Abstract
Importance
Visual impairment due to myopia is an important public health issue. Recent analysis of population-based cohorts aged 15-22 years-old recruited from the UK and Israel, suggested myopia and high myopia were ~10% more common in first-born compared to later-born children.
Objectives
To examine whether myopia was associated with birth order in an earlier generation than studied previously, and if so, whether the association was attenuated after adjusting for education exposure, as predicted by the hypothesis that the education of children with later birth orders is less intense.
Design, setting, and participants
Cross-sectional study of UK Biobank participants recruited from 2006 to 2010. Analysis was restricted to participants 40-69 years-old who had a vision assessment, self-reported ethnicity ‘White’, and no history of eye disorders (N=89,120). Myopia and high myopia were defined as autorefraction <= −0.75D and <= −6.00D, respectively.
Exposures
Birth order and information on potential confounders including highest educational qualification ascertained using a structured questionnaire.
Main Outcome Measures
Odds ratio (OR) for myopia and high myopia by birth order, using logistic regression adjusting for age and sex (Model 1), or age, sex, and highest educational qualification (Model 2).
Results
Model 1 (no adjustment for education): Birth order was associated with both myopia and high myopia, e.g. comparing first versus second born individuals, OR = 1.12 (95% CI 1.08 to 1.16, P=1.4E-11) and OR = 1.21 (95% CI 1.11 to 1.30, P=3.6E-6) for myopia and high myopia, respectively. The risk of myopia became progressively lower for later-birth orders suggesting a dose-response. Model 2 (after adjusting for education): The effect sizes were attenuated by approximately 25%: OR = 1.09 (95% CI 1.05 to 1.12, P=1.3E-6) and OR = 1.15 (95% CI 1.06 to 1.25, P=4.6E-4) for myopia and high myopia, respectively, and the apparent dose-response was abolished.
Conclusions and Relevance
These data suggest that the association between birth order and myopia is not due to a new environmental pressure in the last 30-40 years. The attenuated effect size after adjusting for educational exposure supports a role for reduced parental investment in education of children with later birth orders in their relative protection from myopia.
Introduction
Myopia is increasing in prevalence in younger generations in many parts of the world, and because the condition is a cause of visual impairment and blindness – either directly through myopic chorioretinal atrophy and choroidal neovascularisation, or indirectly through predisposition to cataract, glaucoma and retinal detachment – it is becoming an increasingly important public health issue1-3. Major known risk factors for myopia are genetic background, time spent outdoors and time spent doing nearwork (including educational activities)4-6. However, refractive error is also associated with early life and life-course factors, such as maternal age, maternal smoking, gestational age, season of birth, and birth order7-11.
In a recent study of four groups of participants (4,401 children aged 15 years from a UK birth cohort; 888,277 Israeli Defense Force recruits aged 16-22 years; 1,959 Singaporean children aged 13 years; 1,344 young adults aged 20 years from an Australian birth cohort) there was strong statistical support for an association between birth order and myopia in the two larger samples, but weak/little support for the two smaller samples10. In the largest cohort, there was also evidence for a “dose-response” relationship, with myopia being increasingly less common in individuals the more older siblings they had. One potential cause of the association between birth order and myopia is parental investment in education12. On average, parents have been reported to direct more of their available resources to earlier-born children, resulting in better educational attainment in earlier-born than later-born individuals13,14. Thus, parents may expose their earlier-born children to a more myopia-predisposing environment. Here, we sought to replicate the previously-reported association between birth order and myopia in an older sample of UK adults, and to examine whether adjusting for educational exposure attenuated any association observed in this sample.
Methods
UK Biobank assessments
The UK Biobank15 recruited 502,649 participants aged 37–73 years, during 2006–2010. Participants attended one of 22 assessment centres, at which they completed a touch-key questionnaire, had a face-to-face interview with a trained nurse, and underwent physical assessments. During later stages of recruitment, the assessments included an ophthalmic component. All assessments adhered to standardised protocols. Ethical approval was obtained from the National Health Service (NHS) National Research Ethics Service (Ref 11/NW/0382) and all participants provided informed consent.
