Abstract
Objectives. We investigated whether Mexican immigration to the United States exerts transnational effects on substance use in Mexico and the United States.
Methods. We performed a cross-sectional survey of 2336 Mexican Americans and 2460 Mexicans in 3 Texas border metropolitan areas and their sister cities in Mexico (the US–Mexico Study on Alcohol and Related Conditions, 2011–2013). We collected prevalence and risk factors for alcohol and drug use; Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, alcohol-use disorders; and 2 symptoms (hazardous use and quit or control) of drug use disorder across a continuum of migration experiences in the Mexican and Mexican American populations.
Results. Compared with Mexicans with no migrant experience, the adjusted odds ratios for this continuum of migration experiences ranged from 1.10 to 8.85 for 12-month drug use, 1.09 to 5.07 for 12-month alcohol use disorder, and 1.13 to 9.95 for 12-month drug-use disorder. Odds ratios increased with longer exposure to US society. These findings are consistent with those of 3 previous studies.
Conclusions. People of Mexican origin have increased prevalence of substance use and disorders with cumulative exposure to US society.
During the past 25 years, epidemiological research in the United States has consistently found that alcohol and drug use and disorders of use among Mexican immigrants and Mexican Americans tend to be associated with increasing immersion into US society.1–8 More recently, transnational effects of migration on substance use in both the United States and Mexico have become apparent. First, in a comparable Mexican population without any migration experience as a reference group, it was found that Mexican immigrants in the United States and US-born persons of Mexican origin exhibited increased risk of alcohol and drug use.9,10 Second, it was also shown that, in Mexico, substance use of return migrants and families of migrants was also affected by this immigration flow.11,12 These findings suggest a transnational pattern whereby Mexican immigrants increase their use of substances while in the United States by means of early age at immigration and years living in the United States,13–15 and transmit, directly and indirectly, substance use behaviors back into Mexico. This conceptualization is intriguing, but the data provided so far are limited to studies either in the United States or in Mexico. The only previous binational study9 collected data from a wide range of communities in Mexico and the United States and evidence with greater geographic detail is needed to corroborate and extend our understanding.
The border regions of Mexico and the United States are particularly important as settings in which the cultures of the 2 countries come into contact and as transit points for migrants moving in both directions. The border region is also filled with contrasts. The US counties are much richer than the Mexican municipalities, but some of the US counties in the border area are among the poorest in the United States. At the same time, some of the Mexican border municipalities are among the richest when compared with national Mexican averages. Research in this region has documented the impact that US nativity, age at immigration, and years living in the United States have in increasing alcohol and drug use and disorders among those of Mexican ancestry living in the US borderland.8,16–18 On the Mexican side of the border, research generally documented higher prevalence rates for substance use and disorders of use when compared with cities off the border or against national averages.19
Previous research nevertheless lacks a binational approach—with a common framework and risk factors. Our project, the first simultaneous study that includes the dynamic experiences of contemporary Mexican immigration on both sides of the border, has started to shed new insights on the alleged differences of alcohol and drug use and disorders of use in the US–Mexico border area.20,21 Our main hypothesis is that with early age of immigration, and increasing time and contact with the US culture, alcohol use, drug use, alcohol use disorders (AUDs) and symptoms of drug use disorder (DUD) will increase along a continuum of immigration experiences in this transnational population. Our main goal is to report the prevalence of, and risk factors for, the occurrence of alcohol use, drug use, AUD, and symptoms of DUD for this population of Mexican ancestry. A second goal is to put these new results in the context of previous findings and to examine the consistency of risk estimates for substance use across the full spectrum of the Mexican immigrant groups.
METHODS
The US–Mexico Study on Alcohol and Related Conditions (UMSARC) is a cross-sectional survey that interviewed probabilistically selected respondents during 2011 to 2013 in areas of the US–Mexico border. Trained interviewers conducted all interviewing with a face-to-face, computer-assisted interview. We carried out sampling simultaneously on each side by using a multistage area–probability sampling design with stratification by city. On the US side, we defined primary sampling units as census block groups with at least a 70% Hispanic population, with blocks serving as the secondary sampling unit. In Mexico, we defined primary sampling units by using the catalog of the census basic geostatistical areas, similar to block groups in the United States, with blocks within the census basic geostatistical area serving as secondary sampling units. On both sides, we randomly selected 3 households per secondary sampling unit, with eligible residents defined as those aged 18 to 65 years (both sides) who were of Mexican origin (US side only). Each household was visited at least 3 times on different days of the week and hours of the day. We took these complex design features into consideration in the generation of weights and the analyses.
Response Rate
On the US side, the border sample consisted of respondents from the 3 Texas border metropolitan areas of Laredo (Webb County; n = 751) and McAllen and Brownsville (Hidalgo and Cameron counties; n = 814); the near-border sample consisted of n = 771 respondents from the metropolitan area of San Antonio. Together, the US samples reflected a combined cooperation rate of 84% (53.1% response rate).22 We carried out parallel sampling in Mexico on respondents living in the respective border sister metropolitan areas (sister cities) of Nuevo Laredo (n = 828) and Reynosa and Matamoros (state of Tamaulipas; n = 821) and in the near-border metropolitan area counterpart of Monterrey (state of Nuevo Leon; n = 811), reflecting a combined cooperation rate of 71.4% (63.3% response rate).
Following the definition of the American Association for Public Opinion Research22 the cooperation rate includes only those households in which enumeration indicated that an eligible respondent was confirmed to reside, and the response rate is based on the fraction of those households in which enumeration was not conducted but that were estimated to contain eligible residents. The lower cooperation rate in Mexico compared with the United States was hypothesized to be a result of outbreaks of violence in the cities where data were being collected during the study period, causing potential respondents to be more fearful for their safety. Respondents in the United States were also told they would be offered a gift card for completing the interview, which may have further increased cooperation rates.
