Abstract
Context
Latinos experience significant health disparities at the end of life compared with non-Latinos.
Objectives
To determine the feasibility of a patient navigator intervention to improve palliative care outcomes for Latino adults with serious illness.
Methods
This was a pilot randomized controlled trial that included 64 Latino adults with life-limiting illness randomized to an intervention or control group. All participants received a packet of linguistically matched materials on palliative care. In addition, intervention participants received up to five home visits from the bilingual, bicultural patient navigator. Visits focused on addressing barriers to palliative care through education, activation, and culturally tailored messaging. Outcomes included feasibility and advance care planning rates, documentation of pain management discussions in the medical record, and hospice utilization.
Results
Of the 32 patients randomized to the intervention arm, 81% had at least one home visit (range 1–5) with the patient navigator. Overall, advance care planning was higher in the intervention group – 47% (n = 15) vs. 25% (n = 8) (P=0.06), and 79% of intervention participants had a discussion about pain management documented in their medical record vs. 54% of control patients (P = 0.05). Hospice enrollment between the two groups (n=18 decedents) was similar (n=7 intervention vs. n=6 control; length of stay in the intervention group was 36.4± 51.6 days vs. 19.7±33.6 days for control patients (P = 0.39).
Conclusion
A culturally tailored patient navigator intervention was feasible and suggests improved palliative care outcomes for Latinos facing advanced medical illness, justifying a fully powered randomized controlled trial.
Keywords: patient navigation, health disparities, palliative care
Introduction
Latinos are more likely to die in an institution,1 less likely to receive adequate pain control,2–7 and rarely receive hospice services.8–10 Palliative care has been shown to improve outcomes for patients at the end of life, including decreasing symptom burden, improving quality of life, and working with patients and families to help ensure that the medical care provided is congruent with goals and preferences. However, cultural values have a major impact on care preferences at the end of life for many ethnic minorities.11–14 A one-size-fits-all approach may not be sufficient and will further widen the gap of cultural differences and health disparities. Culturally congruent or tailored interventions to improve palliative care outcomes for Latinos facing serious illness are needed.
Latinos are now the largest ethnic minority in the United States and are expected to grow by 188% over the next 50 years.15 As the size of this ethnic group increases, we must meet the goal of improved end-of-life care in a manner that is compatible with identified unique needs and preferences and addresses perceived barriers to quality palliative care.14,16,17 Observational data suggests that Latinos are less likely to have a living will, a medical durable power of attorney (MDPOA), or a Do Not Resuscitate (DNR) order.12,18–22 Furthermore, Latinos are more likely to choose very aggressive care in the face of serious or incurable illness and less likely to acknowledge their terminally ill status.12,18 Latinos are less likely to have knowledge of advance directives18,23,24 and are more likely to report that they have not discussed advance care planning with their health care providers.25 Ethnicity is increasingly recognized as being predictive of poor pain assessment and management.26–29 Barriers to adequate pain management have been identified at the institution level; because of physician bias; and as a result of cultural beliefs.6,30,31 A landmark study of outpatient oncology practices6 found that 65% of minorities did not receive guideline-recommended analgesic prescriptions, compared with 50% of non-minority patients. Latino patients in particular reported less pain relief and had less adequate analgesia. Latinos, however, also reported more concerns about taking too much medication, were more worried about medication side effects, and believed they needed more information about pain management. More recent studies suggest these disparities persist. 32–36 Lastly, hospice services are rarely accessed by non-Caucasians.37,38 Barriers experienced by Latinos include lack of awareness of hospice, language discordance, cultural insensitivity of care providers, socioeconomic factors related to citizenship, prohibitive cost of care,10 and a preference for family caregiving networks.39
Patient navigators work with patients and families to address barriers to care and have been involved with efforts to improve health outcomes within the Latino community for over a decade. The role of patient navigator has been defined in different ways in various settings. In a health care system, a navigator may be a nurse or social worker trained to facilitate navigating a particular health care system. In the community, navigators (also referred to as promotores de salud, guias, native sisters, health advocates) are often lay people who are part of or identify with the community with which they work. Their role is to educate, activate, and advocate for patients and families, addressing barriers to care. In 1990, Dr. Harold Freeman started one of the first community patient navigation demonstration projects to improve screening mammography in East Harlem.40–43 In the decades that have followed, navigators have demonstrated they can help reduce health disparities in underserved and vulnerable populations by improving rates of cancer screening, following up on abnormal diagnostic tests and adherence to chemotherapy regimens, and providing support through survivorship.44–47 Although there has been interest in and acknowledgement that palliative care is an important part of the training of patient navigators, there have been no previous studies examining the effects of a patient navigation intervention to improve palliative care outcomes.48
In our study, we have adapted Dr. Freeman’s patient navigator model41–43 to deliver a culturally tailored intervention aimed at improving palliative care outcomes for seriously ill Latinos. We have combined rigorous scientific methods and community engagement from the earliest development to help design and inform the intervention. This study is a pilot randomized controlled trial to assess the feasibility of and explore the effectiveness of the patient navigator intervention to improve palliative care outcomes.