The touch-key questionnaire included information about demographics and potential confounders, namely: ethnicity, ophthalmic history, number of total/older siblings, birth weight, maternal age, current time spent outdoors during summer ( “In a typical DAY in summer, how many hours do you spend outdoors?”) and educational or professional qualifications ( “Which of the following qualifications do you have [you can select more than one]?”; with the options, “College or University degree, A-levels/AS-levels, O-levels, CSEs or equivalent, NVQ or HND or HNC or equivalent, other professional qualifications, e.g: nursing, teaching, none of the above”). Age at which continuous full time education was completed was asked of individuals not reporting a college or university degree. Refractive error was measured by non-cycloplegic autorefraction (Tomey RC5000 autorefractor) after removing habitual spectacles or contact lenses, as part of the ophthalmic assessment.
Classification of participant demographics and ocular phenotype
Birth orders of 4 and above were combined due to small numbers. Non-singletons (e.g. twins) were excluded. Ethnicity was classified as either “White” (self-report of “British, Irish, or any other white background”) or “Other” (self-report of Indian, Pakistani, African, Chinese, mixed-race, or “prefer not to answer”). Individuals who reported non-White ethnicity, and those aged <40 or >69 years-old, were excluded due to their low numbers, especially for higher birth orders. Since the relationship between age and the prevalence of myopia was non-linear (Figure 1) age was modelled as a categorical variable in 3-year intervals (40-42, 43-45, 46-48, 49-51, 52-54, 55-57, 58-60, 61-63, 64-66 and 67-69 years). Maternal age was categorised as five groups: <20, 20-24, 25-29, 30-34, and >34 years. Self-reported birth weight was filtered to exclude participants with a Z-score >4. Each participant was assigned a Townsend Deprivation Index (TDI) score corresponding to their postcode area, based on the preceding national census output areas. Highest educational qualification was categorised into 4 levels: None; O-levels, CSEs or equivalent; A-levels/AS-levels, NVQ or HND or HNC or equivalent, or other professional qualification; Degree. For the Biobank participants’ generation, the UK school system provided free universal compulsory education between the ages of 5 and 15/16 years. Standard examinations were taken at the ages of 16 (O-levels, CSEs), 17 (A/S-levels), and 18 years (A-levels). NVQ, HND and HNC refer to vocational qualifications that required approximately 2 or more years of part-time or full-time study after the age of 15.
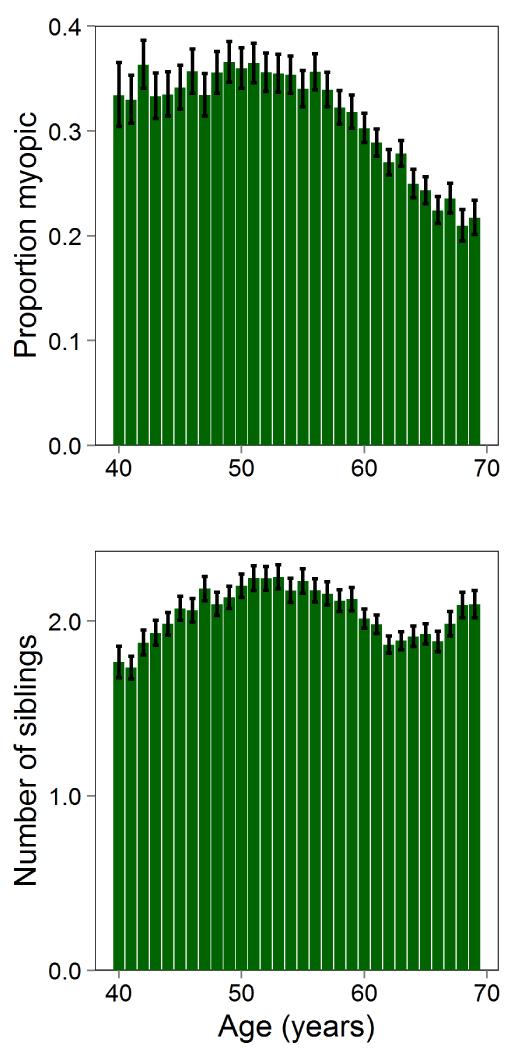
Figure 1. Relationship between myopia prevalence and age, and between proband-reported number of siblings and age.
Proportion of UK Biobank participants (N= 89,120) categorized as myopic (upper panel) and average number of siblings reported (lower panel) plotted for each one-year age interval. Note that “only-children” were included in these analyses. Error bars denote 95% confidence intervals.
