Abstract
To investigate whether aberrant interactions between brain structure and function present similarly or differently across probands with psychotic illnesses [schizophrenia (SZ), schizoaffective disorder (SAD), and bipolar I disorder with psychosis (BP)] and whether these deficits are shared with their first-degree non-psychotic relatives. A total of 1199 subjects were assessed, including 220 SZ, 147 SAD, 180 psychotic BP, 150 first-degree relatives of SZ, 126 SAD relatives, 134 BP relatives, and 242 healthy controls (1). All subjects underwent structural MRI (sMRI) and resting-state functional MRI (rs-fMRI) scanning. Joint-independent component analysis (jICA) was used to fuse sMRI gray matter and rs-fMRI amplitude of low-frequency fluctuations data to identify the relationship between the two modalities. jICA revealed two significantly fused components. The association between functional brain alteration in a prefrontal–striatal–thalamic–cerebellar network and structural abnormalities in the default mode network was found to be common across psychotic diagnoses and correlated with cognitive function, social function, and schizo-bipolar scale scores. The fused alteration in the temporal lobe was unique to SZ and SAD. The above effects were not seen in any relative group (including those with cluster-A personality). Using a multivariate-fused approach involving two widely used imaging markers, we demonstrate both shared and distinct biological traits across the psychosis spectrum. Furthermore, our results suggest that the above traits are psychosis biomarkers rather than endophenotypes.
Keywords: schizophrenia, schizoaffective, bipolar, relatives, multimodal neuroimaging, joint-independent component analysis
Introduction
Whether schizophrenia (SZ), schizoaffective disorder (SAD), and psychotic bipolar disorder are distinct illnesses or represent a continuum continues to be debated (2–4). There is overlap among clinical symptoms (5), cognitive functional deficits (6), and disease risk genes (7) among these disorders (8) that challenge traditional diagnostic categories. Clarifying similarities and differences in anatomical and functional deficits among psychotic probands may contribute to the better understanding of the mechanisms underlying psychotic disorders. The above disorders are highly heritable (9, 10), and illness-related genes associated with the abnormalities in brain structure and function (11) may also be present in their unaffected relatives. Thus, shared abnormalities between probands and unaffected relatives can serve as endophenotypes, which may provide biological genetic substrates for improved diagnostic classification (12), and ultimately may lead to better, more focused treatments.
Psychotic illnesses are widely assumed to be brain disorders characterized by distributed cerebral dysconnectivity across large-scale neural networks. Resting-state networks reflect correlated spontaneous fluctuations in brain regional activity at rest (13) and show a similar correspondence to task-related networks that control brain action and cognition (14). A recent resting-state functional MRI (rs-fMRI) study reported that SZ, SAD, and psychotic bipolar disorder share disruptions within the fronto-parietal control network (7). Both default mode network (DMN) and prefrontal–thalamic–cerebellar network connectivity have been reported to be abnormal in probands with SZ and bipolar disorder (15, 16) and between probands and relatives with SZ (17–19). Lui et al. (20) compared resting-state functional network connectivity between SZ and psychotic bipolar probands and their unaffected first-degree relatives and found probands with SZ and psychotic bipolar shared deficits in striatal–thalamic–cortical network as well as bipolar relatives. Independent structural MRI (sMRI) studies reveal both common and unique regional gray matter (GM) abnormalities across psychotic probands (21–24). Ivleva et al. (24) reported that SZ, SAD, psychotic bipolar disorder probands, and their relatives with psychosis showed overlapping GM deficits throughout the neocortex as a psychosis endophenotype. Collectively, overlaps and differences in both functional and structural networks across psychosis probands and their relatives have been identified, but no studies to date have examined both structural and functional deficits together. Brain regions are highly interconnected and local changes in brain structure may result in altered brain activity in distant regions (25, 26). Inter-regional correlations of GM volume may reflect changed inter-regional functional connectivity (27). Thus, examining abnormalities in structure and function together may help better characterize illness-related features and provide more information than each measure independently.
Joint-independent component analysis (jICA), a data-driven feature-based approach, enables joint analysis of different data types, for example, relationships between brain function and structure (28). In the present study, we utilized two commonly employed techniques to quantify anatomy and function. Anatomical data were indexed by GM volumes obtained through voxel-based morphometry (VBM), while resting-state function was measured using amplitude of low-frequency fluctuations (ALFF) (0.01–0.08 Hz) of the blood oxygen level dependent. ALFF measures, particularly in the 0.01–0.08 Hz frequency range have been demonstrated to be physiologically relevant and related to neuronal fluctuations in brain GM in resting state (29, 30). In the current study, we utilized the joint approach to integrate GM and ALFF, to investigate joint structure–function anomalies across the SZ-psychotic bipolar disorder spectrum using data from the large-scale multi-site bipolar-schizophrenia network on intermediate phenotypes (B-SNIP) psychosis study (31). Our aims were to (1) detect whether aberrancies detected by fusing rs-fMRI and sMRI would be specific to SZ, SAD, or bipolar I disorder with psychosis (BP) or shared by these psychotic disorders relative to healthy controls; (2) investigate whether these abnormalities across two modalities would be shared by probands and their non-psychotic relatives, suggesting that they may represent endophenotypes across the psychosis dimension.
Materials and Methods
Participants
A total of 1199 subjects (passing quality control) were used for the current analysis. Subjects were drawn from the B-SNIP study from six sites, including 220 SZ, 180 psychotic BP, 147 SAD, 150 first-degree relatives of SZ, 134 first-degree relatives of psychotic BP, 126 first-degree relatives of SAD, and 242 healthy controls. The details of characteristics of the B-SNIP clinical population are described in Ref. (31). All participants provided written informed consent approved separately by institutional review boards of individual sites after a complete explanation of the study. All probands and relatives were diagnosed using the Structured Clinical Interview for DSM-IV Axis I Disorder, Patient Edition (SCID-I/P) (32). Relatives were also diagnosed with the structured interview for DSM-IV personality (SIDP-IV) (33) for axis-II diagnoses. Relatives meeting the criteria for axis I proband-like psychotic disorders (N = 64) were classified to the corresponding proband groups and those with no axis I or no lifetime psychotic diagnoses were included in the non-psychotic relative groups. In addition, relatives without a psychotic disorder were administered the SIDP-IV (34) and were considered to have elevated psychosis spectrum personality traits if meeting full or within one criteria of Cluster-A (psychosis spectrum; N = 63) Axis-II diagnosis. Healthy controls were evaluated using the SCID Non-Patient Edition to confirm lifetime absence of Axis I illness or a family history of SZ-bipolar spectrum disorders. All probands were assessed with positive and negative syndrome scale (PANSS) (35), Montgomery–Åsberg depression rating scale (MADRS) (36), Young Mania Rating Scale (YMRS) (37), and schizo-bipolar scale (SBS) (5). Additionally, all subjects were assessed with brief assessment of cognition in schizophrenia (BACS) (38) and the Birchwood social functioning scale (SFS) (39).
The demographic and clinical characteristics of study sample are outlined in Table 1, and details are described in the previous B-SNIP papers (24, 31). Medication data are listed in Table S2 in Supplementary Material.
Table 1.
Demographic and clinical characteristics of the study sample.