Methods
Participants
Participants were recruited from Denver Health Medical Center (DHMC), the safety net hospital for the city and county of Denver, from May 2010 through September 2011. This safety net hospital serves over 25% of Denver residents, including 43% of the Denver Latino community. The majority of DHMC’s clients live in Denver’s 32 medically underserved neighborhoods (258,769 residents), which are composed disproportionately of minority and poor persons. Patients were screened for study eligibility on the first day following an index hospital admission to the adult general medical service. Patients were eligible if they were 18 years of age or older, self-identified as Latino, spoke either English or Spanish as a primary language, and were appropriate for a palliative approach as determined by the CARING criteria.49,50 The CARING criteria were developed and validated to help identify patients at an index hospitalization who are at higher risk for death in the following year and might benefit from a palliative approach. The CARING criteria comprise the following items: admitted to the hospital with a primary diagnosis of Cancer, Admitted to the hospital two times or more in the past year for a chronic illness, Resident in a nursing home, admitted to the ICU with multi-organ failure, and meeting more than two National Hospice and Palliative Care Guidelines for non-cancer diagnoses. To be eligible for the study, at the time of the index hospitalization, patients had to meet at least one of the CARING criteria. One of the major domains of interest was advance care planning and to participate in that process, one must have decisional capacity. Therefore, patients lacking decisional capacity were excluded. Another important outcome of interest was hospice utilization. In this small pilot, we were concerned that community hospices would not be able to absorb the additional costs and burden of unsponsored care; therefore, we excluded undocumented persons, who do not have a payer source for hospice care. Finally, patients had to have a place of residence within a 20-mile radius of Denver to facilitate home visits by the patient navigator. Patients also were excluded if they were incarcerated or were pregnant.
Recruitment Process
Eligible patients were identified by the co-investigator (L.C.) from the inpatient medicine service at DHMC. The navigator would then approach the patient while the patient was in the hospital. Infrequently, the patient’s treating provider was available and willing to introduce the navigator to the patient and their family members. The navigator used a standard recruitment script that described the study. Patients who wished to participate then completed the informed consent process.
Randomization
Patients were randomized to control group or intervention following a 1:1 assignment post informed consent and collection of baseline pain and sociodemographic data. We used a computer-generated blocked (randomly varying two to six per block) randomization to assign participants into the two groups. The patient navigator was unblinded at the time of group assignment (was not able to view future assignments to prevent selection bias in recruitment). The principal investigator (PI) and other members of the research team remained blinded throughout the study. This study was approved by the Colorado Multiple Institutional Review Board.
Study Groups
All participants (control and intervention) received a packet of written information that included a booklet about advance directives, hospice care, and pain management. The packet also included an advance directive form, developed by Sudore et al.51 for a low health literacy population. All materials were written at a fifth grade reading level and were available in English and Spanish, depending on the patient’s preference. These educational materials also were culturally tailored at both a surface and deep structural level. Surface level tailoring is a strategy to increase the relevance of the topic to a population by using images related to the cultural group. In our study, for example, the photos in the brochures were all Latinos. We also employed deeper structural tailoring, framing and grounding messages in core cultural values. In our pain brochure, when talking about why it is important to have pain well treated, the brochure states “If you have your pain treated, you can care for your family.” Familia is a core Latino cultural value and grounding the importance of pain control with familia frames pain control in a culturally relevant and meaningful way. An interdisciplinary, bicultural community advisory panel helped to select, modify, and adapt the materials used in this study.52
Intervention
In addition to the packet of written materials, patients randomized to the intervention also received home visits from a patient navigator. The patient navigator, a bilingual, bicultural Latina, has a community health background, and completed patient navigator training through the Colorado Patient Navigator Training Program (http://patientnavigatortraining.org). Study-specific training included one-on-one training based on the Education in Palliative and End-of-Life Care (EPEC) modules (http://www.epec.net/), experiential learning with our institution’s inpatient palliative care consult service, home hospice visits, and additional self-study focusing on advance care planning, pain assessment and myths and barriers to pain management, and hospice care. Following the month-long intensive training described above (approximately 200 hours), the navigator was able to demonstrate mastery of the consent process and intervention components, and we began recruitment.