Weights, Instruments, and Variables
The approach to weighting the sample was to first calculate the weights appropriate for the cluster sample design and then to modify these weights to adjust for demographic differences between the population and the sample. In both the United States and Mexico, we first weighted data to reflect the multistage clustered sampling design. Then we used a raking algorithm23,24 approach to iteratively adjust the sampling weights to match Census marginal distributions of education and the combined gender-by-age distribution, separately within each site. To adjust for design effects inherent in multistage clustered sampling, we used Stata version 13.1 (StataCorp LP, College Station, TX) survey commands for all model parameter estimation.
We obtained data on alcohol and other substance use patterns and problems, and demographic characteristics, among other items. For this article, we selected alcohol and drug use outcomes variables that were consistent with previous reports9–12: lifetime and past-year alcohol use, any drug use (illicit or prescription-type psychotherapeutics used nonmedically), and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV),25 lifetime and past-year AUD, defined as alcohol abuse or dependence. Prescription drugs included pain relievers, sedatives, stimulants, and other prescription medicines. Illicit drugs included marijuana, cocaine or crack, heroin or opium, methamphetamines, hallucinogens, and other recreational drugs. Limited interview time precluded a parallel assessment of DUD so, as an alternative, we selected 2 items from the DSM-IV with a high prevalence of endorsement across different drugs26,27: recurrent use in physically dangerous situations (e.g., while driving, operating machinery) or injury while drinking (hazardous use), and persistent desire, or unsuccessful efforts, to reduce consumption (quit or control). The report of these 2 symptoms of DUD can be interpreted here only as a marker of heavier drug involvement.
Independent variables.
Our main independent variable for these analyses was a variable with 7 mutually exclusive groups representing a continuum of migration experience in the Mexican and Mexican American populations. In Mexico, respondents were asked if they ever migrated to the United States (n = 58 respondents) or have a family member living in the United States (Mexican migrant background; n = 270) or not (Mexicans with no migrant experience; n = 2124). In the United States, respondents were asked if they were born in Mexico and arrived after or at age 13 years (Mexican immigrants first generation ≥ 13 years; n = 467) or before age 13 years (Mexican immigrants first generation < 13 years; n = 227), born in the United States with no US-born parent (second generation; n = 702), or born in the United States from at least 1 US-born parent (third generation; n = 932).9,11 The decision to define early versus late arrival of immigrants as before or after age 13 years was made on the basis of previous research on immigration and risk for psychiatric and substance use disorders.2 Thus, the first 3 groups represent Mexicans interviewed in Mexico, whereas the other 4 groups were Mexican immigrants and Mexican Americans interviewed in the United States. For this variable, Mexicans with no migrant experience was the nonexposed group for all comparisons.
We included other variables known or suspected to influence the prevalence of alcohol and drug use and disorders as statistical controls in our main models. The demographic variables were gender, age, education, marital status, and whether the interview was conducted in a border city. We also included variables related to the mobility of this border population that could affect the prevalence of alcohol and drug use. They were whether the respondent was a native of the surveyed city (and in the case of immigrants, whether they had lived in that city since their arrival), and whether the respondent visited the neighbor country in the past 12 months.
Data analyses.
After estimating the prevalence of key demographic and mobility variables and the prevalence of alcohol and drug use among immigrant groups in the UMSARC, we estimated odds ratios (ORs) in logistic regression models28 with Stata software to adjust for design effects, with and without statistical adjustment for sociodemographic and mobility variables. We used weights developed for the UMSARC as described previously. We conducted significance tests of cross-tabulations by using the design-based Pearson χ2 test. We estimated standard errors and 95% confidence intervals (CIs) of coefficients by the Taylor series method with Stata version 13.1 to adjust for the design effects, stratification, clustering, and unequal weighting of the observations.29
Other data sets.
For the comparison of OR estimates from previous studies, 1 other data set was available that included the full spectrum of migrant groups (7 groups),9 whereas 3 other data sets included only the 3 groups interviewed in Mexico, as described previously.9,12,30 Odds ratio estimates of immigration and alcohol and drug use and disorders, which are compared with the current findings from the UMSARC, are available for 2 previous reports that used these data sets,9,12 whereas for the Encuesta Nacional de Adicciones 2008,10,31 these estimates were unpublished and newly calculated for the current report.
RESULTS
A total of 2336 Mexican Americans from Texas and 2460 Mexicans from the states of Nuevo Leon and Tamaulipas participated. Table 1 presents the basic demographic information for the sample by migration status. All variables showed significant differences across migration groups. Mexicans with no migration experience were younger whereas Mexican immigrants that arrived later were older; second-generation Mexican Americans had the highest level of educational attainment, whereas return migrants had the lowest; and single people were more common among third-generation Mexican Americans, whereas married people were more common in the Mexican immigrant group that arrived later. The highest prevalence of residing in a border city was among return migrants and the lowest among third-generation Mexican Americans. Mexican immigrants that arrived late were more likely to visit the neighbor country within the past 12 months and third-generation Mexican Americans the least likely, and return migrants were more likely to be nonnative to the surveyed city, whereas third-generation Mexican Americans were more likely to be a native.
