Abstract
Objective
To examine associations of chronic insufficient sleep with diet, and whether diet explains the sleep-adiposity relationship.
Methods
In Project Viva, 1,046 parents reported children’s sleep duration at 6m and annually until mid-childhood (7y). The main exposure was a sleep curtailment score (6m–7y) ranging from 0 (maximal curtailment) to 13 (adequate sleep). In mid-childhood, parents reported children’s diet; researchers measured height/weight. Multivariable linear regression assessed associations of sleep with diet (Youth Healthy Eating Index [YHEI]); sleep with BMI z-score adjusting for YHEI; and, secondarily, joint associations of sleep and YHEI with BMI.
Results
Mean (SD) sleep and YHEI scores were 10.21 (2.71) and 58.76 (10.37). Longer sleep duration was associated with higher YHEI in mid-childhood (0.59 points/unit sleep score; 95%CI: 0.32, 0.86). Though higher YHEI was associated with lower BMI z-score (−0.07 units/10-point increase; 95%CI: −0.13, −0.01), adjustment for YHEI did not attenuate sleep-BMI associations. Children with sleep and YHEI scores below the median (<11 and <60) had BMI z-scores 0.34 units higher (95%CI: 0.16, 0.51) than children with sleep and YHEI scores above the median.
Conclusions
While parent-reported diet did not explain inverse associations of sleep with adiposity, both sufficient sleep and high-quality diets are important to obesity prevention.
Keywords: sleep curtailment, diet quality, early childhood, obesity
Introduction
Early childhood is a critical period for obesity prevention: dietary behaviors and weight trajectories established in early childhood often carry forward into later years. (1, 2, 3) One influential behavior may be sleep: many studies support an association of shorter sleep duration (4, 5, 6) and chronic insufficient sleep (7) with risk of childhood obesity in diverse populations with parent-reported and actigraph-measured sleep. (8, 9, 10, 11) Yet, the underlying mechanisms remain unclear.
Lower diet quality is one proposed pathway through which inadequate sleep may lead to adiposity. In adults, experimentally restricting sleep alters appetite hormones and changes in hunger ratings, energy intake and food preferences. (12, 13) Recently, functional magnetic resonance imaging studies suggest disinhibited eating and altered food selection in a sleep-deprived state. (14, 15) Outside the laboratory, epidemiologic evidence supports a cross-sectional relationship of shorter sleep with lower diet quality and altered appetite hormones in children (16) and adults. (17) However, since children often have less autonomy in food choice, (18) findings in older populations may not apply. A recent prospective study found that compared to parent-reported sleep duration of 11-<12-hours/day at 16-months, children sleeping <10-hours/day consumed 50 kcal/day more at 21 months. (19) However, the authors could not examine mediation since the relationship of insufficient sleep with adiposity was not yet apparent among their young participants. Regardless of its possible role as a mediator, diet quality may have effects in combination with chronic sleep insufficiency that increase risk of childhood obesity.
This study examines chronic insufficient sleep as a predictor of diet quality in mid-childhood and whether diet explains previously observed associations of chronic insufficient sleep with mid-childhood BMI z-score. (7) As a secondary aim, we examine the joint association of low quality diet and chronic insufficient sleep with mid-childhood BMI z-score.
Methods
Subjects/Study Design
We studied participants in Project Viva, which recruited women during early pregnancy from Harvard Vanguard Medical Associates, a multi-specialty practice in eastern Massachusetts. Procedural details are available elsewhere. (20) Of the 2,128 live infants delivered, 1,116 attended a mid-childhood in-person visit. Our main exposure was chronic sleep curtailment from age 6-months to 7-years. We excluded 70 participants without sleep data for these time points for a final sample of n=1,046.
After obtaining informed consent, we performed in-person study visits with the mother and child in infancy (mean [SD] child age 6 [0.9] months), early childhood (mean [SD] 3.2 [0.3] years) and mid-childhood (mean [SD] 7.8 [0.7] years). Mothers completed mailed questionnaires at 1, 2, 4, 5, and 6 years after birth. The Institutional Review Board of Harvard Pilgrim Health Care approved the study.