Participants were excluded if they reported a history of cataract, cataract surgery, corneal graft surgery, laser eye surgery, or serious eye trauma, as were autorefraction readings if accompanied by a “low reliability” or “lower reliability” error message. Spherical equivalent was calculated as the spherical power plus half the cylinder power, and averaged between fellow eyes. Individuals with a refractive error <= −0.75 D and <= −6.00 D were classified as myopic and highly myopic, respectively.
Statistical analyses
The odds ratio (OR) for myopia in participants of birth orders 1 through 4+ was estimated using logistic regression. An initial analysis was conducted that adjusted for age and sex only (Model 1) followed by analyses that also included highest educational qualification (Model 2) and highest educational qualification, maternal age, birth weight, TDI (natural-log-transformed to remove skew), and time currently spent outdoors in summer (Model 3). Analogous models were used to calculate the OR for high myopia vs. non-myopic (this resulted in a reduction in participant numbers due to the exclusion of mild/moderate myopes). A final model was used to gauge an alternative measure of educational exposure; this model adjusted for age, sex and age-completed-full-time-education (Model 4). Details of participants included and excluded from each analysis model are presented in eTables 1-3 in the Supplement. An analysis of the relationship between birth order and the level of refractive error was also carried out (Online Supplementary Material). Only-children were included in all analyses, except where indicated.
Results
Approximately 23% of UK Biobank participants underwent autorefraction and N=89,120 were included in the analysis (white, aged 40-69: see Table 1). The prevalence of myopia varied non-linearly with age (Figure 1, upper panel) while the number of siblings was relatively stable at an average of 2 (Figure 1, lower panel).
Table 1. Demographic characteristics in participants with complete or incomplete information on potential confounders.
| Variable | Sample with incomplete information (N=63,842) | Sample with full information (N=25,278) | P-value |
|---|---|---|---|
| Age (years) a | 59.0 (7.2) | 51.7 (7.2) | <1.0E-99 |
| Birth weight (kg) a | 3.3 (0.7) | 3.4 (0.6) | 3.70E-07 |
| Townsend Deprivation Index (natural log) a | 2.0 (0.4) | 2.0 (0.4) | 7.60E-03 |
| Time spent outdoors currently (hours/day) a | 3.9 (2.3) | 3.4 (2.2) | <1.0E-99 |
| Age completed full time education (years) a,b | 16.6 (2.1) | 17.1 (2.0) | <1.0E-99 |
| Female gender | 33075 (51.8%) | 15104 (59.8%) | <1.0E-99 |
|
| |||
| Maternal age category c | 4.00E-14 | ||
| <20 | 383 (3.7%) | 888 (3.5%) | |
| 20-24 | 2842 (27.8%) | 7842 (31.0%) | |
| 25-29 | 3987 (38.9%) | 9894 (39.1%) | |
| 30-34 | 2149 (21.0%) | 4955 (19.6%) | |
| 35+ | 879 (8.6%) | 1699 (6.7%) | |
|
| |||
| Birth order c | <1.0E-99 | ||
| First born | 28598 (44.8%) | 13621 (53.9%) | |
| Second born | 19457 (30.5%) | 7583 (30.0%) | |
| Third born | 8432 (13.2%) | 2738 (10.8%) | |
| Fourth or higher born | 7355 (11.5%) | 1336 (5.3%) | |
|
| |||
| Highest educational qualification c | <1.0E-99 | ||
| None | 11375 (17.8%) | 1693 (6.7%) | |
| O-levels, CSEs or equivalent | 16575 (26.0%) | 7496 (29.7%) | |
| A-levels, professional, or equivalent | 14891 (23.3%) | 5708 (22.6%) | |
| Degree | 21001 (32.9%) | 10381 (41.1%) | |
|
| |||
| Refractive error category c | 1.2E-27 | ||
| Non-myopic (>-0.75 D) | 45059 (70.6%) | 16898 (66.8%) | |
| Low/moderate myopia (≤-0.75 D & >-6.00 D) | 16389 (25.7%) | 7231 (28.6%) | |
| High myopia (≤-6.00 D) | 2394 (3.7%) | 1149 (4.5%) | |
Values give the mean ± SD.
Age completed full time education was only asked of individuals who did not report having a college or University degree.
Values give percentage within each sample.
