventricular outflow tract (LVOT) obstruction in HCM is 20–30% at rest (2) and up to 70% with provocation (3). LVOT obstruction is associated with increased dyspnoea, a greater incidence of stroke and higher mortality (2). Successful alcohol septal ablation (ASA) can improve symptoms of dyspnoea and chest pain, and may improve prognosis (4, 5, 6, 7).
Systolic anterior motion (SAM) of the mitral valve (MV) is critical to the pathophysiology of LVOT gradient formation in most hypertrophic obstructive cardiomyopathy (HOCM) patients. The development of significant intra-cavity pressure is associated with severe SAM. Movement of the MV apparatus towards the septum significantly reduces LVOT area. LV pressures then increase to eject blood through the narrowed LVOT and maintain systemic blood pressure, resulting in increased flow velocities through the LVOT. This increased pressure accentuates SAM, leading to a further reduction in LVOT area until the anterior MV leaflet contacts the basal septum. This can initiate a positive amplifying feedback loop resulting in significant gradients through the LVOT (8). Interrupting this positive amplifying feedback loop by damaging myocardium at the SAM-septal contact area is the aim of ASA.
Failure of ASA can occur when the iatrogenic infarct is exclusively sited in the right ventricular septal myocardium (9, 10); the most common site for undesirable contrast localisation has been reported to be the RV septum and moderator band (11). Other structures of high importance are the mid-septum and anterior papillary muscle as they are closely linked in vascular supply (12). Alcohol injection these regions will not affect LVOT haemodynamics and can be dangerous.
The procedure has been well described (13). International guidelines recommend the use of myocardial-contrast echocardiography (MCE) during ASA (14). MCE is used to confirm the myocardial distribution of individual septal vessels before injection of alcohol. Transthoracic echocardiography (TTE) is the imaging modality of choice for guiding ASA. There are significant difficulties in using TTE for this procedure. The images must be taken on-table, with the patient in a supine position. There are further logistical difficulties resulting from narrow catheterisation tables, lack of arm support and cramped space in most laboratories. These difficulties can result in substandard image quality.
In most cases, the images obtained are deemed to be of sufficient quality to comment on the localisation of contrast and likely alcohol distribution. However, a significant proportion of ASA procedures fail to resolve the LVOT gradient (6, 15, 16). This is usually due to inaccurate location of the iatrogenic infarct (9). Substandard procedural imaging may account for the inability to comment on highlighted territory from MCE before alcohol injection. We must therefore consider alternative approaches to procedural imaging.
Other echocardiographic modalities available are trans-oesophageal echocardiography and intra-cardiac echocardiography (ICE). ICE has been shown to provide high-quality images in other interventional procedures (17, 18). No sedation or anaesthetic agents are required for the use of ICE; it is therefore an attractive modality to guide ASA.
The aim of this study was therefore to assess the ability of ICE to guide ASA. Our hypothesis covered two aspects of analysis: ICE will be superior to TTE in determination of key anatomical features required for successful ASA, and ICE will be equivalent to TTE in localisation of myocardial contrast.
Methods
Study design
Before patient recruitment, a panel of experts comprising operators familiar with ICE, TTE and ASA devised a scoring system. This was created to directly compare the ability of ICE and TTE to identify anatomy relevant to ASA. It is imperative that the operator can see the movement of the MV, the target myocardium in the septum and other key structures (the mid-septum, anterior papillary muscle and RV cavity) adjacent to the target myocardium. Consequently, the scoring system was devised to assess each modality in these three domains (Table 1). In addition, the use of MCE to highlight the intended target zone was also directly compared between the two modalities.
Table 1.
Scoring system used to assess quality of echocardiographic images to guide ASA
| Score | Observation |
|---|---|
| Mitral valve and SAM | |
| 2 | Able to determine SAM – septal contact point with precision such that images could allow determination of the length of AMVL in contact with septum at maximum excursion (or if no contact – ability tocomment with confidence on the movement of the anterior mitral valve leaflet in systole and diastole) |
| 1 | Able to localise approximate SAM – septal contact point (or, if there is no contact with the septum, able to localise approximate anterior leaflet tip position at point of maximum excursion) |
| 0 | Unable to determine tip position of the anterior leaflet in relation to the interventricular septum |
| Target septum | |
| 2 | Able to define endocardial border of basal ventricular septum in both RV and LV with visualisation of central intra-septal ‘fusion line’ between RV and LV. On-axis images |
| 1 | Able to define endocardial border of proximal ventricular septum in both RV and LV but no visualisation of central intra-septal ‘fusion line’ between RV and LV |
| 0 | Unable to clearly define endocardial border of one or both sides of the ventricular septum. |
| Other structures; RV cavity, anterior papillary muscle, mid-septum | |
| 2 | 3 key structures |
| 1 | 2 key structures |
| 0 | 0 or 1 key structure |
ICE and TTE were performed in HOCM patients undergoing ASA. Twenty consecutive patients undergoing ASA at Liverpool Heart and Chest Hospital (LHCH) were recruited. LHCH is a large volume centre for ASA in the UK (19).
The study was approved and supported by the research and development board of LHCH. Patients were informed and consented accordingly; the patient information leaflet is available upon request.