Measurements
Sleep measurements
At 6-months and annually (1–7 years), mothers reported children’s 24-hour sleep duration. At 6-months and 1-year, mothers reported in hours/minutes their baby’s average length of naps and nighttime sleep in the past month. Between 2–7 years, mothers reported the child’s typical 24-hour sleep duration in the past month, separating weekends and weekdays. Response categories included, “< 9, 9, 10, 11, 12, 13, and >14-hours/day.” At 7-years response options were in hours/minutes. In a recent validation, parental report of sleep duration in children 4–6 years correlated well with actigraphy (ρ=0.85). (21)
Our primary exposure was chronic insufficient sleep as quantified by a sleep score tallying the adequacy of parent-reported sleep duration from infancy to mid-childhood. For consistency with prior research, (7, 22) the score was derived from mean sleep duration at each of 8 measurements (6-months and 1–7 years). Using sleep durations associated with elevated BMI (≥= 95th percentile), (23) and the age-specific recommendations available in 2014 from the National Sleep Foundation (24) and the National Heart, Lung and Blood Institute, (25) we scored sleep duration as follows: from 6-months to 2-years, the score was 0 for <12-hours/day and 1 for ≥=12-hours/day; from 3 to 4-years, <10-hours/day = 0, 10-<11-hours/day = 1, and ≥= 11-hours/day = 2; at 5 and 7-years, <9-hours/day = 0, 9-<10-hours/day = 1, and ≥ = 10-hours/day = 2. The range was 0 (indicating maximal sleep curtailment) to 13 (indicating never having curtailed sleep). We grouped scores into five categories, collapsing scores of 0–4, 5–7 and 8–9 due to small frequencies and 10–11 and 12–13 due to comparable results. (7, 26)
The National Sleep Foundation updated age-specific recommendations for sleep duration in 2015, after the initial development and use of the sleep curtailment score. In sensitivity analyses, re-derived the sleep score to align with the current recommendations but with the same range (0–13) as the original score described above by awarding 1.625 points if children’s sleep duration fell within the recommended ranges: 6-months, 12–15 hours 1–2 years, 11–14 hours; 3–5 years, 10–13 hours; 6–7 years, 9–11 hours.
Diet measurements
In mid-childhood, parents reported children’s dietary behaviors (times/week eating dinner with family, skipping breakfast, and consuming fast food outside the home) and intake. Dietary intake was recorded on a Prime-Screen composed of 18 Food Frequency Questionnaire (FFQ) items asking about consumption of specific food groups, including servings/day of fruits/vegetables, dairy, whole grains, snacks, and lean, red or processed meat, as well as sugary drinks (soda/fruit drinks). The Prime-Screen has not been validated for parent-report of children’s intake; in adults, the average correlation with estimates from a full FFQ over 18 food groups was 0.6. (27)
Our primary outcome was the Youth Healthy Eating Index (YHEI), a summary measure of diet developed in adolescents. (28) In addition to foods (whole grains, vegetables/fruits, dairy, lean:fatty meat ratio and drinks), the YHEI also includes multivitamins, margarine/butter, and incorporates behaviors: fried foods outside the home, eating breakfast, and family dinner. The original YHEI included 5-points for removing visible animal fat; this information was not available for a theoretical range of 0–95 rather than 0–100 points. The YHEI awards up to 10-points for favorable consumption of whole grains, vegetables, fruits, dairy, lean:fatty meat ratio, less consumption of sweet/salty snack foods and soda/drinks, and up to 5-points for multivitamins, eating breakfast and family dinner and less consumption of margarine/butter and fried foods outside the home. Further description of the YHEI and components is in Table S1.
Demographic and anthropometric measurements
At enrollment, we collected information about maternal age and education, and household income. In early childhood, parents reported the child’s race/ethnicity. In mid-childhood, we measured height/weight using a calibrated stadiometer (Shorr Productions, Olney, MD) and scale (Seca model 881, Seca Corporation, Hanover, MD). We calculated age/sex-specific BMI z-scores using national reference data.
Statistical Analysis
Multiple imputation
Confounding variables were not available for all subjects (e.g. race/ethnicity, n=59 and income, n= 84); we used multiple imputations to generate plausible values for each missing value. We replicated analyses across 50 completed datasets and combined multivariable modeling results from the 50 datasets (Proc MI ANALYZE) in SAS version 9.3 (SAS Institute, Cary NC), which recovers information in partially observed subjects erroneously presuming imputed values are known true values.
Primary analyses
Our primary analysis examined associations of the sleep curtailment score as a predictor of mid-childhood dietary factors. All multivariable linear regression models adjusted for socio-demographic factors (child race/ethnicity, age and sex, maternal education and income). Models with a mid-childhood dietary factor as the main outcome were adjusted for all other dietary factors in mid-childhood, except for our summary measure of diet, YHEI.
Prior research in Project Viva demonstrated associations of the sleep score with mid-childhood BMI z-score. (7) To assess whether diet plays a mediating role, we examined the sleep score as a predictor of mid-childhood BMI z-score in multivariable linear regression models, with/without adjustment for mid-childhood dietary factors; the degree of attenuation in the sleep score coefficient was inferred as mediation by diet.
Supplemental analyses
In supplemental analyses, we assessed joint associations of chronic insufficient sleep and diet quality with BMI z-score. We cross-classified participants according to their sleep (≥ versus < 11, the median score), and diet quality in mid-childhood (YHEI: ≥ 60 versus < 60, the median score), and entered these four categories as predictors of BMI z-score in multivariable-adjusted models; children above the median score for both sleep and diet were the reference. We also examined mutually-adjusted associations of mid-childhood dietary factors as predictors of mid-childhood BMI z-score. All models adjusted for socio-demographic factors.
Sensitivity analyses
In sensitivity analyses, we restricted to non-Hispanic white children with college-educated mothers and considered additional adjustment for maternal pre-pregnancy BMI. Neither sensitivity analysis materially altered point estimates for the sleep score’s association with mid-childhood BMI z-score or diet quality.