| Variablea | Schizophrenia probands (n =220) | Schizoaffective disorder probands (n =147) | Psychotic bipolar probands (n =180) | Relatives of schizophrenia (n =150) | Relatives of schizoaffective disorder (n =126) | Relatives of psychotic bipolar (n =134) | Healthy controls (n =242) | Statisticc | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | χ2 | p | |
| Male gender | 145 | 65.91 | 66 | 44.90 | 58 | 32.22 | 49 | 32.67 | 40 | 31.75 | 49 | 36.57 | 103 | 42.56 | 71.27 | 2 × 10−13 |
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | F | p | |
| Age (years) | 35.15 | 12.31 | 35.08 | 12.01 | 36.94 | 13.04 | 43.33 | 15.55 | 41.01 | 16.14 | 40.59 | 16.13 | 38.14 | 12.65 | 7.72 | 4 × 10−8 |
| PANSS | ||||||||||||||||
| Positive | 16.91 | 5.42 | 18.12 | 5.32 | 12.77 | 4.38 | – | – | – | – | – | – | – | – | 50.47 | 1 × 10−22 |
| Negative | 16.27 | 5.93 | 15.49 | 4.95 | 11.79 | 3.61 | – | – | – | – | – | – | – | – | 40.96 | 3 × 10−17 |
| General | 32.02 | 8.72 | 34.80 | 9.00 | 28.60 | 8.04 | – | – | – | – | – | – | – | – | 20.57 | 3 × 10−9 |
| Total | 65.20 | 16.78 | 68.41 | 16.28 | 53.17 | 13.48 | – | – | – | – | – | – | – | – | 43.74 | 3 × 10−18 |
| MADRS | 8.90 | 7.93 | 14.31 | 10.26 | 10.51 | 8.99 | – | – | – | – | – | – | – | – | 15.76 | 2 × 10−7 |
| YMRS | 5.76 | 5.79 | 7.69 | 6.48 | 5.69 | 6.46 | – | – | – | – | – | – | – | – | 5.22 | 0.006 |
| SBS | 7.79 | 1.36 | 5.01 | 1.60 | 1.35 | 1.24 | – | – | – | – | – | – | – | – | 1006.21 | 2 × 10−178 |
| BACSb (z) | ||||||||||||||||
| Verbal memory | −1.14 | 1.32 | −1.04 | 1.39 | −0.44 | 1.28 | −0.08 | 1.09 | −0.46 | 1.26 | −0.13 | 1.07 | −0.04 | 1.08 | 23.13 | 8 × 10−26 |
| Token motor | −1.33 | 1.18 | −1.36 | 1.17 | −0.95 | 1.24 | −0.33 | 1.16 | −0.24 | 1.03 | −0.31 | 1.07 | 0.02 | 1.12 | 39.24 | 3 × 10−43 |
| Digit sequencing | −1.26 | 1.20 | −0.94 | 1.28 | −0.51 | 1.11 | −0.38 | 1.14 | -0.27 | 1.15 | −0.03 | 1.11 | −0.06 | 1.12 | 26.71 | 8 × 10−30 |
| Verbal fluency | −0.76 | 1.15 | −0.50 | 1.27 | −0.20 | 1.23 | −0.93 | 1.08 | 0.02 | 1.20 | 0.07 | 1.07 | 0.14 | 1.05 | 14.20 | 1 × 10−15 |
| Symbol coding | −1.41 | 1.10 | −1.37 | 1.18 | −0.87 | 1.01 | −0.37 | 1.08 | −0.39 | 1.10 | −0.07 | 1.04 | −0.00 | 1.01 | 49.42 | 1 × 10−53 |
| Tower of London | −0.87 | 1.39 | −0.70 | 1.30 | −0.28 | 1.10 | −0.19 | 1.08 | −0.18 | 1.27 | 0.11 | 0.85 | 0.02 | 1.17 | 15.80 | 2 × 10−17 |
| Composite score | −1.79 | 1.34 | −1.54 | 1.37 | −0.87 | 1.24 | −0.38 | 1.19 | −0.40 | 1.25 | −0.09 | 1.11 | 0.02 | 1.17 | 54.99 | 3 × 10−59 |
| SFS | 123.27 | 23.13 | 119.28 | 24.42 | 134.10 | 22.77 | 151.03 | 18.23 | 144.64 | 21.89 | 151.42 | 21.60 | 156.09 | 15.94 | 68.31 | 2 × 10−70 |
aPANSS, positive and negative syndrome scale; MRADS, Montgomery–Åsberg depression rating scale; YMRS, Young Mania Rating Scale; SBS, schizo-bipolar scale; BACS, brief assessment of cognition in schizophrenia; SFS, Birchwood social functioning scale.
bz-Scores are calculated using the overall means and standard deviations of all healthy controls and corrected with age and sex.
cPost hoc statistic are presented as follows: age: SADR, SZR > HC; SZR, BPR, SADR > BP; HC, BPR, SADR, SZR > SZ; BPR, SADR, SZR > SAD. PANSS_Positive: SZ > BP; SAD > SZ, BP; PANSS_Negative: SZ > BP, SAD; SAD > BP; PANSS General: SAD > SZ > BP. MADRS: BP > HC; SZ > HC; SAD > all groups. YMRS: BP > HC; SZ > HC; SAD > all groups. SBS: SZ > BP, SAD; SAD > BP. BACS Verbal memory: BP > SZ, SAD; HC > SZ, SAD, BP; SADR > BP; SZR, BPR, HC > SADR; BACS token motor: BP > SZ, SAD; HC > SZ, SAD, BP; HC, SADR > SZR, BPR; BACS digit sequencing: BP > SAD > SZ; HC > SZ, SAD, BP, SZR; BACS verbal fluency: BP > SAD > SZ; HC > SZ, SAD, BP; BACS symbol coding: BP > SZ, SAD; HC > SZ, SAD, BP, SZR, SDAR; BACS tower of London: BP > SZ, SAD; HC > SZ, SAD, BP; BACS composite Score: BP > SZ, SAD; HC > SZ, SAD, BP; SADR > BP; SZR, BPR, HC > SADR.SFS: BP, SZR, BPR, SADR, HC > SZ, SAD; BP > SAD, SZ; SZR, BPR, SADR, HC > BP; SZR, BPR > SADR; HC > BP, SAD, SZ, SZR, SADR.
MRI Data Acquisition and Preprocessing
Structural and functional MRI scans were acquired on 3-T scanners at each site (Scanning platforms and platforms parameters are listed in Table S1 in Supplementary Material). Structural and functional images were collected during the same scan session. Foam pads and ear plugs were used to minimize head motion and scanner noise. All the subjects were instructed to keep their eyes fixated on a crosshair, not to think about anything in particular and to move as little as possible.
Voxel-Based Morphometry
Voxel-based morphometry analyses of structural images were performed using the VBM8 toolbox1 as implemented in SPM8. T1-weighted images were bias-corrected and segmented into GM, white matter (WM), and cerebrospinal fluid (CSF) by “New Segment” using a customized template, which was constructed from our 1199 study samples by DARTEL in SPM8 (40). The segmented images were normalized to Montreal Neurological Institute (MNI) space (41) using the DARTEL template and resampled to 1.5 mm × 1.5 mm × 1.5 mm voxels. In the final step, the segmented normalized images were spatially smoothed with an 8 mm × 8 mm × 8 mm full width at half maximum Gaussian kernel.
Amplitude of Low-Frequency Fluctuations
Functional image preprocessing was carried out using data processing assistant for resting-state fMRI (DPARSF), version 2.3 (42), implemented in the MATLAB toolbox (Mathworks, Inc.). The first 9 s of each subject data were discarded before slice timing and head motion correction were performed. Then, the individual structural T1 image was coregistered to the mean functional image after motion correction. Subjects with head motion >3.0 mm of maximal translation in any direction or 3.0° of maximal rotation were excluded from further analysis. In addition, six motion parameters, CSF, and WM signals were used as nuisance covariates to reduce effects of head motion and non-neuronal BOLD fluctuations. Images were then DARTEL normalized to MNI space and resampled to 3 mm × 3 mm × 3 mm voxels. Subsequently, the time series were band-pass filtered (0.01–0.08 Hz) and linear trends removed. Then, the preprocessed time series were transformed to the frequency domain using fast Fourier transform, and power spectra obtained. Because the power of a given frequency is proportional to the square of the amplitude of this frequency component of the original time series in the time domain, the square root was calculated at each frequency of the power spectrum and the averaged square root was obtained across 0.01–0.08 Hz at each voxel. This averaged square root was taken as the ALFF. For standardization purpose, the ALFF of each voxel was divided by the global mean ALFF value. Finally, all images were spatially smoothed with an 8 mm × 8 mm × 8 mm full width at half maximum Gaussian kernel.
Joint-Independent Component Analysis
Joint-independent component analysis is a second-level fMRI analysis method that assumes two or more features (modalities) share the same mixing matrix and maximizes the independence among joint components. ICA is performed on the horizontally concatenated feature sets (along voxels in structure–function in this case), thus uncovering patterns of data that commonly fluctuate or are connected across both modalities (see Figure S1 in Supplementary Material). It is suitable for examining a common modulation across subjects among modalities and has been applied to link a variety of feature sets in the past (43, 44). jICA (28, 45) assumes a model χ = AS where joint-independent sources (S) are linearly mixed by a common mixing parameter (A) to generate the observations data matrix (χ). In this case, we use ICA analysis algorithms to form the overall data matrix χ = [χGM, χALFF] and derive spatially independent joint sources S = [SGM, SALFF] along with their shared mixing parameter (A), which are presented as loading parameters for each subject. A total of 22 independent components were estimated according to minimum description length criteria (46) using the Group ICA of fMRI Toolbox (GIFT).2 The jICA was performed using the Fusion ICA Toolbox.3 First, the preprocessed ALFF and GM images were normalized to have the same average sum of squares to ensure that units were shared between data types. Normalization was performed on group level, so covariations among subjects were preserved. Then, the ALFF and GM data were modeled by matching the sums of squares across modalities and combined into a single data matrix, used to identify the common mixing matrix parameters using the infomax algorithm (47) shared by spatially independent joint source images (ALFF and GM images). The complete details of the method were as reported in Ref. (28).
