Abstract
Introduction:
Dyslipidemia is one of the most common risk factor for cardiac-related disorders in diabetes mellitus. Diabetic dyslipidemia is characterized by hypertriglyceridemia, low high density lipoprotein and elevated low density lipoprotein concentration.
Aim:
To explore the effect of Lawsonia inermis hydroalcoholic extract (LIHE) for diabetic dyslipidemic activity along with its safety profile.
Materials and Methods:
LIHE administered at doses of 100, 200 and 400 mg/kg in rats after induction of hyperglycemia by alloxan. Insulin (1 IU/kg), glibenclamide (2.5 mg/kg), and metformin (100 mg/kg) were used as positive control and 1% gum acacia as normal control. Statistical analysis was performed using one-way analysis of variance, followed by Dunnett's t-test.
Results:
The percentage reduction in blood glucose level of LIHE at dose of 400 mg/kg was 39.08% on day 21 when compared to baseline (day 0), which is comparable to glibenclamide (44.77%) and metformin (46.30%). Decrease in blood glucose level exhibited significant improvement in lipid profile, plasma albumin, total plasma protein and serum creatinine.
Conclusion:
Results of this study demonstrated that LIHE significantly improved lipid and lipoprotein pattern observed in diabetic rats and this could be due to improvement in insulin secretion or action, thus has potential to be used in treatment of diabetes mellitus associated dyslipidemia.
Keywords: Alloxan, anti-dyslipidemic, anti-hyperglycemic, Lawsonia inermis, metformin
Introduction
Diabetes mellitus is a metabolic disorder constituting a major health concern today whose prevalence has continuously increased worldwide over the past few decades. Moreover, it has been considered as an incurable metabolic disorder affecting about 4.4% of the global population.[1] It is primarily characterized by chronic hyperglycemia with disturbances of carbohydrate, fat and protein metabolism resulting from defects in insulin secretion, insulin action, or both.[2,3] Despite the availability of conventional anti-diabetic drugs and insulin, morbidity and mortality due to complications of diabetes is high. Furthermore, cost and adverse effects like hypoglycemia are major issues for anti-diabetic drugs. Hence, the search of new drugs for diabetes mellitus associated dyslipidemia continues along traditional and alternative medicine, which should be more effective with fewer adverse effects.[4]
Lawsonia inermis Linn. (known as Madayantika in Ayurveda) is an herbaceous member of the Lythraceae family.[5,6] Different parts of L. inermis have been widely used in Ayurvedic system of medicine for the treatment of bleeding disorders, ulcers, eczema, skin disorders.[7,8] The reported biological properties of L. inermis are anti-hyperglycemic,[9] immunomodulatory effect,[10] hepatoprotective[11] and memory enhancing activity.[12] The methanolic (95%) extract of leaves from L. inermis showed significant in-vitro anti-hyperglycemic effect.[13] Ethanolic (70%) extract of L. inermis showed significant hypoglycemic activities in alloxan-induced diabetic mice. L. inermis extract at dose of 0.8 g/kg decreased the concentration of glucose, cholesterol, and triglycerides to normal. The present study was thus designed to evaluate the diabetes associated anti-dyslipidemic efficacy of L. inermis hydroalcoholic extract (LIHE) in alloxan-induced diabetic male Wistar rats.
Materials and Methods
Plant material
The leaves of L. inermis were obtained from the Herb Suppliers in Delhi, India. The leaves were identified and authenticated at Department of Pharmacognosy and Phytochemistry, Faculty of Pharmacy, Hamdard University, New Delhi. A voucher specimen (No. NK/011/2012) was deposited in the laboratory for future references.
Extraction
Dried and pulverized leaves (400 g) of L. inermis were extracted by cold maceration with 50% v/v methanol for 72 h with solvent changes at every 24 h (5 L solvent/per change). The collected solvent was decanted, pooled together and filtered through tightly packed cotton wool to remove suspended particulate matter. The solvent was then evaporated at 40°C under reduced pressure (Buchi R-220 Rotary Evaporator) till a semisolid residue was obtained.