Image acquisition
ICE images were acquired by the interventional cardiologist performing ASA using an 8Fr AcuNav catheter (Siemens Acuson, Mountain View, CA, USA) and VIVID Q console (GE Healthcare, Horten, Norway), GE. The catheter tip was inserted via the right femoral vein. This was manipulated into the right ventricular inlet area for image acquisition. The phased array probe was directed to image the inter-ventricular septum; this displayed a left ventricle long-axis view. TTE images (VIVID I, GE Healthcare, 3Sc RS probe, GE) were acquired focussing on the LVOT and were predominantly the parasternal long axis (PLAX), apical five chamber and apical three chamber. Images were acquired according to standard British Society of Echocardiography guidelines (20). Myocardial contrast (0.5 ml Sonovue, Bracco, High Wycombe, UK) was injected into previously identified septal vessels. Separate coronary injections were performed for ICE and TTE.
Image analysis
Two expert reviewers experienced in the use of ICE independently performed off-line analysis of all images. ICE and TTE were assessed according to the pre-defined scoring system. The scores presented are a mean of the two reviewers. Due to the difference in appearance of TTE and ICE images blinding to the echocardiographic modality was not possible.
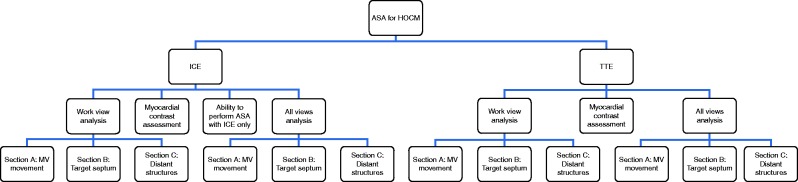
The comparison of each modality to identify relevant anatomy using the scoring system was performed in two pre-determined stages (see Fig. 1). In the primary analysis, the reviewers applied the scoring system using only the ‘work view’. This was a single view chosen from a standard range of TTE and ICE images before contrast injection. The work view was chosen by the expert reviewer as the projection that maximised scoring according to the pre-defined scoring system.
Figure 1.
Flow chart describing method of analysis for ICE and TTE in phases 1 and 2 respectively.
This was designed to mimic the approach used in ASA as a single-contrast injection can highlight perfused myocardium for <10 s. This only allows acquisition of a single view in most cases. The chosen loops were recorded and declared (the cines for phase 2 are available in Video 1).
The chosen ICE and TTE cines for all patients are presented in sequence. Each patient has a unique identifier ‘HOCM_number’. Where the reviewers did not agree on the best film to maximise scores each chosen cine is shown. These are the films used to create scores in phase 2. Download Video 1 via http://dx.doi.org/10.1530/ERP-15-0002-v1
Download Video 1 (63.4MB, avi)
If required multiple-contrast injections can be performed in ASA allowing multiple views to be obtained. Therefore, a secondary analysis was performed allowing reviewers to choose separate views in order to maximise the scores for each of the three domains; MV, target septum and other structures. This was termed ‘all views’ analysis.
Statistical analysis was performed using Stats Direct version 2.8.0.0 (Altrincham, Cheshire, UK). We used Wilcoxon's signed rank test to compare the non-parametric ICE and TTE scores.
Finally, we assessed the potential of ICE to be used in ASA instead of TTE. ICE images were therefore acquired before TTE. The interventional cardiologist performing ASA was asked to comment on the ability to perform the procedure using ICE as the sole imaging modality. This relied on visualising relevant anatomy and highlighted myocardium with contrast injection.
Results
Analysis of scores: working view
The results are summarised in Table 2. ICE was superior when viewing the MV and SAM, a score of 1.88 (±0.28) vs TTE value of 1.60 (±0.45) (P=0.02). There was no significant difference in viewing target septum. The ability of ICE to see the intra-septal fusion line was greater in this section, but it often lost points on the inability to clearly see the RV endocardial border. The probe was usually positioned very close to the septum; the echo window therefore did not include any RV cavity. TTE scored higher when viewing other structures. The low scores were due to the inability of both modalities to see the anterior papillary muscle. The mid-septum and RV cavity were visible in almost all TTE images, and in a smaller number of ICE images (Table 3).
Table 2.
Analysis scores for ICE vs TTE
| ICE | TTE | P | |
|---|---|---|---|
| Work view (n=20) | |||
| MV and SAM | 1.88 (±0.28) | 1.60 (±0.45) | 0.02 |
| Target septum | 1.28 (±0.64) | 1.08 (±0.39) | 0.30 |
| Other structures | 0.63 (±0.39) | 1.03 (±0.19) | 0.002 |
| All views (n=20) | |||
| MV and SAM | 1.93 (±0.18) | 1.63 (±0.39) | 0.007 |
| Target septum | 1.35 (±0.49) | 1.10 (±0.21) | 0.06 |
| Other structures | 0.85 (±0.43) | 1.08 (±0.24) | 0.13 |
Table 3.