Statistical Analysis
A one-way analysis of variance (ANOVA) and chi-square test were carried out for demographic and clinical variables. The effects of age, sex, and site were regressed out using linear regression, and residuals of loading parameters of the independent components were compared across probands, relatives, and HC using ANOVA. Independent components showing significant main effect of group difference after Bonferroni correction were further evaluated using post hoc pair-wise group comparisons. A false discovery rate (FDR) correction for multiple comparisons was applied to post hoc tests. To assess whether the estimated ICA joint sources were associated with clinical symptoms, cognitive, or general socio-functioning, we derived associations between the residuals of the independent components and PANSS, MADRS, YMRS, BACS, and SFS scores across all available subjects. For the above association analyses, we added group as an additional covariate to covary any baseline group differences in cognition and social function.
In addition, relative risk (48) of joint structural–functional abnormalities presented by the independent components was calculated as the ratio of percentage of relatives classified as “affected” based on a threshold of 2 SD above the control mean to the percentage of healthy controls designated as “affected.” A chi-square was used to test for significance of relative risk in relatives compared with HC.
Furthermore, we used an ANCOVA model to detect the main effect of site across healthy controls and the effect of diagnosis-by-site across all groups separately. The above analyses were performed using SPSS v17.0 (Statistical Package for the Social Sciences, IBM, Chicago, IL, USA).
Results
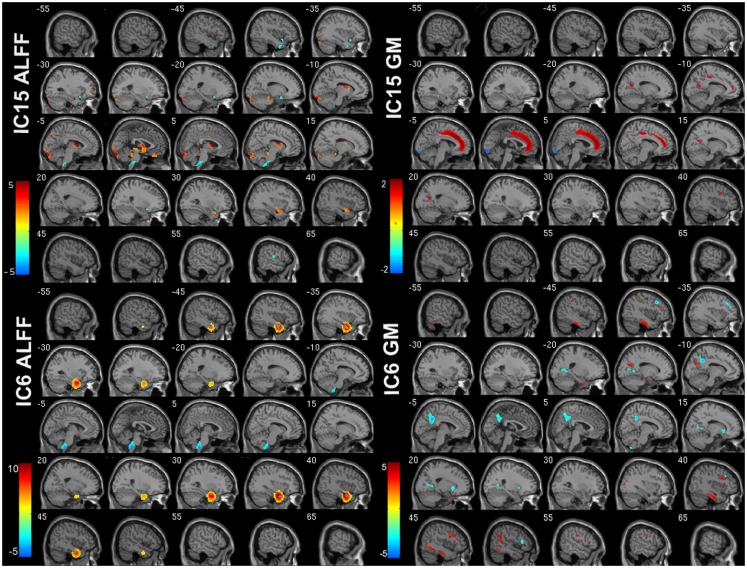
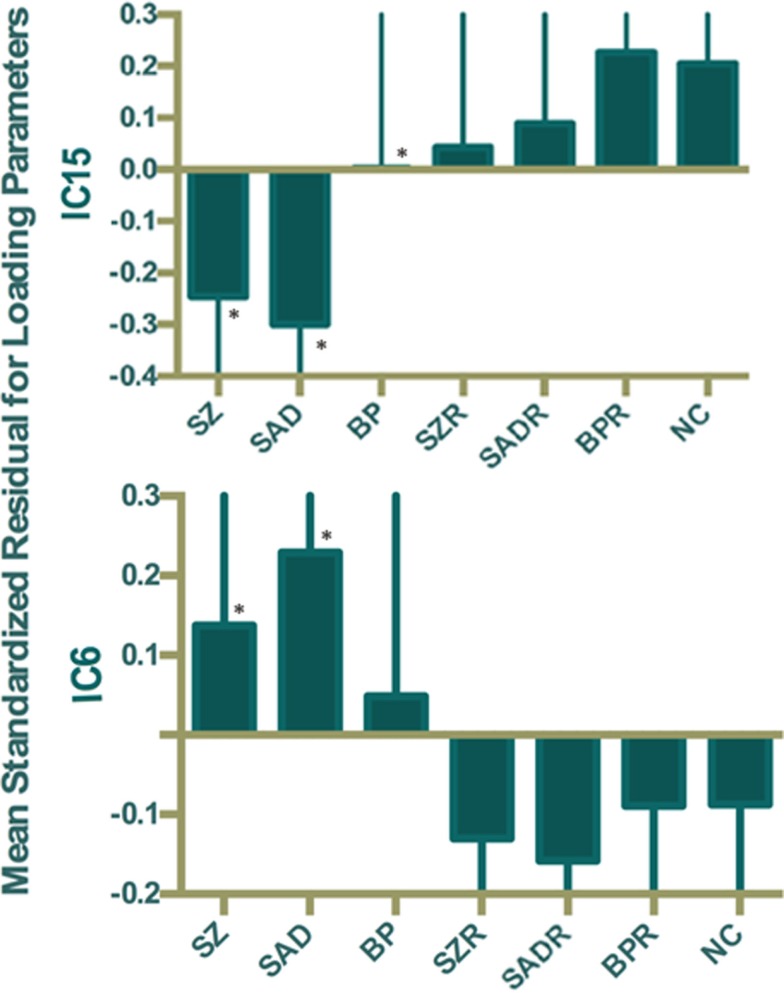
Of the 22 components estimated from the data, only network pair 6 (IC6) (F = 9.62; p = 7 × 10−5) and IC15 (F = 17.79; p = 2 × 10−8) showed a group main effects after Bonferroni correction. Talairach coordinates for the regions of IC15 and IC6 at a threshold of |Z| > 2.5 are summarized in Tables 2 and 3. The ALFF/GM maps of IC15 and IC6 are shown in Figure 1. As part of the output, jICA also produces loading parameters for each component pair that reflects the component’s influence at the subject level (49). This is further used to assess the between-subject differences in sMRI–fMRI association. Post hoc tests revealed loading parameters of IC6 were higher both in probands with SZ (p = 0.024) and SAD (p = 0.012) in relative to healthy controls. For IC 15, loading parameters were lower in probands with SZ (p = 0.012), SAD (p = 0.024), and BP (p = 0.036) relative to healthy controls separately. Contrasts revealed no effect of relatives and healthy controls in either IC6 or IC15. The mean standardized residual of loading parameters are shown in Figure 2. All posthoc measures were corrected using the FDR method (for reference).
Table 2.
Talairach coordinates for significant regions of component 15.