Animals
Male Wistar rats, of approximately same age (12–14 weeks old), weighing about 150–180 g, obtained from Central Animal Facility, AIIMS, New Delhi were used for the study. They were housed in polypropylene cages at 23 ± 2°C with a 45–55% of relative humidity and exposed to alternate cycles of 12 h light and darkness. The animals were allowed to adapt to the environment for a week prior to experimentation with free access to water and standard diet for laboratory animals. Before experimentation, animals were kept on fasting overnight with free access to water. The experimental protocol was reviewed and approved by the Institutional Animal Ethics Committee (IAEC), All India Institute of Medical Sciences, New Delhi, India (IAEC approval no. IAEC/597/2010 dated 3rd May 2011).
Chemicals
Alloxan was purchased from Sigma–Aldrich Co., St. Louis, MO, USA and insulin from Novo Nordisk, Denmark. All the biochemicals used in this study were obtained from E. Merck (India) Pvt. Ltd., Mumbai, and were of analytical grade.
Acute toxicity (LD50) test
The acute oral toxicity test (LD50) of LIHE was performed as per Organization for Economic Cooperation and Development (OECD-425) Guidelines.[13] A limit test (2000 mg/kg body weight) was done for hydroalcoholic extract by using five male Wistar rats (150–180 g). Animals were administered a dose of 2000 mg/kg body weight of the extract and observed for signs of mortality for a period of 48 h.
Twenty-eight day sub-acute oral toxicity study
Evaluation of 28 days oral toxicity of the extract was carried out according to OECD Guidelines for testing of chemicals-407.[14] Two groups of Wistar rats of both sexes (n = 10, five female and five male rats) were used in the study. Group I received vehicle (2 ml/kg, 1% gum acacia orally) and served as normal control, group II received LIHE (1200 mg/kg orally). Vehicle/test was administered daily for 28 days. Body weight was recorded on days 1, 7, 14, 21, and 28. At the end of 28 days, rats were sacrificed after an overnight fasting, under diethyl ether anesthesia. Blood was collected for hematological and biochemical analysis through the retro-orbital sinus. The liver, kidney and heart were harvested immediately, and organ weights were measured. The liver and kidney were then fixed in 10% formalin for histopathological examination.
Alloxan induced hyperglycemia
Eight groups of male Wistar albino rats (n = 6) were used in the study. Animals were fasted overnight with free access to water before the experiment. The rats were treated with a single dose of 120 mg/kg alloxan monohydrate (intraperitoneal injection), dissolved in normal saline and was injected immediately within few minutes to avoid degradation. 5% glucose solution was given overnight to the animals to prevent hypoglycemia. The development of hyperglycemia in rats was confirmed by estimating blood glucose level, 72 h post alloxan injection. The rats with blood glucose level above 200 mg/dL were considered diabetic, and only diabetic rats were included in the study. Thereafter group I received 2 ml/kg 1% gum acacia suspension and served as the normal control, group II served as diabetic control (vehicle-treated diabetic rats) and groups III, IV and V received LIHE at doses of 100, 200 and 400 mg/kg body weight, respectively by oral gavage. Groups VI, VII and VIII received insulin (1 IU/kg), glibenclamide (2.5 mg/kg) and metformin (100 mg/kg) and served as a positive control. Vehicle, LIHE, insulin, glibenclamide, and metformin were administered once daily for 21 days from the day of the start of the experiment. Blood samples were taken on day 0, 7, 14, and 21 by puncturing the retro-orbital sinus under mild ether anesthesia for hematological and biochemical estimation.[15]
Oral glucose tolerance test in rats
Animals were divided into eight groups (n = 6) and were fasted overnight with free access to water ad libitum. Group I received 1% gum acacia (2 ml/kg) and served as normal control, group II served as diabetic control (glucose at a dose of 2 g/kg). In groups III, IV and V, rats were fed with glucose (2 g/kg), 30 min after the administration of LIHE (100, 200 and 400 mg/kg) respectively. Thereafter, groups VI, VII and VIII received glucose (2 g/kg), 30 min after the administration of insulin (1 IU/kg), glibenclamide (2.5 mg/kg) and metformin (100 mg/kg) and served as positive control. Blood samples were taken from the retro-orbital sinus under mild ether anesthesia at 30, 60, 90, and 120 min of glucose administration on the end of 21st day. Blood samples were centrifuged at 2000 rpm and serum was separated from each sample. All animals were then sacrificed, and their liver and kidney were preserved in 10% neutral buffered formalin for histopathological examination.[16]
Biochemical assays
Stored serum samples were analyzed for glucose level on days 0, 7, 14, and 21 using the kits available from Vital Diagnostics (P) Ltd., India. Estimation of serum total cholesterol (TCH), serum triglyceride, serum high density lipoprotein (HDL), total plasma protein (TP), plasma albumin and serum creatinine was done on days 0, 7, 14, and 21 using the method described by Friedewald's formula, 1972.[17]
Statistical analysis
Statistical analysis was performed using GraphPad InStat software, Inc. CA 92037 USA. Data obtained were expressed as mean ± standard error of the mean. The data were analyzed using one-way analysis of variance, and the group mean were compared by Dunnett's multiple comparisons. Values were considered as statistically significant at P < 0.05.