Results
The mean (SD, range) was for the sleep score 10.21 (2.71, 0 – 13) and for the YHEI score was 58.76 (10.37, 30 – 91). Table 1 shows characteristics by category of sleep curtailment. Children with longer duration of sleep during childhood (higher sleep scores), were more likely to be non-Hispanic white, have college-educated mothers and live in households with incomes ≥ > $70,000/year. In mid-childhood, children with higher sleep scores had lower BMI z-scores and higher YHEI diet quality scores.
Table 1.
Participant Characteristics by Sleep Curtailment Category (N=1,046)
| Characteristic | Sleep curtailment score: 0=maximal curtailed sleep to 13=never curtailed sleep | ||||
|---|---|---|---|---|---|
| 0 to 4 41 (4%) |
5 to 7 129 (12%) |
8 to 9 151 (15%) |
10 to 11 306 (29%) |
12 to 13 419 (40%) |
|
| Mean (SD) or N (%) | |||||
| Sleep curtailment score | 3.20 (1.30) | 6.09 (1.02) | 8.61 (0.65) | 10.59 (0.62) | 12.46 (0.54) |
| Maternal/Household Characteristics | |||||
| College graduate, % | 14 (34) | 62 (49) | 95 (62) | 233 (76) | 337 (81) |
| Household income >70k/year, % | 11 (27) | 60 (47) | 81 (54) | 205 (67) | 311 (74) |
| Child Characteristics | |||||
| Race/ethnicity, % | |||||
| Asian | 2 (4) | 7 (5) | 6 (4) | 10 (3) | 10 (2) |
| Black | 15 (36) | 43 (33) | 42 (28) | 39 (13) | 17 (4) |
| Hispanic | 4 (9) | 11 (8) | 6 (4) | 6 (2) | 10 (2) |
| Other | 12 (29) | 19 (15) | 17 (11) | 38 (12) | 39 (9) |
| Non-Hispanic White | 9 (21) | 49 (38) | 81 (54) | 213 (70) | 343 (82) |
| Female, % | 23 (57) | 51 (39) | 74 (49) | 151 (49) | 226 (54) |
| Sleep duration, hours/day | |||||
| 6 months | 10.17 (2.42) | 11.00 (2.17) | 11.46 (2.47) | 12.17 (1.96) | 13.09 (1.65) |
| 1 year | 10.64 (2.31) | 11.63 (2.19) | 12.20 (1.90) | 12.73 (1.67) | 13.47 (1.24) |
| 2 years | 10.12 (1.44) | 10.71 (1.39) | 11.43 (1.38) | 12.02 (1.14) | 12.61 (0.84) |
| 3 years | 9.53 (1.26) | 9.97 (1.24) | 10.67 (1.40) | 11.18 (1.12) | 11.82 (0.83) |
| 4 years | 9.37 (0.96) | 9.85 (1.14) | 10.37 (1.12) | 10.78 (1.06) | 11.36 (0.83) |
| 5 years | 8.88 (1.42) | 9.82 (1.58) | 10.24 (1.27) | 10.63 (1.06) | 11.03 (0.96) |
| 6 years | 8.85 (1.33) | 9.47 (1.28) | 9.98 (1.11) | 10.31 (1.06) | 10.65 (0.78) |
| 7 years | 8.26 (1.04) | 8.99 (1.13) | 9.44 (1.04) | 9.93 (0.81) | 10.32 (0.59) |
| Mid-Childhood, 7-Year Visit | |||||
| BMI z-score | 0.98 (1.03) | 0.57 (1.03) | 0.49 (0.96) | 0.36 (1.00) | 0.21 (0.93) |
| Television, hours/day | 2.35 (1.43) | 2.00 (1.36) | 1.70 (1.20) | 1.52 (1.02) | 1.28 (0.83) |
| Family dinner, times/week | 4.93 (2.46) | 5.01 (2.41) | 5.48 (2.29) | 5.52 (2.06) | 5.78 (1.73) |
| Skipping breakfast, times/week | 0.61 (1.22) | 0.54 (1.45) | 0.32 (1.09) | 0.25 (0.97) | 0.19 (0.77) |
| Fast food, servings/week | 0.82 (0.91) | 0.88 (1.13) | 0.72 (0.90) | 0.70 (0.87) | 0.62 (0.72) |
| Youth Healthy Eating Index | 54.39 (13.63) | 54.49 (11.23) | 57.5 (11.12) | 58.81 (10.08) | 60.92 (10.80) |
| Fruit, servings/day | 1.20 (1.14) | 1.29 (1.32) | 1.60 (1.58) | 1.69 (1.45) | 1.70 (1.32) |
| Vegetables, servings/day | 1.22 (1.26) | 1.18 (1.08) | 1.29 (1.02) | 1.35 (0.90) | 1.35 (0.94) |
| Whole grains, servings/day | 0.55 (0.65) | 0.66 (0.86) | 0.76 (0.95) | 0.79 (0.90) | 0.97 (0.98) |
| Total dairy, servings/day | 1.97 (1.63) | 1.92 (1.66) | 2.12 (1.73) | 2.47 (1.74) | 2.40 (1.54) |
| Red/processed meats, servings/day | 0.50 (0.64) | 0.54 (0.67) | 0.47 (0.44) | 0.55 (0.48) | 0.49 (0.44) |
| Sweet/salty snacks, servings/day | 0.26 (0.38) | 0.38 (0.50) | 0.29 (0.36) | 0.38 (0.39) | 0.37 (0.34) |
| Sugary drinks, servings/day | 0.68 (1.18) | 0.57 (1.09) | 0.43 (0.96) | 0.34 (0.67) | 0.25 (0.51) |
Table 2 shows the primary results: chronic insufficient sleep from infancy to mid-childhood is associated with dietary factors in mid-childhood. Each incremental increase in the sleep score (indicating more adequate sleep duration) was associated with more favorable dietary intake (indicated by the YHEI). The mean difference in the YHEI per 1-unit increase in the sleep score was 0.59 points; 95% Confidence Interval [95%CI]: 0.32, 0.86. Components of the YHEI were modestly associated with the sleep score, as follows: whole grains (0.02 more servings/day; 95%CI: 0.00, 0.05); sugary drinks (−0.02 fewer servings/week; 95%CI: −0.04, 0.00); family dinner (0.05 more times/week; 95%CI: 0.00, 0.10); and skipping breakfast (−0.03 fewer times/week; 95%CI: −0.05, 0.00). Intake of fast food, dairy and fruits and vegetables were not associated with the sleep score.