| Region | BA | Left/right volume (cc) | Left/right Zmax (x, y, z) |
|---|---|---|---|
|
IC15_ALFF CONTROLS > PROBANDS | |||
| Lingual gyrus | 17, 18 | 2.3/1.4 | 6.9 (−3, −91, −11)/6.7 (6, −88, −11) |
| Thalamus | NA | 1.6/2.1 | 4.5 (−9, −5, 11)/4.1 (6, −5, 11) |
| Culmen | NA | 1.7/1.5 | 3.2 (−18, −30, −16)/3.5 (0, −39, −21) |
| Declive | NA | 1.1/1.0 | 3.6 (−18, −88, −18)/3.5 (3, −79, −11) |
| Superior temporal gyrus | 38 | 0.0/1.9 | NA/4.0 (36, 8, −21) |
| Caudate | NA | 0.6/1.0 | 5.0 (−9, 4, 14)/4.5 (9, 6, 11) |
| Superior frontal gyrus | 6, 8, 10 | 1.3/0.0 | 2.8 (−30, 61, −3)/NA |
| Rectal gyrus | 11 | 0.6/0.5 | 2.7 (−3, 34, −22)/2.5 (3, 37, −25) |
| Cuneus | 17, 18, 19 | 0.7/0.0 | 3.3 (−3, −93, 0)/NA |
| Fusiform gyrus | 18 | 0.6/0.0 | 5.0 (−21, −91, −13)/NA |
| Inferior occipital gyrus | 17, 18 | 0.6/0.0 | 4.1 (−30, −88, −13)/NA |
| Precuneus | 7 | 0.5/0.0 | 3.3 (−3, −76, 45)/NA |
| Anterior cingulate | 25 | 0.5/0.0 | 3.5 (0, 2, −10)/NA |
| PROBANDS > CONTROLS | |||
| Inferior frontal gyrus | 13, 47 | 1.2/0.8 | 3.2 (−39, 11, −13)/2.8 (24, 11, −16) |
| Middle temporal gyrus | 21, 38 | 1.3/0.3 | 3.0 (−39, 4, −30)/2.4 (48, 4, −30) |
| Middle occipital gyrus | 18, 37 | 0.0/0.9 | NA/2.5 (33, −76, −9) |
| Superior temporal gyrus | 22, 38 | 0.6/0.0 | 2.6 (−39, 7, −28)/NA |
| Cuneus | 17, 18 | 0.0/0.6 | NA/2.6 (6, −84, 12) |
| Transverse temporal gyrus | 41, 42 | 0.0/0.5 | NA/3.2 (62, −14, 12) |
|
IC15_GM CONTROLS > PROBANDS | |||
| Cingulate gyrus | 24, 31, 32 | 7.0/6.4 | 3.6 (−4, 25, 28)/3.4 (6, 28, 28) |
| Medial frontal gyrus | 6, 8, 9, 10, 11, 32 | 5.9/5.6 | 3.2 (−7, 46, 12)/3.6 (4, 42, 15) |
| Anterior cingulate | 10, 24, 32 | 4.1/4.6 | 3.5 (−4, 43, 13)/3.8 (7, 36, 19) |
| Paracentral lobule | 5, 6, 31 | 1.1/1.0 | 2.9 (−3, −11, 43)/3.0 (9, −25, 44) |
| Precuneus | 7, 31 | 1.3/0.6 | 3.0 (−13, −62, 22)/2.7 (15, −57, 24) |
| Posterior cingulate | 30 | 0.8/0.7 | 3.2 (−13, −56, 17)/2.7 (15, −53, 15) |
| Middle frontal gyrus | 9 | 0.0/0.8 | NA/3.0 (40, 10, 30) |
| PROBANDS > CONTROLS | |||
| Lingual gyrus | 17, 18 | 1.7/1.3 | 3.1 (0, −86, −7)/3.0 (3, −88, −4) |
| Fusiform gyrus | 19, 20, 37 | 0.3/0.7 | 2.3 (−52, −66, −12)/2.5 (52, −63, −13) |
NA = not applicable.
Table 3.
Talairach coordinates for significant regions of component 6.
| Region | BA | Left/right volume (cc) | Left/right Zmax (x, y, z) |
|---|---|---|---|
|
IC6_ALFF PROBANDS > CONTROLS | |||
| Uncus | 20, 28, 34, 36 | 5.1/4.9 | 8.6 (−33, −1, −28)/8.9 (33, −4, −28) |
| Superior temporal gyrus | 38 | 3.4/4.4 | 7.8 (−33, 5, −23)/7.9 (39, 2, −20) |
| Middle temporal gyrus | 20, 21, 38 | 2.6/2.9 | 7.6 (−39, 2, −28)/10.5 (39, −4, −28) |
| Parahippocampal gyrus | 34, 35 | 2.6/2.5 | 8.1 (−33, −4, −20)/9.4 (36, −1, −20) |
| Inferior temporal gyrus | 20 | 1.9/2.7 | 5.2 (−45, −4, −28)/8.4 (42, −7, −27) |
| Fusiform gyrus | 20 | 0.5/0.5 | 4.1 (−39, −13, −25)/6.9 (42, −10, −25) |
|
IC6_GM PROBANDS > CONTROLS | |||
| Fusiform gyrus | 20, 36, 37 | 1.2/1.1 | 3.9 (−42, −17, −24)/4.2 (42, −16, −24) |
| Superior temporal gyrus | 13, 22, 38, 39, 41 | 0.8/1.0 | 3.3 (−27, 15, −30)/3.4 (49, −44, 19) |
| Middle frontal gyrus | 6, 9, 10, 46 | 0.4/1.2 | 2.7 (−37, 37, 11)/3.9 (40, 13, 27) |
| Precuneus | 7, 31 | 1.1/0.2 | 3.7 (−13, −69, 26)/2.1 (19, −60, 28) |
| Uncus | 20, 28, 36, 38 | 1.0/0.3 | 4.1 (−19, 3, −32)/2.8 (22, 9, −27) |
| Inferior parietal lobule | 40 | 0.8/0.3 | 3.2 (−43, −34, 39)/4.9 (46, −46, 22) |
| Inferior frontal gyrus | 9, 47 | 0.3/0.8 | 2.5 (−39, 34, 13)/3.8 (42, 6, 33) |
| Inferior temporal gyrus | 20, 37 | 0.0/0.8 | NA/3.9 (40, −13, −27) |
| Precentral gyrus | 6, 9, 13, 43 | 0.0/0.8 | NA/3.0 (53, −4, 10) |
| Supramarginal gyrus | 40 | 0.0/0.8 | NA/5.0 (48, −47, 26) |
| Middle temporal gyrus | 37, 39 | 0.0/0.4 | NA/2.7 (34, −76, 18) |
| CONTROLS > PROBANDS | |||
| Precuneus | 7, 31 | 2.8/2.0 | 4.6 (−7, −46, 34)/3.2 (4, −48, 33) |
| Cingulate gyrus | 31 | 1.8/1.6 | 4.2 (−7, −43, 37)/4.2 (9, −42, 37) |
| Middle frontal gyrus | 9, 10 | 1.9/1.2 | 4.6 (−37, 22, 32)/4.5 (37, 25, 32) |
| Posterior cingulate | 23, 30, 31 | 1.5/0.9 | 3.8 (−19, −65, 10)/3.5 (18, −64, 10) |
| Middle temporal gyrus | 20, 21 | 1.7/0.5 | 2.8 (−56, −41, −9)/2.6 (55, −2, −20) |
| Lentiform nucleus | * | 0.0/1.6 | NA/3.2 (19, 14, −3) |
| Inferior frontal gyrus | 45, 47 | 0.0/1.2 | NA/3.4 (50, 22, 10) |
| Inferior temporal gyrus | 20, 21 | 0.7/0.3 | 2.5 (−61, −21, −22)/2.6 (58, −23, −15) |
| Declive | * | 0.0/0.7 | NA/2.6 (40, −75, −15) |
| Cuneus | 18, 23, 30 | 0.6/0.0 | 3.9 (−16, −68, 12)/NA |
| Precentral gyrus | 6, 9 | 0.3/0.3 | 5.2 (−37, 21, 36)/3.0 (50, 19, 7) |
| Lingual gyrus | 18, 19 | 0.4/0.2 | 3.1 (−16, −51, 5)/2.5 (22, −54, 5) |
| Parahippocampal gyrus | 30 | 0.3/0.2 | 2.7 (−22, −52, 5)/3.4 (19, −49, 5) |
Figure 1.
ALFF and GM spatial maps for joint IC6 and IC15. For display, the components were converted to Z-values and thresholded at |Z| > 2.5.
Figure 2.
Mean standardized residual of loading parameters for IC15 and IC6, controlling for age, sex, and site. *Individual group had significantly different loading parameters compared to control subjects after false discovery rate (FDR) correction.
We correlated the loading parameters of both ICs with the PANSS, MADRS, YMRS, BACS, SBS, and SFS scores for all available subjects. While, loading parameters of IC6 showed no correlation with any of the above scores. Loading parameters of IC15 were positively correlated with the BACS composite scores, BACS symbol coding scores, and BACS tower of London scores after FDR correction (Table 4).
Table 4.
Significant correlations between IC15 loading parameters and the brief assessment of cognition in schizophrenia adjusted using FDR correction for multiple comparisons.
| IC15 | BACS (z) | R | p* |
|---|---|---|---|
| Symbol coding | 0.175 | 0.001 | |
| Tower of London | 0.157 | 0.003 | |
| Composite score | 0.169 | 0.001 |
*FDR corrected.
There was no significant difference between relatives and healthy controls in relative risk of joint structural–functional abnormalities. Main effects of site were observed for both IC6 (F = 40.63, p = 4 × 10−30) and IC15 (F = 9.98, p = 1 × 10−8). However, more importantly, no diagnosis-by-site interaction was noted.
Discussion
The human brain is connected on a variety of different spatial scales, from synaptic signaling at the cellular level to a more broad systems level containing inter-regional communication across physically distant brain regions. A natural starting point to examine system level architecture is by using traditional “unimodal” techniques. However, it is also possible to apply more advanced statistical techniques to define “cross-modal” brain relationships between disparate measures (e.g., structure and function). In this study, we took this approach to detect common and unique abnormalities in a large psychosis sample by fusing two modalities (rs-fMRI and sMRI) using a jICA approach across the psychotic spectrum (SZ, SAD, and psychotic BP) and to investigate which of those are shared by their unaffected first-degree relatives, suggesting possible endophenotypes. Since multimodal techniques such as joint ICA capture “cross-feature” information simultaneously, they naturally contribute to a different set of information compared to their individual “unimodal” counterparts.