Results
Results of toxicity studies showed that in LIHE treated group, >50% of the animals survived, which concludes that the oral LD50 of the plant extract is more than 2000 mg/kg body weight. In sub-acute oral toxicity study, no abnormalities were seen in hematological parameters and biochemical parameters in 28 days of the administration of LIHE. However, bleeding time showed a significant increase in LIHE treated group compared with normal control. The treatment of LIHE in sub-acute toxicity study did not show any significant toxicological changes as observed by histopathological examination in liver and kidney tissues.
LIHE in the doses of 100 mg/kg and 200 mg/kg did not reduce blood glucose levels significantly in alloxan-diabetic rats as compared to diabetic control rats which signify that these doses are not efficacious in reducing elevated blood glucose in diabetic rats. The higher dose of 400 mg/kg of LIHE significantly (P < 0.01) reduced blood glucose levels in alloxan-induced diabetic rats when compared to diabetic control [Table 1]. The percentage reduction of blood glucose at 400 mg/kg dose was 39.08% on day 21 as compared to base line (day 0), which is comparable to glibenclamide (44.77%) and metformin (46.30%), thus LIHE may act by potentiating the secretion of insulin from intact pancreatic β-cells or by increasing the consumption of glucose in peripheral tissues, or by both. In oral glucose tolerance test, LIHE treatment also showed significant improvement in glucose tolerance with a decrease in blood glucose started from 60 min of administration of LIHE [Figure 1]. A significant decrease in TCH, triglycerides, low-density lipoprotein (LDL), and very LDL (VLDL) levels, and an increase in HDL level were seen [Table 2] and a significant increase in plasma albumin and TP were also observed [Table 3]. Histological examination of liver and kidney did not reveal any pathological changes in sub-acute toxicity study [Figure 2 and 3].
Table 1.
Effect of LIHE on fasting blood glucose in alloxan-induced diabetic Wistar rats
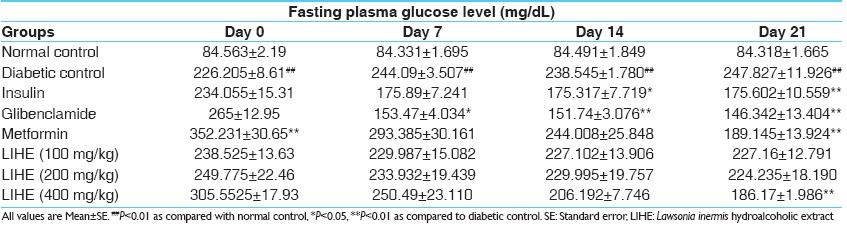
Figure 1.
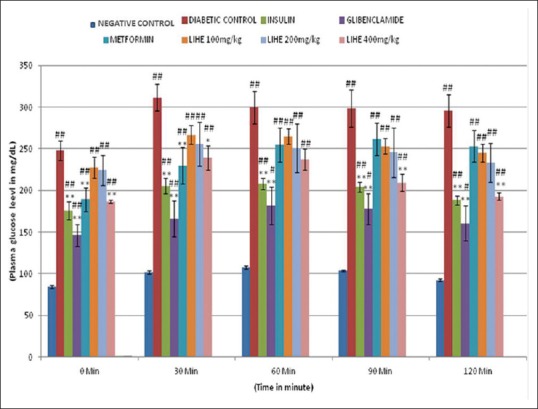
Effect of Lawsonia inermis hydroalcoholic extract on glucose tolerance test in alloxan-induced diabetic Wistar rats. All values are mean ± standard error #P < 0.05, ##P < 0.01 as compared with positive control; *P < 0.05, **P < 0.01 as compared to diabetic control
Table 2.
