Abstract
The incidence of skin cancer worldwide is constantly growing and it is the most frequently diagnosed tumor. Brachytherapy (BT) in particular localizations is a valuable tool of the exact radiation depot inside the tumor mass. In localizations such as the face, skull skin and inoperable tumors, relapses after surgery, radiotherapy are usually not suitable for primary or secondary invasive treatment. Brachytherapy is a safe procedure for organs at risk according to rapid fall of a dose outside the axis of the applicator with satisfactory dose localization inside the target. The complications rate is acceptable and treatment costs are low. In some tumors (great skin lesions in the scalp, near eyes or on the nose) BT allows for a great dose reduction in surrounding healthy tissues. Brachytherapy provides minimal dose delivery to surrounding healthy tissue, thus enabling good functional and cosmetic results. Treatment is possible almost in all cases on an outpatient basis.
Keywords: electronic brachytherapy, high dose rate brachytherapy, pulsed dose rate brachytherapy, radiotherapy, skin cancer
Purpose
Nonmelanoma skin cancer (NMSC) is the most common malignancy and affects 2–3 million people each year only in the United States. The incidence is underestimated in many countries. Although NMSC has a low mortality rate, its incidence continues to rise; it significantly affects quality of life. Basal cell (BCC) and squamous cell carcinomas (SCC) of the skin usually occur on sun-exposed areas, the face being one of the sites of predilection, accounting for 95% of cases. Surgery in these sites (nose, ears, eyelids, lips) may be mutilating or require complex plastic reconstruction techniques under general anesthesia [1–4]. Radiation therapy has been used to treat NMSC for more than 40 years, and different techniques include superficial X-rays, orthovoltage X-rays, megavoltage photons, electron beam irradiation, and HDR brachytherapy (BT). Radiotherapy (RT), in particular a well-planned BT, is often the treatment of choice in cases of skin cancer which cannot be surgically removed without serious defects, cosmetic and reconstructive procedures [5–7]. There are many techniques of radiation that can be used to treat skin cancers. In external beam radiation therapy (EBRT), partial or photon radiation obtained from linear accelerators is used. In contrast, BT (from Greek – close, in French – curietherapy) uses the energy of photons or particles coming from the decay of radioactive isotopes located in the tumor (BT interstitial) or in its immediate proximity (BT superficial) [5–7].
Before starting the treatment of skin cancer, radiation therapy should be considered by a number of clinical parameters such as the total dose of radiation, dose fractionation, dose distribution, the size of the treated field, the beam type and the total treatment time, because they have a significant impact on the final results of therapy [8]. External beam radiation therapy has several adverse features, which include a decrease in the dose to the skin surface requiring the use of bolus doses, greater absorption by the bones and decrease in the dose on the perimeter of the field in the case of inclined surfaces [9]. In addition, ionizing radiation can penetrate deeply, potentially injuring adjacent tissue and organs causing brain and bone necrosis. Differences in the dose distribution after the application of 6 MeV electrons (EBRT) and high dose rate (HDR) BT (HDR-BT) are shown in Table 1. Dose distribution is more favorable for HDR due to better protection of subcutaneous tissues (bones, ligaments, joints, lacrimal gland, etc.) located close to the tumor being treated. Brachytherapy is better than EBRT in tumor radiation coverage and is connected with a lower complications rate. After BT, recurrence rates for NMSC are low, especially for small, superficial lesions, with good to excellent functional and cosmetic results.
Table 1.
Dose distribution of 6 MeV electrons (EBRT) (with 0.5 cm bolus) and HDR-BT (Freiburg applicator, distance between applicator and skin surface – 5 mm) [9]
| Depth [cm] | Electrons 6 MeV, % dose | HDR-BT (normalized on 0.2 cm depth),% dose |
|---|---|---|
| 0.0 | 88 | 105–110 |
| 0.5 | 98 | 85 |
| 1.0 | 98 | 65 |
| 1.5 | 78 | 55 |
| 2.0 | 36 | 30 |
Indications for brachytherapy
The basis for the HDR-BT of NMSC is TNM clinical classification. For this reason, in the preparatory proceedings, the clinical stage should be assessed, accurate measurements made, lesions documented photographically if possible, and in case of the suspicions of deep infiltration of the eye, ear or other structures, computed tomography should be considered [5].
