Abstract
Objectives
Progress has been made in recent years in the provision of amplification and early intervention for children who are hard of hearing. However, children who use hearing aids (HA) may have inconsistent access to their auditory environment due to limitations in speech audibility through their HAs or limited HA use. The effects of variability in children’s auditory experience on parent-report auditory skills questionnaires and on speech recognition in quiet and in noise were examined for a large group of children who were followed as part of the Outcomes of Children with Hearing Loss study.
Design
Parent ratings on auditory development questionnaires and children’s speech recognition were assessed for 306 children who are hard of hearing. Children ranged in age from 12 months to 9 years of age. Three questionnaires involving parent ratings of auditory skill development and behavior were used, including the LittlEARS Auditory Questionnaire, Parents Evaluation of Oral/Aural Performance in Children Rating Scale, and an adaptation of the Speech, Spatial and Qualities of Hearing scale. Speech recognition in quiet was assessed using the Open and Closed set task, Early Speech Perception Test, Lexical Neighborhood Test, and Phonetically-balanced Kindergarten word lists. Speech recognition in noise was assessed using the Computer-Assisted Speech Perception Assessment. Children who are hard of hearing were compared to peers with normal hearing matched for age, maternal educational level and nonverbal intelligence. The effects of aided audibility, HA use and language ability on parent responses to auditory development questionnaires and on children’s speech recognition were also examined.
Results
Children who are hard of hearing had poorer performance than peers with normal hearing on parent ratings of auditory skills and had poorer speech recognition. Significant individual variability among children who are hard of hearing was observed. Children with greater aided audibility through their HAs, more hours of HA use and better language abilities generally had higher parent ratings of auditory skills and better speech recognition abilities in quiet and in noise than peers with less audibility, more limited HA use or poorer language abilities. In addition to the auditory and language factors that were predictive for speech recognition in quiet, phonological working memory was also a positive predictor for word recognition abilities in noise.
Conclusions
Children who are hard of hearing continue to experience delays in auditory skill development and speech recognition abilities compared to peers with normal hearing. However, significant improvements in these domains have occurred in comparison to similar data reported prior to the adoption of universal newborn hearing screening and early intervention programs for children who are hard of hearing. Increasing the audibility of speech has a direct positive effect on auditory skill development and speech recognition abilities, and may also enhance these skills by improving language abilities in children who are hard of hearing. Greater number of hours of HA use also had a significant positive impact on parent ratings of auditory skills and children’s speech recognition.
INTRODUCTION
In recent years, substantial progress has been made in lowering the age of confirmation of hearing loss from around 2 years of age (Harrison & Roush 1996; Moeller 2000) to around 7 months of age (Holte et al. 2012). Even with this progress, childhood hearing loss fundamentally alters auditory experience and opportunities for development. The cumulative auditory experience of children who are hard of hearing (CHH) during early childhood is varied and can be influenced by the audibility of speech through amplification (McCreery, Bentler & Roush 2013; McCreery et al. this issue, pp. XXXX) and the extent and consistency of hearing aid (HA) use (Walker et al. 2013; Walker et al. this issue, pp. XXXX). In addition to monitoring communication development, parent-reported development of auditory skills and tests of speech recognition are often recommended to document and monitor progress in CHH clinically (Bagatto et al. 2010). The broad effects of early amplification on parent ratings of auditory skills and on speech recognition outcomes in CHH have been reported (Blamey et al. 2001; Davidson & Skinner, 2006; Sininger et al. 2010; Ching et al. 2013a). However, the effects of individual variability in aided audibility and HA use on these outcomes have been considered only in a few recent studies (Bagatto et al. 2011; Stiles et al. 2012; Koehlinger, Van Horne & Moeller 2013; Ambrose et al. 2014; Tomblin et al. 2014). In this manuscript, the influence of speech audibility and amount of HA use on parent ratings of auditory development and on children’s speech recognition was analyzed for a large group of infants and young CHH who were followed as part of the longitudinal Outcomes of Children with Hearing Loss (OCHL) study.
The effects of congenital hearing loss on the development of speech and language in CHH has been well-documented (see Moeller and Tomblin, this issue pp. XXXX, for a review). Documenting auditory skill development and speech recognition in CHH are also crucial for assessing the effectiveness of early intervention strategies, including amplification. Yet, few standardized questionnaires assessing early auditory skill development in infants and young children were available or reported in the literature prior to the adoption of universal newborn hearing screening because many CHH were not usually identified until after two years of age (e.g., Moeller 2000). The limited data on auditory development questionnaires focused primarily on children with cochlear implants (e.g., Osberger, Zimmerman-Phillips, & Koch, 2002) or pre-implant development in children with profound hearing losses (e.g., Waltzman & Roland, 2005). More recently, new auditory development questionnaires based on parent-report have been developed (Ching & Hill, 2006; Tsiakpini et al. 2004). These measures query emergent language abilities and auditory behavior during infancy and early childhood. Data are now available from CHH on these measures (Bagatto et al. 2010; Ching et al. 2013a; Bagatto & Scollie, 2013), but the auditory and linguistic factors that predict individual variability among CHH on these questionnaires has not been widely reported.
Additionally, speech recognition in children who are deaf and hard of hearing was generally delayed and highly variable across children in past research (Geers & Moog 1992; Boothroyd & Eran 1994; Kirk, Pisoni & Osberger 1995; Blamey et al. 2001; Davidson & Skinner 2006). Among children who were born prior to the era of universal newborn hearing screening, a wide range of factors were found to influence speech recognition abilities in children with HAs or cochlear implants, including degree of hearing loss and language and cognitive abilities. Greater degrees of hearing loss were generally associated with poorer outcomes. For example, Blamey et al. (2001) reported language and speech recognition outcomes for two groups of children who were deaf or hard of hearing, one group with HAs and one with cochlear implants. Children with better language abilities, better thresholds, and earlier age of implantation or amplification had better speech recognition in both auditory and auditory/visual tasks for children with HAs and those with cochlear implants. Similarly, Davidson et al. (2011) indicated that school-age children and adolescents with cochlear implants who had higher language abilities also had better speech recognition scores. Cleary, Pisoni and Geers (2001) also suggested that children with cochlear implants with better working memory abilities were likely to have better speech recognition than peers with more limited working memory abilities. The influence of auditory, linguistic and cognitive factors on speech recognition has not been widely reported for a large group of CHH. Many children who were reported in the previous literature were identified at later ages than are observed in the current era of universal newborn hearing screening. CHH who have been identified through newborn hearing screening are likely to have earlier ages of identification, earlier ages of amplification, and earlier access to intervention services (Holte et al. 2012, Walker et al. 2014). These advantages may lead to better speech recognition outcomes than have been observed previously, as CHH have increased auditory-linguistic experience.
For children who have received cochlear implants, the positive effects of earlier identification and intervention have been documented for language outcomes (Niparko et al. 2010; Tobey et al. 2013), speech perception (Geers, Brenner & Davidson 2003; Wang et al. 2008) and health-related quality of life (Meserole et al. 2013). However, CHH who wear HAs have not been as widely studied as children who have received cochlear implants. Children who wear HAs face challenges that increase the variability in auditory experience they receive from amplification. For example, HAs are increasingly being fit during infancy, which is a period of rapid ear canal growth (Keefe et al. 1993). Increases in the length and volume of the ear canal reduce the effective output of the HA over time, potentially leading to reduced audibility for speech (Bagatto et al. 2002; Bingham, Jenstad & Shanaz, 2009). Variation in the amount of audibility provided through amplification has also been documented among CHH, related either to changes in hearing or to amplification that does not sufficiently improve audibility (Strauss & van Dijk 2008; McCreery, Bentler & Roush 2013; McCreery et al. this issue, pp. XXXX). Frequent hearing evaluation, electroacoustic verification and adjustment of the HAs are necessary to maintain the audibility of speech as the child grows. Differences between children in the amount or consistency of HA use also influences variability in auditory experience. The amount of HA use varies widely across infants and children (Moeller et al. 2009; Walker et al. 2013; Walker et al. this issue, pp. XXXX). The amount of speech audibility and the consistency of HA use are both likely to moderate the amount of benefit a child receives from amplification. Despite the potential for variability in speech audibility and HA use among CHH, few studies have considered whether these factors affect parent ratings of auditory skills and speech recognition.
Bagatto and colleagues (2011) summarized results from parent ratings on auditory development questionnaires for a group of 129 infants and young children with HAs between 1 month and 8 years of age. Outcomes reported included aided audibility and responses from two parental questionnaires of auditory development, the LittlEARS Auditory Questionnaire (Tsiakpini et al. 2004) and Parents’ Evaluation of Aural/Oral Performance of Children (PEACH; Ching & Hill 2007). Nearly all of the children in the study were reported to have acceptable aided speech audibility for their degree of hearing loss. CHH were classified as being otherwise typically-developing, having additional developmental comorbidities (mild or severe), or having complex factors. Children with complex factors had limited HA use and/or late-identification of hearing loss. As expected, parents of children with severe developmental comorbidities reported more substantial delays in auditory development compared to parents of children with hearing loss who were otherwise typically-developing. Children who had complex factors that limited the consistency of auditory experience from amplification had developmental trajectories for the LittlEARS questionnaire that were lower on average than children with mild developmental comorbidities and the typically-developing group. These differences were not observed between groups on the PEACH questionnaire, which characterizes auditory skills in older children. Differences among CHH in auditory experience due to either age of identification or consistency of HA use appeared to influence parents’ ratings of early auditory development; however, the amount of delay in identification and the amount of HA use that were used to classify children into the complex factors group was not specified. Additionally, grouping HA use and age of identification together did not allow for the independent quantification of these factors on early auditory development.
In another recent study, Sininger and colleagues (2010) reported on developmental outcomes for a group of 44 infants and children who used a cochlear implant or HAs at three years of age. Results included two different measures of speech perception with amplification. Substantial variability in speech-recognition measures was observed among children who wore HAs. The amount and consistency of HA use across subjects was not reported. Like Bagatto et al. (2011), the aided audibility for children in the study was consistently high across subjects. Because of the limited variability in aided audibility and high colinearity between aided audibility and pure tone average, the relationship between aided audibility and aided speech recognition could not be analyzed. Results from Sininger et al. suggest that for a group of children with good aided audibility, significant variability in auditory development outcomes is still likely to be observed. However, not all children who wear HAs have amplification that is optimized to provide consistent audibility for their degree of hearing loss (Strauss & van Dijk 2008; McCreery, Bentler & Roush 2013). Therefore, clinical populations of children who use HAs may have an even wider range of auditory experience and related outcomes than the subjects in Sininger et al.
Another investigation of outcomes in a large group of 451 three year-old children who wore either HAs or cochlear implants was reported by Ching and colleagues (see Ching et al. 2013a and Ching et al. 2013b for summaries). The major predictors of language outcomes at three years of age were maternal education level (higher maternal education associated with better outcomes), severity of hearing loss (greater degree of hearing loss associated with poorer outcomes), additional disabilities (children with additional developmental comorbidities had poorer outcomes than those with hearing loss alone), and gender (females with better outcomes than males). As in most previous studies of development in children who are deaf and hard of hearing, substantial variability in outcomes was reported. Neither the influence of aided audibility nor consistency of HA use was analyzed as a predictor of outcomes, so it remains unresolved whether or not these variables would have contributed to outcomes observed by Ching and colleagues.
