Abstract
Spontaneous spinal epidural hematoma (SSEH) is an acute neurological emergency which carries significant morbidity unless diagnosed and treated in a timely fashion. Some cases of SSEH are idiopathic but there is a well-recognised association with deranged coagulation and abnormalities of clotting. In recent years there has been increasing availability of novel anti-platelet agents, often prescribed in the setting of suspected acute coronary syndromes (ACS) and following percutaneous coronary interventions and these agents also present an increased risk of SSEH. We present a case of SSEH following an acute presentation with chest pain and treatment with dual anti-platelet therapy.
Keywords: Spinal haematoma, magnetic resonance imaging (MRI), neurosurgery
Introduction
Spontaneous spinal epidural hematoma (SSEH) is an acute neurological emergency first described in the medical literature in 1869 (1-4). It is a rare condition (incidence 0.1 patients/100,000) but one which carries significant morbidity unless diagnosed and treated in a timely fashion. While some cases of SSEH are idiopathic there is a strong association with deranged coagulation and abnormalities of clotting including patients taking coumadin anti-coagulations such as warfarin (1-4). In recent years there has been increasing availability of novel anti-platelet agents, often prescribed in the setting of suspected acute coronary syndromes (ACS) and following percutaneous coronary interventions and these agents also present an increased risk of SSEH. We present a case of a patient developing SSEH following acute presentation to hospital with chest pain and treated with dual anti-platelets for suspected ACS.
Case report
A 73-year-old woman presented to the emergency assessment unit with central chest pain radiating to the back and down both arms. Symptoms were relieved with glycerol trinitrate spray and oral aspirin 300 mg. There was no significant past medical history of note apart from a strong family history of stroke. On arrival at hospital she complained of spontaneously resolving transient upper limb weakness and paraesthesia. The cardiovascular physical examination was normal as were serial 12-lead electrocardiograms. Serial troponin measurements were slightly elevated at 139 and 101 ng/L (ref: <32 ng/L). Routine blood tests including a full blood count, electrolytes and renal function were within normal limits. Initial neurological examination demonstrated normal power, deep tendon reflexes, fine touch sensation and intact bladder tone. She was treated with a loading dose of clopidogrel 300 mg and enoxaparin 1 mg/kg body weight in view of central chest pains, minor troponin rise and resolution of symptoms with GTN spray.
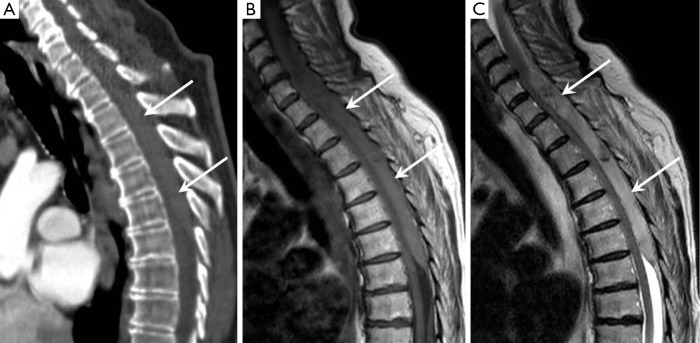
Within 12 hours of admission she developed worsening chest pains radiating to the back along with paraplegia and loss of sensation in both limbs. There was no evidence of blood pressure variation in the upper limbs. An urgent contrast enhanced thoracic computed tomography (CT) scan excluded acute aortic syndrome and central pulmonary embolism but high density material was noted within the spinal epidural space extending between C5 and T6 vertebral levels (Figure 1A). Urgent spinal magnetic resonance imaging (MRI) confirmed the presence of a large acute epidural haematoma compressing the spinal cord and prompted transfer to the local neurosurgical team (Figure 1B,C). The patient underwent spinal laminectomy and clot evacuation. She made an uneventful post-operative recovery and quickly regained full power in her extremities. She was discharged on day 5 and remains well on follow up.
Figure 1.
(A) Sagittal CT reconstruction showing a posteriorly sited elliptical 15 cm high attenuation collection compressing the spinal cord in keeping with a large epidural haematoma (arrows); (B) and (C) sagittal T1 and sagittal T2 weighted MRI images showing the collection to be of intermediate T1 and high T2 signal intensity in keeping with a subacute haematoma. CT, computed tomography; MRI, magnetic resonance imaging.