TABLE 1—
Sociodemographic, Nativity, and Cross-Border Mobility by Migration Category: US–Mexico Study on Alcohol and Related Conditions Survey, 2011–2013
| Characteristic | Mexican Without Migrant Experience, No. (Weighted %) | Mexican With a Family Member in the United States, No. (Weighted %) | Mexican Return Migrant, No. (Weighted %) | US Immigrants First Generation Aged ≥ 13 y, No. (Weighted %) | US Immigrants First Generation Aged < 13 y, No. (Weighted %) | US-Born Second Generation, No. (Weighted %) | US-Born Third-Plus Generation, No. (Weighted %) | P |
| Gender | < .001 | |||||||
| Male | 1216 (49.4) | 133 (42.1) | 54 (87.2) | 203 (41.3) | 112 (49.1) | 364 (50.0) | 468 (49.3) | |
| Female | 908 (50.6) | 137 (57.9) | 4 (12.8) | 264 (58.7) | 115 (50.9) | 338 (50.0) | 464 (50.7) | |
| Age category, y | < .001 | |||||||
| 18–29 | 773 (35.3) | 38 (14.3) | 11 (13.1) | 75 (14.8) | 75 (28.8) | 260 (35.0) | 333 (35.4) | |
| 30–49 | 942 (48.4) | 125 (55.1) | 33 (61.3) | 250 (50.2) | 99 (49.1) | 318 (48.1) | 378 (40.6) | |
| ≥ 50 | 409 (16.3) | 107 (30.6) | 14 (25.6) | 142 (35.0) | 53 (22.1) | 124 (16.9) | 221 (24.1) | |
| Education | < .001 | |||||||
| < high-school graduate | 1274 (67.8) | 192 (77.6) | 43 (78.5) | 285 (69.5) | 85 (40.4) | 178 (23.4) | 234 (22.0) | |
| High-school graduate | 424 (15.7) | 37 (10.8) | 8 (9.9) | 70 (9.7) | 45 (16.3) | 166 (20.3) | 248 (26.0) | |
| Some college | 126 (5.3) | 9 (2.1) | 2 (3.2) | 54 (8.1) | 62 (22.6) | 239 (30.6) | 321 (34.1) | |
| College graduate | 277 (11.2) | 31 (9.5) | 5 (8.4) | 56 (12.7) | 35 (20.7) | 119 (25.8) | 129 (17.9) | |
| Marital status | < .001 | |||||||
| Single | 664 (30.6) | 45 (15.4) | 11 (21.0) | 53 (11.5) | 63 (27.7) | 233 (32.4) | 329 (35.4) | |
| Married or living together | 1127 (53.4) | 165 (60.4) | 33 (58.4) | 339 (74.1) | 126 (57.5) | 340 (48.1) | 415 (44.9) | |
| Separated or divorced | 236 (11.8) | 37 (18.1) | 10 (19.5) | 55 (10.0) | 37 (14.5) | 113 (16.6) | 167 (16.7) | |
| Widowed | 94 (4.1) | 21 (6.0) | 4 (1.2) | 20 (4.3) | 1 (0.3) | 16 (2.9) | 20 (3.0) | |
| Border area | < .001 | |||||||
| No | 752 (35.0) | 49 (19.9) | 9 (16.8) | 121 (30.3) | 46 (17.6) | 159 (20.9) | 441 (48.8) | |
| Yes | 1372 (65.0) | 221 (80.1) | 49 (83.2) | 346 (69.7) | 181 (82.4) | 543 (79.1) | 491 (51.2) | |
| Native of survey city | < .001 | |||||||
| No | 654 (33.0) | 99 (38.7) | 31 (49.9) | 131 (30.2) | 54 (24.0) | 227 (34.9) | 219 (24.5) | |
| Yes | 1469 (67.0) | 171 (61.3) | 27 (50.1) | 336 (69.8) | 173 (76.0) | 475 (65.1) | 713 (75.5) | |
| In neighbor country past 12 mo | < .001 | |||||||
| No | 1770 (85.6) | 177 (69.4) | 50 (81.5) | 246 (51.3) | 136 (62.5) | 445 (60.4) | 818 (88.3) | |
| Yes | 348 (14.4) | 93 (30.6) | 8 (18.5) | 221 (48.7) | 91 (37.5) | 257 (39.6) | 113 (11.7) |
Table 2 shows the lifetime and past-12-month prevalence of alcohol, AUD, drug use, and DUD symptoms by immigrant groups. In general, these prevalences tended to increase with increasing time into US society. For example, the prevalence of lifetime drug use was 10.5% among Mexicans with no migrant experience, 13.4% among families of immigrants, 30.8% among return migrants, and 24.7% among later immigrants, increasing sharply among the first generation of early immigrants (38.6%) and even higher among second (47.3%) and third generations (55.0%). The prevalence of other outcomes tended also to increase in a similar fashion.
TABLE 2—
Prevalence of Alcohol Use, Alcohol Use Disorders, Drug Use, and 2 Symptoms of Drug Use Disorder, by Migration Category: US–Mexico Study on Alcohol and Related Conditions Survey, 2011–2013
| Variable | Mexican Without Migrant Experience, No. (Weighted %) | Mexican With a Family Member in the United States, No. (Weighted %) | Mexican Return Migrant, No. (Weighted %) | US Immigrants First Generation Aged ≥ 13 y, No. (Weighted %) | US Immigrants First Generation Aged < 13 y, No. (Weighted %) | US-Born Second Generation, No. (Weighted %) | US-Born Third-Plus Generation, No. (Weighted %) | P |
| Lifetime alcohol use | < .001 | |||||||
| No | 822 (41.0) | 118 (47.0) | 5 (11.9) | 159 (35.2) | 43 (20.6) | 124 (17.3) | 125 (13.7) | |
| Yes | 1300 (59.0) | 152 (53.0) | 53 (88.1) | 308 (64.8) | 184 (79.4) | 578 (82.7) | 807 (86.3) | |
| Past-year alcohol use | < .001 | |||||||
| No | 1005 (48.3) | 143 (53.5) | 13 (19.3) | 206 (44.3) | 56 (26.9) | 169 (23.6) | 214 (23.0) | |
| Yes | 1117 (51.7) | 127 (46.5) | 45 (80.7) | 261 (55.7) | 171 (73.1) | 533 (76.4) | 718 (77.0) | |
| Lifetime any drug use | < .001 | |||||||
| No | 1880 (89.5) | 229 (86.6) | 39 (69.2) | 348 (75.3) | 135 (61.4) | 354 (52.7) | 396 (45.0) | |
| Yes | 241 (10.5) | 40 (13.4) | 19 (30.8) | 119 (24.7) | 92 (38.6) | 348 (47.3) | 533 (55.0) | |
| Past-year any drug use | < .001 | |||||||
| No | 1999 (94.8) | 251 (94.7) | 50 (87.6) | 411 (86.0) | 179 (76.8) | 534 (76.8) | 668 (74.3) | |
| Yes | 114 (5.2) | 18 (5.3) | 8 (12.4) | 56 (14.0) | 47 (23.2) | 168 (23.2) | 259 (25.7) | |
| Past year any DSM-IV alcohol-use disorder | < .001 | |||||||
| No | 1960 (92.5) | 251 (93.8) | 39 (67.8) | 420 (91.1) | 193 (84.4) | 567 (81.2) | 753 (81.7) | |
| Yes | 164 (7.5) | 19 (6.2) | 19 (32.2) | 47 (8.9) | 34 (15.6) | 135 (18.8) | 179 (18.3) | |
| Lifetime drug-use disorder symptoms | < .001 | |||||||
| No | 2041 (98.2) | 255 (97.2) | 47 (83.3) | 429 (95.0) | 198 (88.5) | 580 (84.1) | 721 (79.5) | |
| Yes | 47 (1.8) | 8 (2.8) | 11 (16.7) | 28 (5.0) | 28 (11.5) | 112 (15.9) | 194 (20.5) | |
| Past-year drug-use disorder symptoms | < .001 | |||||||
| No | 2064 (99.1) | 260 (99.3) | 53 (91.6) | 448 (98.6) | 213 (93.4) | 647 (93.6) | 839 (93.2) | |
| Yes | 24 (0.9) | 3 (0.7) | 5 (8.4) | 9 (1.4) | 13 (6.6) | 45 (6.4) | 76 (6.8) |
Note. DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.25 Drug-use disorder symptoms are hazardous use and quit or control. Drug use includes prescription drugs (pain relievers, sedatives, stimulants, and other prescription drugs) and illicit drugs (marijuana, cocaine or crack, heroin or opium, methamphetamines, hallucinogens, and other recreational drugs).