The intervention was designed to include five navigator-initiated home visits for each intervention participant. Each home visit followed a visit guide (a script developed by the PI that serves as a framework for each visit –first visit, second visit, etc. – to ensure that each visit covered similar material) and focused on reviewing the packet of educational materials, addressing barriers to the three study domains of interest –advance care planning, pain management, and hospice utilization. The visits were structured yet flexible. The navigator used advocacy, activation, education, and motivational interviewing to help address barriers to the domains of interest.45 The navigator also was available by phone or to make additional visits if the patient or family requested help. Although we planned for most of the visits to be in the patients’ homes, the navigator was allowed to visit patients in the hospital, at a clinic visit, or other facility if necessary or preferred by the patient or family.
Intervention Tracking
The navigator completed detailed field notes that included careful tracking of contacts and number, length, and content of visits. Investigators (S.M.F. and L.C.) evaluated a random selection of audio-recorded visits (10%) for fidelity to the visit guide and intervention.
Measures
At the time of study enrollment, patients completed the Brief Pain Inventory (BPI)53 enabling responders to rate their current pain, and pain at its worst, least, and average during the past week, location and description of pain, and interference with functional status. Patients also completed a sociodemographic survey including detailed information on their ethnicity, primary language spoken, gender, marital status, and insurance/payer details (e.g. Medicare, Medicaid, private insurance, self-pay, Colorado Indigent Care Program [CICP]). The PI and co-investigator (L.C.), blinded to study group allocation, collected outcome data at 12 months following study enrollment. Outcomes included documentation of advance care planning in the electronic medical record, documentation of a pain management discussion in the medical record, and hospice utilization. Primary outcomes for this pilot were all from secondary data sources, that is, electronic medical record review and hospice records. We relied on secondary data sources to reduce missing follow-up data, concerned that seriously ill patients, especially in the control group, of a socially unstable population, may be difficult to contact months after enrollment.
Statistical Analysis
SAS 9.3© (SAS Institute, Inc., Cary, NC) was used for all analyses. To assess the effectiveness of the randomization, we compared the two groups across participant level variables including age, gender, diagnoses, degree of acculturation (e.g., language spoken in the home), and socioeconomic status. We compared categorical variables using Chi-square tests (or Fisher’s exact tests if cell size < 5) and continuous variables using t-tests (or Wilcoxon tests if distribution was not normal). Hospice utilization in days for decedents was compared using t-tests. For the dichotomous outcome measures (hospice utilization more than seven days, presence of an advance directive in the medical record, documentation of a pain management discussion in the medical record, and outpatient pain medication order), we used Chi-square tests (or Fisher’s exact tests if cell size < 5) to test the intervention effect on the outcome. This study was designed as a feasibility pilot study and not powered to detect efficacy of the intervention or statistical differences in the measured outcomes.