Phase 1; other structures visible for work view and all view analysis in both phases. The number of times each reviewer commented a structure was visible is displayed along with a mean of observations
| ICE | TTE | |||||
|---|---|---|---|---|---|---|
| ICE 1 | ICE 2 | Mean | TTE1 | TTE2 | Mean | |
| Work view | ||||||
| Mid septum n (%) | 13 | 14 | 13.5 (67.5) | 20 | 20 | 20 (100) |
| Anterior papillary n (%) | 0 | 1 | 0.5 (2.5) | 0 | 2 | 1 (5) |
| RV cavity | 17 | 14 | 15.5 (77.5) | 20 | 20 | 20 (100) |
| All views | ||||||
| Mid septum n (%) | 17 | 15 | 16 (80) | 19 | 20 | 19.5 (97.5) |
| Anterior papillary n (%) | 1 | 2 | 1.5 (7.5) | 1 | 3 | 2 (10) |
| RV cavity | 19 | 15 | 17 (85) | 20 | 20 | 20 (100) |
Analysis of scores: all views
Using multiple views had a greater effect in ICE than in TTE (Table 2). ICE remained superior at seeing the MV. The difference in seeing target myocardium was more marked and neared statistical significance. ICE scored better when viewing other structures, there was now no significant difference between modalities. The PLAX view was the preferred TTE view from both reviewers, with a much smaller percentage of apical views chosen.
Assessment of agreement between reviewers
We examined the inter-observer difference in image assessment between the two experts. The κ statistic value over all scores was 0.55, P<0.0001. For each pair of observations, the observed mean difference was 0.36 (95% CI 0.29–0.43). This suggests that, on average, for each three sets of paired score groups, there is an isolated difference of a single point (e.g. reviewer A scores 2, 2, 1 in the respective three sections and reviewer B scores 2, 1, 1). This demonstrates a good clinical agreement.
Myocardial contrast echocardiography
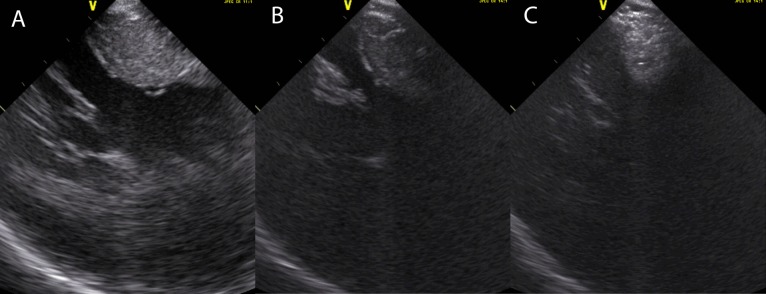
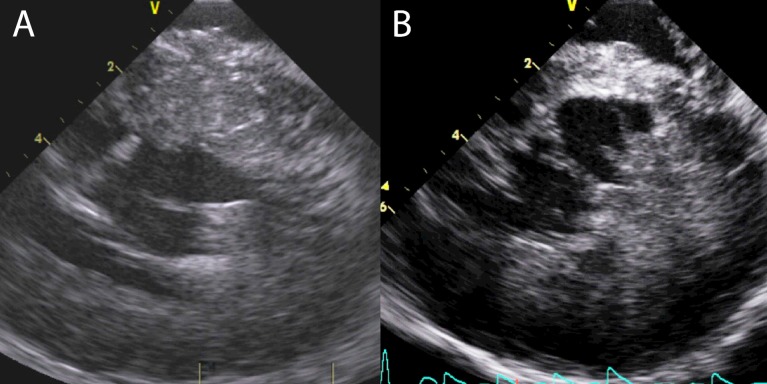
The ability to comment on contrast localisation is critical to safe and accurate ASA and was significantly better with TTE (Table 4). In some ICE images, the contrast did not opacify the myocardium adequately. The operator could not confidently comment on localisation in these cases. Contrast could be clearly seen in paired, simultaneous TTE images (see Fig. 2). In others, the opacification was vivid, but the acoustic shadowing was so pronounced that it was impossible to comment on cardiac structures beyond the contrast (see Fig. 3).
Table 4.
Observations from ICE images following intra-coronary contrast injection
| Observation | Incidence (n=20) |
|---|---|
| Dense acoustic shadowing | 8 |
| Inadequate opacification of myocardium | 6 |
| Contrast localised to distal structures | 3 |
| Possible using just ICE | 2 |
| No injection | 1 |
Figure 2.
(A) and (B) show ICE images. (C) and (D) show paired TTE images. (B) and (D) are simultaneous images taken with myocardial contrast injection. The contrast is much more vivid in TTE (D) than ICE (B).
Figure 3.
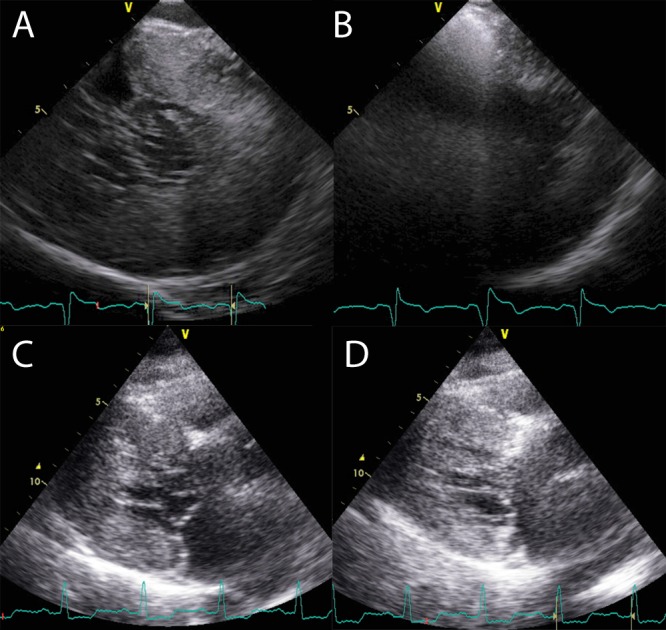
(A) and (B) show ICE images. (C) and (D) show paired TTE images. (B) and (D) are simultaneous images taken with myocardial contrast injection. There is significant acoustic shadowing seen following contrast injection in the ICE image (B). There is minimal shadowing seen on TTE (D).
