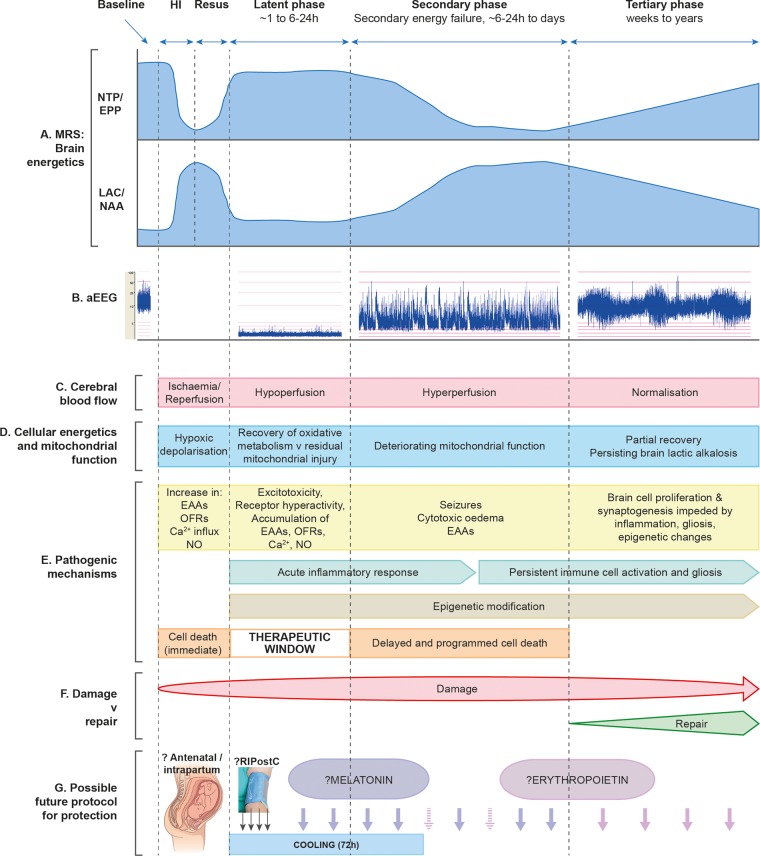
Figure 1.
Schematic diagram illustrating the different pathological phases of cerebral injury after cerebral HI. The primary phase (acute HI), latent phase, secondary energy failure phase and tertiary brain injury phase are shown. (A) Magnetic resonance spectra showing the biphasic pattern of NTP/EPP decline and lactate/NAA increase during primary and secondary phases following HI insult. Persisting lactic alkalosis is shown in tertiary phase. (B) Amplitude-integrated EEG showing normal trace at baseline, flat tract following HI, burst-suppression pattern in latent phase, emergence of seizures in secondary phase and normalisation with sleep–wake cycling in tertiary phase. (C) Following HI, there is a period of hypoperfusion associated with hypometabolism during latent phase, followed by relative hyperperfusion in secondary phase. (D) Cellular energetics and mitochondrial function are reflected in the biphasic response shown on magnetic resonance spectroscopy (A), with a period of recovery in latent phase followed by deterioration in secondary phase. There is partial recovery in tertiary phase. (E) The most important pathogenic changes are shown for each phase (see main text for description), including generation of toxic free radical species, accumulation of EAAs, cytotoxic oedema, seizures and inflammation. Cell lysis occurs immediately following HI, while programmed cell death occurs in secondary phase; latent phase provides a therapeutic window. Persisting inflammation and epigenetic changes impede long-term repair. (F) Damage is maximal in the secondary phase, but persists into the tertiary phase as inflammation and gliosis evolve. (G) In the future, neuroprotective treatments are likely to involve a ‘cocktail’ of therapies to be administered intrapartum, in the latent phase to prevent secondary energy failure and through secondary and tertiary phases to offset evolving damage. HI, hypoxia-ischaemia; EAAs, excitatory amino acids; EPP, exchangeable phosphate pool; NAA, N-acetylaspartate; NO, nitric oxide; NTP, nucleoside triphosphate (this is mainly ATP); OFRs, oxygen free radicals; RIPostC, remote ischaemic postconditioning.