Differences in auditory experience among CHH due to variability in the amount of aided audibility (McCreery et al. this issue, pp. XXXX) and the consistency of their HA use over time (Walker et al. this issue, pp. XXXX) are likely to affect speech recognition and parent ratings of auditory skills. Few studies have examined whether these factors might explain variability in these outcomes in CHH, particularly when accounting for other influential factors such as socioeconomic status and language abilities. One recent study by Stiles and colleagues (2012) described the influence of aided audibility and vocabulary on word recognition and nonword repetition in quiet for a group of 16 children between 6–9 years of age who wore HAs. For both word recognition and nonword repetition tasks, children with higher aided audibility had higher outcomes. Receptive language ability was not a significant predictor after controlling for audibility and age. Most of the CHH in the study had high audibility and word recognition scores in quiet. The influence of auditory, linguistic and cognitive factors on speech recognition in noise or for a larger group of children with a wider range of audibility could help to further describe the role of audibility and HA use on speech recognition and auditory development questionnaires. An earlier investigation of the OCHL cohort suggested that higher aided audibility positively affected speech and language outcomes at three years of age (Tomblin et al. 2014), but the effects on speech recognition and parent ratings of auditory skills have not been explored in this group. The purpose of the current investigation was to describe speech recognition and parent ratings of auditory skills in a large group of CHH measured at multiple time points during early childhood. Three research questions were posed:
How do aided audibility and HA use influence parent ratings of auditory skills and speech perception in CHH at different time points during early childhood? We predict that children with higher aided audibility and more hours of HA use would have higher parent ratings of auditory development on questionnaires and better speech recognition at each time point during the study.
How do concurrent linguistic, cognitive and demographic factors affect parent-reported auditory skill development and speech recognition of CHH during early childhood? We predict that CHH with stronger language and phonological working memory abilities and who come from families with higher socioeconomic status will have higher parent ratings on auditory development questionnaires and better speech recognition than children with lower abilities or socioeconomic status.
How do aided audibility and HA use influence speech perception in a subgroup of CHH over time? We predicted that children with higher aided audibility and more hours of HA use at three years of age would have better speech recognition in quiet at five years of age than peers with more limited audibility and HA use.
These findings could improve our understanding of the relationship between audiological factors, like degree of hearing loss, aided audibility and HA use, and outcomes, like speech recognition and parent ratings of auditory skill development.
MATERIALS AND METHODS
Participants
All of the children and parents who participated in the study were recruited as part of the OCHL study. Amplification, speech recognition and parent ratings of auditory development were obtained from 306 CHH. For comparison purposes, data were obtained from 185 children with normal hearing (CNH). The better-ear pure tone average (PTA; 500, 1000 and 2000 Hz) for the group of CHH ranged from 20 to 92.5 dB HL during the study (Mean = 48.5 dB, SD =14.4 dB). Two hundred ninety-two children were fitted with air conduction HAs and seven children used a bone conduction HA. Seven children with mild hearing loss did not wear HAs. Ten children received cochlear implants after study enrollment. Only pre-implantation data for the group of children who received cochlear implants are included in the current analysis.
The study utilized an accelerated longitudinal design (Duncan, Duncan & Hops, 1996 or see Tomblin et al. this issue pp. XXXX for a detailed description). Unlike a single-cohort longitudinal study design, the accelerated longitudinal design enrolls children at different ages, which provides the opportunity to enroll a larger number of subjects and study a broader age range of development. Children and their families participated in an initial baseline visit, followed by visits twice a year for children under age two and once a year for children two years and older. Study participation continued for up to four years, or until nine years of age, whichever came first. Study visits occurred in close proximity to the child’s birthday or two specific age milestones (6 months and 18 months). All audiometric test data collection occurred in a sound-treated audiometric test booth, audiology clinic office or mobile testing van.
HA measures
The aided audibility of speech through the HA was assessed with probe microphone measures at each visit. Individually-measured real-ear-to-coupler difference (RECD) values were used whenever possible. If the child would not cooperate with individually-measured RECD, age-related average RECD values were used to simulate in situ measurements of HA output in the 2 cm3 coupler of the Audioscan Verifit HA analyzer. In situ measurements of HA output with the HA on the ear were completed with some cooperative older children. Verification was completed for soft (50 or 55 dB SPL) and average (60 or 65 dB SPL, 10 dB higher than the level for soft) input levels using the standard speech stimulus (“carrot passage”) to represent the long-term average speech spectrum. Results were compared to Desired Sensation Level Targets (DSL; Scollie et al. 2005). Maximum power output (MPO) was verified using swept pure tone stimuli. Verification was completed for 203 children with conventional processing. For children with nonlinear frequency compression (NFC) activated in their HAs at one or more visits (n = 79), filtered speech bands were used as verification stimuli to estimate the sensation level and frequency location of those bands after lowering. In addition to verification of speech audibility, ANSI (ANSI S3.22-2003) conformity measures of HA function were completed to document that the HAs were functioning within manufacturer specifications.
Aided audibility calculation
To estimate the aided audibility of speech, a modification of the Speech Intelligibility Index (SII; ANSI S3.5 – 1997, R2007; Bentler et al. 2014) that permits calculation of audibility with conventional amplification or amplification with nonlinear frequency compression (NFC) was applied to verification data obtained for soft and average input levels for speech. The amplified long-term average speech spectrum was measured for each listener, ear and input level (soft and average speech). The calculation was based on the 1/3-octave-band method using the average band-importance weighting function from Table 3 of the standard (ANSI S3.5-1997, R2007). The intensity levels of speech were converted to free-field using the free-field to eardrum transfer function from the SII. Audiometric thresholds were converted from dB HL to dB SPL and then interpolated and extrapolated to correspond with 1/3-octave-band frequencies. A frequency-specific bandwidth adjustment was used to convert pure tone thresholds to equivalent 1/3-octave-band levels (Pavlovic, 1987). The spectrum levels of speech and threshold-equivalent noise for each child’s audiogram were entered into a spreadsheet to estimate the sensation level (SL) for each 1/3-octave band. The SL for each band was multiplied by the importance weight for that band, and the sum of these products for all bands was the SII for each condition.
For children with NFC signal processing activated in their HAs, the aided SII calculation was modified to account for the compression of outputs above the lowest frequency where NFC was applied, known as the start frequency. The 1/3-octave bands above the start frequency for NFC were shifted to lower frequencies in the output. For children with NFC, the SII calculation was the same as for children with conventional processing, except that the SL for each frequency band above the start frequency was calculated at the frequency where the filtered band was measured during the verification process with NFC activated. The outputs of the filtered speech bands above the start frequency were entered into an SII calculator to estimate the amount of information that was audible with lowering. This approach assumes that speech information carries the same importance after frequency lowering but does not account for the potential reduction in spectral distinctiveness that could occur with NFC.
HA use
Daily HA use was determined by parent responses to a HA use questionnaire (Moeller et al. 2009; Walker et al. 2013; Available at ochlstudy.com) completed at each visit. The questionnaire included an estimate of the average hours of HA use per day and the amount of HA use in different listening situations. A subset of the children in the study also had data logging in their HAs, but parent report was used in the following analyses because the correlation between data logging and parent report was high (r = .71) and parent report was available for a larger proportion of children in the study (Walker et al. 2013; Walker et al. this issue, pp.xxxx). Based on parent report, the overall mean for HA use was 10.8 hours per day.
Auditory development outcomes
The test battery for auditory development outcomes depended on the age of the child at each visit. Table 1 displays the number of measures that were completed at each visit by age.
Table 1.
Number of CHH for auditory development outcomes by visit
| 12 mo | 18 mo | 2 yr | 3 yr | 4 yr | 5 yr | 6 yr | 7 yr | 8 yr | 9 yr | |
|---|---|---|---|---|---|---|---|---|---|---|
| Total CHH | 58 | 79 | 119 | 145 | 157 | 143 | 142 | 105 | 45 | 27 |
| Questionnaires | ||||||||||
| LittlEARS | 52 | 72 | 77 | |||||||
| PEACH | 15 | 37 | 85 | |||||||
| SSQ | 140 | 125 | 39 | |||||||
| Word recognition measures | ||||||||||
| O&C | 105 | |||||||||
| ESP | 72 | 106 | ||||||||
| LNT - Easy | 126 | 42 | ||||||||
| LNT - Hard | 121 | 43 | ||||||||
| PBK | 42 | 141 | 125 | 74 | 40 | |||||
| CASPA | 67 | 38 | 24 | |||||||
mo = months; yr = years
CHH = Children who are hard of hearing
O&C = Open and closed set test
PEACH = Parent’s Evaluation of Aural/Oral Performance of Children
SSQ = Speech Spatial and Qualities of Hearing Questionnaire
ESP = Early Speech Perception Test; LNT = Lexical Neighborhood Test
PBK = Phonetically-Balanced Kindergarten Word Lists
CASPA = Computer-Assisted Speech Perception Assessment
Auditory development questionnaires
LittlEARS Auditory Questionnaire (Tsiakpini et al. 2004)
The LittlEARS Auditory Questionnaire was developed as a measure of early auditory development and verbal skills for children who had received cochlear implants (Coninx et al. 2009). The measure has subsequently been validated for use with CHH who wear HAs (Bagatto et al. 2011). The LittlEARS consists of 35 questions that evaluate the child’s auditory development and selected expressive and receptive language skills. Parents indicate whether (1) or not (0) their child exhibits the behavior described in each question. The LittlEARS was completed by the parents of children at 12 months, 18 months and 2 year visits. Children who received a score of 28 or higher on the LittlEARS did not receive the LittlEARS at the next study visit, as a score of 28 on the LittlEARS is a criterion score that indicates children have reached the maximum level of performance on the test.
Parents’ Evaluation of Aural/Oral Performance of Children Rating Scale (Ching & Hill 2007)
The Parents’ Evaluation of Aural/Oral Performance of Children (PEACH) Rating Scale is a questionnaire that assesses children’s listening performance in a wide range of communicative situations, including specific questions about listening in quiet and in background noise. The PEACH rating scale was developed as an abbreviated version of the PEACH Diary (Ching & Hill 2005) and has been validated in previous studies for CNH and CHH (Ching & Hill 2007; Ching et al. 2010; Bagatto & Scollie, 2013). The PEACH requires parents to rate their child’s performance in different listening situations on a scale with categories from “Never” to “Always or more than 75% of the time.” The PEACH rating scale includes 13 questions, including one question about HA use, one question about tolerance for loud sounds, six questions about quiet listening situations, and five questions about listening situations with background noise. The response categories on the PEACH are based on a 0–4 scale where in most cases 0 corresponds with a rating of “Never” and 4 corresponds with a rating of “Always”, except for Question 2 (“How often has your child complained or been upset by loud sounds?”) where the scale is reversed. A percentage score for the PEACH Quiet and Noise subscales are calculated by adding the numerical values for the response to each question and dividing by the total number of potential points for each subscale or the Total PEACH score. Once children reached a criterion score of 28 on the LittlEARS, their parent completed the PEACH at that same visit and subsequent visits up to at least the 2 year-old visit.