The differences in the prevalence persisted after we adjusted for demographics and mobility factors by using logistic regression models for estimating ORs (Table 3). In summary, we describe the effects on past-year alcohol use and 12-month DUD symptoms, which represent 2 ends of a spectrum (i.e., from the least-problematic simple alcohol use to the most-serious DUD symptoms). When compared with Mexicans with no migrant experience, the adjusted ORs of past-year alcohol use were 0.99 (95% CI = 0.78, 1.27) for families of migrants, 3.17 (95% CI = 1.51, 6.64) for return migrants, 1.36 (95% CI = 1.08, 1.71) for Mexican-born respondents living in the United States and arriving later, 2.53 (95% CI = 1.85, 3.46) for Mexican-born respondents living in the United States and arriving earlier, 2.95 (95% CI = 2.41, 3.63) for US-born second-generation, and 3.32 (95% CI = 2.67, 4.13) for US-born third-plus generation.
TABLE 3—
Association of Alcohol Use, Alcohol-Use Disorders, Drug Use, and 2 Symptoms of Drug Use Disorder, With Migration Category, Adjusted by Demographic and Mobility Variables: US–Mexico Study on Alcohol and Related Conditions Survey, 2011–2013
| Variable | Lifetime Alcohol Use, OR (95% CI) | Past-Year Alcohol Use, OR (95% CI) | Lifetime Any Drug Use, OR (95% CI) | Past-Year Any Drug Use, OR (95% CI) | Past-Year Any DSM-IV Alcohol-Use Disorder, OR (95% CI) | Lifetime Drug-Use Disorder Symptoms, OR (95% CI) | Past-Year Drug-Use Disorder Symptoms, OR (95% CI) |
| Mexican without migrant experience (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Mexican with a family member in the United States | 0.92 (0.72, 1.18) | 0.99 (0.78, 1.27) | 1.58 (1.10, 2.27) | 1.10 (0.66, 1.82) | 1.09 (0.65, 1.80) | 2.03 (0.94, 4.37) | 1.13 (0.38, 3.39) |
| Mexican return migrant | 3.70 (1.39, 9.85) | 3.17 (1.51, 6.64) | 2.84 (1.61, 5.01) | 2.12 (1.00, 4.49) | 5.07 (2.86, 8.99) | 8.43 (4.19, 16.98) | 8.95 (3.09, 25.91) |
| US immigrants first generation aged ≥ 13 y | 1.48 (1.16, 1.89) | 1.36 (1.08, 1.71) | 3.73 (2.76, 5.05) | 3.57 (2.38, 5.37) | 1.74 (1.10, 2.75) | 3.83 (2.38, 6.18) | 2.52 (1.21, 5.27) |
| US immigrants first generation aged < 13 y | 2.71 (1.90, 3.86) | 2.53 (1.85, 3.46) | 6.91 (5.05, 9.44) | 5.97 (4.02, 8.84) | 2.67 (1.82, 3.92) | 8.17 (5.01, 13.34) | 8.48 (4.29, 16.76) |
| US-born second generation | 3.34 (2.68, 4.16) | 2.95 (2.41, 3.63) | 10.64 (8.38, 13.50) | 6.52 (4.82, 8.83) | 3.32 (2.59, 4.27) | 11.65 (8.03, 16.90) | 8.00 (4.68, 13.66) |
| US-born third-plus generation | 4.66 (3.59, 6.04) | 3.32 (2.67, 4.13) | 15.10 (11.97, 19.06) | 8.85 (6.62, 11.84) | 3.32 (2.60, 4.24) | 16.63 (11.61, 23.83) | 9.95 (6.11, 16.22) |
Note. CI = confidence interval; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition25; OR = odds ratios computed with logistic regression models (standard errors were corrected using the SVY module in Stata version 13.1 [StataCorp LP, College Station, TX]). Drug use disorder symptoms are hazardous use and quit or control. Models adjusted by gender, continuous age, education (less than high school vs other), married (vs not married), border area, native of survey area, and being in the neighbor country in the past year. Drug use includes prescription drugs (pain relievers, sedatives, stimulants, and other prescription drugs) and illicit drugs (marijuana, cocaine or crack, heroin or opium, methamphetamines, hallucinogens, and other recreational drugs).