There were three examples of contrast localising to distal structures only rather than the target area. These patients did not receive alcohol injection. This was not visualised on the ICE working view, but was seen on TTE. The contrast had passed by the time the ICE catheter was manipulated into the correct position. It is impossible to know in these cases whether the contrast is in the correct area and cannot be seen due to issues with the use of ICE, or if it localised outside the target area and echocardiographic window. There were only two cases in which the procedure could potentially have been performed using just ICE-contrast images.
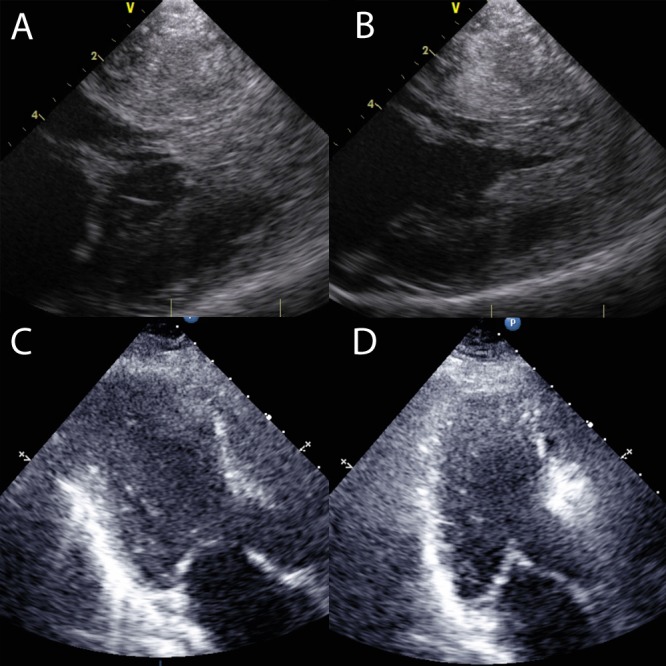
We adapted frequency settings on the ICE probe to attempt to see contrast in those cases with inadequate opacification of myocardium. The baseline of 11 MHz was reduced sequentially down to 5 MHz. This allowed us to see contrast in some, but the image quality was so poor that we were unable to relate it to relevant anatomy (see Fig. 4). Using tissue harmonics settings (5.0/9.5 MHz) had a similar effect.
Figure 4.
(A) shows a long-axis ICE view of the left ventricle using a frequency of 11 MHz. (B) shows the same transducer position with a frequency of 5 MHz. (C) shows a myocardial contrast injection at a frequency of 5 MHz. Myocardial contrast is visible in the basal septum in (C), but to allow the operator to see this a reduction in frequencies is required. This degrades the image to the extent that it cannot be relied upon to accurately comment on cardiac anatomy.
TTE was performed very well in this section. Ultimately all alcohol injections were guided by TTE as contrast could be seen in all 19 patients without the phenomena described in ICE.
Discussion
ICE was able to see the interaction of the MV and the target septum very well, ICE was superior to TTE in this section. The proximity of the probe to the MV and increased fidelity of images provided a clear, real-time image of the motion of the valve, allowing accurate identification of target myocardium.
There was no significant difference between ICE and TTE when viewing target myocardium in the septum. ICE images were often unsatisfactory as we were unable to see the RV endocardial border. The catheter seemed to lie on the RV endocardial septal surface more often than when used for other interventions such as patent foramen ovale (PFO) closure. This could be due to the altered anatomy seen in HCM. When it was possible to create space between the catheter and the septum, the ICE images were superior in detailing LV endocardium and intra-septal fusion line.
TTE was superior to ICE in seeing other structures. In the HOCM population, the anterior papillary muscle was seen only once in all of the working views that focussed on the LVOT. The anterior displacement of papillary muscle architecture previously described in HCM would explain this (21). As the muscle moves anteriorly in the LV, it moves further away from a plane of image that incorporates the LVOT (see Fig. 5). The proximity of the ICE catheter to the target area meant that the echocardiographic field was more limited. The predominant TTE work view was PLAX.
Figure 5.