Table 2.
Sleep Curtailment Score as a Predictor of Dietary Intake in Mid-Childhood (N=1,046)1
| Mean difference in mid-childhood dietary factor (95%CI) | ||||||
|---|---|---|---|---|---|---|
| Sleep Curtailment Score2 | ||||||
| 0 to 4 4% |
5 to 7 12% |
8 to 9 15% |
10 to 11 29% |
12 to 13 40% |
Continuous Score | |
| YHEI score3 | −4.17 (−8.29,−0.04) | −4.51 (−6.84,−2.18) | −2.16 (−4.29,−0.03) | −1.66 (−3.24,−0.08) | 0.0 (ref) | 0.59 (0.32, 0.86)* |
| Whole grains, servings/day | −0.20 (−0.50, 0.09) | −0.14 (−0.33, 0.06) | −0.11 (−0.28, 0.06) | −0.16 (−0.30,−0.03) | 0.0 (ref) | 0.02 (0.00, 0.05)* |
| Sugary drinks, servings/week | 0.18 (−0.10, 0.46) | 0.11 (−0.07, 0.28) | 0.09 (−0.05, 0.23) | 0.04 (−0.06, 0.14) | 0.0 (ref) | −0.02 (−0.04, 0.00)* |
| Family dinner, times/week | −0.48 (−1.18, 0.21) | −0.39 (−0.83, 0.05) | −0.08 (−0.48, 0.31) | −0.15 (−0.45, 0.15) | 0.0 (ref) | 0.05 (0.00, 0.10)* |
| Total dairy, servings/day | −0.03 (−0.58, 0.52) | −0.21 (−0.55, 0.14) | −0.03 (−0.34, 0.27) | 0.19 (−0.05, 0.43) | 0.0 (ref) | 0.02 (−0.02, 0.06) |
| Fruits and vegetables, servings/day | −0.10 (−0.77, 0.57) | −0.11 (−0.51, 0.29) | 0.09 (−0.28, 0.46) | 0.12 (−0.15, 0.39) | 0.0 (ref) | 0.01 (−0.04, 0.06) |
| Fast food, servings/week | −0.01 (−0.30, 0.27) | 0.06 (−0.13, 0.25) | 0.03 (−0.13, 0.19) | 0.01 (−0.11, 0.13) | 0.0 (ref) | −0.01 (−0.03, 0.01) |
| Skipping breakfast, times/week | 0.23 (−0.13, 0.59) | 0.18 (−0.03, 0.40) | 0.04 (−0.16, 0.24) | 0.03 (−0.12, 0.17) | 0.0 (ref) | −0.03 (−0.05, 0.00)* |
indicates statistical significance at the p≤0.05 level for the continuous score outcome
Models adjust for child sex, age in days and race/ethnicity; maternal college graduate (yes/no); and household income (>/≤ 70k)
Higher sleep scores indicate more often meeting the recommended sleep for age, i.e., children with higher sleep scores had more adequate sleep duration over childhood.
Youth Healthy Eating Index (YHEI) score is not adjusted for other mid-childhood dietary factors.