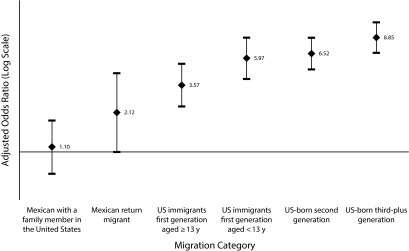
In the same vein, when compared with Mexicans with no migrant experience, the adjusted ORs of past-year DUD symptoms was 1.13 (95% CI = 0.38, 3.39) for families of migrants, 8.95 (95% CI = 3.09, 25.91) for return migrants, 2.52 (95% CI = 1.21, 5.27) for Mexican-born respondents living in the United States and arriving later, 8.48 (95% CI = 4.29, 16.76) for Mexican-born respondents living in the United States and arriving earlier, 8.00 (95% CI = 4.68, 13.66) for US-born second-generation, and 9.95 (95% CI = 6.11, 16.22) for US-born third-plus generation. Figure 1 presents these results for past-year use of any drug that shows a clear tendency for increased ORs with cumulative exposure to US society.
FIGURE 1—
Association of Past-Year Any Drug Use With Migration Category: US–Mexico Study on Alcohol and Related Conditions Survey, 2011–2013
Note. Whiskers indicate 95% confidence intervals. Reference category = Mexican without migrant experience. Odds ratios and 95% confidence intervals adjusted by demographic and mobility variables.
Table 4 presents a summary of all studies to date that have a Mexican population without a migrant experience as a baseline, nonexposed group for estimating ORs for alcohol and drug use and related disorders between Mexican immigration groups. Together, these studies sum 36 362 observations. Although estimates for lifetime alcohol and drug use are 100% comparable across studies, the time frame (lifetime or 12-month) and definition of substance use disorder (DSM-IV, problems and symptoms of disorder) are different across some studies, especially for DUD, but less so for AUD. By putting together all these studies, limitations from studies carried within specific border areas on one hand and studies that used wider national samples on the other hand can be compared.
TABLE 4—
Alcohol and Drug Use and Disorders (Problems) Associated With Migration Experience Among Mexican and Mexican-Origin Populations: Results From 4 Studies, 2001–2013
| Study (Publication Year) and Migrant Categorya | No. | Lifetime Alcohol Use, AOR (95% CI) | Lifetime Any Drug Use, AOR (95% CI) |
DSM-IV Alcohol Use Disorder |
Lifetime Drug Problems |
|||
| Timeframe | Type | ORb (95% CI) | Type | ORb (95% CI) | ||||
| Study 1 (2009)c,12 | ||||||||
| Mexican with a family member in the United States | 272 | 1.30 (0.75, 2.23) | 1.17 (0.63, 2.18) | 12 mo | Dep | 1.10 (0.56, 2.16) | Prob | 1.42 (0.38, 5.26) |
| Mexican return migrant | 100 | 3.40 (1.61, 7.15) | 2.48 (1.33, 4.63) | 12 mo | Dep | 2.23 (0.93, 5.36) | Prob | 4.73 (2.24, 9.99) |
| Study 2 (2012)d,30 | ||||||||
| Mexican with a family member in the United States | 2975 | 1.60 (1.39, 1.84) | 0.79 (0.62, 1.01) | 12 mo | AUD | 1.38 (0.93, 2.05) | Prob | 0.93 (0.64, 1.34) |
| Mexican return migrante | 1050 | 2.19 (1.72, 2.78) | 1.65 (1.27, 2.14) | 12 mo | AUD | 1.31 (0.97, 1.77) | Prob | 1.59 (1.13, 2.23) |
| Study 3 (2007 and 2011)f,9,11 | ||||||||
| Mexican with a family member in the United States | 2519 | 1.18 (1.09, 1.29) | 1.49 (1.15, 1.92) | LT | AUD | 1.48 (1.14, 1.92) | DUD | 3.22 (1.80, 5.78) |
| Mexican return migrant | 385 | 1.41 (1.20, 1.66) | 2.33 (1.59, 3.40) | LT | AUD | 1.93 (1.19, 3.13) | DUD | 3.57 (1.38, 9.24) |
| US immigrants first generation aged ≥ 13 y | 412 | 0.81 (0.57, 1.17) | 6.55 (3.81, 11.26) | LT | AUD | 1.31 (0.73, 2.36) | DUD | 3.71 (1.72, 8.03) |
| US immigrants first generation aged < 13 y | 136 | 1.22 (0.98, 1.52) | 5.13 (3.19, 8.25) | LT | AUD | 0.84 (0.45, 1.55) | DUD | 4.71 (1.86, 11.93) |
| US-born second generation | 172 | 1.82 (1.44, 2.32) | 8.05 (5.70, 11.37) | LT | AUD | 2.72 (1.61, 4.62) | DUD | 13.70 (7.24, 25.94) |
| US-born third-plus generation | 488 | 2.04 (1.66, 2.51) | 13.26 (9.55, 18.42) | LT | AUD | 3.65 (2.49, 5.36) | DUD | 14.17 (7.94, 25.29) |
| Study 4 (2014)g,20 | ||||||||
| Mexican with a family member in the United States | 270 | 0.92 (0.72, 1.18) | 1.58 (1.10, 2.27) | 12 mo | AUD | 1.09 (0.65, 1.80) | Scr | 2.03 (0.94, 4.37) |
| Mexican return migrant (current) | 58 | 3.70 (1.39, 9.85) | 2.84 (1.61, 5.01) | 12 mo | AUD | 5.07 (2.86, 8.99) | Scr | 8.43 (4.19, 16.98) |
| US immigrants first generation aged ≥ 13 y | 467 | 1.48 (1.16, 1.89) | 3.73 (2.76, 5.05) | 12 mo | AUD | 1.74 (1.10, 2.75) | Scr | 3.83 (2.38, 6.18) |
| US immigrants first generation aged < 13 y | 227 | 2.71 (1.90, 3.86) | 6.91 (5.05, 9.44) | 12 mo | AUD | 2.67 (1.82, 3.92) | Scr | 8.17 (5.01, 13.34) |
| US-born second generation | 702 | 3.34 (2.68, 4.16) | 10.64 (8.38, 13.50) | 12 mo | AUD | 3.32 (2.59, 4.27) | Scr | 11.65 (8.03, 16.90) |
| US-born third-plus generation | 932 | 4.66 (3.59, 6.04) | 15.10 (11.97, 19.06) | 12 mo | AUD | 3.32 (2.60, 4.24) | Scr | 16.63 (11.61, 23.83) |
Note. AOR = adjusted odds ratio; AUD = DSM-IV alcohol-use disorders (abuse or dependence); CI = confidence interval; Dep = dependence; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DUD = DSM-IV drug-use disorders (abuse or dependence); LT = lifetime; OR = odds ratio; Prob = problems; Scr = screening of 2 drug-use disorder symptoms: hazardous use and quit or control.