Effect of LIHE on serum lipid profile in alloxan-induced diabetic Wistar rats
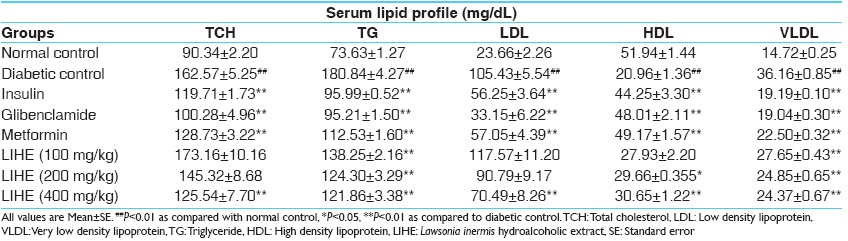
Table 3.
Effect of LIHE extract on plasma albumin, total plasma protein and serum creatinine level in alloxan-induced diabetic Wistar rats
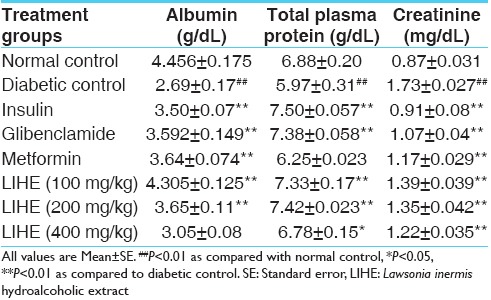
Figure 2.
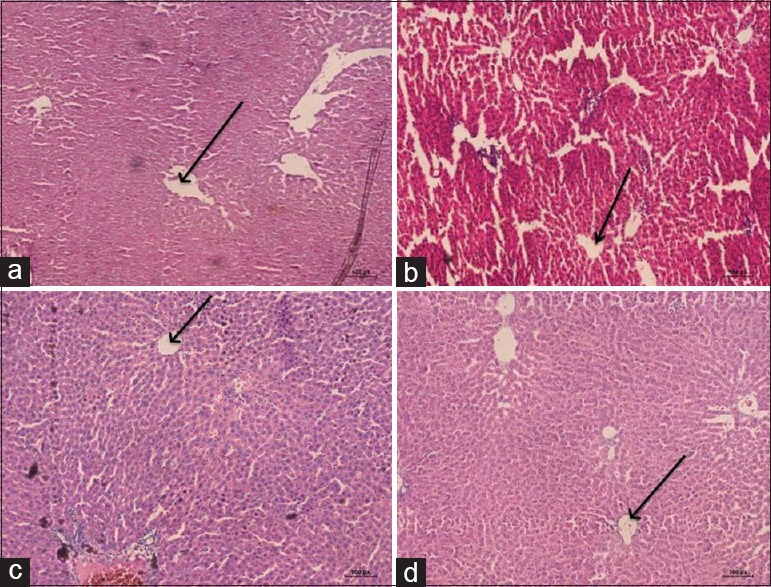
Photomicrographs were taken at magnification (×10). (a) Photomicrographs demonstrated intact cellular architecture of liver in normal control rat. (b) Distortion of cellular architecture with swelling of hepatocytes of liver diabetic control rat and (c-d) partial restoration of normal cellular architecture of liver by insulin and Lawsonia inermis hydroalcoholic extract 400 mg/kg
Figure 3.