Speech, Spatial & Qualities of Hearing Scale (Gatehouse & Noble 2004)
The Speech, Spatial and Qualities of Hearing Scale (SSQ) was developed to assess listening difficulties across a wide range of situations with adults who are hard of hearing. The scale has been adapted for use in children who use cochlear implants (Galvin et al. 2007). The version of the SSQ used in this study included the subscales of Speech, Spatial and Qualities, but also was adapted by the OCHL team to include questions for a fourth dimension relating to conversational uses of hearing. Each subscale consisted of multiple items that query specific listening behaviors and asks parents to rate their child’s abilities on a scale of 0 (minimal ability) to 10 (maximal ability). The Speech subscale includes eight questions about the child’s ability to follow conversations in different listening situations. The Spatial subscale includes five questions about the child’s ability to locate talkers in listening situations with background noise. The Qualities of Hearing subscale consists of eight questions about awareness and identification of environmental sounds, including music, as well as the child’s ability to selectively attend to specific talkers in noise. The Conversational Uses of Hearing subscale included six questions: two questions regarding listening in the car, one question about recognition of words or songs overheard from media (i.e. TV, radio), one question about overhearing and two questions about recognition of novel sounds in the child’s listening environment. Parents rated their children’s listening abilities across four subscales. The SSQ was administered to the parents of CHH at 4-, 6- and 8-year-old study visits.
Speech perception measures
Open and Closed-Set Test (Ertmer, Miller, & Queensberry 2004)
The Open and Closed-Set Test (O&C) is a measure that assesses the child’s speech production and word recognition abilities. The O&C test includes an open-set task where the child must imitate a parent or examiner’s production of a target word, followed by a closed-set task where the child must point to a picture of the target word from a set of three pictures. The O&C test yields three scores: phonemes correctly produced, words correctly produced and words correctly identified during the point-to-picture task. The stimuli are words within the lexicon of 75% of two-year-old children. The O&C was administered using live-voice presentation as an audio-visual task during the two-year-old study visit. Children wore their HAs during the task. The outcomes for the O&C Test test for two-year-olds in the Outcomes of Children with Hearing Loss study have been reported in a previously published report on speech production abilities (Ambrose et al. 2014). In the current analyses, the word identification data from the O&C test are reported as an early measure of word recognition and used as a predictor for later monosyllabic word recognition abilities, which was not included in the analyses reported by Ambrose and colleagues. The scores are presented as a percent of words correctly identified in the closed-set, point-to-picture task.
Early Speech Perception test (Moog & Geers 1990)
The Early Speech Perception (ESP) test is a closed-set speech recognition task that requires the child to point to a target syllable or word from a set of toys or pictures and includes subtests of syllable pattern perception, spondee words, and monosyllabic words. The test was administered as a live-voice, auditory-only task with the examiner’s mouth covered by an acoustic hoop and the child wearing their HAs. The ESP test has both low-verbal and standard versions. The low-verbal version, using a closed-set of four toys for 12 trials, was administered to children at the two-year-old visit, while the standard version, a closed-set of 12 picture items for 24 trials, was administered at the three-year-old visit. The pattern perception subtest was administered to children who could not complete the spondee test. The scores are reported for each subtest as a percent of targets correct in each condition..
The Lexical Neighborhood Test (Kirk, Pisoni, & Osberger 1995)
The Lexical Neighborhood Test (LNT) is an open-set monosyllabic word recognition task that was completed using recorded stimuli in an auditory-only task with the children wearing their HAs. The task was completed without competing noise at a presentation level of 65 dBA at 0 degrees azimuth from a loudspeaker. The LNT includes monosyllabic words that are both easy (words with high lexical frequency and low lexical neighborhood density) and hard (words with low lexical frequency and high lexical neighborhood density). The scores are reported as the percent of targets correct for easy and hard words (25 words for each list). The LNT was administered as part of the four-year-old and five-year-old visits.
The Phonetically Balanced Kindergarten Word Lists (Haskins 1949)
The Phonetically Balanced Kindergarten (PBK) Word Lists were used to assess monosyllabic word recognition in quiet with the child’s HAs starting at the four-year-old visit and each annual study visit thereafter. The child was asked to listen to a recorded list of 50 words presented at 65 dBA at 0-degree azimuth from a loudspeaker. The scores are the percent correct of 50 words. The PBK was administered as part of the four- through eight-year old visits.
The Computer-Assisted Speech Perception Assessment (Boothroyd, 1999)
The Computer-Assisted Speech Perception Assessment (CASPA) was completed as a measure of monosyllabic word recognition with competing steady-state noise. CASPA consists of 30 lists that include 10 monosyllabic words. Each list is balanced for phonemic content and can be scored as either words or phonemes correct. The CASPA was presented via loudspeaker at 50, 65, and 75 dBA at 0-degree azimuth at three signal-to-noise ratios (−5, +10 and +20 dB) by varying the level of the talker, and presenting the steady-state speech-spectrum noise at a constant 55 dBA. The scores are the percent correct of 10 words or 30 phonemes in each condition. The CASPA was administered to the children with and without their HAs on, as part of the seven-through nine-year-old visits.
Language and phonological working memory measures
English receptive language abilities were measured using two measures depending on the age of the child. For children at 12 months, 18 months, 3 years and 4 years, spoken language abilities were represented using the Receptive Language subscale scores from the Vineland Adaptive Behavior Scales (Sparrow, Balla & Cicchetti 1984). The Vineland is a parent-report measure that was found to relate to other measures of language in this cohort (Tomblin et al. this issue, pp. XXXX). The Peabody Picture Vocabulary Test IV (Dunn & Dunn, 2012) was used to represent receptive language for the 5 and 7 year-old children. Phonological working memory was measured at the 5, 7 and 9 year visits using the Nonword Repetition subtest of the Comprehensive Test of Phonological Processing (Torgesen, Wagner, & Rashotte, 1999). The Nonword Repetition subtest requires the child to repeat nonsense words of increasing length.
Statistical analyses
Statistical analyses were completed either using SAS v9.3 or the R software interface (Version 3.0.2; R Core Team, 2014). Descriptive statistics for each outcome measure were calculated to demonstrate range of abilities for each of the auditory development questionnaires and speech perception measures. All predictor variables were mean-centered to minimize the potential for multicollinearity. Regression assumptions, including normality, were assessed through residual analysis and there was no evidence of violation of the modeling assumptions. Variance inflation factors for all linear regression analyses were less than 5. Two different analysis approaches were used to address the research questions. The first research question was addressed using cross-sectional data with linear regression to evaluate the multivariate relationship between concurrent predictors and speech recognition and parent ratings of auditory development from questionnaires. For the cross-sectional analyses, each predictor variable was based on concurrent measures collected at the same visit as the outcome. Maternal educational level was used as a proxy variable for socioeconomic status (Bradley & Corwin 2002) and was parameterized into four categories: high school education or less, some college education, college graduate or graduate education. Maternal education level was selected because this measure was more consistently reported than paternal education level and annual family income. Based on previous research that suggests that speech recognition may be influenced by a child’s spoken language abilities (e.g. Blamey et al. 2001; Davidson et al. 2011) and working memory (Stiles et al. 2012), English spoken language ability and phonological working memory were used as predictors of speech recognition at ages where those measures were also collected. The better-ear three-frequency pure tone average (PTA) was used to represent degree of hearing loss. The aided SII for average speech was used to represent audibility of speech with amplification. HA use was based on a weighted-average of parent report to account for weekday and weekend use. Word recognition measures were also included as predictors of auditory development questionnaires to examine the correspondence between speech recognition and auditory development questionnaires. Age was included as a predictor in analyses where data from children in different age groups were included in the same analysis. For the SSQ questionnaire and CASPA speech recognition data in noise, repeated measures over time were present for the same subject. For CASPA, each participant was measured in both aided and unaided conditions as well as in three signal to noise ratio (SNR) settings. Due to the repeated measures, a linear mixed model was constructed which included the same predictor variables as the regression models but also included a random intercept for each subject to account for within subject correlation.
The second research question pertained to the effects of predictors at age 3 on speech recognition in quiet at age 5 on a subset of 49 CHH who had data at both 3-year and 5-year visits. Due to the accelerated longitudinal design of the study, there were a sufficient number of subjects in this age range to perform this analysis. A linear regression model was used. The predictor variables of better-ear PTA, better-ear aided SII, Vineland Receptive Language Subtest and HA use were represented by the data collected at the child’s 3 year-old visit. The outcome was the average word recognition score in quiet for PBK, LNT-Easy and/or LNT-Hard from the 5 year-old visit.
RESULTS
Auditory development questionnaires
The descriptive results from the LittlEARS Auditory Questionnaire, PEACH and SSQ Questionnaires are displayed in Table2.
Table 2.
Descriptive statistics for parent ratings on auditory development questionnaires
| Outcome | Mean | Standard Deviation | Range |
|---|---|---|---|
| LittlEars | 28.9 | 5.9 | 8–35 |
| PEACH Quiet | 2.7 (67.5%) | 0.7 (17.5%) | 1–4 (25–100%) |
| PEACH Noise | 2.6 (65%) | 0.7 (17.5%) | 1.2–4 (30–100%) |
| PEACH Total | 5.3 (66.3%) | 1.3 (16.3%) | 2.2–8 (27.5–100%) |
| SSQ – Composite | 6.9 | 1.4 | 3.1–9.7 |
| SSQ - Speech | 6.4 | 1.7 | 1.6–10 |
| SSQ - Spatial | 6.7 | 1.9 | 0–10 |
| SSQ - Qualities | 7.5 | 1.3 | 2.3–10 |
| SSQ - Conversational | 6.5 | 1.8 | 1.2–10 |
SSQ = Speech, Spatial and Qualities
LittlEARS Auditory Questionnaire
For the LittlEARS questionnaire, the average score was equal to the established criterion score of 28, reflecting that most of the children in the sample had ratings of early auditory behavior that were within the normal range for their age. Figure 1 displays the LittlEARS data for each visit as a function of age in months compared to the normative range from Tsiakpini et al. (2004).
Figure 1.
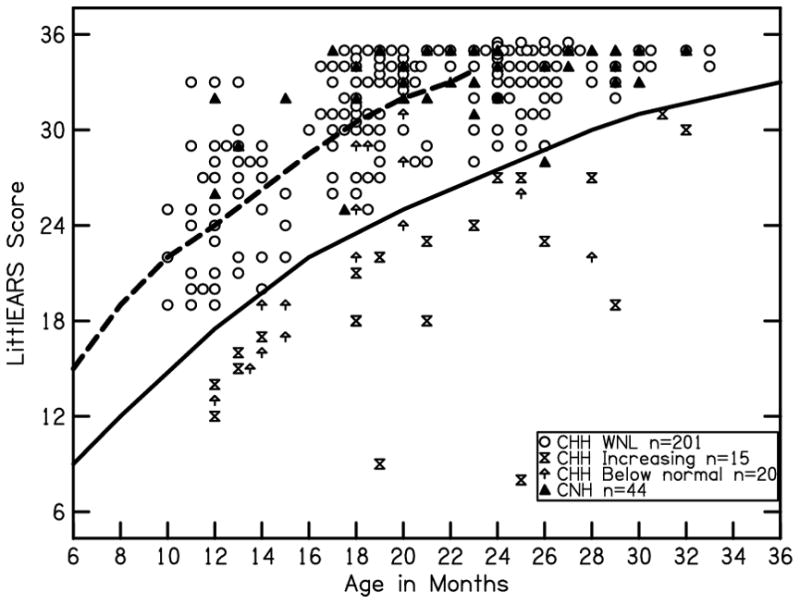
LittlEARS data for all subjects as a function of age in months as compared to normative range from Tsiakpini et al (2004). The solid line represents the lower bound of the 95% confidence interval for the LittlEARS normative range. The dashed line represents the average of the LittlEARS normative range. Open circles represent children who are hard of hearing (CHH) who were always within the normative range. Hourglass symbols represent CHH who were always below the normative range. Upward arrows represent children with scores below the normative range that increased into the normal range at subsequent visits. Black triangles represent children with normal hearing.