Birth order and myopia
In analyses adjusted for age and sex, the OR for myopia was 1.12 (95% CI 1.08 to 1.16) for first born vs. second born individuals, and this increased to OR=1.38 (95% CI 1.31 to 1.46) for first born vs. fourth-or-higher born individuals. The corresponding ORs obtained after including highest educational qualification were reduced, especially for higher birth orders (Table 2, Model 2). Thus, for first born vs. second born individuals, the OR reduced by 25% from 1.12 to 1.09, while for first born vs. fourth-or-higher born individuals the OR reduced by almost 50% from 1.38 to 1.17.
Table 2. OR for myopia and high myopia in UK biobank participants by birth order after adjusting for highest educational qualification.
| Model 1a |
Model 2b |
|||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| MYOPIA (N=89,120) | ||||||
| First vs. second born | 1.12 | (1.08 to 1.16) | 1.40E-11 | 1.09 | (1.05 to 1.12) | 1.30E-06 |
| First vs. third born | 1.18 | (1.12 to 1.23) | 4.30E-12 | 1.10 | (1.05 to 1.15) | 1.20E-04 |
| First vs. fourth born or higher | 1.38 | (1.31 to 1.46) | 6.00E-34 | 1.17 | (1.11 to 1.23) | 1.70E-08 |
| HIGH MYOPIA (N=65,500 c ) | ||||||
| First vs. second born | 1.21 | (1.11 to 1.30) | 3.60E-06 | 1.15 | (1.06 to 1.25) | 4.60E-04 |
| First vs. third born | 1.29 | (1.15 to 1.44) | 6.40E-06 | 1.16 | (1.04 to 1.30) | 7.90E-03 |
| First vs. fourth born or higher | 1.44 | (1.27 to 1.64) | 1.50E-08 | 1.13 | (1.00 to 1.29) | 5.50E-02 |
Model 1; Adjusted for age and sex only.
Model 2; Adjusted for age, sex and highest educational qualification.
Sample size reduced since participants with mild/moderate myopia were excluded.
Further analyses were carried out in a subset of participants (N=25,278) with data available for a range of potential confounders. In this subset there was a smaller association between birth order and myopia than was observed in the full sample (Model 1 results in Table 2 vs. 3). Adjusting for highest educational qualification attenuated these associations further (Table 3; Model 2), whilst adjusting for maternal age, social deprivation, birth weight, time spent outdoors currently in summer, and highest educational qualification yielded results comparable to the unadjusted analyses (Table 3; Model 3).
Table 3. OR for myopia and high myopia in UK biobank participants by birth order after adjusting for full set of potential confounders.
| Model 1a |
Model 2b |
Model 3c |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | |
| MYOPIA (N=25,278) | |||||||||
| First vs. second born | 1.10 | (1.04 to 1.17) | 1.70E-03 | 1.08 | (1.01 to 1.15) | 1.60E-02 | 1.14 | (1.07 to 1.21) | 6.10E-05 |
| First vs. third born | 1.09 | (1.00 to 1.19) | 6.00E-02 | 1.04 | (0.95 to 1.14) | 3.60E-01 | 1.15 | (1.05 to 1.27) | 3.20E-03 |
| First vs. fourth born or higher | 1.16 | (1.02 to 1.30) | 1.90E-02 | 1.02 | (0.90 to 1.15) | 7.50E-01 | 1.17 | (1.03 to 1.34) | 1.80E-02 |
| HIGH MYOPIA (N=18,047 d ) | |||||||||
| First vs. second born | 1.18 | (1.03 to 1.36) | 2.10E-02 | 1.14 | (0.99 to 1.31) | 7.30E-02 | 1.23 | (1.06 to 1.43) | 5.10E-03 |
| First vs. third born | 1.18 | (0.96 to 1.44) | 1.20E-01 | 1.11 | (0.90 to 1.36) | 3.30E-01 | 1.29 | (1.04 to 1.60) | 2.20E-02 |
| First vs. fourth born or higher | 0.93 | (0.72 to 1.19) | 5.50E-01 | 0.77 | (0.60 to 1.00) | 4.70E-02 | 0.95 | (0.73 to 1.25) | 7.40E-01 |
Model 1; Adjusted for age and sex only.
Model 2; Adjusted for age, sex and highest educational qualification.
Model 3; Adjusted for age, sex, highest educational qualification, Townsend Deprivation Index, current time spent outdoors, birth weight and maternal age.
Sample size reduced since participants with mild/moderate myopia were excluded.
The suggestion of a dose-response relationship between birth order and myopia, whereby myopia risk decreased with umber of older siblings, was substantially weakened or lost completely after adjusting for highest educational attainment (Model 1 vs. Models 2 or 3) both for the full set of participants (Table 2) and the subset with full information (Table 3).