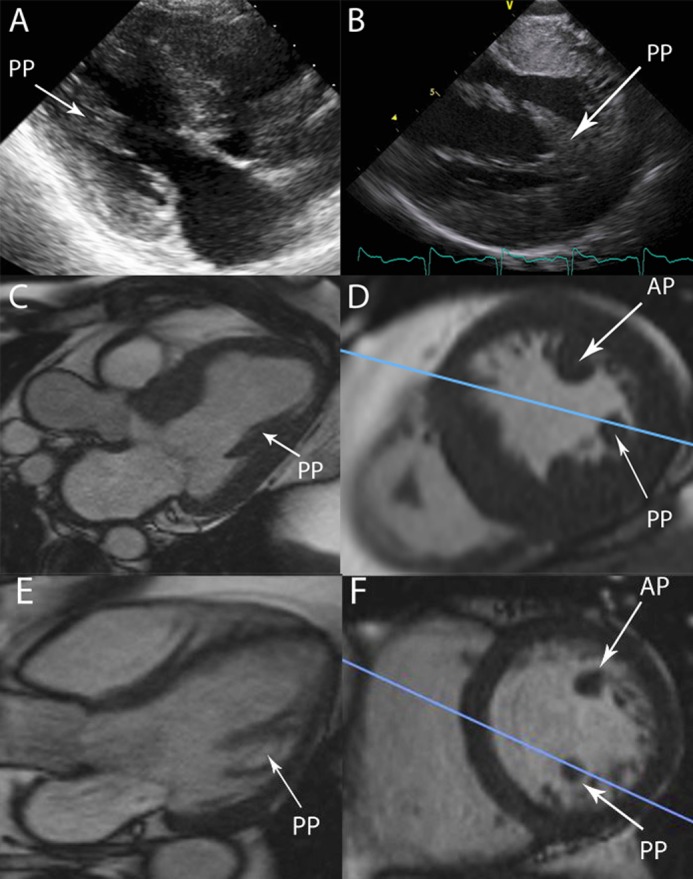
(A) shows a typical TTE PLAX echo image, the papillary muscle in view is the posterior muscle. (B) shows a typical ICE long-axis view of the left ventricle, with both heads of the posterior muscle visible. (C) shows a three-chamber CMR still with a papillary muscle labelled. Relational short axis CMR images show this to be the posterior muscle (PP), the blue line represents the plane displayed in the three chamber view in (C). The anterior muscle (AP) is out of shot and would be very difficult to see in the same plane as the LVOT. The same perspectives are displayed in the non-HCM heart in (E) and (F).
The ability to use more than one loop in the ‘all views’ section allowed ICE to improve scores when viewing target septum, and to achieve near parity with TTE in seeing other structures. This required manipulation of the ICE catheter, an acquired skill that was often not straightforward.
Myocardial contrast echocardiography
Visualisation of contrast distribution is imperative to ASA. Several problems were encountered when using ICE. Contrast agents are predominantly used in TTE to opacify the LV cavity when assessment of function is difficult. The development of these agents has been targeted at providing appropriate backscatter when ultrasound is projected from several centimetres away, as is the case in TTE. When TTE image quality is good, contrast localisation can be seen well during ASA.
The technology of the Acunav ICE transducer is similar to that of TTE, a miniaturised phased-array probe. The major differences are the proximity to the visualised structures and higher frequencies used. The signal processing techniques used in modern echocardiographic modules have previously allowed assessment of MCE in high- and low-mechanical index settings (22). We therefore did not anticipate a problem visualising contrast with ICE.
The paradoxical events of inability to visualise contrast in some, and acoustic shadowing in others were difficult to explain. The explanation of this phenomenon is an area for future study. This should involve exploring differing doses of contrast and echocardiographic frequencies.
The images acquired with ICE alone were of sufficient quality to progress to alcohol injection in only 2/19 (11%) cases. The inability to see contrast with ICE means that this modality cannot be used to guide ASA.
Anatomical observations
Some important anatomical lessons were noted. In the majority of ICE LV long-axis images, the focus of the echocardiographic field was the inferior septum. This position displays the LV similar to a four-chamber view in TTE. To see appropriate target myocardium adjacent to the LVOT, further right rotation is required on the ICE catheter. This brings the true LVOT in to view. An example of this is shown in Fig. 6.
Figure 6.
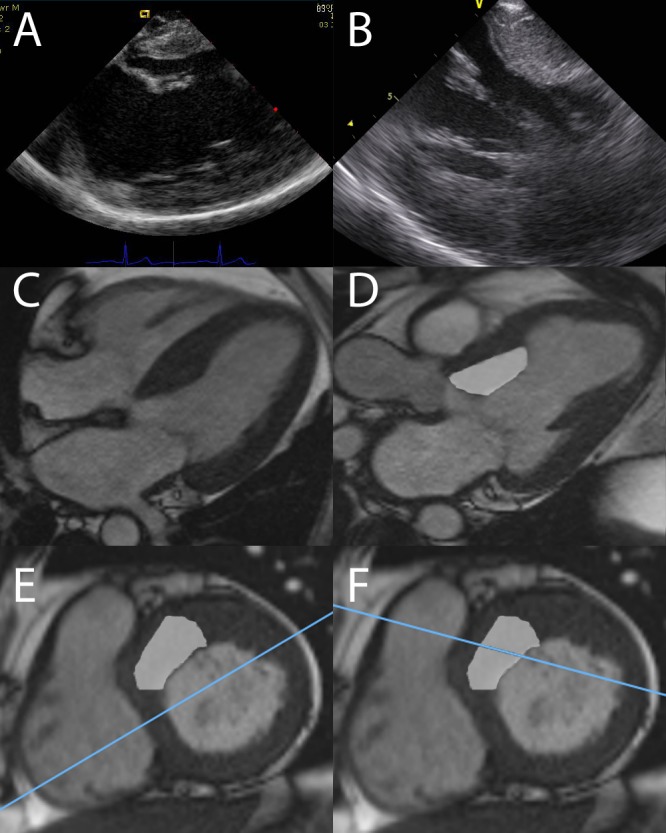
(A) shows a typical ICE image taken from phase 1. It is similar projection to a TTE four-chamber view taken from inside the RV. (C) shows a typical four chamber view In CMR. (E) shows a short-axis cut of the same heart. The blue line represents the cut of the LV that is shown in (C). The shaded area is the target for ASA. The blue line clearly passes through the inferior septum, missing the target area. (B) shows an ICE image with the true LVOT in view. This is represented in the three-chamber cardiac magnetic resonance (CMR) image in (D). The shaded area is the target for ASA. (F) shows the corresponding short-axis view, the blue line this time passes through the target myocardium in the true septum.