All but one of the CNH had scores within the normal range based on the normative data. Ninety-six parents of CHH contributed 236 LittlEARS scores at the 12, 18 and 24 month visits. At the 12 month visit, 33% of CHH had reached the criterion score, increasing to 81% and 91% of CHH at the 18 month and 24 month visits, respectively. Only 9% of the CHH had LittlEARS scores that fell below the normative range for their age at one or more visits. Of the nineteen children with LittlEARS scores outside of the normative range, thirteen were below the normative range at every visit where LittlEARS was administered. Six of the children had LittlEARS scores that increased into the normal range at subsequent visits.
For the statistical analysis of LittlEARS ratings, the highest LittlEARS score at either the 18-month or 2-year visit for each subject was used as an outcome for each subject. Ninety-six CHH contributed LittlEARS scores to the analysis. A linear regression model evaluated the influence of age, degree of hearing loss, aided audibility, HA use, speech recognition, receptive language abilities, and maternal education level on LittlEARS score at the 18-month or 2-year visit. Speech recognition was the word identification score from the O&C test. The overall model was significant [R2 = 0.48, F(7,89) = 12.5, p < 0 .001] suggesting that this combination of factors predicted 48% of the variability in LittlEARS scores. Better hearing thresholds (β = −.32, p = .005), higher aided audibility (β = .28, p = .01), more hours of HA use (β = .19, p = .03), higher word recognition (β = .37, p = .004), and higher receptive language ability (β = .29, p = .02) were associated with higher LittlEARS scores. Age (β = .10, p = .34) and maternal education (β = .17, p = .22) were not significant predictors of LittlEARS scores after controlling for other variables.
PEACH Questionnaire
The data from the PEACH questionnaire for each subject are displayed in Figure 2 along with the normative range for the Quiet and Noise subscales and Total score. The average age at which the PEACH was administered was 21.8 months of age (SD = 4.7 months). The correlation between PEACH and LittlEARS scores for children who had both measures at the 2 year visit was positive and significant (r = 0.68, p < 0.001), indicating that children with higher LittlEARS scores also had higher PEACH scores. For the Quiet subscale and Total PEACH score, the median level of performance for children with hearing loss was below the normal range and within the “possible review indicated” range, suggesting that at least half of the children in the study would be outside of the normal range on this scale. Median scores for children with hearing loss were above the “possible review indicated” range for the Noise subscale. To determine which factors predicted the Total PEACH score (Quiet + Noise subscales) at the 2 year visit, a linear regression model was used to evaluate the influence of age in months, degree of hearing loss, aided audibility, HA use, speech recognition, and receptive language abilities, while controlling for maternal education level. Seventy-five children had PEACH scores and predictors at the 2 year-old visit. The predictor variables included in the model were the same as those used to assess LittlEARS. The overall model was significant [R2 = 0.43, F(6,69) = 7.7, p < 0.001] suggesting that this combination of factors predicted approximately 43% of the variability in Total PEACH score. Lower better-ear PTA (β = −0.48, p = 0.02) and higher aided audibility (β = .58, p < 0.001) and receptive language ability (β = .49, p < 0.001) were associated with higher Total PEACH scores. The relationship between Total PEACH score and average HA use (p = .35), O&C word identification (p = .20), and maternal education (p = .85) were not significant after controlling for the other predictors. Separate analyses of the predictors for PEACH Quiet and Noise subscales were not undertaken because of the high correlation between individual scores for the subscales (r=0.92, p < 0.001).
Figure 2.
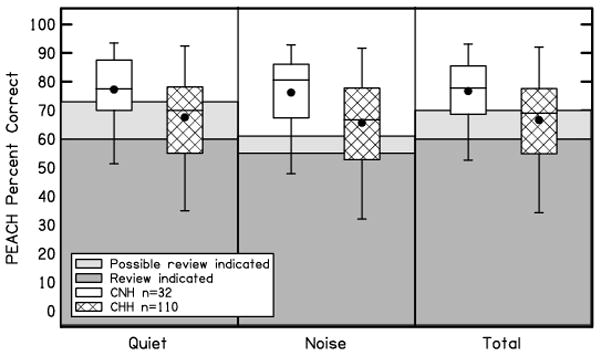
PEACH data with the normative ranges for the Quiet and Noise subscales and Total score for CNH (White boxes) and CHH (Hatched boxes). The data include 85 children who are hard of hearing at the 2 year-old visit and 25 children who are hard of hearing from the 18 month-old visit. The children with normal hearing were all collected at the 2 year-old visit. The boxes represent the 25th-75th percentiles (interquartile range) and the whiskers represent the 5th and 95th percent confidence intervals of the mean. Solid lines are the median and solid circles represent the mean. The light gray shaded region represents the “Possible review indicated” normative range and the dark gray shaded region represents the “Review indicated” normative range from the PEACH.
SSQ Questionnaire
The scores for the SSQ Composite and subscales are displayed in Figure 3. The overall composite mean score of 6.9 is consistent with good listening ability overall and represents an average of all the subtest scores. The differences between subscale scores were evaluated using repeated-measures ANOVA with subscale as a factor. The overall effect of subscale was significant [F(3,921) = 68.15, p < .001, η2p = .18], indicating that the average SSQ rating varied across subscales. Post hoc analysis was completed using Tukey’s Honestly Significant Difference (HSD) with a calculated minimum mean significant difference of 0.24. Given the small minimum mean significant differences, all of the average subscale scores were significantly different from each other. The Speech subscale ratings were lowest (mean = 6.4), followed by Conversational uses of hearing subscale (mean = 6.6), Spatial subscale (mean = 7.2) and Qualities subscale (mean = 7.7). Despite the pattern of significant differences, the subscale ratings were in a similar range indicating good listening abilities on average.
Figure 3.
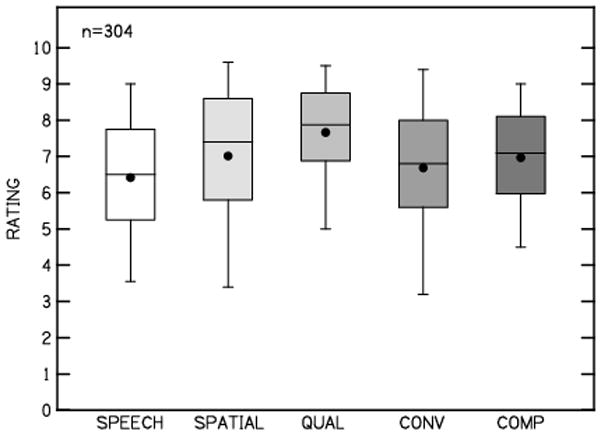
SSQ Composite and Subscale scores. The boxes represent the 25th-75th percentiles (interquartile range) and the whiskers represent the 5th and 95th percent confidence intervals of the mean. Solid lines are the median and solid circles represent the mean. Boxes represent Speech, Spatial, Qualities (QUAL), Conversational Uses of Hearing (CONV) subscales and Composite (COMP).
To evaluate the factors that predicted composite SSQ rating, a linear mixed model was used to evaluate what factors predicted the composite SSQ rating. The SSQ composite scores included repeated-measures from the same subjects at different ages. To account for the correlation between repeated-measures from the same subject at different visits, a random intercept term was included in the model, which is assumed to follow a normal distribution with mean zero and a variance component for each subject. The model included 164 SSQ ratings for 140 unique CHH. The estimated subject specific standard deviation is 0.9 with residual standard deviation 0.88. This yields an intra-cluster correlation of 16% reflecting a small amount of within-subject association. The predictors in the model were degree of hearing loss (better-ear PTA), aided audibility (better-ear aided SII), average HA use, PBK word recognition, receptive language, age in months, and maternal education level. Possible interaction terms were evaluated but were not significant; therefore, they were not included in the final model. The main effect of receptive language (F = 9.78, p = .02) was the only significant predictor of SSQ composite. The relationship between composite SSQ score and degree of hearing loss (p = .623), aided audibility (p = .60), average HA use (p = .54), PBK word recognition (p = .60), age (p=.374), maternal education (p = .70), and were not significant after controlling for receptive language ability.
Cross-sectional word recognition in quiet
The descriptive statistics for the speech perception measures are displayed in Table 3. For all speech recognition measures, scoring was completed at the time of testing.
Table 3.
Descriptive statistics for speech perception outcomes
| Outcome | Mean | SD (% points) | Range |
|---|---|---|---|
| Open and Closed Set | 71% | 30% | 0 – 100% |
| ESP-Monosyllables | 89.7% | 23.1% | 0 – 100% |
| ESP - Spondees | 91.5% | 20.3% | 0 – 100% |
| LNT-Easy | 85.3% | 17.4% | 0 – 100% |
| LNT-Hard | 83.7% | 20.1% | 0 – 100% |
| PBK | 85.5% | 15.6% | 0 – 100% |
| CASPA – Words (−5/10/20 dB SNR) | 15.7/54.5/68.4% | 20.9/35.9/35.2% | 0 – 100% |
| CASPA – Words Aided(−5/10/20 dB SNR) | 16.7/69.7/81.4% | 18.7/18.7/16.6% | 0 – 100% |
| CASPA – Phonemes (−5/10/20 dB SNR) | 32.4/67.5/77.9% | 30.4/36.2/31.9% | 0 – 100% |
| CAPSA – Phonemes Aided(−5/10/20 dB SNR) | 38.9/85.3/92.1% | 19.8/17.4/8.9% | 0 – 100% |
SD = standard deviation
ESP = Early Speech Perception Test
LNT = Lexical Neighborhood Test
PBK = Phonetically-Balanced Kindergarten Word Lists
CASPA = Computer-Assisted Speech Perception Assessment
Open and Closed-Set Task
The percent correct for O&C Phonemes correctly produced, Words correctly produced and words identified in the point-to-picture task are plotted in Figure 4. Of the 119 CHH and 65 CNH who had a 2 year-old visit, 105 CHH (88%) and 60 CNH (92%) were able to complete the word identification component of the O&C. Overall, there was a wide range of performance from 0 – 100 % correct. Two CHH had scores of 0% and 25 had scores of 100% on the identification component.
Figure 4.
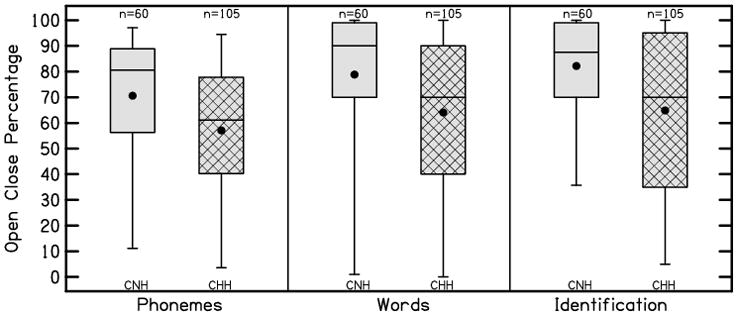
O&C phonemes correctly produced (Phonemes), words correctly produced (Words) and words identified in the point-to-picture task (Identification) for CNH (gray) and CHH (hatched gray) The boxes represent the 25th-75th percentiles (interquartile range) and the whiskers represent the 5th and 95th percent confidence intervals of the mean. Solid lines are the median and solid circles represent the mean.