Birth order and high myopia
The relationship between birth order and high myopia (Tables 2 for full sample & Table 3 for subset) shared several of the features of its relationship with myopia. In the full sample after adjusting for age and sex (Model 1) there was evidence for a relationship between high myopia and birth order with OR =1.21 (95% CI 1.11 to 1.30; N=65,500) for first vs. second born individuals. However, there was no suggestion of a dose-response relationship between birth order and high myopia, either before or after adjustment for education.
Birth order and refractive error
After adjusting for age and sex, there was evidence suggesting a dose-response relationship between later birth order and a more positive (residual) refractive error, which was again much reduced after adjusting for highest educational attainment (eFigure 1 in the Supplement).
Adjusting for age completed full-time education
Highest educational qualification may not capture all aspects of the myopia-predisposing influence of education, such as the amount of near work undertaken. Therefore, we also carried out analyses adjusted for age completed full-time education (N=57,447; Table 4). In keeping with our previous analyses, using this measure of educational exposure led to a 31% attenuation of the association between birth order and myopia (prior to adjustment, OR=1.13; after adjustment, OR=1.09), and eliminated all evidence of a dose-response relationship (Table 4). In the case of birth order vs. high myopia, adjusting for age completed full-time education also yielded results that were very similar to those observed when adjusting for highest educational qualification.
Table 4. OR for myopia and high myopia by birth order, after adjusting for age completed full-time education.
| Model 1a |
Model 4b |
|||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| MYOPIA (N=57,447) | ||||||
| First vs. second born | 1.13 | (1.08 to 1.18) | 1.00E-07 | 1.09 | (1.04 to 1.14) | 1.50E-04 |
| First vs. third born | 1.19 | (1.12 to 1.27) | 8.60E-09 | 1.11 | (1.04 to 1.18) | 8.40E-04 |
| First vs. fourth born or higher | 1.31 | (1.22 to 1.39) | 3.50E-16 | 1.14 | (1.07 to 1.22) | 6.90E-05 |
| HIGH MYOPIA (N=44,473 c ) | ||||||
| First vs. second born | 1.21 | (1.08 to 1.36) | 1.60E-03 | 1.15 | (1.03 to 1.30) | 1.80E-02 |
| First vs. third born | 1.22 | (1.04 to 1.43) | 1.40E-02 | 1.10 | (0.93 to 1.29) | 2.60E-01 |
| First vs. fourth born or higher | 1.24 | (1.05 to 1.47) | 1.00E-02 | 1.02 | (0.86 to 1.20) | 8.40E-01 |
Model 1; Adjusted for age and sex only.
Model 2; Adjusted for age, sex and age completed full-time education.
Sample size reduced since participants with mild/moderate myopia were excluded.
Family size
To investigate whether the association between birth order and myopia could be a feature of a more general underlying association between family size and myopia, we repeated our analyses using a statistical approach to control for family size,13,14 namely including only families containing 2 children. There were 30,727 participants who had only1 sibling (54% first born; 46% second born, compared to the 50-50% proportions expected under random ascertainment). Adjusting for age and sex yielded an OR for myopia in first-born vs. second-born individuals of OR=1.12 (95% CI 1.06 to 1.17; P=1.0E-05) while adjusting for age, sex, and highest educational qualification yielded an OR for myopia of OR=1.08 (95% CI 1.03 to 1.13; P=2.1E-03). These estimates were close to those for the full sample (Table 2) suggesting that they were not driven by family size per se.
Exclusion of only-children
A proportion of first born children will be “only-children”, i.e. individuals with no brothers or sisters. As shown in eTable 4 in the Supplement, repeating our analyses after excluding only-children had very little effect, thus confirming that only-children were not driving the associations.
Risk ratios vs. odds ratios
The prevalence of myopia in the UK Biobank sample was ~30% (Table 1). For such a highly prevalent condition, an odds ratio will accentuate the true relative risk (RR); for example, ORs of 1.10 and 1.20 would correspond to RRs of 1.07 and 1.13, respectively16. For high myopia (prevalence ~4% in UK Biobank participants) the corresponding RRs would be 1.10 and 1.19. The (unadjusted) relative risk of myopia and high myopia in first born vs. later born individuals are shown in eTables 5 and 6 of the Supplement.