Results
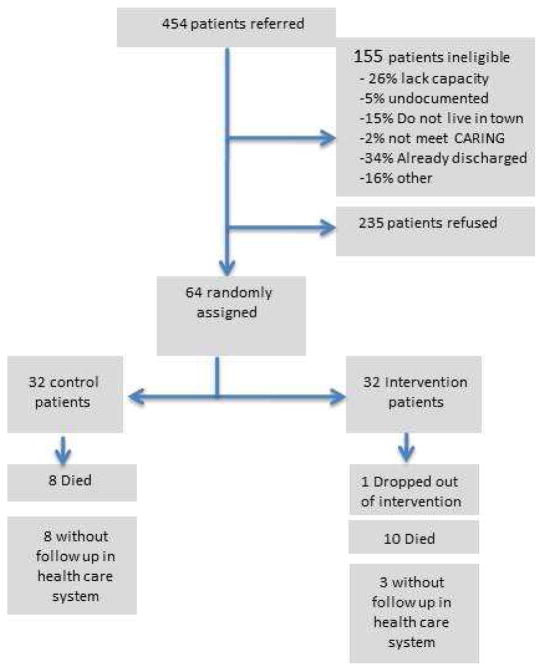
In total, 454 Latino adults who met one of the CARING criteria were referred for study enrollment (Fig. 1). Subsequently, 155 were found not to be eligible for participation for the following reasons: had already been discharged before the navigator could visit, lacked decisional capacity, did not live in Denver, did not appropriately meet CARING criteria, were undocumented, or a small number of other miscellaneous reasons. Of the 299 who were eligible, 235 declined to participate (78%) and 64 consented. The majority of patients who declined to participate stated they did not need any help, that they were not that sick, or were too worried to participate. Consented participants were randomized to either the control (n=32) or intervention group (n= 32).
Figure 1.
Accrual and study flow
As is shown in Table 1, the average participant was 57±13 years old and female (65%). Nearly 30% spoke Spanish as their primary language. Slightly over half had less than a high school education (54%) and the vast majority had an annual income of under $15,000 (85%). No participants had private health care insurance; 90% were receiving discounted care through the CICP, Medicaid, or a combination. The remaining participants had Medicare (10%) or had no payer source (5%). Participants had a wide range of chronic illnesses that included cancer, liver disease, renal failure, and heart and lung disease.
Table 1.
Participants’ Characteristics
| Total (n = 64) | Intervention (n =32) | Control (n =32) | P-value | |
|---|---|---|---|---|
| Age, yrs (mean ± SD) | 57.4±13.5 | 55.4±13.7 | 59.5±13.2 | 0.2 |
| Female gender | 65.6% (42) | 65.6% (21) | 65.6% (21) | 1.0 |
| Married or domestic partner | 26.6% (17) | 40.6% (13) | 12.5% (4) | 0.01 |
| Spanish primary language spoken in the home | 29.7% (19) | 15.6% (10) | 14.1% (9) | 0.78 |
| Less than high school education | 54.0% (34) | 53.1% (17) | 53.1% (17) | 1.0 |
| Annual income < $15,000 | 85.9% (55) | 81.3% (26) | 90.6% (29) | 0.47a |
| Not currently working | 93.8% (60) | 46.9% (30) | 46.9% (30) | 1.0 |
| Medicaid/CICP | 85.9% (55) | 96.9% (24) | 75.0% (31) | 0.01 |
| Medicare (A ± B) | 9.4% (6) | 3.1% (1) | 15.6% (5) | 0.19a |
| CARING criteria: | ||||
| Cancer | 18.8% (12) | 31.3% (10) | 6.3% (2) | 0.01 |
| Admitted to hospital ≥2 times in the past year for chronic illness | 74.6% (47) | 80.7% (25) | 68.8% (22) | 0.27 |
| Resident in a nursing home | 6.3% (4) | 6.3% (2) | 6.3% (2) | 1.0a |
| ICU with multi organ failure | 1.6% (1) | 0 | 3.1% (1) | 1.0a |
| Non-cancer hospice guidelines (≥2) | 57.8% (37) | 50% (16) | 65.6% (21) | 0.2 |
Fisher’s exact test used because cell size < 5.
The sample was fairly balanced between the intervention and control groups for gender, Spanish as first language, and income and education levels. Patients in the intervention group (97% vs. 75%) were more likely to have some form of low income health plan (CICP or Medicaid). Intervention patients were more likely to be married or with a domestic partner (40%) compared with controls (12%). More patients with cancer were randomized to the intervention group (31%) compared with the control group (6%).
Feasibility Outcomes
Participants in the intervention group had a mean of 2.7± 1.9 visits (range 1–5); 81% of intervention participants had at least one visit and 31% completed all five visits. First visits occurred on average 36±21 days following hospital admit date. Average visit time was 91±31 minutes. Visits took place in the home, at the clinic, or in the hospital during the current or subsequent hospitalization. The patients chose the location for the visits based on where they felt most comfortable. The navigator was able to complete the visits over a mean of 5±2 months.