By using a jICA approach, two components showing group differences were identified. Joint loadings computed from IC15 showed significant differences in SZ, SAD, and BP (compared to HC), while IC6 distinguished only SZ and SAD from controls. However, first-degree, non-psychotic relatives showed no common abnormalities with the probands and no significant differences compared to HC. Consistent with this finding, we found that the relative risk estimates for the two components were non-significant. Brain changes in function and structure correlated with certain sub-scales of the BACS inventory, suggesting direction relationships between affected structure–function patterns and cognitive function scores.
The IC15-ALFF network encompassed regions, including thalamus, cerebellum, prefrontal cortex, and caudate, which are primarily involved in the prefrontal–striatal–thalamic–cerebellar network that has been implicated in the pathophysiology of both SZ (50, 51) and BP (52), supported by growing evidence (53–59). The prefrontal cortex plays a critical role in executive cognitive control, whereas the striatum and the cerebellum, which are connected with the prefrontal cortex via thalamus (60, 61), are also involved in executive function, working memory, spatial cognition, and language (62). The thalamus not only functions as a nexus to integrate cortical and subcortical activity (63, 64) but is also implicated in processing and integrating sensory information via connections with sensory–motor cortices (65, 66). Remaining brain regions in IC15-ALFF included visual areas, such as lingual gyrus, cuneus, fusiform gyrus, and occipital cortex; and auditory-related areas, such as superior temporal and transverse temporal gyri, which may indicate dysconnectivity between sensory cortices and thalamus in psychosis. Thus, dysfunctions in this network may be associated with abnormal cognition, difficulty in coordinating processing, prioritization, retrieval, and expression of the information associated with psychotic symptoms (51, 67). Consistent with our results, Anticevic et al. (68) documented that thalamic connectivity with prefrontal–striatal–cerebellar regions successfully classified SZ and psychotic bipolar patients, suggesting that this network may be abnormal across diagnoses. Interestingly, IC15 also showed decreased GM in regions that constitute the functional DMN (69), consistent with previous findings in both SZ/SAD and BP that showed reduced GM (24, 70–75). Two regions within IC15 showing increased GM in psychosis probands were lingual gyrus and fusiform gyrus, consistent with previous studies with larger fusiform gyrus in both SZ and BP (76) and larger lingual gyrus in SZ (77) compared with healthy controls. Positive correlation between the loading parameters of IC15 and BACS scores support a link between abnormalities in prefrontal–striatal–thalamic–cerebellar network and DMN and cognitive function, consistent with previous studies (38, 78–84). Interestingly, symbol coding was the most sensitive indicator of genetic liability for SZ/SAD and performance distinguished psychotic BP from major depression (85).
Among the IC6-ALFF regions, a subset of temporal regions showed higher ALFF in both SZ and SAD in relative to HC and no difference between BP and controls. These results are consistent with previous studies that increased ALFF were found in inferior temporal gyrus, uncus, fusiform gyrus (86), superior temporal gyrus (87), and parahippocampal gyrus (88) in SZ when compared to HC. All these regions overlap with the IC6-GM regions, which suggest that both temporal lobe function and structure are disturbed in SZ and SAD (89, 90). Regions noted as part of IC6-GM have been consistently shown to have reduced GM in SZ compared to HC (91, 92), often in association with psychotic symptoms (93). Another jICA study (28) that combined fMRI (from an auditory oddball task) and sMRI data showed similar brain regions to ours with both increased GM and abnormal activation primarily located in temporal lobe in SZ compared to HC. Furthermore, consistent with our results, Calhoun et al. (94) reported that temporal lobe functional data successfully discriminated HC from SZ during an auditory oddball task, and combined temporal lobe and DMN data in resting-state discriminated between SZ and psychotic BP, consistent with well-studied temporal lobe anomalies in SZ (45).
A natural question is what mechanisms may be responsible for these types of long-distance structural–functional couplings and how functional data in one region might be linked to a different/remotely located functional region or vice versa. One possibility is that the local GM volume in one region affects the quantity of functional output from that region, which in turn has a causal influence on synaptic input arriving at a distal cortical location, thus suggesting a relationship from structure to downstream functional response. Alternatively, the causal direction of the relationship could be reversed, with the amount of functional activity in a region influencing the structural volume of a downstream region, either through excitotoxic or neurotrophic influences. Notably, an excitotoxic downstream effect would be a mechanism by which increased functional activity in one region (if consistently elevated) could lead to decreased structural volume in another region. In all these hypothesized mechanisms, it is possible that the observed structure–function relationship is mediated by intervening regions (either direct or indirect connections). Overall, multiple mechanisms and pathways could lead to a coupling between structural and functional characteristics of the brain. Because these mechanisms are not static, it seems likely that the strength and directionality of structure–function correlations could vary in psychiatric populations, such as SZ, where brain connectivity is compromised in general.
The current subject sample largely overlapped with two previously published studies from our group investigating sMRI and ALFF individually in a more traditional “unimodal” voxel-wise fashion (24, 95). Importantly, these previous studies did not look at connectivity of regions as being presently reported here. Overall, in these previously reported studies, we identified larger structural and functional anomalies in SZ/SAD compared to PBP, consistent with findings from the current jICA approach. However, not all regions reported in the current study overlapped with previous findings. This is not surprising, given that jICA (a) is a purely data-driven (blind) technique, (b) captures data patterns that are linked between multimodal features, and (c) explores connectivity patterns among large-scale networks as opposed to regional effects. The jICA approach is therefore a completely different and novel approach to explore the data compared to traditional voxel-wise/regional methods, as reported previously.
Advantages of our study are the relatively large population with psychosis probands and relatives across the psychosis dimension and we combine two different data type to investigate the abnormalities. Limitations of the study include the potential confounds related to medication and illness state (96).
In summary, this study provides evidence based on a large sample of psychosis probands and relatives that associate between functional brain alterations (ALFF) in a prefrontal–striatal–thalamic–cerebellar network and structural abnormalities (GM) in DMN are common disturbances across psychotic diagnoses, while the alteration in both function and structure in temporal lobe are unique to SZ and SAD. Our results also suggest that SAD is more similar to SZ across the schizo-bipolar spectrum. Comparisons between relatives and HC reveal that these structural–functional abnormalities may be psychosis biomarkers rather than endophenotypes. Future research investigating associations between different data types, fusing information from different modalities, may provide more clues to uncover the mechanisms of psychotic illnesses, leading to a biologically driven classification and more efficient and ultimately personalized treatment strategies.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
2http://mialab.mrn.org/software/gift, version 2.0a
3http://mialab.mrn.org/software/fit, version 1.2c
Funding
The current study was funded and supported by the following grants NIMH MH077851, MH078113, MH077945, MH077852, P20GM103472, and MH077862. MK has received a grant from Sunovion. JS has receives support from Janssen, Takeda, BMS, Roche, and Lilly. GP has been a consultant for Bristol-Meyer Squibb.