Discussion
We observed strong evidence that first born individuals were more often myopic than non-first born UK Biobank participants, confirming previous findings8,10. The magnitude of this association was small: first born participants were ~10% more likely to be myopic than non-first born participants, which equated to first born individuals having a refractive error that was less than −0.25 D more negative, on average, than non-first-born participants. Much larger shifts towards a more negative refractive error have been observed in East and Southeast Asia over the past few decades, implicating additional environmental influences over those assessed in these analyses.
The results did not support the idea that the association between birth order and myopia arose through confounding via the participant demographic-related effects, age, sex and socio-economic status, nor the maternal/birth-related effects, maternal age and birth weight. In contrast, there was evidence of confounding due to educational exposure. After adjusting for either of two measures of educational exposure – highest educational qualification or age completed full-time education – the association between birth order and myopia was attenuated and no dose-response relationship was evident. Morgan12 suggested that such confounding was a plausible cause of the association between birth order and myopia based on reports that after controlling for family size children with an earlier birth order do relatively better at school, due to parents investing more time, effort and/or resources in educating children with an earlier birth order13,14. Greater educational exposure in earlier-born children may expose them to a more myopiagenic environment; for example, more time doing nearwork, and less time spent outdoors12. Our findings that statistical adjustment for indices of educational exposure partially attenuated the magnitude of the association between birth order and myopia, and completely removed the evidence for a dose-response relationship, therefore support the idea that reduced parental investment in children’s education for offspring of later birth order contributed to the observed birth order vs. myopia association and produced the observed dose-response relationship. However, since the increased risk of myopia in first-born vs. non-first-born individuals was reduced but not abolished, either the statistical adjustment failed to adequately capture the true relationship fully, or other unmeasured factor(s) contributed to the higher prevalence of myopia in first-born vs. non-first-born individuals. These results add to the extensive literature17-20 implicating a role for education in the etiology of myopia, although a causal relationship cannot be confirmed using observational data.
The association between birth order and high myopia was similar in magnitude to that between birth order and any myopia, and also was reduced by adjusting for educational exposure. This implies a role for environment, i.e. education, in the etiology of high myopia as well as myopia.
Surprisingly, the magnitude of the association between birth order and myopia appeared weaker in the subset with full data than the full sample (compare Model 1 in Table 2 vs. 3), especially as regards the dose-response relationship. A comparison of demographic characteristics between those with complete or incomplete information for potential confounders highlighted many differences, including age, sex and highest educational attainment (Table 1). The lack of uniformity of the association in two subgroups of the sample argues against a biological factor such as a parity-related maternal effect during pregnancy being fully responsible for causing the association between birth order and myopia.
Strengths of this study were highly standardised methods of data collection, a large sample size, use of an objective and reliable method of quantifying refractive error in this age group, participant selection not being directly aimed at ocular health (thus reducing selection bias) and availability of information on a range of potential confounders. Weaknesses were using self-report to exclude participants with cataracts and the wide age range of the sample which increased the risk of bias due to confounding between myopia and changing demographic variables. The 2 measures of education that were available may not have captured all relevant aspects of the educational process. Additionally, the participants were not selected at random from the population and had non-random variations in levels of missing information for covariates (Table 1); therefore the results may not be fully representative of the general population. Finally, information on the time UK Biobank participants spent outdoors during childhood was not collected, and therefore any potential role of this important exposure in mediating the association of birth order and myopia could not be investigated.
In conclusion, first-born individuals in a sample of UK adults were ~10% more likely to be myopic or highly myopic than later-born individuals. The results replicate earlier findings from two contemporary international cohorts of adolescents/young adults10, implying that the cause of the birth order-myopia association is widespread and has been in existence for several decades. The association was larger before adjusting for educational exposure, suggesting that reduced parental investment in the education of children of later birth order may be partly responsible.
Supplementary Material
Acknowledgements
This research has been conducted using the UK Biobank Resource (https://www.ukbiobank.ac.uk/). The authors acknowledge the members of the UK Biobank Eye and Vision Consortium (http://www.ukbiobankeyeconsortium.org.uk).
Funding/Support: The work was funded by a NIHR Career Development Fellowship CDF-2009-02-35 (CW) and an internal award Z0GM from the Hong Kong Polytechnic University (JAG). The funding bodies had no role in: the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; decision to submit the manuscript for publication.
Footnotes
Conflicts of interest: None of the authors has any conflict of interest relevant to this work, including relevant financial interests, activities, relationships, or affiliations.
