Abstract
Nevus sebaceus of Jadassohn is a congenital cutaneous hamartoma comprising of multiple skin structures. It has the potential to develop into variety of neoplasms of various epidermal adnexal origins. While multiple tumors may occasionally arise, it is unusual to develop two different types of tumor, benign and malignant, to arise simultaneously within a single sebaceus nevus. Here in, we report a case of a 27-year-old male with two neoplastic proliferations including a syringocystadenoma papilliferum a benign tumor and basal cell carcinoma a malignant tumor arising in a long-standing nevus sebaceus on the face. Neoplastic changes are common in nevus sebaceous present on scalp but our case is unique due to the presence of two different types of neoplasm in a nevus sebaceous which was present on face.
Keywords: Basal cell carcinoma, nevus sebaceus of Jadassohn, syringocystadenoma papilliferum
What was known?
Sebaceous nevi are uncommon congenital skin lesions with a well-recognized potential for neoplastic change.
Introduction
Nevus sebaceous is uncommon hamartomatous lesions occurring in 0.3% of neonates.[1] They were first described by Jadassohn in 1895 and are most commonly seen on the head and neck whilst similar lesions elsewhere on the body are termed verrucous epidermal nevi.[2,3] Usually recognized at birth or in early childhood, sebaceous nevi remain small and hairless until puberty when they may become larger and verrucous. In late adult life they have a well-documented neoplastic potential. Such changes are rarely seen in childhood. We report a patient with nevus sebaceous with one benign and one malignant tumor simultaneously occurring in a single lesion- syringocystadenoma papilliferum and basal cell carcinoma on face.
Case Report
A 27-year-old male came to the department of dermatology with a lesion on the left cheek that had been present since birth. In the preceding 2 months he had noticed a change in the lesion. On close inspection he had a linear lesion on the left cheek that measured 5 cm in length with a maximum width of 3 cm. This was a well-defined brownish, plaque with a rough surface [Figure 1]. Past medical history and general physical examination were unremarkable. Under local infiltration of xylocain 2% with adrenalin the lesion was excised as an ellipse with a 2 mm clearance margin and the wound closed primarily. Sections were stained with hematoxylin and eosin and examined with a light microscope. On histology epidermis revealed hyperkeratosis, hyperplasia, mild koilocytosis, papillomatosis and focal invagination in dermis lined by squamous cells. Dermis revealed mature sebaceous glands, few hair follicles and sweat glands. The invaginating epidermis into the dermis forms a cyst with numerous papillary projections [Figure 2]. The cross sections of these papillae were lined by two layers—a luminal columnar epithelium with evidence of decapitation secretions and outer flattened cuboidal epithelium. Abundant plasma cells were present in the stromal core of papillae. Careful examination showed a cluster of basaloid cells with peripheral pallisading of lesional cell nuclei [Figure 3]. Brownish pigment melanin was also seen in few of these basaloid cells. On the basis of these pathological findings a diagnosis of nevus sebaceous with foci of basal cell carcinoma and syringocystadenoma papilliferum was made.
Figure 1.
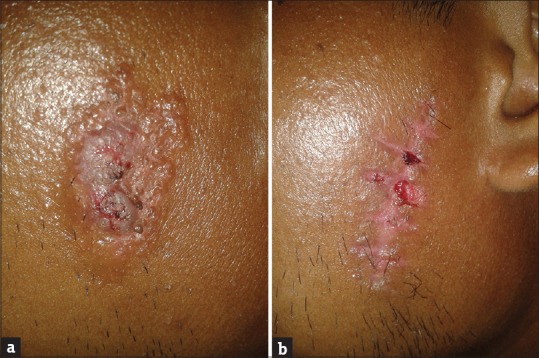
(a) Lesion of nevus sebaceous of Jadassohn on the left side of the face. (b) Scar of the lesion after 10 days of complete excision
Figure 2.