Supplementary Material
The Supplementary Material for this article can be found online at http://journal.frontiersin.org/article/10.3389/fpsyt.2015.00174
References
- 1.Théberge J, Williamson KE, Aoyama N, Drost DJ, Manchanda R, Malla AK, et al. Longitudinal grey-matter and glutamatergic losses in first-episode schizophrenia. Br J Psychiatry (2007) 191(4):325–34. 10.1192/bjp.bp.106.033670 [DOI] [PubMed] [Google Scholar]
- 2.Berrettini W. Evidence for shared susceptibility in bipolar disorder and schizophrenia Am J Med Genet C Semin Med Genet (2003) 123C(1):59–64. 10.1002/ajmg.c.20014 [DOI] [PubMed] [Google Scholar]
- 3.Lake CR, Hurwitz N. Schizoaffective disorder merges schizophrenia and bipolar disorders as one disease-there is no schizoaffective disorder. Curr Opin Psychiatry (2007) 20(4):365–79. 10.1097/YCO.0b013e3281a305ab [DOI] [PubMed] [Google Scholar]
- 4.Craddock N, O’Donovan MC, Owen MJ. Psychosis genetics: modeling the relationship between schizophrenia, bipolar disorder, and mixed (or “schizoaffective”) psychoses. Schizophr Bull (2009) 35(3):482–90. 10.1093/schbul/sbp020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keshavan MS, Morris DW, Sweeney JA, Pearlson G, Thaker G, Seidman LJ, et al. A dimensional approach to the psychosis spectrum between bipolar disorder and schizophrenia: the schizo-bipolar scale. Schizophr Res (2011) 133(1–3):250–4. 10.1016/j.schres.2011.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hill SK, Harris MS, Herbener ES, Pavuluri M, Sweeney JA. Neurocognitive allied phenotypes for schizophrenia and bipolar disorder. Schizophr Bull (2008) 34(4):743–59. 10.1093/schbul/sbn027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker JT, Holmes AJ, Masters GA, Yeo BT, Krienen F, Buckner RL, et al. Disruption of cortical association networks in schizophrenia and psychotic bipolar disorder. JAMA Psychiatry (2014) 71(2):109–18. 10.1001/jamapsychiatry.2013.3469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ivleva E, Thaker G, Tamminga CA. Comparing genes and phenomenology in the major psychoses: schizophrenia and bipolar 1 disorder. Schizophr Bull (2008) 34(4):734–42. 10.1093/schbul/sbn051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cardno AG, Marshall EJ, Coid B, Macdonald AM, Ribchester TR, Davies NJ, et al. Heritability estimates for psychotic disorders: the Maudsley twin psychosis series. Arch Gen Psychiatry (1999) 56(2):162–8. 10.1001/archpsyc.56.2.162 [DOI] [PubMed] [Google Scholar]
- 10.McGuffin P, Rijsdijk F, Andrew M, Sham P, Katz R, Cardno A. The heritability of bipolar affective disorder and the genetic relationship to unipolar depression. Arch Gen Psychiatry (2003) 60(5):497–502. 10.1001/archpsyc.60.5.497 [DOI] [PubMed] [Google Scholar]
- 11.Meda SA, Ruaño G, Windemuth A, O’Neil K, Berwise C, Dunn SM, et al. Multivariate analysis reveals genetic associations of the resting default mode network in psychotic bipolar disorder and schizophrenia. Proc Natl Acad Sci U S A (2014) 111(19):E2066–75. 10.1073/pnas.1313093111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gottesman II, Gould TD. The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry (2003) 160(4):636–45. 10.1176/appi.ajp.160.4.636 [DOI] [PubMed] [Google Scholar]
- 13.Smith SM, Vidaurre D, Beckmann CF, Glasser MF, Jenkinson M, Miller KL, et al. Functional connectomics from resting-state fMRI. Trends Cogn Sci (2013) 17(12):666–82. 10.1016/j.tics.2013.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith SM, Fox PT, Miller KL, Glahn DC, Fox PM, Mackay CE, et al. Correspondence of the brain’s functional architecture during activation and rest. Proc Natl Acad Sci U S A (2009) 106(31):13040–5. 10.1073/pnas.0901846106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ongür D, Lundy M, Greenhouse I, Shinn AK, Menon V, Cohen BM, et al. Default mode network abnormalities in bipolar disorder and schizophrenia. Psychiatry Res (2010) 183(1):59–68. 10.1016/j.pscychresns.2010.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calhoun VD, Sui J, Kiehl K, Turner J, Allen E, Pearlson G. Exploring the psychosis functional connectome: aberrant intrinsic networks in schizophrenia and bipolar disorder. Front Psychiatry (2012) 2:75. 10.3389/fpsyt.2011.00075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whalley HC, Simonotto E, Flett S, Marshall I, Ebmeier KP, Owens DG, et al. fMRI correlates of state and trait effects in subjects at genetically enhanced risk of schizophrenia. Brain (2004) 127(Pt 3):478–90. 10.1093/brain/awh070 [DOI] [PubMed] [Google Scholar]
- 18.Whalley HC, Simonotto E, Marshall I, Owens DG, Goddard NH, Johnstone EC, et al. Functional disconnectivity in subjects at high genetic risk of schizophrenia. Brain (2005) 128(Pt 9):2097–108. 10.1093/brain/awh556 [DOI] [PubMed] [Google Scholar]
- 19.Whitfield-Gabrieli S, Thermenos HW, Milanovic S, Tsuang MT, Faraone SV, McCarley RW, et al. Hyperactivity and hyperconnectivity of the default network in schizophrenia and in first-degree relatives of persons with schizophrenia. Proc Natl Acad Sci U S A (2009) 106(4):1279–84. 10.1073/pnas.0809141106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lui S, Yao L, Xiao Y, Keedy SK, Reilly JL, Keefe RS, et al. Resting-state brain function in schizophrenia and psychotic bipolar probands and their first-degree relatives. Psychol Med (2015) 45(1):97–108. 10.1017/S003329171400110X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McDonald C, Marshall N, Sham PC, Bullmore ET, Schulze K, Chapple B, et al. Regional brain morphometry in patients with schizophrenia or bipolar disorder and their unaffected relatives. Am J Psychiatry (2006) 163(3):478–87. 10.1176/appi.ajp.163.3.478 [DOI] [PubMed] [Google Scholar]
- 22.Emsell L, McDonald C. The structural neuroimaging of bipolar disorder. Int Rev Psychiatry (2009) 21(4):297–313. 10.1080/09540260902962081 [DOI] [PubMed] [Google Scholar]
- 23.Ivleva EI, Bidesi AS, Thomas BP, Meda SA, Francis A, Moates AF, et al. Brain gray matter phenotypes across the psychosis dimension. Psychiatry Res (2012) 204(1):13–24. 10.1016/j.pscychresns.2012.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ivleva EI, Bidesi AS, Keshavan MS, Pearlson GD, Meda SA, Dodig D, et al. Gray matter volume as an intermediate phenotype for psychosis: bipolar-schizophrenia network on intermediate phenotypes (B-SNIP). Am J Psychiatry (2013) 170(11):1285–96. 10.1176/appi.ajp.2013.13010126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mesulam MM. From sensation to cognition. Brain (1998) 121(6):1013–52. 10.1093/brain/121.6.1013 [DOI] [PubMed] [Google Scholar]
- 26.Skudlarski P, Jagannathan K, Anderson K, Stevens MC, Calhoun VD, Skudlarska BA, et al. Brain connectivity is not only lower but different in schizophrenia: a combined anatomical and functional approach. Biol Psychiatry (2010) 68(1):61–9. 10.1016/j.biopsych.2010.03.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhojraj TS, Prasad KM, Eack SM, Francis AN, Montrose DM, Keshavan MS. Do inter-regional gray-matter volumetric correlations reflect altered functional connectivity in high-risk offspring of schizophrenia patients? Schizophr Res (2010) 118(1–3):62–8. 10.1016/j.schres.2010.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Calhoun VD, Adali T, Giuliani NR, Pekar JJ, Kiehl KA, Pearlson GD. Method for multimodal analysis of independent source differences in schizophrenia: combining gray matter structural and auditory oddball functional data. Hum Brain Mapp (2006) 27(1):47–62. 10.1002/hbm.20166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Biswal B, Yetkin FZ, Haughton VM, Hyde JS. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn Reson Med (1995) 34(4):537–41. 10.1002/mrm.1910340409 [DOI] [PubMed] [Google Scholar]
- 30.Cordes D, Haughton VM, Arfanakis K, Carew JD, Turski PA, Moritz CH, et al. Frequencies contributing to functional connectivity in the cerebral cortex in “resting-state” data. Am J Neuroradiol (2001) 22(7):1326–33. [PMC free article] [PubMed] [Google Scholar]