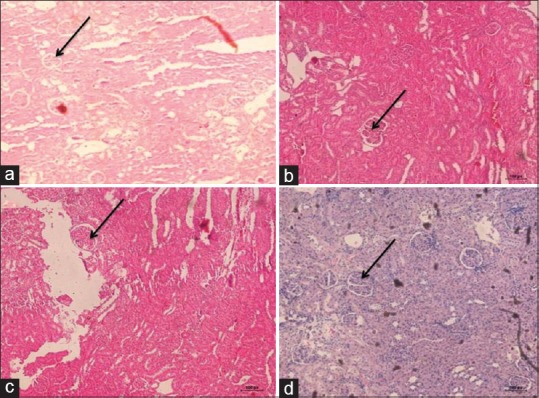
Photomicrographs were taken at magnification (×10). (a) Photomicrographs demonstrated intact cellular architecture of kidney in normal control rat. (b) Distortion of cellular architecture with irregular glomeruli in kidney in diabetic control rat and (c-d) Partial restoration of normal cellular architecture of kidney by insulin and Lawsonia inermis hydroalcoholic extract 400 mg/kg
Discussion
Alloxan (2,4,5,6-tetraoxypyrimidine) is a toxic glucose analogue, which selectively causes destruction of pancreatic β-cells, provoking a state of primary deficiency of insulin and thus producing a hyperglycemic condition.[18] It has been used as an experimental agent to induce diabetes mellitus in Wistar rats but due to the reported high incidence of ketosis and resulting mortality, low dose (120 mg/kg) of this agent was used. The animals developed significant hyperglycemia, hyperlipidemia, and other symptoms of uncontrolled diabetes mellitus within 72 h of administration of alloxan and this persisted till the end of the experimental period of 21 days.[19] The animals also showed increased serum creatinine, decreased plasma albumin and TP, most probably due to muscle wasting or due to complications associated with diabetes mellitus. Plasma albumin concentration is a predictor of hemoglobin A1c among type II diabetic patient. In present study, the blood sugar level was increased subsequent to alloxan administration, due to excess production of reactive oxygen species leading to cytotoxicity in pancreatic β-cells which reduces the synthesis and release of insulin, while affecting organs such as liver, kidney, pancreas and hemopoitic system.[20] The findings of the study revealed that LIHE treatment significantly reduced the blood glucose level and serum lipid level in the diabetic-treated rats. The reduction in glucose level may be due to insulin release that was impaired due to pancreatic beta-cell destruction by alloxan.
In addition to altered glucose homeostasis in diabetic rats, dyslipidemia was evident by increased triglycerides, TCH, LDL and by decreased HDL levels.[21] The significant reduction in triglyceride and cholesterol levels of LIHE-treated rats indicates its beneficial effect on fat metabolism, thus improving dyslipidemia. Hyperlipidemia is mostly coupled with hyperglycemia. High levels of triglycerides and LDL cholesterol are associated with high risk of coronary dysfunction, whereas increase in HDL cholesterol is associated with a decrease in coronary risk.[22] The main cause of the lipid changes associated with diabetic dyslipidemia is the increased free fatty-acid release from insulin-resistant fat cells.[23,24] The increased flux of free fatty acids into the liver in the presence of adequate glycogen stores promotes triglyceride production, which in turn stimulates the secretion of apolipoprotein B and VLDL cholesterol. Thus, the continuous treatment of diabetic rats with L. inermis for a period of 21 days normalizes all the parameters attributing the anti-dyslipidemic activity of plant. This could be due to the presence of some biomolecules present in the plant extract that might have stimulated the beta cells of Langerhans to release insulin, leading to the improvement in the carbohydrate metabolizing enzymes and thus establishing normal blood glucose level.[25]
The probable mechanism behind hypolipidemic action in diabetic rat may be by potentiating the insulin effect of plasma by increasing either the pancreatic secretion of insulin from the existing beta cells or by its release from the bound form. In recent years, considerable interest has been directed towards the investigation of plasma lipids and lipoprotein pattern in diabetes mellitus due to the fact that abnormal lipid level leads to the development of coronary artery disease in diabetic patients.
Conclusion
Lawsonia inermis hydroalcoholic extract showed significant anti-hyperlipidemic effects in diabetic rats, thus endorsing its potential to be used in treatment of diabetes mellitus. The observed effects emphasize the importance of isolating the active molecule (s) from the hydroalcoholic leaf extract of L. inermis and explore the possible mechanism of its anti-hyperlipidemic activity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.Nathan DM. Long-term complications of diabetes mellitus. N Engl J Med. 1993;328:1676–85. doi: 10.1056/NEJM199306103282306. [DOI] [PubMed] [Google Scholar]