Linear regression was used to evaluate the concurrent factors at the 2 year visit that predicted O&C word recognition. Degree of hearing loss (better-ear PTA), aided audibility, HA use, maternal education and receptive language ability were used as predictors. The overall model was significant [R2 = 0.35, F(5,85)= 8.9, p <.001] suggesting that this combination of factors predicted approximately 35% of the variability in O&C word identification. Lower better-ear PTA (β = −.42, p < .001), higher aided audibility (β = .27, p =.02), higher receptive language ability (β = .35, p < .001), more hours of HA use (β = .19, p = .04) and higher maternal education level (β = .24, p = .02) were significantly associated with higher O&C word recognition at 2 years of age.
Early Speech Perception Test, Lexical Neighborhood Test and PBK
Aided performance for the ESP for both monosyllables and spondee words was near ceiling levels on average. Figure 5 shows the performance for ESP for CNH and CHH. Further analyses of specific predictors were not attempted for ESP due to the limited range of performance observed across subjects.
Figure 5.
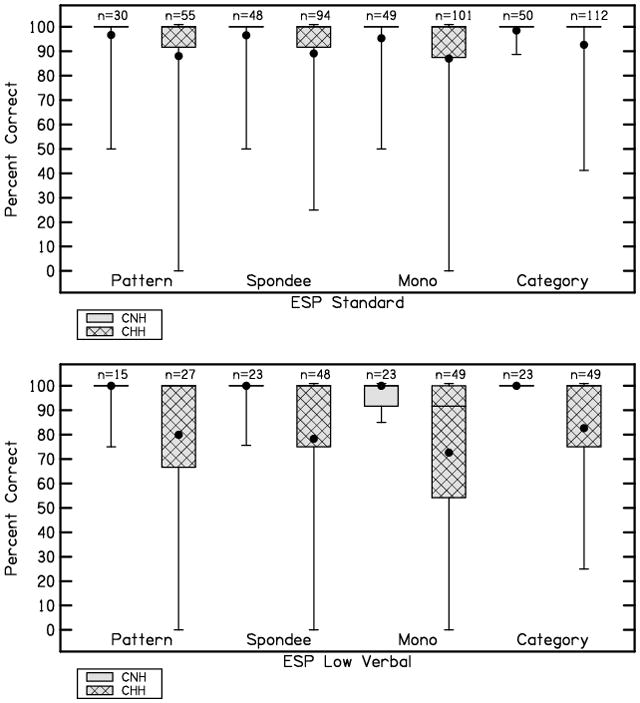
Performance on the Standard and Low Verbal versions of the Early Speech Perception Test for CNH (gray) and CHH (hatched gray). The boxes represent the 25th-75th percentiles (interquartile range) and the whiskers represent the 5th and 95th percent confidence intervals of the mean. Solid lines are the median and solid circles represent the mean.
Figure 6 shows the range of aided performance for LNT-Easy, LNT-Hard and PBK. Children with normal hearing had word recognition above 90% for all three conditions. Average word recognition for LNT-Easy, LNT-Hard and PBK were approximately 85% correct for CHH. To evaluate specific predictors of aided word recognition in quiet for CHH, linear regression was used to evaluate which individual abilities were associated with word recognition. Because of the strong correlations between LNT-Easy, LNT-Hard and PBK (range of r=0.77–0.84, p < .001), linear regression was completed for the average word recognition in quiet for each subject. The average word recognition score was derived by taking the mean of the LNT-Easy, LNT-Hard and PBK scores for an individual subject only if they were collected on the same visit. If a subject had multiple word recognition scores at different visits, only the average word recognition score from the earliest visit for each subject was included in the analysis. The earliest visit was used because word recognition in quiet measured at earlier ages was less likely to be at ceiling than later visits. The age range of children in the analysis was 4–8 years.
Figure 6.
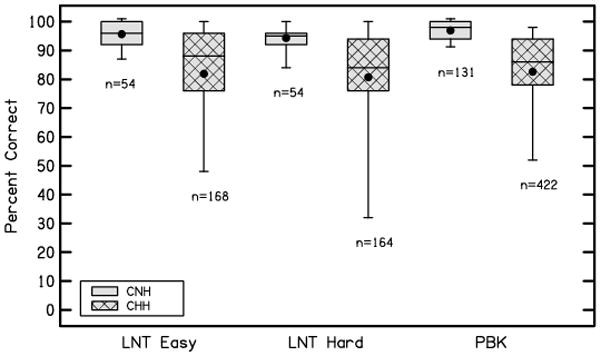
Performance on the LNT-Easy, LNT-Hard and PBK for CNH (gray) and CHH (hatched gray). The boxes represent the 25th-75th percentiles (interquartile range) and the whiskers represent the 5th and 95th percent confidence intervals of the mean. Solid lines are the median and solid circles represent the mean.
For average word recognition in quiet, age (in months), degree of hearing loss (better-ear PTA), aided audibility, HA use, maternal education level, phonological working memory and receptive vocabulary (PPVT) were used as predictors. The overall model was significant [R2 =0 .43, F(7,195) = 20.93, p < .001] suggesting that this combination of factors predicted approximately 43% of the variability in average word recognition in quiet. Higher age (β=0.397, p= < 0.001), higher receptive vocabulary (β = .20, p < .001), higher aided audibility (β = .40, p < .001), and higher phonological working memory (β=0.289, p= < 0.001) were significantly associated with higher average word recognition in quiet. The relationship between average word recognition in quiet and HA use (p = .74) and maternal education level (p = .65) were not significant after controlling for other variables.
Longitudinal predictors of speech recognition in quiet at age 5
For a subset of 49 CHH who contributed data at both 3 year and 5 year visits, a predictive analysis was conducted to determine which factors at 3 years of age predict word recognition in quiet at 5 years of age. Aided audibility, better-ear PTA, Vineland Receptive Language, HA use and maternal education level were used to predict the average word recognition score in quiet at 5 years of age. The overall linear regression model was significant [R2 = .37, F(5,44) = 8.86, p < .001] suggesting that this combination of factors predicted approximately 37% of the variability in average word recognition at 5 years of age. Higher receptive language ability (β = .44, p < .001) and higher aided audibility (β = .30, p = .02) at 3 years of age were significantly associated with higher word recognition at 5 years of age. The relationship between word recognition and degree of hearing loss (p=.52), HA use (p = .73) and maternal education level (p = .41) were not significant after controlling for other variables.
Cross-sectional word recognition in noise
Computer-Aided Speech Perception Assessment
The word and phoneme recognition in noise scores for CNH and the unaided and aided scores for CHH are displayed in Figure 7.
Figure 7.
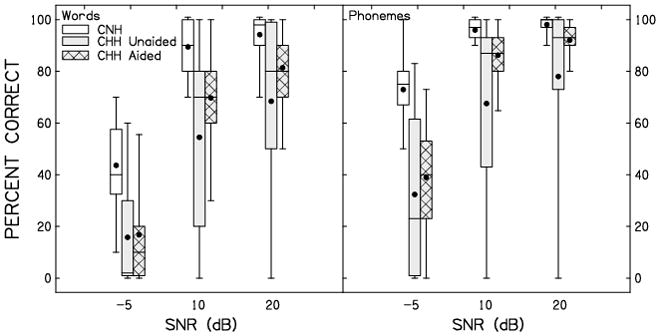
Word and phoneme recognition in noise scores at three signal-to-noise ratios (SNR; −5 dB, 10 dB and 20 dB) for CNH (white) and unaided (gray) and aided (gray hatched) scores for CHH. Left panel is words correct, and right panel is phonemes correct. The boxes represent the 25th-75th percentiles (interquartile range) and the whiskers represent the 5th and 95th percent confidence intervals of the mean. Solid lines are the median and solid circles represent the mean.
The CHH experienced gains in speech recognition in noise with amplification, but did not reach levels of performance equivalent to CNH, even at the most favorable signal-to-noise ratio.
To determine predictors of word recognition in noise, a linear mixed model was used to predict CASPA word recognition scores. The following independent variables were considered: aided condition (aided vs unaided), SNR, aided audibility, age in months, receptive vocabulary (Peabody Picture Vocabulary Test - IV), phonological working memory (Comprehensive Test of Phonological Processing, Nonword Repetition subtest), HA use and maternal education. A linear mixed model allows for the type of correlated responses required for this analysis, because there are repeated measures both across aided and unaided conditions as well as at three signal-to-noise ratios. To account for the correlation, a random intercept term was included in the model which is assumed to follow a normal distribution with mean zero and a variance component for subject. The estimated subject specific standard deviation is 2.01 with residual standard deviation 20.7. This yields an intra-cluster correlation of 9% reflecting a small amount of within-subject association. Possible interaction terms were evaluated but were not significant; therefore, they were not included in the final model. The main effects aided condition (F = 90.01, p < .0001), SNR (F = 272.14, p < .0001), receptive vocabulary (F = 10.99, p = .0004), better ear aided SII (F = 27.86, p < .0001), age in months (F = 3.54, p = .015), maternal education level (F=3.81, p = 0.03) and phonological working memory (F = 11.33, p = .0009) were all significant predictors of CASPA word recognition. Performance in the aided condition was higher than in the unaided condition. Word recognition increased, as expected, as the SNR increased. CHH with higher vocabularies, aided SII, age, maternal education level and phonological working memory had higher CASPA word recognition in noise than peers with lower scores on these factors.
DISCUSSION
Parent responses from auditory development questionnaires and speech recognition measures were documented for CHH from infancy through elementary school years as part of a prospective longitudinal study. Three research questions were posed: 1) How do aided audibility and HA use affect parent-reported auditory skills and children’s speech recognition abilities during early childhood? 2) How do concurrent linguistic, cognitive and demographic factors affect parent-reported auditory skills and children’s speech recognition of CHH during early childhood? and 3) How do aided audibility and HA use influence speech perception in a subgroup of CHH over time? As hypothesized in this study and observed in previous studies (Bagatto et al. 2010; Sininger et al. 2010; Stiles et al. 2012), the overall effects of aided audibility and HA use on parents ratings of auditory skills and on children’s speech recognition were positive. Children who are hard of hearing with greater aided audibility had better outcomes than children with lower aided audibility across a wide range of ages and measures. Greater HA use was associated with higher parent ratings of auditory skills and better speech recognition for the youngest children in the study, but the positive effect of HA use was less consistent at three years of age or older. Higher language abilities also were associated with higher scores on auditory development questionnaires and measures of speech recognition from age two years through early elementary school ages. Children with higher verbal working memory abilities had higher word recognition in quiet and in noise than children with more limited working memory skills, consistent with previous research in children who received cochlear implants (Cleary, Pisoni & Geers, 2001). Higher aided audibility and receptive language at 3 years of age was associated with higher word recognition at 5 years of age.