A papillary muscle was often visible and interpreted as the anterior muscle during image acquisition. A further investigation of papillary muscle architecture using relational images from cardiac magnetic resonance imaging showed this to be the posterior papillary muscle (see Fig. 5). Historically, in anatomical studies, the posterior muscle has been described as receiving blood supply from the right coronary system (12). It is unlikely to be of vascular relevance when injecting contrast into septal vessels originating from the left coronary system. It is rare to visualise the anterior papillary muscle in the same plane as the target septum and LVOT.
ICE images of the interaction of the anterior MV leaflet and the septum are of such high quality that they provide new insights. The ability to visualise the abnormal MV anatomy was extremely clear on ICE. It has been previously reported that the anterior mitral valve leaflet (AMVL) is elongated in HCM (23, 24). It has been proposed to be part of the genetically determined phenotype rather than the effects of haemodynamic disturbance in the LVOT (25). A long AMVL would lend itself to the pathophysiology seen in obstruction in HCM. The extra length results in coaptation with the posterior leaflet towards its mid-point, leaving a redundant tip. This redundant tip is then caught in the abnormal flow in the LV. This is seen clearly with ICE (see Fig. 7, Video 2 and Video 3). This redundant tip is very flexible and bends back in to the LVOT to contact the septum.
The redundant tip of the mitral valve displays great flexibility and bends back into the LVOT to contact the septum. This is seen with great clarity on ICE films. It is this contact that initiates the positive amplifying feedback cycle leading to significant LVOT gradients. Download Video 2 via http://dx.doi.org/10.1530/ERP-15-0002-v2
Download Video 2 (234.6KB, avi)
An area of previous infarct is visible in the mid septum. The myocardium is thinned and akinetic. This patient had an initial good response to alcohol ablation before a deterioration in symptoms and gradients at 6 months. The anterior leaflet of the MV now bends back to contact the viable myocardium in the extreme basal septum. She returned for repeat ASA. Download Video 3 via http://dx.doi.org/10.1530/ERP-15-0002-v3
Download Video 3 (294.3KB, avi)
Figure 7.
Both (A) and (B) show ICE images in systole with SAM-septal contact. In each example, the AMVL is folded back and has a bend of nearly 90. In (B), an area of iatrogenic infarct in the mid-septum from previous ASA is seen. The contact area for the AMVL is further basal, there is viable, contracting myocardium in this area.
The target for ASA is the SAM-septal contact point, as the phenomenon of contact leads to the majority of the intra-cavity gradient formation. This can be seen in several planes of ICE imaging and could be marked and projected onto available software to accurately detail the contact area in three dimensions. The damage we aim to deliver could then be more accurate and potentially more likely to succeed. This is an area for future study.
ICE can provide such accurate detail of myocardial structure that a coronary wire measuring 0.014” can be seen in target myocardium (see Fig. 8).
Figure 8.
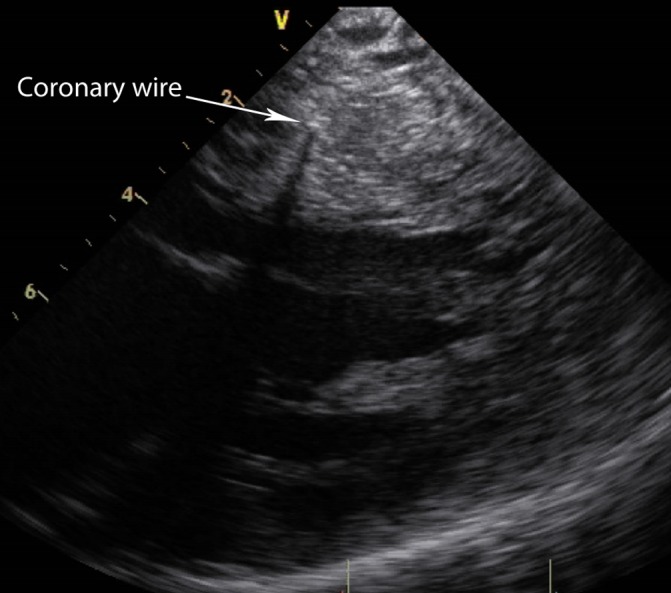
The arrow points towards the coronary wire. Acoustic shadowing is also seen. This is in the target myocardium.
ICE vs TTE in haemodynamic assessment of LVOT gradients
Earlier techniques in ASA relied on the change in LVOT gradient during balloon occlusion to identify the correct septal artery for alcohol injection (26). This has been largely superseded by the introduction of myocardial contrast echocardiography, but the improvement in LVOT gradient can provide the operator with an additional level of information regarding the suitability of the chosen septal vessel. To perform correct and accurate gradient assessment, Doppler echocardiography should be performed with the cursor in line with the LVOT, any ‘off angle’ assessment can underestimate velocity and hence gradients. ICE images of the LV are predominantly in a long-axis view with the LVOT perpendicular to the probe, thus underestimating velocity. It is possible to create a view akin to a TTE three- or five-chamber, but this is often unstable and unreliable. TTE remains the gold standard in this respect due to its flexibility.