Reference group is Mexicans (living in Mexico) without migrant experience.
Adjusted estimates (except for study 1—crude estimates).
Mexican National Addiction Survey in 3 Mexican northern cities, 2005. Total n = 1630; adjusted estimates by gender, age, marital status, education, and city of residence.
Mexican National Addiction Survey, 2008. Total n = 22 962; adjusted estimates by gender, age, education, marital status, region, border metropolitan area, and employment.
Borges and Medina-Mora, unpublished data, 2014.
Mexican National Comorbidity Survey, 2001–2002 and the Mexican Sample from the American Collaborative Psychiatric Epidemiology Surveys, 2001–2003. Total n = 6990; adjusted estimates by gender, age, education, any mood disorder, any anxiety disorder, and person years as a categorical variable.
US–Mexico Study on Alcohol and Related Conditions Survey in 4 Mexican northern cities, 2011–2013. Total n = 4780; adjusted estimates by gender, age, education, marital status, border area, native of survey city, and being in the neighbor country in the past year.
For brevity, we only stress 2 main patterns that stand out in the comparison of these results (with a few exceptions). First, as we move from families of migrants to return migrants, and from first to second-plus generation of US-born people of Mexican ancestry, the ORs for these outcomes move away from the null, with higher ORs and CIs that do not include the null along this continuum of migration experiences. That is, more robust and increased ORs are found with higher levels of exposure to US society. Second, estimates for the impact of immigration on increasing drug use and DUD tended to be more consistent and robust than the ones found for alcohol use and AUD. That is, across all migration groups, the associations between immigration and drug use and disorders are consistently higher than the ones reported for alcohol use and disorders.
DISCUSSION
Findings suggest strong associations of migration with the occurrence of alcohol and drug use and disorders of use in the population of Mexican ancestry living on both sides of the Mexico–US border. These findings were generally consistent with the hypothesized association between greater alcohol and drug use, AUD, and symptoms of DUD, and more intensive exposure to American society. With increasingly complex patterns of immigration in modern times, knowledge of baseline rates of alcohol and drug use and their related disorders among immigrant groups, as provided here, are needed but seldom available.32 Our study design allowed us to discard that common sources of bias33 in research of immigrants34–36 could fully explain the findings reported here.
Consistency of Findings Across Studies
The finding that immigration to the United States has such a profound and extensive effect on different segments of this Mexican transnational population mirrors our 2 previous reports9,10 and it is unlikely that this finding can be solely attributed to a single factor. In Mexico, migration-related factors that affect substance-related outcomes may include changes in domestic arrangements because of a missing family member,37 and the way in which immigrants affected by alcohol and drug use disorders search for mental health services and treat their disorders, either in the United States or in Mexico.9,33,36,38 In the United States, substance use and disorders may be linked to the so-called acculturation process,13,39,40 including nativity, time in the United States, and age of immigration3,6,14,41; to language, social relations, and assimilation changes42; to baseline and cultural differences among Hispanic ethnicities43; or, more simply, to changes in alcohol and drug norms together with changes in availability of these substances.9,10,15
It is also important to consider that, although the US-born Mexican Americans have levels of alcohol and drug use and disorders that are much higher than those of Mexicans in Mexico, evidence from other studies suggests that they may not differ substantially from other US-born minority ethnic groups.44,45 This suggests that a great deal of the differences between Mexicans and Mexican Americans are attributable to baseline differences in the prevalence of mental disorders (including substance use disorders) between both countries46,47 and that the factors contributing to the high level of substance use among Mexican Americans relative to Mexicans in Mexico may not be distinctive exposures associated with migration, but rather exposures broadly shared within the US population, regardless of ethnicity.48 This study contributes to the larger goal of understanding these factors by exploring a particular geographic site within the transnational flow of migrants, the border region. Identifying the pattern of association between migration and substance use in this region, differentiating by type of drug, is an important step toward studies targeted to specific explanatory factors.
Limitations
Our results should be viewed within the scope of some limitations. First, we selected the sister cities in the Texas–Tamaulipas and Nuevo Leon border to increase homogeneity of the comparisons and these are not representative of other sister cities in these states or in other sister cities of other states in the US–Mexico border, or other ethnic minorities in the border; nor are the off-border cities selected for comparison representative of the entire interior of each country.
A second limitation lies in the reduced response rates. In the United States, the response rate probably reflects a general trend toward lower participation in surveys of this kind that could be even more apparent in a population that may include persons without proper immigration status. In Mexico, although the rate was somewhat better, lack of confidence in surveys during a period of high violence and crime probably accounted for lower participation. Although our response rates seem low, they are within other surveys’ range on the topic both for the region17 and nationally.49 Even with lower response rates, current evidence suggests growing nonresponse may not necessarily lead to additional bias in samples.50
The screening measure of DUD is limited because it may underestimate the true prevalence of DUD by yielding a large number of false-negatives and cannot substitute a true diagnostic instrument. Although both the studies in Mexico and in the United States were conducted simultaneously, using the same methodology and questionnaire, the political, economic, and security situation in Mexico was in particular turmoil during the period of data collection. The combination of data from 4 surveys showed the consistency of our findings; however, these surveys were conducted almost 15 years apart. This period witnessed a peak in Mexican migration to the United States, the acceleration of the Mexican drug war, and strengthened security and border control in the United States. In summation, during this period the migration process and exposure to the US culture was subject to multiple contributory risk factors that could have had an impact on our estimates but that are well beyond the scope of this research. Finally, the present study was cross-sectional, and although we found some associations of interest, we cannot claim causality in these associations.