Brachytherapy is a valued method due to the excellent results and very good cosmetic effects after treatment of unfavorably located cancer [10–13]. Brachytherapy is a method recommended in situations where changes are localized on anatomical curves and near critical organs (nasal bridge, periorbital region and skin of the chest) [14]. It also enables treatment of large tumors with minimal detriment of healthy tissues and a high probability of cure without adverse local complications [15]. In many clinical situations, BT is the only possibility we can offer after recurrence previously treated with RT.
Basic indications for BT are: 1. radical sole (mono) BT of T1-2N0 tumors (primary lesions, recurrences after surgery and/or radiotherapy); 2. adjuvant therapy after non radical surgery; 3. as a boost in larger tumors (T2–T3) or in TxN1 cases after EBRT to the primary tumor and lymph nodes; 4. palliative treatment (Table 2).
Table 2.
Indications for radiotherapy (both – EBRT and BT) in a group of skin tumors based on histopathology [6]
| Highly recommended | Recommended | Rarely recommended |
|---|---|---|
| Sarcoma Kaposi Mycosis fungoides Lymphomas |
BCC/SCC (except scrotum, soles of the feet and hand) Bowen disease/erythroplasia Angiosarcoma Merkel cell carcinoma |
Fibrosarcoma, BCC/SCC of scrotum, soles of the feet and hand Melanoma (except treatment after non radical surgery) |
SCC – Squamous cell carcinoma, BCC – basal cell carcinoma.
Contraindications for brachytherapy
1. Malignant melanoma of the skin which is not radiosensitive (except in chosen cases of treatment combined with hyperthermia, after non radical surgery); 2. Skin cancers invading bony structures; 3. Upper eyelid lesions; 4. Pinna tumour involving both the concha and the external auditory canal, ear conduct or any other site where the anatomical situation makes the source positioning needed to provide adequate covering of the target volume impossible [16].
Brachytherapy techniques
Brachytherapy with radioactive Ir-192 isotope (source) is applied to small skin cancer lesions, using surface applicators, I.e. Freiburg/French, Leipzig or Valencia type. New developments in the field of radiotherapy for skin cancer include electronic BT [17].
Continuous technological advances in recent years in the field of BT allowed us to the use well-prepared applications of radioactive sources (usually Ir-192) using after-loading techniques (automatic source loading systems) [18, 19]. Under the control of a computer system for treatment planning, a single source is inserted into all previously established applicators and positioned on the basis of the planned treatment area. The source moves along the guide axis at a given distance, which is roughly equal to the tumor size [16]. General principles of treatment planning include extending the tumor with an applicator, applicator stabilization (interstitial or superficial), the treatment dose covering the tumor with an adequate margin. Currently, the most commonly used BT techniques are HDR using radioactive isotopes Ir-192 or Co-60 with the original activity of 370 Gbq (10 Ci) and dose rate > 12 Gy/h and pulsed dose rate (PDR), which uses the same isotope, but with a lower activity level of 15–37 Gbq (0.5–1 Ci).
Superficial brachytherapy
Among the several techniques of superficial BT, different applicators are used: 1. mats (made of classical catheters and adhesive tape), useful in the treatment of large and flat surface; 2. shapes and forms to allow irradiation of the surrounding area of irregular shapes (e.g. pinna); 3. surface applicators individually tailored to the individual patient or commercial ones (Brock applicators, Leipzig, Freiburg, HAM). A typical applicator comprises 2–10 parallel positioned catheters (filled during the irradiation with a radioactive source sequentially) with an equal distance of 5–10 mm preserved between them. Examples of some applicators are presented in Figures 1 and 2.
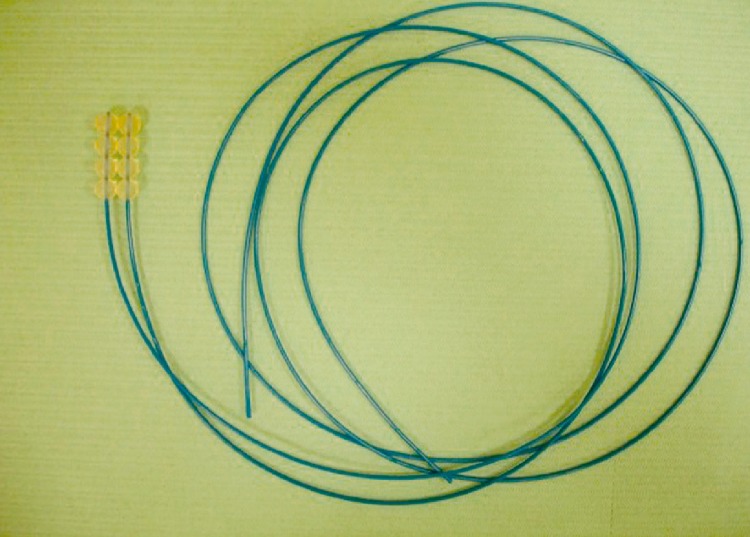
Figure 1.