Conclusion
ICE does not visualise myocardial contrast well and therefore cannot be used in the assessment of myocardial supply by septal coronary arteries during ASA. TTE was superior to ICE in visualising myocardial contrast. There was no significant difference between ICE and TTE in the overall ability to determine cardiac anatomy relevant to the performance of ASA.
Declaration of interest
This research was conducted with support from the Investigator-Initiated Study Program of Biosense Webster, Inc.; 20 Acunav ICE catheters and financial support were received.
References
- 1. Elliott P McKenna WJ Hypertrophic cardiomyopathy Lancet 363 2004. 1881–1891. 10.1016/S0140-6736(04)16358-7 [DOI] [PubMed] [Google Scholar]
- 2. Maron MS Olivotto I Betocchi S Casey SA Lesser JR Losi MA Cecchi F Maron BJ Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy New England Journal of Medicine 348 2003. 295–303. 10.1056/NEJMoa021332 [DOI] [PubMed] [Google Scholar]
- 3. Maron MS Olivotto I Zenovich AG Link MS Pandian NG Kuvin JT Nistri S Cecchi F Udelson JE Maron BJ Hypertrophic cardiomyopathy is predominantly a disease of left ventricular outflow tract obstruction Circulation 114 2006. 2232–2239. 10.1161/CIRCULATIONAHA.106.644682 [DOI] [PubMed] [Google Scholar]
- 4. Sorajja P Ommen SR Holmes DR Jr Dearani JA Rihal CS Gersh BJ Lennon RJ Nishimura RA Survival after alcohol septal ablation for obstructive hypertrophic cardiomyopathy Circulation 126 2012. 2374–2380. 10.1161/CIRCULATIONAHA.111.076257 [DOI] [PubMed] [Google Scholar]
- 5. Jensen MK Prinz C Horstkotte D van Buuren F Bitter T Faber L Bundgaard H Alcohol septal ablation in patients with hypertrophic obstructive cardiomyopathy: low incidence of sudden cardiac death and reduced risk profile Heart 99 2013. 1012–1017. 10.1136/heartjnl-2012-303339 [DOI] [PubMed] [Google Scholar]
- 6. Nagueh SF Groves BM Schwartz L Smith KM Wang A Bach RG Nielsen C Leya F Buergler JM Rowe SK et al. Alcohol septal ablation for the treatment of hypertrophic obstructive cardiomyopathy a multicenter North American registry Journal of the American College of Cardiology 58 2011. 2322–2328. 10.1016/j.jacc.2011.06.073 [DOI] [PubMed] [Google Scholar]
- 7. Jensen MK Almaas VM Jacobsson L Hansen PR Havndrup O Aakhus S Svane B Hansen TF Køber L Endresen K et al. Long-term outcome of percutaneous transluminal septal myocardial ablation in hypertrophic obstructive cardiomyopathy: a Scandinavian multicenter study Circulation. Cardiovascular Interventions 4 2011. 256–265. 10.1161/CIRCINTERVENTIONS.110.959718 [DOI] [PubMed] [Google Scholar]
- 8. Sherrid MV Chaudhry FA Swistel DG Obstructive hypertrophic cardiomyopathy: echocardiography, pathophysiology, and the continuing evolution of surgery for obstruction Annals of Thoracic Surgery 75 2003. 620–632. 10.1016/S0003-4975(02)04546-0 [DOI] [PubMed] [Google Scholar]
- 9. van Dockum WG ten Cate FJ ten Berg JM Beek AM Twisk JW Vos J Hofman MB Visser CA van Rossum AC Myocardial infarction after percutaneous transluminal septal myocardial ablation in hypertrophic obstructive cardiomyopathy: evaluation by contrast-enhanced magnetic resonance imaging Journal of the American College of Cardiology 43 2004. 27–34. 10.1016/j.jacc.2003.08.031 [DOI] [PubMed] [Google Scholar]
- 10. Amano Y Kitamura M Yamada F Aita K Takayama M Tachi M Kumita S Magnetic resonance imaging of microvascular obstruction in hypertrophic obstructive cardiomyopathy after percutaneous transluminal septal myocardial ablation. Acta Radiologica. 2014 doi: 10.1177/0284185114559871. [in press] [DOI] [PubMed] [Google Scholar]
- 11. Wallace EL Thompson JJ Faulkner MW Gurley JC Smith MD Septal perforator anatomy and variability of perfusion bed by myocardial contrast echocardiography: a study of hypertrophic cardiomyopathy patients undergoing alcohol septal ablation Journal of Interventional Cardiology 26 2013. 604–612. 10.1111/joic.12068 [DOI] [PubMed] [Google Scholar]
- 12. Rusu MC Petrescu CI Niculescu V Ionescu N Vlad M Considerations on the left papillary muscles microangioarchitecture Romanian Journal of Morphology and Embryology 47 2006. 63–66. [PubMed] [Google Scholar]
- 13. Cooper RM Shahzad A Stables RH Current status of nonsurgical septal reduction therapy in hypertrophic obstructive cardiomyopathy Interventional Cardiology 5 2013. 427–439. 10.2217/ica.13.33 [DOI] [Google Scholar]
- 14. Gersh BJ Maron BJ Bonow RO Dearani JA Fifer MA Link MS Naidu SS Nishimura RA Ommen SR Rakowski H et al. ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Circulation 124 2011. 2761–2796. 10.1161/CIR.0b013e318223e230 [DOI] [PubMed] [Google Scholar]
