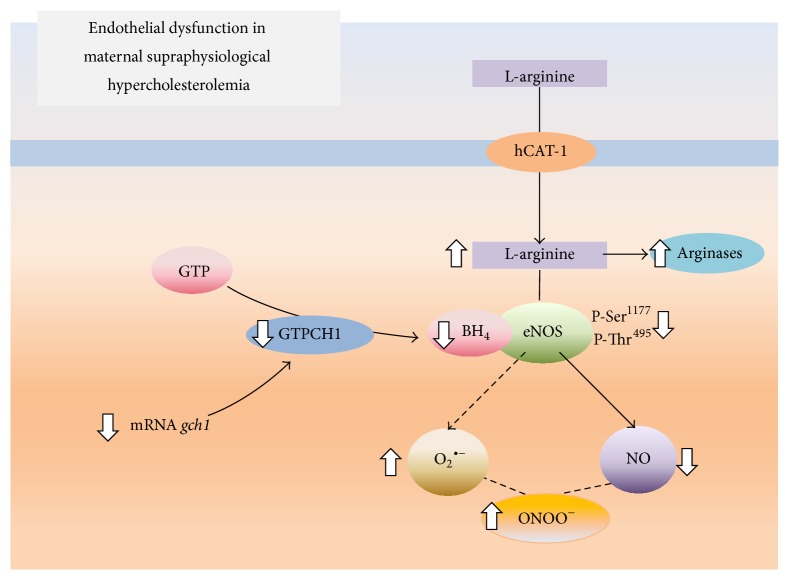
Figure 2.
Effect of maternal supraphysiological hypercholesterolemia on the endothelial L-arginine/NO signaling pathway. In umbilical vein endothelial cells from pregnancies complicated by maternal physiological hypercholesterolemia, the amino acid L-arginine is taken up by the human cationic amino acid transporter 1 (hCAT-1) and metabolized by endothelial nitric oxide synthase (eNOS) and, to a lesser extent, arginases. This phenomenon occurs in the presence of tetrahydrobiopterin (BH4), resulting in NO generation. BH4 is generated by the enzyme GTP cyclohydrolase 1 (GTPCH1), which is coded by the gch1 gene and whose substrate is GTP. In cells from pregnancies where the pregnant women had maternal supraphysiological hypercholesterolemia, hCAT-1-mediated L-arginine transport is increased (⇑), increasing the availability of this amino acid for eNOS and arginases. In this pathological condition, L-arginine is mainly used by arginases, limiting the formation of NO via eNOS. In addition, eNOS has reduced (⇓) activity because of the lower phosphorylation of Ser1177 and the bioavailability of BH4. The reduction in the BH4 concentration results from a reduced expression of gch1, leading to eNOS uncoupling and the generation of a superoxide anion (O2 ∙−). The O2 ∙− reacts with NO to form peroxynitrite (ONOO−; from data in [5–7, 14]).