Advance Directive Documentation
Thirty-four percent of the intervention group vs. 13% of the control group (P = 0.15) completed some form of an advance directive (including living wills, MDPOA, or more comprehensive advance directive forms) 12 months post study enrollment. For MDPOA documentation, 40% of intervention patients had a MDPOA form in their medical record vs. 25% of control group participants (P = 0.18). Finally, 25% of intervention participants had the study advance directive form documented in their medical record whereas no (0%) control group patients had one in their medical record (P = 0.005). This form was included in all participants’ educational packets (Table 2).
Table 2.
Palliative Care Outcomes of the Patient Navigator Intervention (N = 64)
| Intervention (n = 32) | Control (n = 32) | P-value | |
|---|---|---|---|
| Any form of advance directive (MDPOA, AD, Living will) | 46.9% (15) | 25.0% (8) | 0.06 |
| Medical Durable Power of Attorney (MDPOA) | 37.5% (12) | 18.8% (6) | 0.1 |
| Apoyo con Cariño advance directive form | 21.9% (7) | 0 | 0.01a |
Fisher’s exact test used because cell size < 5.
Pain Management Discussion Documentation
Fifty-three participants had an outpatient follow-up visit in the Denver health system within 12 months following the enrollment hospitalization. Of the 11 participants who did not have a follow-up visit documented, eight were control patients (25%) and three were in the intervention group (9%) (P = 0.1). Excluding the 11 without outpatient records, 79% (23) of intervention patients vs. 54% (13) of control participants had a discussion about pain management documented in their chart (P = 0.05). A total of 22 patients in the intervention group (76%) compared with 14 control patients (58%) had some kind of pain medication prescribed (P = 0.17) (Table 3).
Table 3.
Pain Management Outcomes for Patients With Outpatient Records Following Index Hospitalization (N = 53)
| Intervention (n =29) | Control (n = 24) | P-value | |
|---|---|---|---|
| Pain management discussion documented in the medical record | 79.3% (23) | 54.2% (13) | 0.05 |
| Outpatient order for pain medication (opioid and non-opioid) | 75.9% (22) | 58.3% (14) | 0.17 |
Hospice Utilization
Eighteen participants died during the 12-month study follow-up period. Of those decedents, seven intervention participants vs. six control participants used some kind of hospice support (P =1.0). Looking at overall length of stay (LOS) in days, we found that the mean hospice LOS was 36.4± 51.6 days for intervention participants vs. 19.7±33.6 days for control patients (P = 0.39). We looked at hospice stays of at least seven days and found that 71% of intervention participants vs. 33% of control patients had a LOS of seven days or more (P =0.15) (Table 4).
Table 4.
Hospice Outcomes for Patients Who Died Within the Follow-Up Period (N =18)
| Intervention (n = 10) | Control (n = 8) | P-value | |
|---|---|---|---|
| Any hospice used | 70%.0 (7) | 75.0% (6) | 1.0 a |
| Mean± SD number of days in hospice | 41.6± 53.4 | 23.0± 35.5 | 0.39 |
| Used hospice ≥ 7 days for the subsample that used some hospice (n = 13) | 71.4% (5) | 33.3% (2) | 0.17 |
Fisher’s exact test used because cell size < 5.
Discussion
This pilot randomized controlled trial demonstrates that a bicultural, bilingual community health worker, trained in a culturally tailored intervention, has the potential to improve palliative care outcomes for seriously ill Latinos. Furthermore, seriously ill patients are willing to participate in a clinical trial of the intervention even though half would be expected to be randomized to a control group. However, the lower enrollment rate suggests that a large sample population of eligible patients would be required to support a fully powered trial of the navigator intervention. We had missing data for 17% (n=11) of the sample who did not have subsequent follow-up clinical encounters within the Denver health system. Future trials would benefit from a combination of secondary data sources and patient-derived outcomes.
The low rate of acceptance of the study is a limitation, as 75% of patients approached declined to participate, which raises concerns about the generalizability of our findings. Working in a busy urban safety net hospital, providers were often too burdened to discuss the study with their patients, leaving the navigator to approach people without an introduction and during the stressful time of an acute hospitalization. When the health care provider did introduce the study, the acceptance/enrollment rates were more than 50%. We also found the language used to introduce the study was critical. The recruitment script was refined throughout the pilot study period to focus on quality of life and avoid introducing terms such as hospice and end-of-life care in the early visits. Finally, the navigator noticed a marked difference in rapport and trust building when visiting in the home versus the hospital setting. An acute hospitalization is likely a time of high stress and we have learned from subsequent trial enrollment that waiting to introduce and enroll patients until discharge is a more effective strategy. In this pilot, we found that patients were able to easily complete the consent process and accompanying surveys. These findings from the pilot have informed recruitment practices in our current American Cancer Society funded trial (RSG-12-0182) of patient navigation where we have achieved enrollment rates of more than 80%.