- 31.Tamminga CA, Ivleva EI, Keshavan MS, Pearlson GD, Clementz BA, Witte B, et al. Clinical phenotypes of psychosis in the bipolar-schizophrenia network on intermediate phenotypes (B-SNIP). Am J Psychiatry (2013) 170(11):1263–74. 10.1176/appi.ajp.2013.12101339 [DOI] [PubMed] [Google Scholar]
- 32.First MB, Spitzer RL, Robert L, Gibbon M, Williams Janet BW. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition, January 1995 FINAL, SCID-I/P Version 2.0. New York, NY: Biometrics Research Department, New York State Psychiatric Institute; (1995). [Google Scholar]
- 33.Pfohl B, Blum N, Zimmerman M. Structured Interview for DSM-IV Personality. Washington, DC: American Psychiatric Association; (1997). [Google Scholar]
- 34.Farmer RF, Chapman AL. Evaluation of DSM-IV personality disorder criteria as assessed by the structured clinical interview for DSM-IV personality disorders. Compr Psychiatry (2002) 43(4):285–300. 10.1053/comp.2002.33494 [DOI] [PubMed] [Google Scholar]
- 35.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull (1987) 13(2):261. 10.1093/schbul/13.2.261 [DOI] [PubMed] [Google Scholar]
- 36.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry (1979) 134(4):382–9. 10.1192/bjp.134.4.382 [DOI] [PubMed] [Google Scholar]
- 37.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry (1978) 133(5):429–35. 10.1192/bjp.133.5.429 [DOI] [PubMed] [Google Scholar]
- 38.Keefe RS, Harvey PD, Goldberg TE, Gold JM, Walker TM, Kennel C, et al. Norms and standardization of the brief assessment of cognition in schizophrenia (BACS). Schizophr Res (2008) 102(1–3):108–15. 10.1016/S0920-9964(08)70325-6 [DOI] [PubMed] [Google Scholar]
- 39.Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The social functioning scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry (1990) 157(6):853–9. 10.1192/bjp.157.6.853 [DOI] [PubMed] [Google Scholar]
- 40.Ashburner J. A fast diffeomorphic image registration algorithm. Neuroimage (2007) 38(1):95–113. 10.1016/j.neuroimage.2007.07.007 [DOI] [PubMed] [Google Scholar]
- 41.Collins DL, Neelin P, Peters TM, Evans AC. Automatic 3D intersubject registration of MR volumetric data in standardized Talairach space. J Comput Assist Tomogr (1994) 18(2):192–205. 10.1097/00004728-199403000-00005 [DOI] [PubMed] [Google Scholar]
- 42.Chao-Gan Y, Yu-Feng Z. DPARSF: a MATLAB toolbox for “pipeline” data analysis of resting-state fMRI. Front Syst Neurosci (2010) 4:13. 10.3389/fnsys.2010.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Franco AR, Ling J, Caprihan A, Calhoun VD, Jung RE, Heileman GL, et al. Multimodal and multi-tissue measures of connectivity revealed by joint independent component analysis. IEEE J Sel Top Signal Process (2008) 2(6):986–97. 10.1109/JSTSP.2008.2006718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sui J, Adali T, Yu Q, Chen J, Calhoun VD. A review of multivariate methods for multimodal fusion of brain imaging data. J Neurosci Methods (2012) 204(1):68–81. 10.1016/j.jneumeth.2011.10.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Calhoun VD, Maciejewski PK, Pearlson GD, Kiehl KA. Temporal lobe and “default” hemodynamic brain modes discriminate between schizophrenia and bipolar disorder. Hum Brain Mapp (2008) 29(11):1265–75. 10.1002/hbm.20581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rissanen J. Stochastic complexity and modeling. Ann Stat (1986) 4:1080–100. 10.1214/aos/1176350051 [DOI] [Google Scholar]
- 47.Bell AJ, Sejnowski TJ. An information-maximization approach to blind separation and blind deconvolution. Neural Comput (1995) 7(6):1129–59. 10.1162/neco.1995.7.6.1129 [DOI] [PubMed] [Google Scholar]
- 48.Egan MF, Goldberg TE, Gscheidle T, Weirich M, Bigelow LB, Weinberger DR. Relative risk of attention deficits in siblings of patients with schizophrenia. Am J Psychiatry (2000) 157(8):1309–16. 10.1176/appi.ajp.157.8.1309 [DOI] [PubMed] [Google Scholar]
- 49.Calhoun VD, Adali T, Pearlson GD, Pekar JJ. A method for making group inferences from functional MRI data using independent component analysis. Hum Brain Mapp (2001) 14(3):140–51. 10.1002/hbm.1048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Andreasen NC, O’Leary DS, Cizadlo T, Arndt S, Rezai K, Ponto LL, et al. Schizophrenia and cognitive dysmetria: a positron-emission tomography study of dysfunctional prefrontal-thalamic-cerebellar circuitry. Proc Natl Acad Sci U S A (1996) 93(18):9985–90. 10.1073/pnas.93.18.9985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Andreasen NC, Paradiso S, O’Leary DS. “Cognitive dysmetria” as an integrative theory of schizophrenia. Schizophr Bull (1998) 24(2):203–18. 10.1093/oxfordjournals.schbul.a033321 [DOI] [PubMed] [Google Scholar]
- 52.Strakowski SM, Delbello MP, Adler CM. The functional neuroanatomy of bipolar disorder: a review of neuroimaging findings. Mol Psychiatry (2005) 10(1):105–16. 10.1038/sj.mp.4001585 [DOI] [PubMed] [Google Scholar]
- 53.Wiser AK, Andreasen NC, O’Leary DS, Watkins GL, Boles Ponto LL, Hichwa RD. Dysfunctional cortico-cerebellar circuits cause ‘cognitive dysmetria’ in schizophrenia. Neuroreport (1998) 9(8):1895–9. 10.1097/00001756-199806010-00042 [DOI] [PubMed] [Google Scholar]
- 54.Soares JC. Can brain-imaging studies provide a ‘mood stabilizer signature?’. Mol Psychiatry (2001) 7:S64–70. 10.1038/sj.mp.4001020 [DOI] [PubMed] [Google Scholar]
- 55.Blumberg HP, Martin A, Kaufman J, Leung HC, Skudlarski P, Lacadie C, et al. Frontostriatal abnormalities in adolescents with bipolar disorder: preliminary observations from functional MRI. Am J Psychiatry (2003) 160(7):1345–7. 10.1176/appi.ajp.160.7.1345 [DOI] [PubMed] [Google Scholar]
- 56.Camchong J, Dyckman KA, Chapman CE, Yanasak NE, McDowell JE. Basal ganglia-thalamocortical circuitry disruptions in schizophrenia during delayed response tasks. Biol Psychiatry (2006) 60(3):235–41. 10.1016/j.biopsych.2005.11.014 [DOI] [PubMed] [Google Scholar]
- 57.Bor J, Brunelin J, Sappey-Marinier D, Ibarrola D, d’Amato T, Suaud-Chagny MF, et al. Thalamus abnormalities during working memory in schizophrenia. An fMRI study. Schizophr Res (2011) 125(1):49–53. 10.1016/j.schres.2010.10.018 [DOI] [PubMed] [Google Scholar]
- 58.Marenco S, Stein JL, Savostyanova AA, Sambataro F, Tan HY, Goldman AL, et al. Investigation of anatomical thalamo-cortical connectivity and FMRI activation in schizophrenia. Neuropsychopharmacology (2012) 37(2):499–507. 10.1038/npp.2011.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Quidé Y, Morris RW, Shepherd AM, Rowland JE, Green MJ. Task-related fronto-striatal functional connectivity during working memory performance in schizophrenia. Schizophr Res (2013) 150(2–3):468–75. 10.1016/j.schres.2013.08.009 [DOI] [PubMed] [Google Scholar]
- 60.Middleton FA, Strick PL. Anatomical evidence for cerebellar and basal ganglia involvement in higher cognitive function. Science (1994) 266(5184):458–61. 10.1126/science.7939688 [DOI] [PubMed] [Google Scholar]
- 61.Middleton FA, Strick PL. Basal ganglia and cerebellar loops: motor and cognitive circuits. Brain Res Rev (2000) 31(2):236–50. 10.1016/S0165-0173(99)00040-5 [DOI] [PubMed] [Google Scholar]
- 62.Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain (1998) 121(4):561–79. 10.1093/brain/121.4.561 [DOI] [PubMed] [Google Scholar]
- 63.Cummings JL. Frontal-subcortical circuits and human behavior. Arch Neurol (1993) 50(8):873–80. 10.1001/archneur.1993.00540080076020 [DOI] [PubMed] [Google Scholar]
- 64.Ramnani N. The primate cortico-cerebellar system: anatomy and function. Nat Rev Neurosci (2006) 7(7):511–22. 10.1038/nrn1953 [DOI] [PubMed] [Google Scholar]
- 65.Geyer MA, Krebs-Thomson K, Braff DL, Swerdlow NR. Pharmacological studies of prepulse inhibition models of sensorimotor gating deficits in schizophrenia: a decade in review. Psychopharmacology (2001) 156(2–3):117–54. 10.1007/s002130100811 [DOI] [PubMed] [Google Scholar]