References
- 1.Foster PJ, Jiang Y. Epidemiology of myopia. Eye. 2014;28:202–208. doi: 10.1038/eye.2013.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flitcroft DI. Emmetropisation and the aetiology of refractive errors. Eye. 2014;28:169–179. doi: 10.1038/eye.2013.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379(9827):1739–1748. doi: 10.1016/S0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 4.Hysi PG, Wojciechowski R, Rahi JS, Hammond CJ. Genome-wide association studies of refractive error and myopia, lessons learned, and implications for the future. Invest Ophthalmol Vis Sci. 2014;55(5):3344–3351. doi: 10.1167/iovs.14-14149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones-Jordan LA, Mitchell GL, Cotter SA, et al. Visual activity prior to and following the onset of juvenile myopia. Invest Ophthalmol Vis Sci. 2011;52:1841–1850. doi: 10.1167/iovs.09-4997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guggenheim JA, Northstone K, McMahon G, et al. Time outdoors and physical activity as predictors of incident myopia in childhood: A prospective cohort study. Invest Ophthalmol Vis Sci. 2012;53:2856–2865. doi: 10.1167/iovs.11-9091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahi JS, Cumberland PM, Peckham CS. Myopia over the lifecourse: Prevalence and early life influences in the 1958 British Birth Cohort. Ophthalmol. 2011;118(5):797–804. doi: 10.1016/j.ophtha.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 8.Rudnicka AR, Owen CG, Richards M, Wadsworth ME, Strachan DP. Effect of breastfeeding and sociodemographic factors on visual outcome in childhood and adolescence. Am J Clin Nutr. 2008;87(5):1392–1399. doi: 10.1093/ajcn/87.5.1392. [DOI] [PubMed] [Google Scholar]
- 9.Mandel Y, Grotto I, El-Yaniv R, et al. Season of birth, natural light, and myopia. Ophthalmol. 2008;115(4):686–692. doi: 10.1016/j.ophtha.2007.05.040. [DOI] [PubMed] [Google Scholar]
- 10.Guggenheim JA, McMahon G, Northstone K, et al. Birth order and myopia. Ophthalmic Epidemiol. 2013;20(6):375–384. doi: 10.3109/09286586.2013.848457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stone RA, Wilson LB, Ying GS, et al. Associations between childhood refraction and parental smoking. Invest Ophthalmol Vis Sci. 2006;47(10):4277–4287. doi: 10.1167/iovs.05-1625. [DOI] [PubMed] [Google Scholar]
- 12.Morgan IG, Cotch MF. Birth order and myopia: What are the messages to readers? Ophthalmic Epidemiol. 2013;20(6):333–334. doi: 10.3109/09286586.2013.860994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Booth A, Kee H. Birth order matters: the effect of family size and birth order on educational attainment. J Popul Econ. 2009;22(2):367–397. [Google Scholar]
- 14.Fergusson DM, Horwood LJ, Boden JM. Birth order and educational achievement in adolescence and young adulthood. Austral J Educ. 2006;50(2):122–139. [Google Scholar]
- 15.Allen N, Sudlow C, Downey P, et al. UK Biobank: Current status and what it means for epidemiology. Health Policy and Technology. 2012;1(3):123–126. [Google Scholar]
- 16.Grant RL. Converting an odds ratio to a range of plausible relative risks for better communication of research findings. BMJ. 2014;348:f7450. doi: 10.1136/bmj.f7450. [DOI] [PubMed] [Google Scholar]
- 17.Rosner M, Belkin M. Intelligence, education and myopia in males. Arch Ophthalmol. 1987;105:1508–1511. doi: 10.1001/archopht.1987.01060110054030. [DOI] [PubMed] [Google Scholar]
- 18.Tay MT, Au Eong KG, Ng CY, Lim MK. Myopia and educational attainment in 421,116 young Singaporean males. Ann Acad Med Singapore. 1992;21:785–791. [PubMed] [Google Scholar]
- 19.Verhoeven VJ, Buitendijk GH, Rivadeneira F, et al. Education influences the role of genetics in myopia. Eur J Epidemiol. 2013;28(12):973–980. doi: 10.1007/s10654-013-9856-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morgan IG, Rose KA. Myopia and international educational performance. Ophthalmic Physiol Opt. 2013;33(3):329–338. doi: 10.1111/opo.12040. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.