Discussion
Anticoagulation (e.g., warfarin) or antiplatelet (e.g., aspirin) therapy are the most frequently reported risk factors for SSEH reported in the medical literature, but the aetiology remains unclear in around 50% to 75% of cases (5). SSEH is more likely to be suspected in patients presenting with sudden onset back pain followed by neurological deficit if the patient is known to be taking anticoagulants or antiplatelet agents.
In the presented case, neck and back pain were initially thought to be atypical symptoms of ACS because of the association with central chest pain and elevated cardiac enzymes. The administration of anti-platelet agents may have unmasked the neurological symptoms of SSEH secondary to rapid progression of epidural bleeding.
SSEH as a mimic of ACS and with a good post-operative recovery despite initial treatment with dual anti-platelet agents has not been previously described. Prior reports of SSEH have been published in the context of myocardial infarction related thrombolysis.
There is ongoing debate in the literature regarding operative decompression/clot evacuation versus conservative/medical management of SSEH with conflicting results in several studies (6). Encouraging results were noted with conservative treatment following factor Xa inhibitor (rivaroxaban) therapy (7). On the contrary the largest published case series of SSEH patients showed a clear benefit of early surgical intervention (8). Post operative recovery in SSEH is thought to be closely related to the severity of the pre-operative neurological deficit as well as the time interval between symptom onset and surgical decompression (8).
The astute physician should be aware of the potential for SSEH in patients presenting with back pain and risk factors for bleeding but also in patients with ACS as highlighted in this report. CT scanning has a high sensitivity for detecting acute blood products within the spinal canal but has limited capability to accurately assess the degree of spinal cord compression which is best achieved with MRI.
Conclusions
The presented case highlights the importance of thorough history taking and physical examination when assessing any patient presenting with chest pain. In the current era of novel anti-platelet (ticagrelor, prasugrel) and anti-coagulant (rivorxaban, apixiban, dabigatran) therapies with no defined antidotes, physicians should be alerted to SSEH as a rare but serious complication in order to expedite patient management and improve the chances of a good functional recovery.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Morales Ciancio RA, Drain O, Rillardon L, Guigui P. Acute spontaneous spinal epidural hematoma: an important differential diagnosis in patients under clopidogrel therapy. Spine J 2008;8:544-7. [DOI] [PubMed] [Google Scholar]
- 2.Moon HJ, Kim JH, Kim JH, Kwon TH, Chung HS, Park YK. Spontaneous spinal epidural hematoma: an urgent complication of adding clopidogrel to aspirin therapy. J Neurol Sci 2009;285:254-6. [DOI] [PubMed] [Google Scholar]
- 3.Kirazli Y, Akkoc Y, Kanyilmaz S. Spinal epidural hematoma associated with oral anticoagulation therapy. Am J Phys Med Rehabil 2004;83:220-3. [DOI] [PubMed] [Google Scholar]
- 4.Alexiadou-Rudolf C, Ernestus RI, Nanassis K, Lanfermann H, Klug N. Acute nontraumatic spinal epidural hematomas. An important differential diagnosis in spinal emergencies. Spine (Phila Pa 1976) 1998;23:1810-3. [DOI] [PubMed] [Google Scholar]
- 5.Kreppel D, Antoniadis G, Seeling W. Spinal hematoma: a literature survey with meta-analysis of 613 patients. Neurosurg Rev 2003;26:1-49. [DOI] [PubMed] [Google Scholar]
- 6.Yang SM, Kang SH, Kim KT, Park SW, Lee WS. Spontaneous spinal epidural hematomas associated with acute myocardial infarction treatment. Korean Circ J 2011;41:759-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaeger M, Jeanneret B, Schaeren S. Spontaneous spinal epidural haematoma during Factor Xa inhibitor treatment (Rivaroxaban). Eur Spine J 2012;21:S433-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim T, Lee CH, Hyun SJ, Yoon SH, Kim KJ, Kim HJ. Clinical Outcomes of Spontaneous Spinal Epidural Hematoma: A Comparative Study between Conservative and Surgical Treatment. J Korean Neurosurg Soc 2012;52:523-7. [DOI] [PMC free article] [PubMed] [Google Scholar]