- 3.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 4.Rates SM. Plants as source of drugs. Toxicon. 2001;39:603–13. doi: 10.1016/s0041-0101(00)00154-9. [DOI] [PubMed] [Google Scholar]
- 5.Gupta AK. Vol. 1. New Delhi: Indian Council of Medical Research; 2003. Quality Standards of Indian Medicinal Plants; p. 23. [Google Scholar]
- 6.Chopra RN, Nayer SL, Chopra IC. New Delhi: CSIR Publications; 1956. Glossary of India Medicinal Plants. [Google Scholar]
- 7.Part-I. IV. New Delhi: Department of AYUSH, Ministry of Health and Family Welfare, Govt. of India; 1996. Anonymous. The Ayurvedic Pharmacopeia of India; pp. 64–6. [Google Scholar]
- 8.Nadkarni KM. I. Bombay, India: Popular Book Depot; 1982. India Materia Medica; pp. 730–73. [Google Scholar]
- 9.Mikhaeil BR, Badria FA, Maatooq GT, Amer MM. Antioxidant and immunomodulatory constituents of henna leaves. Z Naturforsch C. 2004;59:468–76. doi: 10.1515/znc-2004-7-803. [DOI] [PubMed] [Google Scholar]
- 10.Hemalatha K, Natraj HN, Kiran AS. Hepatoprotective activity of leaves of Lawsonia alba. Indian J Nat Prod. 2004;20:14–7. [Google Scholar]
- 11.Iyer MR, Pal SC, Kasture VS, Kasture SB. Effect of Lawsionia inermis on memory and behaviour mediated via monoamine neurotransmitters. Indian J Pharmacol. 1998;30:181–5. [Google Scholar]
- 12.Arayne MS, Sultana N, Mirza AZ, Zuberi MH, Siddiqui FA. In vitro hypoglycemic activity of methanolic extract of some indigenous plants. Pak J Pharm Sci. 2007;20:268–73. [PubMed] [Google Scholar]
- 13.OECD 2001, OECD-Guidelines for testing of chemicals-425, organization for economic corporation and development: Paris. [Last accessed on 2014 May 29]. Available from: http://www.OECDLibrary.org/content/package/chem_guide_pkg-en .
- 14.OECD 2008, OECD-Guidelines for testing of chemicals-407, organization for economic corporation and development: Paris. [Last accessed on 2014 May 29]. Available from: http://www.OECDLibrary.org/content/package/chem_guide_pkg-en .
- 15.González Mosquera DM, Hernandez Ortega Y, By B, Vicet Muro L, Saucedo Hernandez Y, Grau Ábalos R, et al. Antihyperglycemic activity of extracts from Boldoa purpurascens leaves in alloxan-induced diabetic rats. Phytother Res. 2013;27:721–4. doi: 10.1002/ptr.4769. [DOI] [PubMed] [Google Scholar]
- 16.Sharma N, Garg V. Antidiabetic and antioxidant potential of ethanolic extract of Butea monosperma leaves in alloxan-induced diabetic mice. Indian J Biochem Biophys. 2009;46:99–105. [PubMed] [Google Scholar]
- 17.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 18.Aruna RV, Ramesh B, Kartha VN. Effect of betacarotene on protein glycosylation in alloxan induced diabetic rats. Indian J Exp Biol. 1999;37:399–401. [PubMed] [Google Scholar]
- 19.Edem DO. Hypoglycaemic effects of ethanolic extracts of alligator pear seed (Persea Americana Mill) in rats. Eur J Sci Res. 2009;33:669–78. [PubMed] [Google Scholar]
- 20.Sabu MC, Kuttan R. Anti-diabetic activity of medicinal plants and its relationship with their antioxidant property. J Ethnopharmacol. 2002;81:155–60. doi: 10.1016/s0378-8741(02)00034-x. [DOI] [PubMed] [Google Scholar]
- 21.Mooradian AD. Dyslipidemia in type 2 diabetes mellitus. Nat Clin Pract Endocrinol Metab. 2009;5:150–9. doi: 10.1038/ncpendmet1066. [DOI] [PubMed] [Google Scholar]
- 22.Alam S, Reddy SK, Baig A, Reddy MK, Mohiuddin M, Reddy MV, et al. Evaluation of anti-diabetic and anti-lipidimic potential of kalongi sugar powder water extract in STZ induced diabetic rats. Int J Pharm Pharm Sci. 2013;5:94–6. [Google Scholar]
- 23.Del Pilar Solano M, Goldberg RB. Management of diabetic dyslipidemia. Endocrinol Metab Clin North Am. 2005;34:1–25, v. doi: 10.1016/j.ecl.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 24.Chahil TJ, Ginsberg HN. Diabetic dyslipidemia. Endocrinol Metab Clin North Am. 2006;35:491–510, vii. doi: 10.1016/j.ecl.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 25.Hossain MS, Alam MB, Asadujjaman M, Islam MM, Rahman MA, Islam MA, et al. Antihyperglycemic and antihyperlipidemic effects of different fractions of Stevia rebaudiana leaves in alloxan induced diabetic rats. Int J Pharm Sci Res. 2011;2:1722–9. [Google Scholar]