Applicator for superficial brachytherapy built of the Freiburg applicator and French 5 applicator (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden)
Figure 2.
Photography of the horizontal (H30) and perpendicular (V30) Leipzig applicators with a 30 mm conediameter (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden)
Applicators are designed for flat surfaces and do not require anesthesia during application. Similarly, the pulmonary French applicators can also be used for the treatment of lesions located on the skin surface. When the applicator is ready, markers are placed in the catheters simulating the radioactive source and X-rays (front-rear and lateral) or computed tomography (CT)-scans are performed and the obtained data are transferred to the planning system. At this stage the irradiated area (planning target volume – PTV) consists of a tumor and 0.5 cm or 1 cm margin (gross tumor volume – GTV) depending on the lesion diameter) [20, 21].
According to the recommendations of the American Brachytherapy Society, tumors with an infiltration depth < 0.5 cm can be treated with superficial BT alone. The suggested dose is 48–51 Gy/16–17 fractions/0.5 cm from the surface of the applicator given once daily [22].
Interstitial brachytherapy
Tumors located on the curved surfaces (naso-buccal folds, fingers, ear pinna) with a diameter of 5–6 cm and a thickness of 0.5–2.0 cm should be treated with interstitial BT. The cases of coexisting fistula, nodal metastasis and bone infiltration are excluded here. Most cancers can be treated by 1 to 3 plastic applicators implanted into the tumor for which the prescribed dose of 65 Gy (45–70 Gy) to the reference isodoses 85% is calculated according to the Paris system. Such proceedings bring benefits in terms of local control in the range of 95–98% with an excellent cosmetic and functional result [23].
In the interstitial method, specially phrasing hypodermic needles bevel of 2–10 cm in length, silk and nylon wire tubes adapted for after-loading applications are still used in some centers. All applications are performed in local or general anesthesia (if necessary). The same is true in the case of metal applicators used for interstitial implantation of radioactive iridium wires with a thickness of 0.5 cm. The number of applicators or needles depends on the tumor diameter and in most skin cancers infiltrating less than 1 cm healthy tissues, single plane HDR applications are performed. Standard doses range for T1-2 tumors – 48 Gy/16 fractions/2 times daily and for the tumors T3-4 – 51 Gy/17 fractions/2 times daily [16, 24].
Electronic brachytherapy
High-dose-rate (HDR) electronic BT (EBT) using surface applicators for the treatment of NMSC is a relatively new technique. Electronic brachytherapy was developed in the last years to provide patients with a shorter treatment schedule and physicians with a more convenient form of BT that does not require radioactive isotopes or dedicated treatment vaults [25, 26].
Bhatnagar [25] in one of the first publications analyzed a group of 122 patients with 171 lesions treated with EBT. They were treated with EBT up to a dose of 40 Gy in eight fractions, delivered twice weekly. There have been no recurrences within a mean follow-up of 10 months (range: 1–28 months). No Grade 3 or higher adverse events were observed at any time point. The EBT system used for this study (Axxent eBx; Xoft-a subsidiary of iCAD, Inc., Sunnyvale, CA, USA) uses a miniaturized X-ray source at its tip, capable of delivering HDR and low energy radiation without the use of radioactive isotopes.
Garcia-Martinez et al. [26] presented the new Esteya® Electronic Brachytherapy System (Esteya EBS, Elekta AB-Nucletron, Stockholm, Sweden) with excellent flatness and penumbra as with the Valencia applicator case, combined with an improved percentage of depth dose (PDD), allowing treatment of lesions of up to a depth of 5 mm in combination with reduced treatment duration. The Esteya® Electronic Brachytherapy System consists of a treatment unit with surface applicators, a user interface with planning software and a treatment control panel (Figure 3). The new Esteya system of electronic BT shows excellent flatness and penumbra as in the Valencia applicator case, but with an improved PDD (allowing treatment of lesions up to 5 mm deep) and increased dose rate (reducing the treatment time). Because of the low energy of the Esteya system it allows HDR-BT superficial treatment within a minimally shielded environment [26].