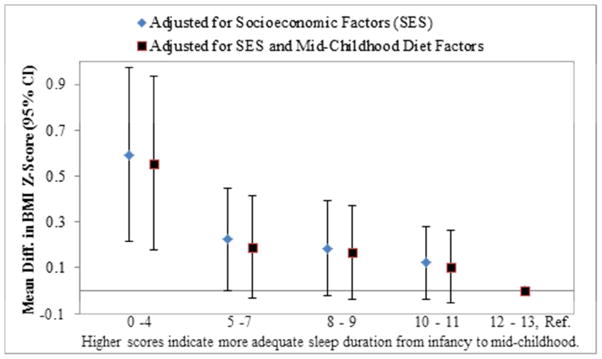
Figure 1 shows previously examined associations of chronic insufficient sleep with mid-childhood BMI z-score, (7) which were not explained by mid-childhood dietary factors. Comparing children with the least adequate sleep (scores 0–4) from infancy to mid-childhood to children with the most adequate sleep (scores 12–13), the mean difference in mid-childhood BMI z-score was 0.59 SD (95%CI: 0.22, 0.97), attenuating only slightly (~5% to 0.56 SD [95%CI: 0.18, 0.93]) with the addition of all YHEI dietary factors to multivariable models. Considering the score continuously, the mean difference in mid-childhood BMI z-score per 1-unit increase in the sleep score was −0.05 SD (95%CI: −0.08, −0.03). This protective association did not attenuate when YHEI components were added to multivariable models (−0.05 SD; 95%CI: −0.07, −0.02).
Figure 1.
Association of Sleep Curtailment Score with BMI Z-Score in Mid-Childhood Does Not Attenuate with Adjustment for Mid-Childhood Dietary Factors (N=1,046) 1, 2
1Results from linear regression models adjusted for maternal education, household income, age in days at mid-childhood visit, sex, and race/ethnicity. The sleep curtailment score is shown categorically, with and without adjustment for all dietary factors other than YHEI in mid-childhood.
2Higher sleep scores indicate more often meeting the recommended sleep for age, i.e., children with higher sleep scores had more adequate sleep duration over childhood.
In supplemental analyses, we examined mutually-adjusted associations of mid-childhood dietary factors with mid-childhood BMI z-score (Figure S1). Though most associations were in the expected direction, the dietary factors that were significantly associated with BMI z-score were overall diet quality (−0.07 SD per 10-point increase in YHEI; 95%CI: −0.13, −0.01); whole grain intake (−0.12 SD per servings/day; 95%CI: −0.19, −0.04); and skipping breakfast (0.07 SD per skipped meal/week; 95%CI: 0.01, 0.14). Sugary drinks and family dinner were not associated with mid-childhood BMI z-score.
Our supplemental analyses assessing joint associations of chronic insufficient sleep and dietary factors found that children in the least favorable category of sleep and diet had the highest estimated mid-childhood BMI z-scores. The mean difference in BMI z-score was 0.34 standard deviation units higher (95%CI: 0.16, 0.51) comparing children with sleep and diet scores below median values (sleep score <11; YHEI <60) to those with sleep and diet scores above median values (Figure S2). However, the interaction term of continuous sleep and YHEI score was not statistically significant (p=0.53).
In sensitivity analyses updating the sleep curtailment score to align with 2015 sleep recommendations, results were similar. Associations per unit increase in the revised sleep score with BMI z-score in mid-childhood (−0.05 SD [95%CI: −0.08, −0.02]), YHEI score (0.61 points [95%CI: 0.34 0.88]), sugary drink intake (−0.02 servings/day [95%CI: −0.04, −0.01]) and frequency of skipping breakfast (−0.04 times/week [95%CI:−0.06, −0.01]) were nearly identical. However, the revised sleep score was not associated with other dietary factors (e.g. whole grain intake or frequency of family dinner).
Discussion
In this cohort of 1,046 children followed from infancy to mid-childhood, we found that chronic insufficient sleep predicted less favorable diet quality in mid-childhood adjusting for child age, sex and race/ethnicity, maternal education and household income. While mid-childhood dietary factors were associated with mid-childhood BMI z-score, diet quality did not explain associations of chronic insufficient sleep with BMI z-score. Dietary assessment in young children is challenging, and typically relies on parental report. Random measurement error could be one explanation for why children’s diet quality did not mediate the sleep score’s association with BMI z-score. Further, total energy intake was not examined (it is not well-measured through dietary questionnaires on habitual intake). Another possibility is that sleep influences energy balance through pathways other than diet quality; e.g., experimental data show timing of feeding impacts metabolic processes and satiety responses independent of calories, reflecting the importance of circadian alignment of eating behaviors with metabolism. (29) Though the impact of chronic insufficient sleep on other aspects of diet (e.g. meal timing) warrant exploration, our finding that chronic insufficient sleep is associated with diet quality plus the previously observed associations of chronic insufficient sleep with BMI z-score (7) both support the need to consider sleep as a relevant behavior in pediatric obesity.