Auditory development questionnaires
Auditory development questionnaires are an important clinical tool for monitoring the progress of auditory skills for CHH. Previous studies have demonstrated that parent ratings of auditory skills during infancy can help to predict the variability in language outcomes at three years of age (Ching et al. 2013a). Three parent-report measures of auditory development were completed, including LittlEARS, PEACH and SSQ questionnaires. For children at 12 months, 18 months and 2 years of age, the LittlEARS questionnaire was completed for CHH and CNH. Once children reached a criterion score of 28 on the LittlEARS, their parent also completed the PEACH at the same visit and all subsequent visits until 2 years of age. For both questionnaires, CHH had lower scores than CNH, consistent with lower parental ratings of auditory skill development for CHH. The relationship between LittlEARS and PEACH scores was significant, suggesting an association between the auditory skills assessed by each questionnaire. By the 18-month visit, 81% of CHH had scores at the criterion score of 28 or higher. Only 9% of the CHH fell below the normative range CNH on the LittlEARS at one or more visits. The average score on the LittlEARS (29.6) was consistent with results reported by Bagatto and colleagues (2010) for children without severe developmental comorbidities. An analysis of auditory and linguistic factors that predicted LittlEARS scores indicated that CHH with higher aided audibility, HA use, receptive language and O&C test word identification scores had higher LittlEARS scores than CHH with lower scores on these factors. LittlEARS scores based on parent ratings reflect the auditory and linguistic factors that are of interest when monitoring auditory development during early childhood. However, the finding that nearly all of the 18 month-old and two year-old CHH had criterion-level scores on the LittlEARS raises questions as to whether or not the measure would be sufficiently sensitive to identify CHH who may be at-risk for developmental concerns. The elevated LittlEARS scores in this study may reflect the fact that this sample of CHH has generally higher socioeconomic status than the general US population and includes only children from English-speaking homes without additional developmental comorbidities.
However, on the PEACH, more than 50% of the CHH in the current study had PEACH scores in the range “possible review indicated” or poorer. The average scores for the Quiet and Noise subscales and Total scale in this study (66.3% average Total PEACH score) were similar to those reported by Ching and Hill (2007; 62.9%), but lower than the average reported by Bagatto and colleagues for typically-develoing children who wear HAs (82% average Total PEACH score). The trend for Higher PEACH scores reported by Bagatto et al. than were observed in the current study could be attributed, at least in part, to differences in the ages at which the PEACH was administered in each study. In data reported by Ching and Hill (2007), age was a significant positive predictor of Total PEACH scores. The average age of administration in this study was 21 months, whereas the average age for the children reported by Bagatto et al. (2010) for the PEACH was approximately 48 months. Ching and Hill included older children in their sample, but also included children with later ages of hearing loss identification than the current sample. Differences in chronological age and age of identification may help to explain differences between PEACH scores observed in this study and those observed in previous studies of children who wear HAs. The current scoring guidelines for the PEACH do not account for the age of the child, which may lead clinicians to conclude that younger children are at risk for delays in auditory development. PEACH scores indicating that a child may be at-risk for developmental concerns also stand in contrast to the ceiling scores on the LittlEARS questionnaire by some children at the same visit. Clinical protocols for auditory development questionnaires (e.g. Bagatto et al. 2011) have suggested that once children reach a criterion score on the LittlEARS that PEACH should be used subsequently to assess auditory skill development. Data from Bagatto and Scollie (2013) suggest that clinicians should use caution interpreting PEACH results in children less than 24 months of age, since the documented influence of age on PEACH results in this age range may complicate identification of children who are at-risk for developmental delays.
An adapted version of the SSQ Questionnaire (Gatehouse & Noble 2004) was used to assess parents’ perceptions of their child’s listening abilities at ages 4 years, 6 years and 8 years. In addition to the Speech, Spatial and Qualities subscales, a conversational uses of hearing subscale was added for this study to specifically evaluate overhearing, listening in the car, and listening in the presence of television or music. Overall, the composite SSQ score was influenced by receptive language ability, but not by age, aided audibility, amount of HA use or maternal education level. Given that the listening situations and scenarios queried by the SSQ are dependent on the ability of the child to communicate, the relationship between language ability and SSQ score is perhaps not surprising. Parent ratings of their child’s listening ability may be tied to how well their child communicates in everyday listening situations, which could explain the relationship between parent ratings on the SSQ and language ability. The lack of a relationship between variables related to amplification and the SSQ was not expected, but could highlight limitations of aided audibility and HA use as predictors of listening abilities in realistic listening situations with multiple talkers and competing background noise. Aided audibility reflects how much speech is audible in quiet, but may not be a direct reflection of how the child hears from a distance or in background noise. Previous studies have used similar adaptations to the SSQ to assess parents’ ratings of children with unilateral or bilateral cochlear implants (Galvin et al. 2007). The adaptation of the SSQ to allow parent responses may have reduced the validity of the measure. Further research is needed to assess the validity of this version of the SSQ for children who wear HAs.
Speech recognition outcomes
Children who wear amplification generally demonstrated high levels of speech understanding in quiet across a wide range of speech recognition measures and ages, particularly compared to results from previous studies with cohorts of children who were identified with hearing loss or fit with amplification at later ages or had greater degrees of hearing loss (Kirk et al. 1995; Blamey et al. 2001; Davidson & Skinner 2006). For two-year-old children on the O&C test, HA use and language abilities explained the variability in performance across subjects. Results from the Early Speech Perception test at ages 2 and 3 years were consistently near ceiling for both CNH and CHH. The O&C task not only had a high rate of successful administration in both groups (CNH-92%, CHH, 88%), but children had a range of performance that was related to aided audibility, language and HA use. This suggests that compared to the Early Speech Perception test, the O&C test may be useful in assessing speech recognition abilities in 2 year-olds and differentiating children with varying auditory abilities.
Aided word recognition in quiet was completed with three different sets of monosyllabic word stimuli (LNT-Easy, LNT-Hard, and PBK) with CHH between 4–8 years of age. The mean for aided word recognition in quiet across all three measures was 85% and strong associations were observed between the three different stimulus sets for the same subjects collected at the same visit. Using a cross-sectional analysis that averaged results from the three stimulus sets for each subject, CHH with higher aided audibility, higher receptive vocabulary, higher phonological working memory, and lower better-ear PTA had higher word recognition scores in quiet compared to CHH with lower scores on these factors. This analysis highlights the combination of bottom-up (aided audibility and degree of hearing loss) and top-down (receptive vocabulary and phonological working memory) factors that influence speech recognition in quiet for CHH. A longitudinal analysis using a subset of CHH was used to evaluated the factors at 3 years of age that predicted word recognition in quiet at 5 years of age. As in the cross-sectional analyses, higher aided audibility and receptive language ability at 3 years of age were associated with higher word recognition in quiet at 5 years of age, though degree of hearing loss and the amount of HA use at age 3 were not associated with word recognition in quiet at age 5 after controlling for other predictors.
Similar results were observed for word recognition abilities in noise, measured by CASPA. Aided audibility, language skills, age and phonological working memory skills were all positively associated with CASPA word recognition scores in noise. Compared to word recognition scores in quiet, which were near ceiling for many CHH, CASPA word recognition in noise was more variable and might be expected to be more sensitive to differences in auditory skills as a result. Children who are hard of hearing had increases in speech recognition in noise with amplification compared to without amplification at all three signal-to-noise ratios. Although HAs are not often considered to help speech understanding in background noise, the additional audibility provided an advantage compared to unaided listening. Even with amplification, however, CHH did not approximate the word recognition in noise abilities of their peers with normal hearing. This discrepancy highlights the fact that HAs alone are unlikely to be sufficient to support optimal speech understanding in noise. Hearing assistance technology, such as remote microphone systems, may be necessary in classrooms and other noisy environments where high levels of speech recognition can support learning.
Aided audibility
The aided audibility of speech was measured with the child’s amplification at each study visit using probe microphone verification techniques. As predicted, children with higher aided audibility through their HAs generally had better auditory development outcomes than children with poorer aided audibility. This finding is consistent with a number of previous studies and supports the fundamental idea that providing optimally fitted amplification can help to offset the negative effects of hearing loss on auditory development skills (Blamey et al. 2001; Sininger et al. 2010; Bagatto et al. 2010; Stiles et al. 2012). . Children with the same pure tone average thresholds may have a wide range of aided audibility due to the configuration of their hearing loss or proximity of the fitting to validated prescriptive targets (Strauss & van Dijk 2008; McCreery, Bentler & Roush 2013; McCreery et al. this issue pp.xxxx). The degree to which speech can be made audible through amplification is strongly dependent on the child’s degree of hearing loss. Aided audibility is preferable to estimates of degree of hearing loss, such as the pure tone average, because it is a more direct estimate of how much the child can hear when wearing their HAs. Aided audibility was positively associated with multiple measures of word recognition in quiet from 2–8 years of age and also was positively associated with word recognition in noise for 7–9 year-olds. Children with higher aided audibility also had higher scores on auditory development questionnaires, including the LittlEARS and PEACH, at 12 months, 18 months and 2 years of age. Although aided audibility was not a significant predictor of SSQ questionnaire scores for 4-, 6-, and 8 year-old children, aided audibility was positively correlated with receptive language ability in this age range, which was the only significant positive predictor of SSQ scores. Aided audibility at 3 years of age was associated with higher word recognition abilities at 5 years of age in a longitudinal analysis. These results support the notion that increased speech audibility through amplification has a significant positive effect on auditory development outcomes in children across a wide range of ages from infancy through early elementary school years.
HA use
The average number of hours per day that children wore their HAs was estimated by parents at each study visit. Consistent HA use is predicted to support auditory development by providing regular access to auditory input. Establishing consistent HA use appears to be most challenging for infants and toddlers with the consistency of use increasing as age increases (Walker et al. 2013; Walker et al. this issue, pp. XXXX). The positive effects of HA use on auditory development outcomes were isolated to outcomes that were measured during infancy and early childhood, including the LittlEARS questionnaire and the O&C word recognition measure at age 2. More hours of HA use were not associated with higher scores on the PEACH or SSQ questionnaires or any of the measures of word recognition obtained at three years of age or older.
Several factors could help to explain why the positive influence of HA use may be limited to the youngest age groups in the study. Because the number of hours of HA use increased as age increased and variability in use across children decreased, HA use may have been sufficiently high to support positive outcomes for older children. More uniform amounts of HA use across children at older ages may have limited its utility as a predictor of variability in outcomes. Children with the greatest degrees of hearing loss may have more hours of HA use per day than children with milder hearing loss (Walker et al. 2013; Walker et al. this issue). Because children with greater degrees of hearing loss may also have poorer aided audibility, the positive influence of HA use on outcomes could potentially be offset by reduced audibility. The negative relationship between HA use and degree of hearing loss is a complicating factor that should be accounted for in studies that attempt to associate outcomes with the amount of HA use.
Nonetheless, more HA use during infancy is associated with better outcomes when controlling for a wide range of other influential factors. The HA use data used to predict auditory development questionnaires and speech recognition was collected based on parent report. The amount of HA use may only reflect the average amount of HA use since the previous study visit. An estimate of HA use that is averaged over a longer time period may be more likely to demonstrate a cumulative effect on developmental outcomes, as was the case with language development in another article in this supplement (Tomblin et al. this issue, pp. XXXX).