Figure 3.
The Esteya Electronic Brachytherapy System (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden) [6]
Published results
Greater Poland Cancer Center (GCC) own results [27]
Four hundred and ninety-seven patients with skin cancer were treated in GCC between November 1999 and April 2008. The group consisted of 257 men and 240 women in the age range of 44–97 years (mean: 72 years). 96.57% of patients were treated radically, and 3.43% – palliatively. The most frequent pathologic types observed were BCC (n = 233, 48.09%) and SCC (n = 118, 23.74%). Thirteen cases of skin cancer were qualified to HDR-BRT after previous external beam radiation treatment. Sixty-three (12.76%) patients were treated as a supplementary therapy, after the surgery procedure. The dose reached 50–60 Gy in 10 fractions (n = 430, 86.52%) and 30–40 Gy in 6–8 fractions (n = 67, 13.48%). The reference point of the dose was estimated on 1 cm. Complete remission (CR) after 12 months appeared in 356 (71.63%) patients, progression – in 73 (4.63%). All patients experienced early skin reaction after radiation treatment according to RTOG classification: 1 degree – 372 (74.8%), 2 degree – 81 (16.3%), 3 degree – 44 (8.9%). Late skin reactions were observed as follows: 1 degree (n = 388, 78.1%), 2 degree (n = 85, 17.1%) and 3 degree (n = 24, 4.9%).
Other results
Many published studies confirm the high percentages of the cure rate using skin cancer BT. Selected results are shown in Table 3.
Table 3.
Selected results of skin cancer brachytherapy [1]
| Author | Location | N | Technique | Follow-up [years] | Local control |
|---|---|---|---|---|---|
| Guix [15] | Face | 136 | HDR | 5 | 99% – primary 87% – recurrence |
| Crook [28] | Nose | 468 | HDR | 5 | 97.5% |
| Debois [29] | Nose | 370 | LDR | 2 | 97% – primary 94% – recurrence |
| Gambaro [30] | Eyelid | 50 | HDR | 6.5 | 96% |
| Maes [31] | Face | 173 | HDR | 3.5 | 95% |
| Ashby [32] | Vary | 642 | Radium | . | 96.8% |
| Daly [33] | Eyelid | 165 | HDR | 5 | 97% – primary 94% – recurrence |
| Svoboda [34] | Vary | 76 | HDR | 9.6 | 96.2% |
| Mazeron [35] | Ear | 70 | HDR | 5 | 99% |
| Tormo [36] | Vary | 32 | HDR | 2 | 98% |
| Gauden [37] | Vary | 200 | HDR (Leipzig) | 5.5 | 98% |
| Arguis [38] | Vary | 141 | HDR (Leipzig) | 3.25 | 92.4% |
In stage T1–T2 (total dose of 60–65 Gy), 5-year local control is achieved in over 95% of cases [15, 28–31]. In treatment of recurrences after the previous surgery failure, rates are slightly higher and range from 6% to 13% [15, 29, 33].
Selected publications are worth discussing. Guix et al. in a group of 136 patients with primary and recurrent cancers treated using superficial applicators showed that the probability of a local cure is 99% and 87%, respectively [15]. The percentage of early and late complications was low. Only in 2% of patients in the group of patients with recurrent skin cancer, with a diameter greater than 4 cm, an unsatisfactory cosmetic result was achieved. At the same time, dosimetric studies demonstrated that the differences between the minimum and maximum radiation dose at a depth of 5 mm, even in the case of major anatomical curves do not exceed 3%. The high dose uniformity in such cases is not possible to be obtained after application of photons or electrons with low-energy irradiation.