Sleep and Diet Quality
We found that chronic sleep curtailment is associated with less favorable overall diet quality as measured by the YHEI, and with less frequent family dinner and consumption of whole grains and more frequent consumption of sugary drinks. To our knowledge, ours is the first study to examine associations of chronic insufficient sleep with diet quality in mid-childhood; few studies are directly comparable. Our findings extend prior cross-sectional research, primarily in older children and adolescents, in two important ways: first we assess chronic insufficient sleep over the course of childhood and habitual dietary intake, and second we assess this in young children still establishing dietary habits and preferences. Key examples of prior cross-sectional research include that of Westerlund et al., who found that questionnaire-measured shorter sleep in Finish schoolchildren (n=1,265) was associated with greater consumption of energy-dense foods including pizza, pasta and refined sugars. (30) With respect to macronutrient composition, Weiss et al found in American adolescents (n=240) that compared to actigraphy-measured sleep of ≥ 8-hours on weekdays, sleeping < 8-hours was associated with a higher proportion of calories from fats. (31)
In the present study, we found no association of chronic insufficient sleep with consumption of fast food or fruits and vegetables in mid-childhood; in contrast, data from the National Longitudinal Study of Adolescent Health (Add Health, n=13,284) found that self-reported short sleep duration (< 7-hours/night compared to >8-hours/night) was associated with reduced odds of vegetable/fruit consumption and increased odds of fast food consumption. However, Add Health data were cross-sectional, from older children, and dietary factors were not mutually adjusted. (32) One possibility is that there is a cross-sectional relationship of shorter sleep duration with fast food and vegetables/fruits but chronic insufficient sleep duration does not influence consumption. Another possibility is that results do not extend to a study population as young as ours (e.g. adolescents have more autonomy over food choice), or, as mentioned previously, measurement error in parent-report of children’s intake attenuates associations.
Prospective studies are few, and provide inconsistent evidence for an association of shorter sleep duration in childhood with lower diet quality; e.g., the United Kingdom’s Gemini cohort (n=1,303) reported that shorter (<10-hours/day) versus longer sleep duration (11-<12-hours/day) at 16-months predicted slightly higher energy intake at 21 months, but found no differences in macronutrient composition. (19) Similar to our findings that shorter sleep duration was associated with sugary drink intake, a recent prospective study with shorter follow-up (200 days) and smaller size (n= 441 Danish 8–11-year-olds) found that each 1-hour decline in accelerometer-measured sleep duration was associated with higher intake of added sugar and sugar-sweetened beverages. (33) Our study extends this literature by showing that chronic insufficient sleep from infancy to mid-childhood is associated with less favorable overall diet quality in mid-childhood as measured by the YHEI and selected components.
Diet Quality’s Role in the Relationship of Sleep to Adiposity
Diet quality did not explain associations of chronic insufficient sleep duration with adiposity in young children. Results from experimental studies are inconsistent, short-term, and in small samples; e.g., a recent intervention assigned (n=37) children 8–11 years to 1.5-hour increased (versus decreased) time in bed and reported lower food intake, fasting leptin and weight at 3-weeks. (16) By contrast, in a crossover trial of Danish adolescents (n=21) short-term sleep restriction was not associated greater ad libitum intake or positive energy balance. (34) In free-living adults, one of the only observational studies examining this question was conducted among Japanese workmen; the authors concluded that diet adjustment (e.g. fatty food preference, skipping breakfast, snacking, and eating out) only partially explained associations of short sleep with obesity. (35)
Longitudinal research in children examining diet as a mediator is limited to one prior study, the Quebec Longitudinal Study of Child Development (n=1,106), which found associations of shorter sleep patterns from birth through mid-childhood with lower diet quality, irregular eating and eating too much too fast at 6 years. Consistent with our finding that dietary quality did not play a strong mediating role in the relationship of chronic insufficient sleep to adiposity, the Quebec study found that irregular eating and eating too much too fast, and not dietary intake, mediated the inverse association between sleep duration and overweight/obesity. (36) These findings are echoed by a small study of Canadian 5–12 year olds (n=56) that found shorter actigraphy-measured sleep duration was associated with emotional eating, greater response to food stimuli, and less dietary restraint. (37) Altered eating behaviors, not just the composition of diet, may play important mediating roles in the associations of sleep duration with adiposity in early childhood when children often have less autonomy in food selection.
We found that children scoring below the median for both the sleep and diet scores had higher BMI z-scores than children scoring below the median on either alone, suggesting that both sufficient sleep and diet quality may aid in childhood obesity prevention. No other study has examined the joint associations of chronic insufficient sleep duration and diet with mid-childhood BMI z-score.
Strengths and Limitations
Ours is one of the first studies examining the relationship of chronic insufficient sleep to diet quality in young children. Strengths include repeated parental report of sleep duration over time and research measures of height/weight. Additionally, prior studies examining sleep duration in relation to single dietary factors or behaviors have not adjusted for other aspects of diet to show independent associations as we did in this study.
This study has limitations. Parental report of children’s sleep duration and diet almost certainly contain error. While this error is likely random, null bias could mask diet’s mediating role in sleep-adiposity relationship. Additionally, our measure of overall diet quality –YHEI – was developed in older children; neither this index nor other common dietary indices are used widely or have been validated in young children. (38) Future prospective research should examine additional aspects of children’s sleep and diet not measured here, including sleep quality (e.g. nighttime awakenings or difficulty falling asleep), night-to-night variation in sleep duration and eating behaviors (e.g. emotional/disinhibited eating). Further work including meal timing may further clarify the inter-relationships among sleep, eating behaviors and energy balance.