Language ability and working memory
Although factors such as aided audibility and HA use are important for describing how CHH access acoustic environments, receptive language and phonological working memory reflect the skills that are necessary to process incoming auditory stimuli. Receptive language ability, as measured by the Vineland Adaptive Behavior Scales, was positively associated with speech recognition and parent ratings on auditory development questionnaires across all measures and age groups. Receptive vocabulary ability based on the Peabody Picture Vocabulary Test was also associated with word recognition in quiet and in noise for older children. The positive relationship between language abilities and word recognition in children has been reported for children with HAs and those with cochlear implants (Blamey et al. 2001; Davidson et al. 2011). Children with higher receptive language abilities also had higher scores on auditory development questionnaires. Auditory development questionnaires often include questions that may reflect the child’s auditory awareness and ability to understand speech in different everyday listening environments. Verbal working memory, which is the ability to temporarily store and process auditory information, was also positively associated with word recognition in quiet and in noise, consistent with previous research in children with cochlear implants (Cleary, Pisoni & Geers, 2001). Top-down processes, such as language abilities and working memory, can be supportive of speech recognition when the audibility of the acoustic representation of speech is limited because of noise (McCreery & Stelmachowicz 2011) and/or hearing loss (Jerger 2007; DesJardin, Ambrose & Eisenberg, 2009; Davidson et al. 2011).
The significant positive association between aided audibility and receptive language ability that was observed across the age range among children in this study should be noted. Aided audibility has clear positive contributions to speech recognition and parent ratings on auditory development questionnaires in CHH, even when the influence of language ability is considered. However, aided audibility also have an indirect influence on these outcomes by enhancing the child’s language abilities. Although further analyses would be needed to quantify the interactions between audibility, language and auditory skills, the complex relationship between these factors highlights the challenges experienced by children with reduced auditory access. Not only do reductions in aided audibility negatively affect auditory development outcomes, but they also may inhibit the development of top-down skills, such as receptive language ability, that can support listening in noise or at a distance when speech is less audible. The long-term effects of limited audibility may extend beyond restricted access to the acoustic signal into the ability to understand degraded speech.
Clinical implications
The positive effects of providing amplification on auditory skill development in a large group of children who wear HAs have multiple clinical implications for audiologists who serve this population. First, these findings highlight the importance of early amplification that provides audibility for speech and is used at a consistently high level by the child. Fortunately, aided audibility and HA use are both easy to document clinically and to monitor over time. Aided audibility can be estimated easily as part of clinical HA verification and parent report of HA use has been shown to be reasonably accurate for identifying challenges to establishing consistent use (Walker et al. 2013).
Results for word recognition from the current study, particularly in quiet, suggest the need for new tools to assess speech recognition abilities in children who wear HAs and are identified with hearing loss and fit with HAs earlier than in the recent past. Children with a wide range of degrees of hearing loss performed near ceiling levels on multiple word recognition measures in quiet. Whereas this represents significant progress from earlier studies of word recognition abilities in later-identified CHH (e.g., Kirk et al. 1995), the utility of these measures in quiet may be limited in identifying children who are at-risk for listening difficulties in their everyday listening situations (Lewis et al. 2014). Word recognition in quiet was not found to be related to auditory skills queried on auditory development questionnaires with the exception of the O&C measure, which was positively associated with LittlEARS scores at age two. The O&C test at age two appears to provide a range of performance across children with varying auditory skills. Performance on the CASPA word recognition in noise test was highly variable across subjects, which allowed for a better examination of individual differences in speech recognition ability than test materials that yield performance near ceiling for most CHH. When CHH reach speech recognition near ceiling in quiet, speech recognition testing in noise may help to better differentiate children who will face challenges listening in realistic situations. The clinical utility of identifying children who at at-risk for listening difficulties using word recognition tests in quiet appears to be limited and warrants further consideration.
Limitations and directions for future research
Several limitations of the findings from this study should be noted. Although the sample of CHH was well-matched to the group with normal hearing, the entire sample was more economically-advantaged (Tomblin et al. this issue, pp. XXXX) than the general population in the United States. For this reason, the results observed in this cohort may be different than would be observed in a population-based sample of children who use HAs. This pattern may have particularly affected measures such as the LittlEARS questionnaire and Early Speech Perception Test, where the results were significantly higher than have been reported in previous studies.
The current study also excluded children with additional disabilities, which is likely to lead to results that are more positive than would be observed in the general population. The goal in doing so was to help to identify the specific developmental consequences of hearing loss. While up to 40% of CHH may have additional disabilities, previous studies that have attempted to include children with additional developmental disabilities (e.g. Ching et al. 2013a) have excluded this group from overall analyses because of missing data. Results from groups that have included children with additional disabilities (Bagatto et al. 2010; Ching et al. 2013a) have found outcomes to be poorer in children with additional disabilities, although the degree to which the group deviates from children with hearing loss who are otherwise typically-developing is highly variable and dependent on the specific condition and severity of the disability. The present results do not reflect the potential range of outcomes among children with additional developmental disabilities.
Finally, a consistent pattern was observed between aided audibility, HA use, language and the auditory development questionnaires and speech recognition outcomes in this study. However, none of the statistical models accounted for more than 50% of the variability in any of the outcomes. While the amount of variance accounted for in these models is consistent with previous studies of children who received cochlear implants (Davidson et al. 2011 or Geers et al. 2003), there may be other factors, such as working memory or executive function, or outcome measures that could better account for the remaining variability in auditory development questionnaires or speech recognition in CHH.
Summary
The goal of the current analysis was to determine the effect of aided audibility and HA use on auditory development outcomes in CHH who use HAs. Aided audibility had a positive impact on auditory skills, as measured by parent report from auditory development questionnaires and speech recognition in quiet and with competing noise. Aided audibility can be maximized by providing early amplification that matches validated prescriptive targets for the child’s degree of hearing loss (McCreery et al. 2013). Children with more hours of HA use had higher word recognition and parent ratings on auditory development questionnaires between 1–2 years of age, but the impact of HA use was not observed for older age groups where use became more consistent across the cohort. Receptive language ability was also positively associated with auditory development outcomes across the age range. Professionals can maximize auditory development in children by verifying that the child has consistent audibility and monitoring and encouraging consistent HA use.
Supplementary Material
SHORT SUMMARY.
This paper describes the influence of audibility, hearing aid use and language abilities on speech recognition and parent ratings of auditory development for a large group of children who are hard of hearing. Audibility, hearing aid use and language ability were positive predictors of parent ratings and speech recognition outcomes across the age range. The clinical implications for increasing audibility and promoting consistent hearing aid use on these outcomes are discussed.
Acknowledgments
Source of Funding:
This research was supported by the following grants from the NIH-NIDCD: R01DC009560 and R01DC013591. The authors had full editorial control of this work and manuscript.
This research was supported by the following grants from the NIH-NIDCD: R01DC009560 and R01DC013591. The authors wish to thank Marc Brennan and Kris Fernau for their helpful contributions in preparing the manuscript and analyzing data.
Footnotes
Conflicts of Interest:
The authors have no conflicts of interest to declare.
See Supplemental Digital Content, Appendix A List of Acronyms used throughout Outcomes in Children with Hearing Loss Study.
References
- Ambrose SE, Berry LMU, Walker EA, Harrison M, Oleson J, Moeller MP. Speech Sound Production in Two-Year-Olds who are Hard of Hearing. American Journal of Speech-Language Pathology. 2014;23:91–104. doi: 10.1044/2014_AJSLP-13-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ANSI. S3. 5-1997 R-2007, American national standards methods for the calculation of the articulation index. New York: American National Standards Institute; 1997. [Google Scholar]
- ANSI. S3.22–2003. Specifications of Hearing Aid Characteristics. New York: American National Standards Institute; 2003. [Google Scholar]
- Bagatto MP, Scollie SD, Seewald RC, Moodie KS, Hoover BM. Real-ear-to-coupler difference predictions as a function of age for two coupling procedures. Journal of the American Academy of Audiology. 2002;13(8):407–415. [PubMed] [Google Scholar]
- Bagatto MP, Moodie ST, Malandrino AC, Richert FM, Clench DA, Scollie SD. The University of Western Ontario Pediatric Audiological Monitoring Protocol (UWO PedAMP) Trends in Amplification. 2011;15(1):57–76. doi: 10.1177/1084713811420304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagatto M, Scollie SD, Hyde M, Seewald R. Protocol for the provision of amplification within the Ontario Infant Hearing Program. International Journal of Audiology. 2010;49(S1):S70–S79. doi: 10.3109/14992020903080751. [DOI] [PubMed] [Google Scholar]
- Bagatto MP, Scollie SD. Validation of the Parents’ Evaluation of Aural/Oral Performance of Children (PEACH) Rating Scale. Journal of the American Academy of Audiology. 2013;24(2):121–125. doi: 10.3766/jaaa.24.2.5. [DOI] [PubMed] [Google Scholar]
- Bentler R, Walker E, McCreery R, Arenas RM, Roush P. Nonlinear Frequency Compression in Hearing Aids: Impact on Speech and Language Development. Ear and hearing. 2014;35(4):e143–e152. doi: 10.1097/AUD.0000000000000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingham K, Jenstad LM, Shahnaz N. Longitudinal changes in real-ear to coupler difference measurements in infants. Journal of the American Academy of Audiology. 2009;20(9):558–568. doi: 10.3766/jaaa.20.9.4. [DOI] [PubMed] [Google Scholar]
- Blamey PJ, Sarant JZ, Paatsch LE, Barry JG, Bow CP, Wales RJ, Tooher R. Relationships among speech perception, production, language, hearing loss, and age in children with impaired hearing. Journal of Speech, Language, and Hearing Research. 2001;44(2):264–285. doi: 10.1044/1092-4388(2001/022). [DOI] [PubMed] [Google Scholar]
- Boothroyd A. Computer-Assisted Speech Perception Assessment (CASPA v2. 2) San Diego, CA: Author; 1999. [Google Scholar]