Daly et al. [33] published the results of treatment of 165 patients with skin cancer of the eyelids. The local control was 96% (6/165 recurrences). Acute treatment toxicity was observed in 49/165 (30%) patients at 8 weeks after treatment, lasting in 3% for more than 4 months. In most cases, the cosmetic effect and the preservation of activity of eyelids was considered as good or very good. Severe late complications occurred in 30 (18%) patients, in some cases requiring the intervention of the surgeon. Rio et al. [24] performed a retrospective analysis of 97 skin carcinomas (88 BCC, 9 SCC) of the nose, periorbital areas, and ears from 40 previously untreated patients (group 1) and 57 patients who had undergone surgery (group 2). The average dose was 55 Gy (range: 50–65 Gy) in group 1 and 52 Gy (range: 50–60 Gy) in group 2. The local control was 92.5% in group 1 and 88% in group 2 (median follow-up – 55 months; range: 6–132 months). Five-year disease-free survival was better in group 1 (91%; range: 75–97) than in group 2 (80%; range: 62–90; p = 0.23). Authors have concluded that BT provided a high level of local control and good cosmetic results for facial periorificial skin carcinomas that pose problems of surgical reconstruction.
Cosmetic effect
The cosmetic effect in the vast majority of reported cases (range: 78–92%) is defined as good or very good (Table 4). A particularly high risk of complications occurs when the tumor is located on the eyelids (cataracts, chronic inflammation of mucous membranes, lacrimal duct stenosis). For small tumors (T1–T2), one should be aware of not exceeding a total dose of 60 Gy, as higher doses significantly influence the increase in complications [5].
Table 4.
Cosmetic results and complications after brachytherapy of skin cancer [1]
| Author | Location | N | Technique | Good cosmetic result | Complications rate |
|---|---|---|---|---|---|
| Guix [15] | Face | 136 | HDR | 0% | |
| Maes [31] | Face | 173 | HDR | 89% | 3.6% |
| Debois [29] | Nose | 370 | LDR | 0% | |
| Crook [28] | Nose | 468 | HDR | 94% | 2% |
| Daly [33] | Eyelid | 165 | HDR | 13% – primary 31% – recurrence |
|
| Gambaro [30] | Eyelid | 50 | HDR | 92% | 4% – cataract 20% – chronic inflammation of the mucous membranes 25% – lacrimal duct stenosis |
| Mazeron [35] | Ear | 70 | HDR | < 4 cm: 78% > 4 cm: 11% |
13% – transient ulcers 4% – necrosis |
In GCC we treat skin tumors according to the following rules (Table 5).
Table 5.
Recommendations for skin cancer brachytherapy (source: Greater Poland Cancer Center, Poznan, Poland)
| Treatment | Indications | Technique | Fraction dose (range) | Total dose (range) |
|---|---|---|---|---|
| Radical | Primary, recurrences. Diameter < 5–6 cm, technically possible application, thickness < 2 cm | HDR | 5.0–10.0 Gy | 50–60.0 Gy |
| PDR | 1.0 Gy (pulse) | 50–60.0 Gy (in 2–3 fractions) | ||
| Radical, after surgery | Typically after non radical surgery (suggested by pathological diagnosis), healthy tissue margin < 5 mm | HDR | 5.0–10.0 Gy | 50–60.0 Gy |
| PDR | 1.0 Gy (pulse) | 50– 60.0 Gy (in 2–3 fractions) | ||
| Palliative | Inoperative tumors, size preventing coverage with curative dose, thickness > 2 cm | HDR | 5.0–10.0 Gy | 20–40.0 Gy |
| PDR | 1.0 Gy (pulse) | 20–40.0 Gy (in 1–2 fractions) |
Conclusions
Brachytherapy is a highly effective treatment method of skin tumors, well known for almost one hundred years, with a big number of confirmed published positive results. The complications rate is acceptable and treatment costs are low. Treatment is possible almost in all cases on an outpatient basis. In some tumors (great skin lesions in the scalp, near eyes or on the nose) BT allows for a great dose reduction in surrounding healthy tissues. Brachytherapy provides minimal dose delivery to surrounding healthy tissue, thus enabling good functional and cosmetic results.
Conflict of interest
The author declares no conflict of interest.