Conclusion
Our results demonstrate that chronic insufficient sleep duration as measured from longitudinal data from infancy to mid-childhood is associated with lower quality diet in children. This association is not explained by measured confounders such as sex, age, race/ethnicity, education or income. With questionnaire data, we did not identify an appreciable mediating role of diet in the sleep-adiposity association. That children with the least favorable diets and sleep duration throughout childhood had the highest estimated BMI z-scores suggests that consideration of sleep duration and diet quality is necessary for childhood obesity prevention.
Supplementary Material
Study Importance.
Diet is one hypothesized mechanism underlying the association of shorter sleep duration with childhood obesity, but prospective studies examining diet quality as a mediator are lacking.
In this study, while chronic insufficient sleep duration from infancy to mid-childhood was associated with less favorable diet quality, diet did not explain associations with adiposity.
Nonetheless, children with the least favorable sleep duration and diet quality had the highest BMI z-scores in mid-childhood, suggesting both factors may contribute to childhood obesity.
Acknowledgments
Funding Source: This work was supported by the National Cancer Institute’s Centers for Transdisciplinary Research on Energetics and Cancer (TREC) (U54CA116847) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R37HD034568). Elizabeth Cespedes is supported by the National Institute of Diabetes and Digestive and Kidney Diseases T32 DK007703.
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.Ambrosini GL, Emmett PM, Northstone K, Jebb SA. Tracking a dietary pattern associated with increased adiposity in childhood and adolescence. Obesity (Silver Spring, Md) 2014;22:458–465. doi: 10.1002/oby.20542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bjelland M, Brantsaeter AL, Haugen M, Meltzer HM, Nystad W, Andersen LF. Changes and tracking of fruit, vegetables and sugar-sweetened beverages intake from 18 months to 7 years in the Norwegian Mother and Child Cohort Study. BMC public health. 2013;13:793. doi: 10.1186/1471-2458-13-793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cunningham SA, Kramer MR, Narayan KMV. Incidence of Childhood Obesity in the United States. New England Journal of Medicine. 2014;370:403–411. doi: 10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Padez C, Mourao I, Moreira P, Rosado V. Long sleep duration and childhood overweight/obesity and body fat. American journal of human biology : the official journal of the Human Biology Council. 2009;21:371–376. doi: 10.1002/ajhb.20884. [DOI] [PubMed] [Google Scholar]
- 6.Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Early life risk factors for obesity in childhood: cohort study. BMJ (Clinical research ed) 2005;330:1357. doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taveras EMGM, Peña MM, Redline S, Rifas-Shiman SL. Chronic Sleep Curtailment and Adiposity. Pediatrics. 2014;133:1013–1022. doi: 10.1542/peds.2013-3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spruyt K, Molfese DL, Gozal D. Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics. 2011;127:e345–352. doi: 10.1542/peds.2010-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matthews KA, Dahl RE, Owens JF, Lee L, Hall M. Sleep duration and insulin resistance in healthy black and white adolescents. Sleep. 2012;35:1353–1358. doi: 10.5665/sleep.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kong AP, Wing YK, Choi KC, Li AM, Ko GT, Ma RC, et al. Associations of sleep duration with obesity and serum lipid profile in children and adolescents. Sleep medicine. 2011;12:659–665. doi: 10.1016/j.sleep.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 11.Kjeldsen JS, Hjorth MF, Andersen R, Michaelsen KF, Tetens I, Astrup A, et al. Short sleep duration and large variability in sleep duration are independently associated with dietary risk factors for obesity in Danish school children. International journal of obesity (2005) 2014;38:32–39. doi: 10.1038/ijo.2013.147. [DOI] [PubMed] [Google Scholar]
- 12.Morselli L, Leproult R, Balbo M, Spiegel K. Role of sleep duration in the regulation of glucose metabolism and appetite. Best practice & research Clinical endocrinology & metabolism. 2010;24:687–702. doi: 10.1016/j.beem.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Annals of the New York Academy of Sciences. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.St-Onge MP, Wolfe S, Sy M, Shechter A, Hirsch J. Sleep restriction increases the neuronal response to unhealthy food in normal-weight individuals. International journal of obesity (2005) 2014;38:411–416. doi: 10.1038/ijo.2013.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benedict C, Brooks SJ, O’Daly OG, Almen MS, Morell A, Aberg K, et al. Acute sleep deprivation enhances the brain’s response to hedonic food stimuli: an fMRI study. The Journal of clinical endocrinology and metabolism. 2012;97:E443–447. doi: 10.1210/jc.2011-2759. [DOI] [PubMed] [Google Scholar]
- 16.Hart CN, Carskadon MA, Considine RV, Fava JL, Lawton J, Raynor HA, et al. Changes in children’s sleep duration on food intake, weight, and leptin. Pediatrics. 2013;132:e1473–1480. doi: 10.1542/peds.2013-1274. [DOI] [PubMed] [Google Scholar]
- 17.Chaput JP. Sleep patterns, diet quality and energy balance. Physiology & behavior. 2014;134:86–91. doi: 10.1016/j.physbeh.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? The international journal of behavioral nutrition and physical activity. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher A, McDonald L, van Jaarsveld CH, Llewellyn C, Fildes A, Schrempft S, et al. Sleep and energy intake in early childhood. International journal of obesity (2005) 2014;38:926–929. doi: 10.1038/ijo.2014.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oken E, Baccarelli AA, Gold DR, Kleinman KP, Litonjua AA, De Meo D, et al. Cohort Profile: Project Viva. International journal of epidemiology. 2014 doi: 10.1093/ije/dyu008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kushnir J, Sadeh A. Correspondence between reported and actigraphic sleep measures in preschool children: the role of a clinical context. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2013;9:1147–1151. doi: 10.5664/jcsm.3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cespedes EM, Rifas-Shiman SL, Redline S, Gillman MW, Pena MM, Taveras EM. Longitudinal associations of sleep curtailment with metabolic risk in mid-childhood. Obesity (Silver Spring, Md) 2014 doi: 10.1002/oby.20894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hart CN, Cairns A, Jelalian E. Sleep and obesity in children and adolescents. Pediatr Clin North Am. 2011;58:715–733. doi: 10.1016/j.pcl.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Sleep Foundation. Sleep in America Princeton, NJ. 2008 [cited 2014 April 9]. Available from: http://sleepfoundation.org/
- 25.National Heart Lung and Blood Institute. Sleep Deprivation and Deficiency: How Much Sleep Is Enough? 2012 [cited 2014 April 9]. Available from: http://www.nhlbi.nih.gov/health/health-topics/topics/sdd/howmuch.
