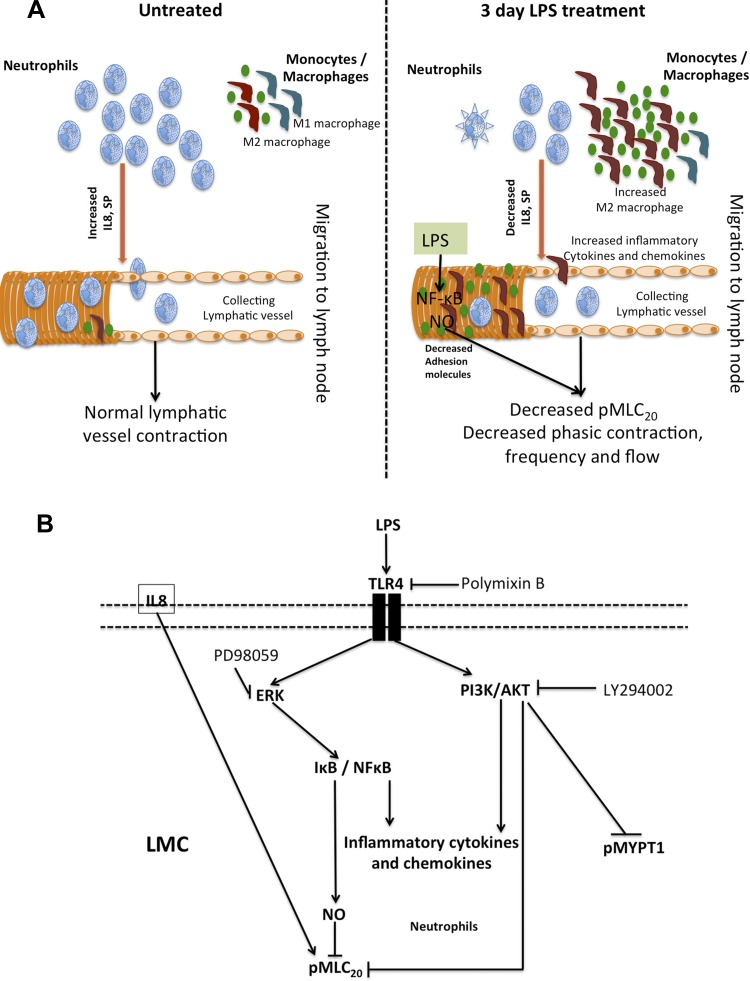
Fig. 8.
A: schematic representation of LPS mediated immune cell modulation and impairment of lymphatic function. Neutrophils and macrophages are present in the lymphatic mesenteric bed in normal physiological conditions. After 3-day LPS challenge, a significant decrease in neutrophils and increase in M2 polarized macrophages is noted in the vicinity of the lymphatics. LPS significantly reduces key neutrophil-associated cell adhesion molecules as CXCR2 and Gal-9 on the LMCs, while activating ICAM1 and VCAM1 that attract monocytes and macrophages. LPS further causes a significant impairment of lymphatic contractility by directly activating NO-mediated inhibitory signaling by activation of NF-κB. The alterations in the immune cell population on/near the mesenteric lymphatics also cause changes in the complex cytokine-mediated signaling that affect lymphatic vessel function. B: schematic representation of LPS-TLR4 pathways in LMCs. In the LMCs, LPS signals through the TLR4 receptor and activates parallel contractile and inflammatory pathways by activation of pAKT and pERK, respectively. Inhibition of ERK inhibits I-κB-mediated induction of inflammatory cytokines, NO and NF-κB activation. On the other hand, induction of pAKT represses pMLC20. IL-8 may also directly activate pMLC20.