Conclusions
Despite these limitations, this study presents new evidence regarding differences in alcohol and drug use related to migration across the US–Mexico border and placed those findings in the context of cross-national research on US–Mexico migration and substance use. This is an important step toward localizing the transnational cultural and social changes that occur with migration and may have broad impacts on health-related behaviors. The finding that patterns in the border region are broadly similar to patterns observed across the 2 countries as a whole in previous epidemiological studies of nationally representative data sets suggests that there are some stable cultural factors in the 2 countries that shape substance use behaviors, despite the frequent movement of individuals from one setting to the other. Further examination of cross-national patterns of substance use, differentiating by type of drug, with binational data, is needed to explore this dynamic in greater detail. These studies have the potential to shed light on how the movement of individuals between populations influences population health in both the sending and receiving populations. Longitudinal studies that can reveal individual trajectories of substance use over time in relationship to migration experiences will be particularly useful.
ACKNOWLEDGMENTS
This study was funded by National Institute on Alcohol Abuse and Alcoholism grant R01AA018365 (C. J. C., PI).
HUMAN PARTICIPANT PROTECTION
Written informed consent was obtained from all respondents. Institutional review boards from the Alcohol Research Group–Public Health Institute in the United States and the Instituto Nacional de Psiquiatría in Mexico approved the research protocol and questionnaire.
REFERENCES
- 1.Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. Am J Public Health. 2007;97(1):68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Breslau J, Aguilar-Gaxiola S, Borges G, Kendler KS, Su M, Kessler RC. Risk for psychiatric disorder among immigrants and their US-born descendants: evidence from the National Comorbidity Survey Replication. J Nerv Ment Dis. 2007;195(3):189–195. doi: 10.1097/01.nmd.0000243779.35541.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic Whites in the United States. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(12):1226–1233. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- 4.Karno M, Golding JM, Burnam MA et al. Anxiety disorders among Mexican Americans and non-Hispanic Whites in Los Angeles. J Nerv Ment Dis. 1989;177(4):202–209. doi: 10.1097/00005053-198904000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Ortega AN, Rosenheck R, Alegría M, Desai R. Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. J Nerv Ment Dis. 2000;188(11):728–735. doi: 10.1097/00005053-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Arch Gen Psychiatry. 1998;55(9):771–778. doi: 10.1001/archpsyc.55.9.771. [DOI] [PubMed] [Google Scholar]
- 7.Caetano R, Medina-Mora ME. Acculturation and drinking among people of Mexican descent in Mexico and the United States. J Stud Alcohol. 1988;49(5):462–471. doi: 10.15288/jsa.1988.49.462. [DOI] [PubMed] [Google Scholar]
- 8.Wallisch LS, Spence RT. Alcohol and drug use, abuse, and dependence in urban areas and colonias of the Texas–Mexico border. Hisp J Behav Sci. 2006;28(2):286–307. [Google Scholar]
- 9.Borges G, Breslau J, Orozco R et al. A cross-national study on Mexico–US migration, substance use and substance use disorders. Drug Alcohol Depend. 2011;117(1):16–23. doi: 10.1016/j.drugalcdep.2010.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Borges G, Rafful C, Benjet C et al. Mexican immigration to the US and alcohol and drug use opportunities: does it make a difference in alcohol and/or drug use? Drug Alcohol Depend. 2012;125(suppl 1):S4–S11. doi: 10.1016/j.drugalcdep.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borges G, Medina-Mora ME, Breslau J, Aguilar-Gaxiola S. The effect of migration to the United States on substance use disorders among returned Mexican migrants and families of migrants. Am J Public Health. 2007;97(10):1847–1851. doi: 10.2105/AJPH.2006.097915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borges G, Medina-Mora ME, Orozco R, Fleiz C, Cherpitel C, Breslau J. The Mexican migration to the US and substance use in Northern Mexico. Addiction. 2009;104(4):603–611. doi: 10.1111/j.1360-0443.2008.02491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burnam MA, Hough RL, Karno M, Escobar JI, Telles CA. Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. J Health Soc Behav. 1987;28(1):89–102. [PubMed] [Google Scholar]
- 14.Vega WA, Sribney WM, Aguilar-Gaxiola S, Kolody B. 12-month prevalence of DSM-III-R psychiatric disorders among Mexican Americans: nativity, social assimilation, and age determinants. J Nerv Ment Dis. 2004;192(8):532–541. doi: 10.1097/01.nmd.0000135477.57357.b2. [DOI] [PubMed] [Google Scholar]
- 15.Shmulewitz D, Wall M, Keyes K et al. Alcohol use disorders and perceived drinking norms: ethnic differences in Israeli adults. J Stud Alcohol Drugs. 2012;73(6):981–990. doi: 10.15288/jsad.2012.73.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reingle JM, Caetano R, Mills BA, Vaeth PA. The role of immigration age on alcohol and drug use among border and non-border Mexican Americans. Alcohol Clin Exp Res. 2014;38(7):2080–2086. doi: 10.1111/acer.12440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Caetano R, Mills B, Vaeth PA. Alcohol consumption and binge drinking among US–Mexico border and non-border Mexican Americans. Alcohol Clin Exp Res. 2012;36(4):677–685. doi: 10.1111/j.1530-0277.2011.01652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caetano R, Vaeth PA, Mills BA, Rodriguez LA. Alcohol abuse and dependence among US–Mexico border and non-border Mexican Americans. Alcohol Clin Exp Res. 2013;37(5):847–853. doi: 10.1111/acer.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Medina-Mora ME, Conyer RT, Sepúlveda J et al. Scope of the consumption of drugs in Mexico: results of the National Survey of Drug Addictions [in Spanish] Salud Ment. 1989;12(2):7–12. [Google Scholar]