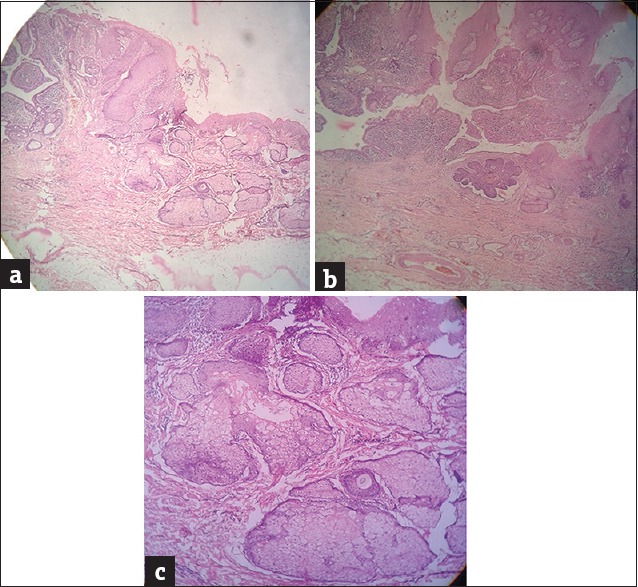
(a) H and E stain scanner view ×4 showing nevus sebaceous and syringocystadenoma papilliferum. (b) H and E stain scanner ×4 view showing basal cell carcinoma and Syringocystadenoma papilliferum. (c) H and E stain, low power ×10 view showing dermis having mature sebaceous glands and a hair follicle
Figure 3.
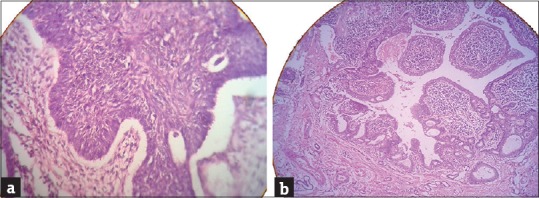
(a) H and E Stain High power ×40 view showing cluster of basaloid cells with peripheral pallisading of lesional cell nuclei and clefting artifact between the epithelium and stroma. (b) H and E stain, low power ×10 view showing dermal cysts with numerous papillary projections lined by two layers of a luminal columnar epithelium with evidence of decapitation secretion and outer flattened cuboidal epithelium
Discussion
Sebaceous nevi are uncommon hamartomatous lesions seen in 0.3% of neonates and 0.68% of skin biopsy specimens.[1,2,3,4,5] Up to 95% occurs on the scalp and face.[3,6]
In 1965, Mehregan and Pinkus described the natural history of the lesion in three stages.[6] In the infantile stage, the lesion presents as a characteristic quiescent yellow plaque. Histologically, there is a paucity of underdeveloped sebaceous glands and hair follicles. At the pubertal stage, growth of the lesion is accelerated and it becomes verrucous. Light microscopy shows masses of hypertrophic sebaceous glands with papillomatosis and hyperkeratosis of the overlying epidermis.
The third or neoplastic stage sees the development of secondary tumors and usually occurs in late adult life. The clinical signs suggesting neoplastic transformation include rapid enlargement or the development of nodularity or ulceration. Several different tumors of epidermal, adnexal and mesenchymal origin are known to arise. Benign tumors are the most common including syringocystadenoma papilliferum, apocrine cystadenoma, trichoblastoma, trichilemmal cysts and keratoacanthoma. Occasionally, multiple tumors are observed within a pre-existing lesion.[6] Malignant degeneration, although less common, occurs with a lifetime risk of between 5% and 20%.[7,8,9] The majority of these tumors are basal cell carcinomas but squamous cell, sebaceous and apocrine carcinomas are also recognized. Most are of low-grade malignancy but more aggressive histological features and metastases are occasionally seen. It has been suggested that these tumors may arise from pluripotential epithelial germ cells as a result of dedifferentiation of sebaceous nevus cells, the nature of the tumor depending upon the degree of subsequent differentiation.[10]
Syringocystadenoma papilliferum is one of the most common benign tumor associated with nevus sebaceous.[11] The histological changes are characterized by the papillomatous hyperplasia of the epidermis to different degrees. There are many irregular ducts like structures and cystic spaces lined with a double-layered epithelium.[12]
Basal cell carcinoma is the most common malignant neoplasm associated with nevus sebaceous, which derives from original epithelial germ cells. It is composed of stroma-dependent multipotent basaloid cells and differentiates toward the epidermis or adnexa. It has the same origin as the nevus sebaceous and has the characteristic of multidifferentiation of the skin stem cells, although many researchers have shown that those lesions were mostly trichoblastomas misinterpreted as basal cell carcinoma.[13]
There is little evidence in the literature upon which to base clinical guidelines on the management of sebaceous nevus, regarding either the age at which intervention should be planned or the best modality of treatment. The two main options are excision with primary reconstruction and histological examination around the time of puberty and the more conservative approach of excision if clinical signs of malignant transformation occur. An alternative is dermabrasion or dermablation with diathermy or laser but this does not provide tissue for histological examination and occult basal cell carcinoma has been found in lesions with no evidence of transformation either clinically or on incisional biopsy.[14] Mehregan and Pinkus go further and hypothesize that superficial destruction of the lesion may provoke cellular transformation.[6]
In our case the lesion was excised as an ellipse with a 2 mm clear margin and primary closer was done. The patient was advised to come for regular follow up at 1 month interval.