- Boothroyd A, Eran O. Auditory speech perception capacity of child implant users expressed as equivalent hearing loss. Volta Review. 1994;96(5):151–67. [Google Scholar]
- Bradley RH, Corwyn RF. Socioeconomic status and child development. Annual Review of Psychology. 2002;53(1):371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Ching TY, Dillon H, Marnane V, Hou S, Day J, Seeto M, Yeh A. Outcomes of early-and late-identified children at 3 years of age: findings from a prospective population-based study. Ear and Hearing. 2013a;34(5):535–552. doi: 10.1097/AUD.0b013e3182857718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TY, Leigh G, Dillon H. Introduction to the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study: Background, design, sample characteristics. International Journal of Audiology. 2013b;52(S2):S4–S9. doi: 10.3109/14992027.2013.866342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TY, Crowe K, Martin V, Day J, Mahler N, Youn S, Orsini J. Language development and everyday functioning of children with hearing loss assessed at 3 years of age. International Journal of Speech-Language Pathology. 2010;12(2):124–131. doi: 10.3109/17549500903577022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching TY, Hill M. The Parents’ Evaluation of Aural/Oral Performance of Children (PEACH) Diary. Chatswood. New South Wales, Australia: Australian Hearing; 2005. Retrieved from outcomes.nal.gov.au. [Google Scholar]
- Ching TY, Hill M. The parents’ evaluation of aural/oral performance of children (PEACH) scale: Normative data. Journal of the American Academy of Audiology. 2007;18(3):220–235. doi: 10.3766/jaaa.18.3.4. [DOI] [PubMed] [Google Scholar]
- Cleary M, Pisoni DB, Geers AE. Some measures of verbal and spatial working memory in eight-and nine-year-old hearing-impaired children with cochlear implants. Ear and Hearing. 2001;22(5):395. doi: 10.1097/00003446-200110000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coninx F, Weichbold V, Tsiakpini L, Autrique E, Bescond G, Tamas L, Brachmaier J. Validation of the LittlEARS Auditory Questionnaire in children with normal hearing. International Journal of Pediatric Otorhinolaryngology. 2009;73(12):1761–1768. doi: 10.1016/j.ijporl.2009.09.036. [DOI] [PubMed] [Google Scholar]
- Davidson LS, Skinner MW. Audibility and speech perception of children using wide dynamic range compression hearing aids. American Journal of audiology. 2006;15(2):141–153. doi: 10.1044/1059-0889(2006/018). [DOI] [PubMed] [Google Scholar]
- Davidson LS, Geers AE, Blamey PJ, Tobey E, Brenner C. Factors contributing to speech perception scores in long-term pediatric CI users. Ear and Hearing. 2011;32(1 Suppl):19S. doi: 10.1097/AUD.0b013e3181ffdb8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DesJardin JL, Ambrose SE, Martinez AS, Eisenberg LS. Relationships between speech perception abilities and spoken language skills in young children with hearing loss. International Journal of Audiology. 2009;48(5):248–259. doi: 10.1080/14992020802607423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan SC, Duncan TE, Hops H. Analysis of longitudinal data within accelerated longitudinal designs. Psychological Methods. 1996;1(3):236. [Google Scholar]
- Dunn LM, Dunn DM. Peabody Picture Vocabulary Test. 4. Circle 676 Pines, MN: American Guidance Service; 2007. [Google Scholar]
- Ertmer DJ, Miller C, Queensberry J. The Open and Closed-Set Test. West Lafayette, IN: Purdue University; 2004. Unpublished document. [Google Scholar]
- Galvin KL, Mok M, Dowell RC. Perceptual benefit and functional outcomes for children using sequential bilateral cochlear implants. Ear and Hearing. 2007;28(4):470–482. doi: 10.1097/AUD.0b013e31806dc194. [DOI] [PubMed] [Google Scholar]
- Gatehouse S, Noble W. The speech, spatial and qualities of hearing scale (SSQ) International Journal of Audiology. 2004;43(2):85–99. doi: 10.1080/14992020400050014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geers A, Brenner C, Davidson L. Factors associated with development of speech perception skills in children implanted by age five. Ear and Hearing. 2003;24(1):24S–35S. doi: 10.1097/01.AUD.0000051687.99218.0F. [DOI] [PubMed] [Google Scholar]
- Geers AE, Moog JS. Speech perception and production skills of students with impaired hearing from oral and total communication education settings. Journal of Speech, Language, and Hearing Research. 1992;35(6):1384–1393. doi: 10.1044/jshr.3506.1384. [DOI] [PubMed] [Google Scholar]
- Harrison M, Roush J. Age of suspicion, identification, and intervention for infants and young children with hearing loss: A national study. Ear and Hearing. 1996;17(1):55–62. doi: 10.1097/00003446-199602000-00007. [DOI] [PubMed] [Google Scholar]
- Haskins J. Kindergarten phonetically balanced word lists (PBK) St. Louis: Auditec; 1949. [Google Scholar]
- Holte L, Walker E, Oleson J, Spratford M, Moeller MP, Roush P, Tomblin JB. Factors influencing follow-up to newborn hearing screening for infants who are hard of hearing. American Journal of Audiology. 2012;21(2):163–174. doi: 10.1044/1059-0889(2012/12-0016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerger S. Current state of knowledge: Perceptual processing by children with hearing impairment. Ear and Hearing. 2007;28(6):754–765. doi: 10.1097/AUD.0b013e318157f049. [DOI] [PubMed] [Google Scholar]
- Keefe DH, Bulen JC, Arehart KH, Burns EM. Ear-canal impedance and reflection coefficient in human infants and adults. The Journal of the Acoustical Society of America. 1993;94(5):2617–2638. doi: 10.1121/1.407347. [DOI] [PubMed] [Google Scholar]
- Kirk KI, Pisoni DB, Osberger MJ. Lexical effects on spoken word recognition by pediatric cochlear implant users. Ear and Hearing. 1995;16(5):470. doi: 10.1097/00003446-199510000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehlinger KM, Van Horne AJO, Moeller MP. Grammatical outcomes of 3-and 6-year-old children who are hard of hearing. Journal of Speech, Language, and Hearing Research. 2013;56(5):1701–1714. doi: 10.1044/1092-4388(2013/12-0188). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis DE, Valente DL, Spalding JL. Effect of Minimal/Mild Hearing Loss on Children’s Speech Understanding in a Simulated Classroom. Ear and Hearing. 2014 doi: 10.1097/AUD.0000000000000092. Published ahead of press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreery RW, Bentler RA, Roush PA. Characteristics of hearing aid fittings in infants and young children. Ear and Hearing. 2013;34(6):701–710. doi: 10.1097/AUD.0b013e31828f1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreery RW, Stelmachowicz PG. Audibility-based predictions of speech recognition for children and adults with normal hearing. The Journal of the Acoustical Society of America. 2011;130(6):4070–4081. doi: 10.1121/1.3658476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreery RW, Walker EA, Spratford M, Bentler R, Holte L, Roush P, Oleson J, Van Buren J, Moeller MP. Longitudinal predictors of aided speech audibility in infants and children. Ear and Hearing. doi: 10.1097/AUD.0000000000000211. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meserole RL, Carson CM, Riley AW, Wang NY, Quittner AL, Eisenberg LS, Niparko JK. Assessment of health-related quality of life 6 years after childhood cochlear implantation. Quality of Life Research. 2013:1–13. doi: 10.1007/s11136-013-0509-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3):e43–e43. doi: 10.1542/peds.106.3.e43. [DOI] [PubMed] [Google Scholar]
- Moeller MP, Hoover B, Peterson B, Stelmachowicz P. Consistency of hearing aid use in infants with early-identified hearing loss. American Journal of Audiology. 2009;18(1):14–23. doi: 10.1044/1059-0889(2008/08-0010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller MP, Tomblin JB. An introduction to the Outcomes of Children with Hearing Loss Study. Ear and Hearing. doi: 10.1097/AUD.0000000000000210. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moog JS, Geers AE. Early speech perception test. St. Louis: Central Institute for the Deaf; 1990. [Google Scholar]
- Niparko JK, Tobey EA, Thal DJ, Eisenberg LS, Wang NY, Quittner AL CDaCI Investigative Team. Spoken language development in children following cochlear implantation. JAMA. 2010;303(15):1498–1506. doi: 10.1001/jama.2010.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osberger MJ, Zimmerman-Phillips S, Koch DB. Cochlear implant candidacy and performance trends in children. ANNALS OF OTOLOGY RHINOLOGY AND LARYNGOLOGY. 2002;111(5 PART 2):62–65. doi: 10.1177/00034894021110s513. [DOI] [PubMed] [Google Scholar]
- Pavlovic CV. Derivation of primary parameters and procedures for use in speech intelligibility predictions. The Journal of the Acoustical Society of America. 1987;82(2):413–422. doi: 10.1121/1.395442. [DOI] [PubMed] [Google Scholar]
- R Core Development Team. R: A language and environment for statistical computing [Computer software] 2014 Available from www.R-project.org.
- Scollie S, Seewald R, Cornelisse L, Moodie S, Bagatto M, Laurnagaray D, Pumford J. The desired sensation level multistage input/output algorithm. Trends in amplification. 2005;9(4):159–197. doi: 10.1177/108471380500900403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sininger YS, Grimes A, Christensen E. Auditory development in early amplified children: Factors influencing auditory-based communication outcomes in children with hearing loss. Ear and Hearing. 2010;31(2):166. doi: 10.1097/AUD.0b013e3181c8e7b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow S, Balla D, Cicchetti D. Vineland Adaptive Behavior Scales. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- Stiles DJ, Bentler RA, McGregor KK. The speech intelligibility index and the pure-tone average as predictors of lexical ability in children fit with hearing aids. Journal of Speech, Language, and Hearing Research. 2012;55(3):764–778. doi: 10.1044/1092-4388(2011/10-0264). [DOI] [PubMed] [Google Scholar]
- Strauss S, van Dijk C. Hearing instrument fittings of pre-school children: Do we meet the prescription goals? International Journal of Audiology. 2008;47(S1):S62–S71. doi: 10.1080/14992020802300904. [DOI] [PubMed] [Google Scholar]
- Tobey EA, Thal D, Niparko JK, Eisenberg LS, Quittner AL, Wang NY. Influence of implantation age on school-age language performance in pediatric cochlear implant users. International Journal of Audiology. 2013;52(4):219–229. doi: 10.3109/14992027.2012.759666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin JB, Oleson JJ, Ambrose SE, et al. The Influence of Hearing Aids on the Speech and Language Development of Children with Hearing Loss. JAMA Otolaryngology - Head & Neck Surgery. 2014;140:403–409. doi: 10.1001/jamaoto.2014.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin JB, Walker EA, McCreery RW, Arenas RM, Harrison M, Moeller MP. Outcomes of children with hearing loss: Data collection and methods. Ear and Hearing. doi: 10.1097/AUD.0000000000000212. this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torgesen J, Wagner R, Rashotte C. Comprehensive test of phonological processing CTOPP. Austin, TX: Pro-ed; 1999. [Google Scholar]
- Tsiakpini L, Weichbold V, Kuehn-Inacker H, Coninx F, D’Haese P, Almadin S. LittlEARS auditory questionnaire. Innsbruck: MED-EL; 2004. [Google Scholar]
- Walker EA, Holte L, Spratford M, et al. Timeliness of Service Delivery for Children With Later- Identified Mild-to-Severe Hearing Loss. American Journal of Audiology. 2014;23:116–128. doi: 10.1044/1059-0889(2013/13-0031). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker EA, McCreery RW, Spratford M, Oleson JJ, Van Buren J, Bentler R, Roush P, Moeller MP. Trends and predictors of longitudinal hearing aid use for children who are hard of hearing. Ear and Hearing. doi: 10.1097/AUD.0000000000000208. in submission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker EA, Spratford M, Moeller MP, et al. Predictors of hearing aid use time in children with mild-to-severe hearing loss. Language, Speech, and Hearing Services in the Schools. 2013;44:73–88. doi: 10.1044/0161-1461(2012/12-0005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waltzman SB, Roland JT. Cochlear implantation in children younger than 12 months. Pediatrics. 2005;116(4):e487–e493. doi: 10.1542/peds.2005-0282. [DOI] [PubMed] [Google Scholar]
- Wang NY, Eisenberg LS, Johnson KC, Fink NE, Tobey EA, Quittner AL CDaCI Investigative Team. Tracking development of speech recognition: longitudinal data from hierarchical assessments in the Childhood Development after Cochlear Implantation Study. Otology & Neurotology. 2008;29(2):240. doi: 10.1097/MAO.0b013e3181627a37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