- 20.Borges G, Zemore SE, Orozco R et al. Co-occurrence of alcohol, drug use, DSM-5 alcohol use disorder, and symptoms of drug use disorder on both sides of the US–Mexico border. Alcohol Clin Exp Res. 2015;39(4):679–687. doi: 10.1111/acer.12672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cherpitel CJ, Ye Y, Bond J, Zemore SE, Borges G, Greenfield TK. Border effects on DSM-5 alcohol use disorders on both sides of the US–Mexico border. Drug Alcohol Depend. 2015;148:172–179. doi: 10.1016/j.drugalcdep.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 7th ed. Deerfield, IL: The American Association for Public Opinion Research; 2011. [Google Scholar]
- 23.Deville JC, Särndal CE, Sautory O. Generalized raking procedures in survey sampling. J Am Stat Assoc. 1993;88(423):1013–1020. [Google Scholar]
- 24.Izrael D, Hoaglin DC, Battaglia MP. SUGI 29 Proceedings. Cary, NC: SAS Institute Inc; 2004. To rake or not to rake is not the question anymore with the enhanced raking macro; pp. 207–229. [Google Scholar]
- 25.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 26.Hasin DS, Fentom MC, Beseler C, Park J, Wall M. Analyses related to the development of DSM-5 criteria for substance use related disorders: 2. Proposed DSM-5 criteria for alcohol, cannabis, cocaine and heroin disorders in 663 substance abuse patients. Drug Alcohol Depend. 2012;122(1-2):28–37. doi: 10.1016/j.drugalcdep.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saha TD, Compton W, Chou S et al. Analyses related to the development of DSM-5 criteria for substance use related disorders 1. Toward amphetamine, cocaine, and prescription drug use disorder continua using Item Response Theory. Drug Alcohol Depend. 2012;122(1-2):38–46. doi: 10.1016/j.drugalcdep.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York, NY: Wiley and Sons; 2000. [Google Scholar]
- 29.Stata Corp. Stata 13 Survey Data Reference Manual. College Station, TX: Stata Press; 2013. [Google Scholar]
- 30.Borges G, Orozco R, Medina-Mora ME. Risk index for attempted suicide in Mexico [in Spanish] Salud Publica Mex. 2012;54(6):595–606. doi: 10.1590/s0036-36342012000600008. [DOI] [PubMed] [Google Scholar]
- 31. Secretaria de Salud, Consejo Nacional contra las Adicciones, Instituto Nacional de Psiquiatría, Fundación Gonzalo Rio Arronte. National Addiction Survey 2008 [in Spanish]. México DF, México: Instituto Nacional de Salud Pública; 2009.
- 32.Stillman S, McKenzie D, Gibson J. Migration and mental health: evidence from a natural experiment. J Health Econ. 2009;28(3):677–687. doi: 10.1016/j.jhealeco.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 33.Abraído-Lanza AF. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89(10):1543–1548. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Breslau J, Borges G, Tancredi D et al. Migration from Mexico to the US and subsequent risk for depressive and anxiety disorders: a cross-national study. Arch Gen Psychiatry. 2011;68(4):428–433. doi: 10.1001/archgenpsychiatry.2011.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Nobles J, Rubalcava L. Migration and mental health: the immigrant advantage revisited. Presented at: Population Association of America 2013 Annual Meeting; April 11–13, 2013; New Orleans, LA.
- 36.Aguila E, Escarce J, Leng M, Morales L. Health status and behavioral risk factors in older adult Mexicans and Mexican immigrants to the United States. J Aging Health. 2013;25(1):136–158. doi: 10.1177/0898264312468155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Salgado de Snyder VN. Family life across the border—Mexican wives left behind. Hisp J Behav Sci. 1993;15:391–401. [Google Scholar]
- 38.Zemore SE, Mulia N, Ye Y, Borges G, Greenfield TK. Gender, acculturation, and other barriers to alcohol treatment utilization among Latinos in three National Alcohol Surveys. J Subst Abuse Treat. 2009;36(4):446–456. doi: 10.1016/j.jsat.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zemore SE. Acculturation and alcohol among Latino adults in the United States: a comprehensive review. Alcohol Clin Exp Res. 2007;31(12):1968–1990. doi: 10.1111/j.1530-0277.2007.00532.x. [DOI] [PubMed] [Google Scholar]
- 40.Caetano R. Acculturation, drinking and social settings among US Hispanics. Drug Alcohol Depend. 1987;19(3):215–226. doi: 10.1016/0376-8716(87)90041-x. [DOI] [PubMed] [Google Scholar]
- 41.Alegría M, Sribney W, Woo M, Torres M, Guarnaccia P. Looking beyond nativity: the relation of age of immigration, length of residence, and birth cohorts to the risk of onset of psychiatric disorders for Latinos. Res Hum Dev. 2007;4(1):19–47. doi: 10.1080/15427600701480980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Canino G, Vega WA, Sribney WM, Warner LA, Alegría M. Social relationships, social assimilation, and substance-use disorders among adult Latinos in the US. J Drug Issues. 2008;38(1):69–101. doi: 10.1177/002204260803800104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alegría M, Canino G, Stinson FS, Grant BF. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and non-Latino Whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67(1):56–65. doi: 10.4088/jcp.v67n0109. [DOI] [PubMed] [Google Scholar]
- 44.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 45.Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(5):566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 46.Demyttenaere K, Bruffaerts R, Posada-Villa J et al. WHO World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health surveys. JAMA. 2004;291(21):2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 47.Breslau J, Borges G, Tancredi D et al. Health selection among migrants from Mexico to the US: childhood predictors of adult physical and mental health problems. Public Health Rep. 2011;126(3):361–370. doi: 10.1177/003335491112600310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gilman SE, Breslau J, Conron KJ, Koenen KC, Subramanian SV, Zaslavsky AM. Education and race–ethnicity differences in the lifetime risk of alcohol dependence. J Epidemiol Commun Health. 2008;62(3):224–230. doi: 10.1136/jech.2006.059022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miller JW, Gfroerer JC, Brewer R, Naimi T, Mokdad A, Giles W. Prevalence of adult binge drinking: a comparison of two national surveys. Am J Prev Med. 2004;27(3):197–204. doi: 10.1016/j.amepre.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 50.Groves R, Peytcheva E. The impact of nonresponse rates on nonresponse bias: a meta-analysis. Public Opin Q. 2008;72(2):167–189. [Google Scholar]