- 26.Taveras E, Rifas-Shiman S, Redline S, Gillman M. Short Sleep Duration in Infancy and Chronic Sleep Curtailment from Infancy to Mid-Childhood Are Associated with Higher Adiposity at Age 7 Years. Pediatric Academic Societies’ Annual Meeting; Boston, Mass. April 28-May 1, 2012. [Google Scholar]
- 27.Rifas-Shiman SL, Willett WC, Lobb R, Kotch J, Dart C, Gillman MW. PrimeScreen, a brief dietary screening tool: reproducibility and comparability with both a longer food frequency questionnaire and biomarkers. Public health nutrition. 2001;4:249–254. doi: 10.1079/phn200061. [DOI] [PubMed] [Google Scholar]
- 28.Feskanich D, Rockett HR, Colditz GA. Modifying the Healthy Eating Index to assess diet quality in children and adolescents. Journal of the American Dietetic Association. 2004;104:1375–1383. doi: 10.1016/j.jada.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 29.McHill AW, Melanson EL, Higgins J, Connick E, Moehlman TM, Stothard ER, et al. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proceedings of the National Academy of Sciences of the United States of America. 2014;111:17302–17307. doi: 10.1073/pnas.1412021111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Westerlund L, Ray C, Roos E. Associations between sleeping habits and food consumption patterns among 10–11-year-old children in Finland. The British journal of nutrition. 2009;102:1531–1537. doi: 10.1017/S0007114509990730. [DOI] [PubMed] [Google Scholar]
- 31.Weiss A, Xu F, Storfer-Isser A, Thomas A, Ievers-Landis CE, Redline S. The association of sleep duration with adolescents’ fat and carbohydrate consumption. Sleep. 2010;33:1201–1209. doi: 10.1093/sleep/33.9.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kruger AK, Reither EN, Peppard PE, Krueger PM, Hale L. Do sleep-deprived adolescents make less-healthy food choices? The British journal of nutrition. 2014;111:1898–1904. doi: 10.1017/S0007114514000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hjorth MF, Quist JS, Andersen R, Michaelsen KF, Tetens I, Astrup A, et al. Change in sleep duration and proposed dietary risk factors for obesity in Danish school children. Pediatric obesity. 2014 doi: 10.1111/ijpo.264. [DOI] [PubMed] [Google Scholar]
- 34.Klingenberg L, Chaput JP, Holmback U, Jennum P, Astrup A, Sjodin A. Sleep restriction is not associated with a positive energy balance in adolescent boys. The American journal of clinical nutrition. 2012;96:240–248. doi: 10.3945/ajcn.112.038638. [DOI] [PubMed] [Google Scholar]
- 35.Nishiura C, Noguchi J, Hashimoto H. Dietary patterns only partially explain the effect of short sleep duration on the incidence of obesity. Sleep. 2010;33:753–757. doi: 10.1093/sleep/33.6.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tatone-Tokuda F, Dubois L, Ramsay T, Girard M, Touchette E, Petit D, et al. Sex differences in the association between sleep duration, diet and body mass index: a birth cohort study. Journal of sleep research. 2012;21:448–460. doi: 10.1111/j.1365-2869.2011.00989.x. [DOI] [PubMed] [Google Scholar]
- 37.Burt J, Dube L, Thibault L, Gruber R. Sleep and eating in childhood: a potential behavioral mechanism underlying the relationship between poor sleep and obesity. Sleep medicine. 2014;15:71–75. doi: 10.1016/j.sleep.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 38.Marshall S, Burrows T, Collins CE. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. Journal of human nutrition and dietetics : the official journal of the British Dietetic Association. 2014 doi: 10.1111/jhn.12208. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.