- 15. Steggerda RC Balt JC Damman K van den Berg MP Ten Berg JM Predictors of outcome after alcohol septal ablation in patients with hypertrophic obstructive cardiomyopathy. Special interest for the septal coronary anatomy Netherlands Heart Journal 21 2013. 504–509. 10.1007/s12471-013-0453-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cooper RM Shahzad A Stables RH Alcohol septal ablation for hypertrophic obstructive cardiomyopathy: safe and apparently efficacious but does reporting of aggregate outcomes hide less-favourable results, experienced by a substantial proportion of patients? Journal of Invasive Cardiology. 2014 [in press] [PubMed] [Google Scholar]
- 17. Ponnuthurai FA van Gaal WJ Burchell A Mitchell AR Wilson N Ormerod OJ Safety and feasibility of day case patent foramen ovale (PFO) closure facilitated by intracardiac echocardiography International Journal of Cardiology 131 2009. 438–440. 10.1016/j.ijcard.2007.07.141 [DOI] [PubMed] [Google Scholar]
- 18. MacDonald ST Newton JD Ormerod OJ Intracardiac echocardiography off piste? Closure of the left atrial appendage using ICE and local anesthesia. Catheterization and Cardiovascular Interventions 77 2011. 124–127. 10.1002/ccd.22652 [DOI] [PubMed] [Google Scholar]
- 19.Ludman P. British Cardiovascular Intervention Society Audit returns 2011, 2012.
- 20.Wharton G, Allen J, Brewerton H, Jones R, Kanagala P, Lloyd G, Masani N, Mathew T, Oxborough D, Rana B, et al. British Society of Echocardiography Minimum Dataset; A Standard Transthoracic Echo 2012; http://www.bsecho.org/tte-minimum-dataset/, 2012. [DOI] [PMC free article] [PubMed]
- 21. Reis RL Bolton MR King JF Pugh DM Dunn MI Mason DT Anterion-superior displacement of papillary muscles producing obstruction and mitral regurgitation in idiopathic hypertrophic subaortic stenosis. Operative relief by posterior–superior realignment of papillary muscles following ventricular septal myectomy Circulation 50: 2 Suppl 1974. Ii181–Ii188. [PubMed] [Google Scholar]
- 22. Kaul S Myocardial contrast echocardiography: a 25-year retrospective Circulation 118 2008. 291–308. 10.1161/CIRCULATIONAHA.107.747303 [DOI] [PubMed] [Google Scholar]
- 23. Jiang L Levine RA King ME Weyman AE An integrated mechanism for systolic anterior motion of the mitral valve in hypertrophic cardiomyopathy based on echocardiographic observations American Heart Journal 113 1987. 633–644. 10.1016/0002-8703(87)90701-0 [DOI] [PubMed] [Google Scholar]
- 24. Grigg LE Wigle ED Williams WG Daniel LB Rakowski H Transesophageal Doppler echocardiography in obstructive hypertrophic cardiomyopathy: clarification of pathophysiology and importance in intraoperative decision making Journal of the American College of Cardiology 20 1992. 42–52. 10.1016/0735-1097(92)90135-A [DOI] [PubMed] [Google Scholar]
- 25. Maron MS Olivotto I Harrigan C Appelbaum E Gibson CM Lesser JR Haas TS Udelson JE Manning WJ Maron BJ Mitral valve abnormalities identified by cardiovascular magnetic resonance represent a primary phenotypic expression of hypertrophic cardiomyopathy Circulation 124 2011. 40–47. 10.1161/CIRCULATIONAHA.110.985812 [DOI] [PubMed] [Google Scholar]
- 26. Gietzen FH Leuner CJ Raute-Kreinsen U Dellmann A Hegselmann J Strunk-Mueller C Kuhn HJ Acute and long-term results after transcoronary ablation of septal hypertrophy (TASH). Catheter interventional treatment for hypertrophic obstructive cardiomyopathy European Heart Journal 20 1999. 1342–1354. 10.1053/euhj.1999.1520 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The chosen ICE and TTE cines for all patients are presented in sequence. Each patient has a unique identifier ‘HOCM_number’. Where the reviewers did not agree on the best film to maximise scores each chosen cine is shown. These are the films used to create scores in phase 2. Download Video 1 via http://dx.doi.org/10.1530/ERP-15-0002-v1
Download Video 1 (63.4MB, avi)
The redundant tip of the mitral valve displays great flexibility and bends back into the LVOT to contact the septum. This is seen with great clarity on ICE films. It is this contact that initiates the positive amplifying feedback cycle leading to significant LVOT gradients. Download Video 2 via http://dx.doi.org/10.1530/ERP-15-0002-v2
Download Video 2 (234.6KB, avi)
An area of previous infarct is visible in the mid septum. The myocardium is thinned and akinetic. This patient had an initial good response to alcohol ablation before a deterioration in symptoms and gradients at 6 months. The anterior leaflet of the MV now bends back to contact the viable myocardium in the extreme basal septum. She returned for repeat ASA. Download Video 3 via http://dx.doi.org/10.1530/ERP-15-0002-v3
Download Video 3 (294.3KB, avi)



 This work is licensed under a
This work is licensed under a