References
- 1.Szewczyk MP, Pazdrowski J, Dańczak-Pazdrowska A, et al. Analysis of selected recurrence risk factors after treatment of head and neck basal cell carcinoma. Postep Derm Alergol. 2014;31:146–51. doi: 10.5114/pdia.2014.40959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sobjanek M, Dobosz M, Pęksa R, et al. Lymphoepithelioma-like carcinoma of the skin in a Polish patient. Postep Derm Alergol. 2015;32:56–8. doi: 10.5114/pdia.2014.40952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marek L, Grzanka A, Chmielowska E, et al. Merkel cell carcinoma: an illustrative case and review. Postep Derm Alergol. 2014;31:325–8. doi: 10.5114/pdia.2014.40797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sopata M, Tomaszewska E, Muszyński Z, et al. The pilot study assessing efficacy and versatility of novel therapy for neoplastic ulceration: clinical and microbiological aspects. Postep Derm Alergol. 2013;30:237–45. doi: 10.5114/pdia.2013.37034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerbaulet A, Potter R, Mazeron JJ, editors. The GEC ESTRO Handbook of Brachytherapy. Bruksela: ESTRO; 2002. [Google Scholar]
- 6.Perez CA, Brady LW. Principles and practice of radiation oncology. 3rd ed. 1997. pp. 723–44. [Google Scholar]
- 7.Chicheł A, Skowronek J. Współczesne leczenie raka skóry – dermatologia, chirurgia czy radioterapia? Contemp Oncol (Poznan) 2005;10:429–35. [Google Scholar]
- 8.Malicki J, Łobodziec W, Ślósarek K. Dose-rate distribution under partially shielded beams. Strahlenther Onkol. 1990;166:733–7. [PubMed] [Google Scholar]
- 9.Leibel SA, Philips TL, editors. Textbook of radiation oncology. Philadelphia: Saunders; 2004. p. 316. [Google Scholar]
- 10.Alam M, Nanda S, Mittal BB, et al. The use of brachytherapy in the treatment of nonmelanoma skin cancer: a review. J Am Acad Dermatol. 2011;65:377–88. doi: 10.1016/j.jaad.2010.03.027. [DOI] [PubMed] [Google Scholar]
- 11.Delannes M, Rio E, Mirabel X, et al. Brachytherapy for cutaneous and lip carcinomas. Cancer Radiother. 2013;17:136–9. doi: 10.1016/j.canrad.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 12.Lukačko P, Pobijáková M, Lederleitner D. HDR brachytherapy for skin carcinoma of the face: treatment by customized mask – case report. J Contemp Brachytherapy. 2009;1:186. abstract. [Google Scholar]
- 13.Kowalik Ł, Łyczek J, Sawicki M, et al. Individual applicator for brachytherapy for various sites of superficial malignant lesions. J Contemp Brachytherapy. 2013;5:45–9. doi: 10.5114/jcb.2013.34340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kordek R, Jassem J, editors. Podręcznik dla studentów i lekarzy. Warsaw: 2003. pp. 217–21. [Google Scholar]
- 15.Guix B, Finestres F, Tello JI, et al. Treatment of skin carcinomas of the face by high-dose-rate brachyterapy and custom-made surface molds. Int J Radiat Oncol Biol Phys. 2000;47:95–102. doi: 10.1016/s0360-3016(99)00547-7. [DOI] [PubMed] [Google Scholar]
- 16.Skowronek J, Chicheł A, Piotrowski T. Brachyterapia HDR nowotworów skóry – doświadczenie Wielkopolskiego Centrum Onkologii. Contemp Oncol (Poznan) 2005;8:347–54. [Google Scholar]
- 17.Garcia-Martinez T, Chan JP, Perez-Calatayud J, et al. Dosimetric characteristics of a new unit for electronic skin brachytherapy. J Contemp Brachytherapy. 2014;6:45–53. doi: 10.5114/jcb.2014.40770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van der Laarse R. Optimization of high dose rate brachytherapy. Activity: The Selectron Users Newsletter. 1989;2:14–5. [Google Scholar]
- 19.Flynn A. Quality assurance checks on a microSelectron-HDR. Selectron Brachytherapy J. 1990;4:112–5. [Google Scholar]