What is new?
Sebaceous nevi can change into tumor in a lifetime but appearance of two different type of tumor like one benign and one malignant tumor in a single nevus is rarest of one. Surgical excision of nevus with a safe margin should be done in all cases of sebaceous nevi.
Acknowledgement
Special thanks to Dr. Rashmi Gupta, consultant.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Alper J, Holmes L. The Incidence and significance of birthmarks in a cohort of 4641 new-borns. Pediatr Dermatol. 1983;1:58–66. doi: 10.1111/j.1525-1470.1983.tb01093.x. [DOI] [PubMed] [Google Scholar]
- 2.Jadassohn J. Bemerkungen zur Histologie der systematisirten Naevi und ueber ‘Talgdruesen-naevi’. Arch Dermatol Symp. 1895;33:355. [Google Scholar]
- 3.Rook A. Naevi and other developmental defects. In: Rook A, Ebling FJG, Wilkinson OS, editors. Textbook of Dermatology. 4th ed. London: Blackwell Scientific Publications; 1986. pp. 174–6. [Google Scholar]
- 4.Solomon L, Fretzin D, Dewald R. The epidermal naevus syndrome. Arch Dermatol. 1968;97:273–85. [PubMed] [Google Scholar]
- 5.Wilson-Jones E, Heyl T. Naevus sebaceous – a report of 140 cases. Br J Dermatol. 1970;82:99–117. doi: 10.1111/j.1365-2133.1970.tb15000.x. [DOI] [PubMed] [Google Scholar]
- 6.Mehregan A, Pinkus H. Life history of organised nevi. Arch Dermatol. 1965;91:574–88. doi: 10.1001/archderm.1965.01600120006002. [DOI] [PubMed] [Google Scholar]
- 7.Chun K, Vazquez M, Sanchez JL. Naevus sebaceous: Clinical outcome and consideration for prophylactic excision. Int J Dermatol. 1995;34:538–41. doi: 10.1111/j.1365-4362.1995.tb02948.x. [DOI] [PubMed] [Google Scholar]
- 8.Piansay-Soriano EF, Pineda VB, Jimenez RI, Mungcal VC. Basal cell carcinoma and infundibuloma arising in separate sebaceous naevi in childhood. J Dermatol Surg Oncol. 1989;15:1283–6. doi: 10.1111/j.1524-4725.1989.tb03148.x. [DOI] [PubMed] [Google Scholar]
- 9.Sasson M, Mallory SB. Malignant primary skin tumours in children. Current Opinion in Paediatrics. 1996;8:372–7. doi: 10.1097/00008480-199608000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Lever W, Schaumburg G. Tumours of the epidermal appendages. In: Lever W, Schaumburg G, editors. Histopathology of the skin. 7th ed. Philadelphia: Lippincott; 1990. pp. 594–6. [Google Scholar]
- 11.Saha A, Das NK, Gharami RC, Chowdhury SN, Datta PK. A clinico-histopathological study of appendageal skin tumors, affecting head and neck region in patients attending the dermatology OPD of a tertiary care centre in Eastern India. Indian J Dermatol. 2011;56:33–6. doi: 10.4103/0019-5154.77548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castilla EA, Bergfeld WF, Ormsby A. Trichilemmoma and syringocystadenoma papilliferum arising in nevus sebaceous. Pathology. 2002;34:196–7. doi: 10.1080/003130201201117000. [DOI] [PubMed] [Google Scholar]
- 13.Cribier B, Scrivener Y, Grosshans E. Tumours arising in nevus sebaceous: A study of 596 cases. J Am Acad Dermatol. 2000;2:263–8. doi: 10.1016/S0190-9622(00)90136-1. [DOI] [PubMed] [Google Scholar]
- 14.Goldstein GD, Whitaker DC, Argenyi Z, Bardach J. Basal cell carcinoma arising in a sebaceous naevus during childhood. J Am Acad Dermatol. 1988;18:429–40. doi: 10.1016/s0190-9622(88)70063-8. [DOI] [PubMed] [Google Scholar]


