Figure 1. Schematic representation of sequential immune mechanisms leading to desensitization state during AIT.
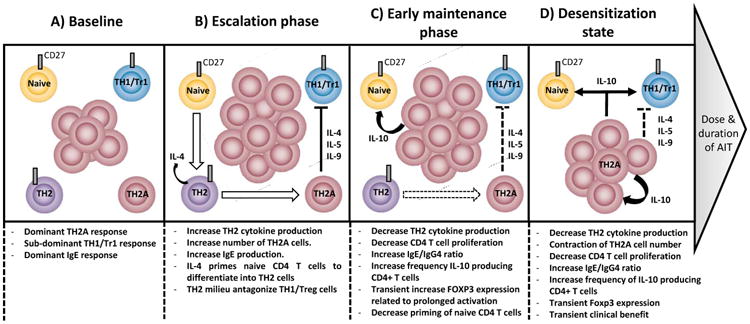
At baseline (A), CD27 expression distinguishes pro-allergic TH2 (TH2A) cell subset from non-pathogenic (CD27+) allergen-specific T cell subset in allergic subjects. While low frequency of CD27(+) allergen-specific TH1/Tr1 cell subset can be observed both in allergic and non-allergic individuals, allergen-specific TH2A cells (CD27-) are confined to allergic individuals and dominate the allergen-specific T cell response. Some CD27(+) allergen-specific TH2 cells (IL-4+) may differentiate from the naïve T cell pool to serve as reservoir to replenished TH2A cells (IL-4+, IL-5+, IL-9+) following chronic allergen challenge. Similar to natural allergen exposure, first low dose exposure to the allergen during escalation phase (B) leads to an increase of allergen-specific TH2A cell response and production of related specific-IgE. This dominant pro-allergic TH2 functional activity antagonizes the induction of regulatory T cells. Early maintenance phase (C) rapidly establishes a negative auto-regulatory feedback loop to prevent excessive pro-allergic TH2 responses.;these in turn drive a desensitization state (D) via decreased TH2 cell activity, IL-10 production and change in the IgE/IgG4 ratio. At this stage, if treatment is not continued long enough, the initial pathogenic feature of CD27(-) allergen-specific T cells may gradually recover after treatment discontinuation.