- 20.Lliso F, Granero D, Perez-Calatayud J, et al. Dosimetric evaluation of internal shielding in a high dose rate skin applicator. J Contemp Brachytherapy. 2011;3:32–5. doi: 10.5114/jcb.2011.21041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lasota J, Kabacińska R, Makarewicz R. Dose estimation for different skin models in interstitial breast brachytherapy. J Contemp Brachytherapy. 2014;6:200–7. doi: 10.5114/jcb.2014.43167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nag S, Caro ER, Demanes JD, et al. The American Brachytherapy Society recommendations for high dose rate brachytherapy for head and neck carcinoma. Int J Oncol Biol Phys. 2001;50:1190–8. doi: 10.1016/s0360-3016(01)01567-x. [DOI] [PubMed] [Google Scholar]
- 23.Toller G, Lakosi F, Antal G, et al. CT assisted 3D high-dose-rate brachytherapy (HDR-BT) in the treatment of skin carcinoma. J Contemp Brachyther. 2009;1:190–1. [Google Scholar]
- 24.Rio E, Bardet E, Ferron C, et al. Interstitial brachytherapy of periorificial skin carcinomas of the face: a retrospective study of 97 cases. Int J Radiation Oncology Biol Phys. 2005;63:753–7. doi: 10.1016/j.ijrobp.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 25.Bhatnagar A. Nonmelanoma skin cancer treated with electronic brachytherapy: results at 1 year. Brachytherapy. 2013;12:134–40. doi: 10.1016/j.brachy.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Garcia-Martinez T, Chan JP, Perez-Calatayud J, et al. Dosimetric characteristics of a new unit for electronic skin brachytherapy. J Contemp Brachytherapy. 2014;6:45–53. doi: 10.5114/jcb.2014.40770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kanikowski M. HDR brachytherapy of skin cancer in material of Greater Poland Cancer Center. J Contemp Brachytherapy. 2009;1:197. Abstract. [PMC free article] [PubMed] [Google Scholar]
- 28.Crook JM, Mazeron JJ, Marinello G, et al. Interstitial irydium 192 for cutaneous carcinoma of the external nose. Int J Radiat Oncol Biol Phys. 1990;18:243–8. doi: 10.1016/0360-3016(90)90289-v. [DOI] [PubMed] [Google Scholar]
- 29.Debois JM. Cesium-137 brachytherapy for epithelioma of the skin of the nose: experience with 370 patients. JBR-BTR. 1994;77:1–4. [PubMed] [Google Scholar]
- 30.Gambaro G, Negri E. Interstitial brachytherapy with irydium-192 for carcinomas of the eyelid and inner canthus. Radiother Oncol. 2001;60(Suppl. 1):16. abstract. [Google Scholar]
- 31.Maes A, Van Limbergen E. LDR – Brachytherapy (BT) for non-melanoma skin cancer of the face: local control rate, functional and cosmetic outcome in 173 patients. Radiother Oncol. 2001;60(Suppl. 1):16. abstract. [Google Scholar]
- 32.Ashby MA, Pacella JA, De Groot R, et al. Use of radon mould technique for skin cancer: results from the Peter MacCallum Cancer Institute. Br J Radiol. 1989;62:608–12. doi: 10.1259/0007-1285-62-739-608. [DOI] [PubMed] [Google Scholar]
- 33.Daly NJ, Lafontan B, Combes PF. Results of the treatment of 165 lid carcinomas by iridium wire implant. Int J Radiat Oncol Biol Phys. 1984;10:455–9. doi: 10.1016/0360-3016(84)90024-5. [DOI] [PubMed] [Google Scholar]
- 34.Svoboda VHJ, Kovarik J, Morris F. High dose rate microselectron molds in the treatment of skin tumors. Int J Radiat Oncol Biol Phys. 1995;31:967–72. doi: 10.1016/0360-3016(94)00485-4. [DOI] [PubMed] [Google Scholar]
- 35.Mazeron JJ, Ghalie R, Zeller J, et al. Radiation therapy for carcinoma of the pinna using irydium 192 wires: a series of 70 patients. Int J Radiat Oncol boil Phys. 1986;12:1757–63. doi: 10.1016/0360-3016(86)90316-0. [DOI] [PubMed] [Google Scholar]
- 36.Tormo A, Celada F, Rodriguez S, et al. Non-melanoma skin cancer treated with HDR Valencia applicator: clinical outcomes. J Contemp Brachytherapy. 2014;6:167–72. doi: 10.5114/jcb.2014.43247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gauden R, Pracy M, Avery AM, et al. HDR brachytherapy for superficial non-melanoma skin cancers. J Med Imaging Radiat Oncol. 2013;57:212–7. doi: 10.1111/j.1754-9485.2012.02466.x. [DOI] [PubMed] [Google Scholar]
- 38.Arguis M, Murcia-Mejía M, Henríquez I. The role of HDR brachytherapy in non-melanoma skin cancer treatment. Radiother Oncol. 2012;103(Suppl. 1):S477. [Google Scholar]