- 66.Turetsky BI, Calkins ME, Light GA, Olincy A, Radant AD, Swerdlow NR. Neurophysiological endophenotypes of schizophrenia: the viability of selected candidate measures. Schizophr Bull (2007) 33(1):69–94. 10.1093/schbul/sbl060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Damaraju E, Allen EA, Belger A, Ford JM, McEwen S, Mathalon DH, et al. Dynamic functional connectivity analysis reveals transient states of dysconnectivity in schizophrenia. Neuroimage Clin (2014) 5:298–308. 10.1016/j.nicl.2014.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Anticevic A, Cole MW, Repovs G, Murray JD, Brumbaugh MS, Winkler AM, et al. Characterizing thalamo-cortical disturbances in schizophrenia and bipolar illness. Cereb Cortex (2013) 24(12):3116–30. 10.1093/cercor/bht165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci (2008) 1124:1–38. 10.1196/annals.1440.011 [DOI] [PubMed] [Google Scholar]
- 70.Farrow TF, Whitford TJ, Williams LM, Gomes L, Harris AW. Diagnosis-related regional gray matter loss over two years in first episode schizophrenia and bipolar disorder. Biol Psychiatry (2005) 58(9):713–23. 10.1016/j.biopsych.2005.04.033 [DOI] [PubMed] [Google Scholar]
- 71.Bora E, Fornito A, Yücel M, Pantelis C. Voxelwise meta-analysis of gray matter abnormalities in bipolar disorder. Biol Psychiatry (2010) 67(11):1097–105. 10.1016/j.biopsych.2010.01.020 [DOI] [PubMed] [Google Scholar]
- 72.Ellison-Wright I, Bullmore E. Anatomy of bipolar disorder and schizophrenia: a meta-analysis. Schizophr Res (2010) 117(1):1–12. 10.1016/j.schres.2009.12.022 [DOI] [PubMed] [Google Scholar]
- 73.Venkatasubramanian G. Neuroanatomical correlates of psychopathology in antipsychotic-naive schizophrenia. Indian J Psychiatry (2010) 52(1):28–36. 10.4103/0019-5545.74304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yu K, Cheung C, Leung M, Li Q, Chua S, McAlonan G. Are bipolar disorder and schizophrenia neuroanatomically distinct? An anatomical likelihood meta-analysis. Front Hum Neurosci (2010) 4:189. 10.3389/fnhum.2010.00189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bora E, Pantelis C. Structural trait markers of bipolar disorder: disruption of white matter integrity and localized gray matter abnormalities in anterior fronto-limbic regions. Biol Psychiatry (2011) 69(4):299–300. 10.1016/j.biopsych.2010.12.020 [DOI] [PubMed] [Google Scholar]
- 76.Anderson D, Ardekani BA, Burdick KE, Robinson DG, John M, Malhotra AK, et al. Overlapping and distinct gray and white matter abnormalities in schizophrenia and bipolar I disorder. Bipolar Disord (2013) 15(6):680–93. 10.1111/bdi.12096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mané A, Falcon C, Mateos JJ, Fernandez-Egea E, Horga G, Lomeña F, et al. Progressive gray matter changes in first episode schizophrenia: a 4-year longitudinal magnetic resonance study using VBM. Schizophr Res (2009) 114(1–3):136–43. 10.1016/j.schres.2009.07.014 [DOI] [PubMed] [Google Scholar]
- 78.Owen AM, Doyon J, Petrides M, Evans AC. Planning and spatial working memory: a positron emission tomography study in humans. Eur J Neurosci (1996) 8(2):353–64. 10.1111/j.1460-9568.1996.tb01219.x [DOI] [PubMed] [Google Scholar]
- 79.Beauchamp MH, Dagher A, Aston JA, Doyon J. Dynamic functional changes associated with cognitive skill learning of an adapted version of the Tower of London task. Neuroimage (2003) 20(3):1649–60. 10.1016/j.neuroimage.2003.07.003 [DOI] [PubMed] [Google Scholar]
- 80.Greicius MD, Krasnow B, Reiss AL, Menon V. Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc Natl Acad Sci U S A (2003) 100(1):253–8. 10.1073/pnas.0135058100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Broyd SJ, Demanuele C, Debener S, Helps SK, James CJ, Sonuga-Barke EJ. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehav Rev (2009) 33(3):279–96. 10.1016/j.neubiorev.2008.09.002 [DOI] [PubMed] [Google Scholar]
- 82.Forsyth JK, Bolbecker AR, Mehta CS, Klaunig MJ, Steinmetz JE, O’Donnell BF, et al. Cerebellar-dependent eyeblink conditioning deficits in schizophrenia spectrum disorders. Schizophr Bull (2012) 38(4):751–9. 10.1093/schbul/sbq148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Caletti E, Paoli RA, Fiorentini A, Cigliobianco M, Zugno E, Serati M, et al. Neuropsychology, social cognition and global functioning among bipolar, schizophrenic patients and healthy controls: preliminary data. Front Hum Neurosci (2013) 7:661. 10.3389/fnhum.2013.00661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Matsuo K, Chen SH, Liu CM, Liu CC, Hwang TJ, Hsieh MH, et al. Stable signatures of schizophrenia in the cortical-subcortical-cerebellar network using fMRI of verbal working memory. Schizophr Res (2013) 151(1–3):133–40. 10.1016/j.schres.2013.10.028 [DOI] [PubMed] [Google Scholar]
- 85.Glahn DC, Almasy L, Blangero J, Burk GM, Estrada J, Peralta JM, et al. Adjudicating neurocognitive endophenotypes for schizophrenia. Am J Med Genet B Neuropsychiatr Genet (2007) 144B(2):242–9. 10.1002/ajmg.b.30446 [DOI] [PubMed] [Google Scholar]
- 86.Turner JA, Damaraju E, van Erp TG, Mathalon DH, Ford JM, Voyvodic J, et al. A multi-site resting state fMRI study on the amplitude of low frequency fluctuations in schizophrenia. Front Neurosci (2013) 7:137. 10.3389/fnins.2013.00137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lui S, Li T, Deng W, Jiang L, Wu Q, Tang H, et al. Short-term effects of antipsychotic treatment on cerebral function in drug-naive first-episode schizophrenia revealed by “resting state” functional magnetic resonance imaging. Arch Gen Psychiatry (2010) 67(8):783–92. 10.1001/archgenpsychiatry.2010.84 [DOI] [PubMed] [Google Scholar]
- 88.Hoptman MJ, Zuo XN, Butler PD, Javitt DC, D’Angelo D, Mauro CJ, et al. Amplitude of low-frequency oscillations in schizophrenia: a resting state fMRI study. Schizophr Res (2010) 117(1):13–20. 10.1016/j.schres.2009.09.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pol HEH, Schnack HG, Mandl RC, van Haren NE, Koning H, Collins DL, et al. Focal gray matter density changes in schizophrenia. Arch Gen Psychiatry (2001) 58(12):1118–25. 10.1001/archpsyc.58.12.1118 [DOI] [PubMed] [Google Scholar]
- 90.McCarley RW, Faux SF, Shenton ME, Nestor PG, Adams J. Event-related potentials in schizophrenia: their biological and clinical correlates and new model of schizophrenic pathophysiology. Schizophr Res (1991) 4(2):209–31. 10.1016/0920-9964(91)90034-O [DOI] [PubMed] [Google Scholar]
- 91.Pearlson GD, Barta PE, Powers RE, Menon RR, Richards SS, Aylward EH, et al. Medial and superior temporal gyral volumes and cerebral asymmetry in schizophrenia versus bipolar disorder. Biol Psychiatry (1997) 41(1):1–14. 10.1016/S0006-3223(96)00373-3 [DOI] [PubMed] [Google Scholar]
- 92.Giuliani NR, Calhoun VD, Pearlson GD, Francis A, Buchanan RW. Voxel-based morphometry versus region of interest: a comparison of two methods for analyzing gray matter differences in schizophrenia. Schizophr Res (2005) 74(2–3):135–47. 10.1016/j.schres.2004.08.019 [DOI] [PubMed] [Google Scholar]
- 93.Barta PE, Pearlson GD, Powers RE, Richards SS, Tune LE. Auditory hallucinations and smaller superior temporal gyral volume in schizophrenia. Am J Psychiatry (1990) 147(11):1457–62. 10.1176/ajp.147.11.1457 [DOI] [PubMed] [Google Scholar]
- 94.Calhoun VD, Kiehl KA, Liddle PF, Pearlson GD. Aberrant localization of synchronous hemodynamic activity in auditory cortex reliably characterizes schizophrenia. Biol Psychiatry (2004) 55(8):842–9. 10.1016/j.biopsych.2004.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Meda SA, Wang Z, Ivleva EI, Poudyal G, Keshavan MS, Tamminga CA, et al. Frequency-specific neural signatures of spontaneous low-frequency resting state fluctuations in psychosis: evidence from bipolar-schizophrenia network on intermediate phenotypes (B-SNIP) consortium. Schizophr Bull (2014) 41(6):1336–48. 10.1093/schbul/sbv064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ren W, Lui S, Deng W, Li F, Li M, Huang X, et al. Anatomical and functional brain abnormalities in drug-naive first-episode schizophrenia. Am J Psychiatry (2013) 170(11):1308–16. 10.1176/appi.ajp.2013.12091148 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.