Figure 1.
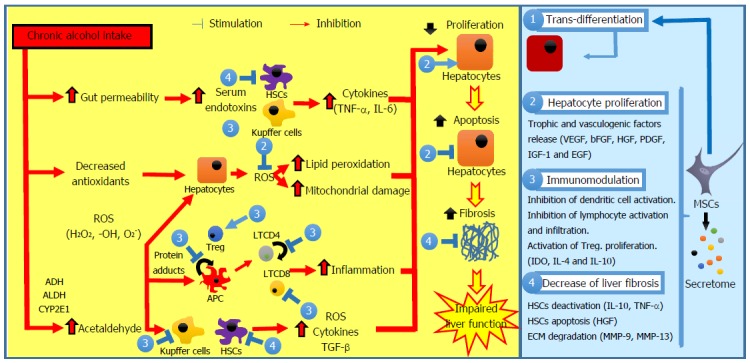
Pathogenesis of alcoholic liver disease and possible interventions of mesenchymal stem cells. Ethanol promotes the translocation of lipopolysaccharides from the gastrointestinal lumen to the portal vein. In Kupffer cells and in HSCs, lipopolysaccharides increase the expression of multiple pro-inflammatory cytokines, reducing liver regeneration. Chronic alcohol exposure reduces the intracellular concentration of antioxidants with subsequent mitochondrial dysfunction, leading to hepatocyte apoptosis. Acetaldehyde is highly toxic to hepatocytes because it binds to proteins forming adducts that promote glutathione depletion, lipid peroxidation, and mitochondrial damage. Additionally, these adducts act as antigens that activate the adaptive immune response, leading to lymphocyte recruitment to the liver. HSCs can be activated by damaged hepatocytes and activated Kupffer cells through various profibrogenic mediators, resulting in ECM accumulation and fibrosis. The interventions of MSCs include: (1) trans-differentiation into parenchymal cells; (2) induction of endogenous regeneration (i.e., stimulation of hepatocyte proliferation, inhibition of hepatocyte apoptosis, and improvement of the impaired endogenous regeneration); (3) modulation of inflammation (i.e., inhibition of APC maturation, proliferation, activation, and/or T-cell priming activity, reduction of lymphocyte proliferation and stimulation of Treg proliferation); and (4) decrease of liver fibrosis (i.e., inhibition of HSC proliferation, stimulation of HSC apoptosis and induction of ECM degradation). APC: Antigen-presenting cell; ECM: Extracellular matrix; HSC: Hepatic stellate cell; MSC: Mesenchymal stem cell; ROS: Reactive oxygen species; TGF-β: Transforming growth factor-β.