Patients also received variable “dosing” of the intervention; whereas the average completed three visits, only 31% received all five visits. We developed several strategies to improve visit completion rates. These included communicating through the consenting process and at the randomization contact (for intervention patients only) the importance of completing the five visits within a three-month time frame, calling to confirm visits the day before, and scheduling the subsequent visit at the end of the current visit. These strategies may facilitate an increase in the number of patients who are able to complete all five visits with the navigator. To date, In our current study, of the 40 intervention patients, 33 have completed all five visits (82%) and 32 of these have occurred within three months of enrollment. Patient and family member feedback about the study focused on how grateful they were for the navigator’s help. However, this may be a biased sample as the patients who did not receive the visits may have believed the intervention or visits to be burdensome as they were generally unavailable or unresponsive for follow-up.
We selected a sample size to determine feasibility rather than detect significant differences in outcomes. However, primary outcomes trended towards improvements across all three domains. We found that participants in the intervention arm were more likely to have an advance directive documented in their electronic medical record, even though an advance directive form and educational information on advance directives were provided to all participants in the educational materials. Additionally, there was a trend towards higher rates of any type of advance directive documented in the electronic medical record. Patients who received the navigator intervention were more likely to have a pain discussion documented in their medical record compared with control patients. Finally, data on hospice LOS and hospice utilization of seven days or more are encouraging; the patient navigator intervention has the potential to improve these outcomes. The sample size is too small to draw any definitive conclusions and although the participants were randomized, there were significant baseline differences between groups in diagnosis, marital status, and payer source. Because of the small sample size, we also were unable to adjust for these differences in the analysis. This is a limitation and future trials must account for the potential need for modeling to adjust for randomization imbalances.
Patient navigation has grown dramatically as a field and area of study; however, there remains a paucity of scientifically rigorous methodology within published studies.44,46,54 One of the major strengths of our trial is the use of a randomized controlled design, blinding of the investigators, and selection of objective outcomes of effectiveness. Furthermore, we utilized detailed tracking of the intervention to estimate “dose” of the time and number of visits with the navigator, content of the visits through detailed field notes, and fidelity testing to ensure adherence to visit protocol and scripts. This is necessary to facilitate reproducibility of the intervention in future effectiveness and implementation research.
As a behavioral intervention, by necessity and design, it must remain flexible and responsive to each individual participant. The navigator completed a rigorous training curriculum and utilized the intervention manual; however, the “dosing” and individualized needs and barriers addressed by the navigator varied. The rigorous attention to fidelity and tracking attempted to address this limitation. However, we acknowledge that 19% of the intervention participants did not receive a visit from the patient navigator. This demonstrates the importance of intent-to-treat analysis.
We must be cautious with any conclusions drawn from this small pilot study. Although the outcomes all showed directionality towards improvement in the intervention group, the study was not powered to examine effectiveness. There is a possibility we have detected differences where there were none, a type I error. However, the outcomes were selected a priori and all findings were in the direction towards a benefit from the navigator intervention. Whereas we cannot conclude the intervention was effective in improving palliative care outcomes for seriously ill Latinos, it provides sufficient evidence to justify a larger trial of the intervention.
The field of palliative care faces real challenges in work force shortages in the coming years, with limited specialty-trained palliative care professionals for the growing number of patients living with-life limiting illness.55 Patient navigator interventions offer a promising opportunity to address this shortage. Although navigators do not provide direct care to patients, they educate and activate patients to have their palliative care needs addressed by their primary care providers and treating medical specialists (e.g., oncologists, cardiologists). Promoting primary palliative care allows for sustainability and accessibility in the current health care landscape.56
Conclusions
This trial represents the first scientifically rigorous pilot study of a patient navigator intervention to improve palliative care outcomes. Our findings suggest that the intervention is feasible in an underserved population and may be effective for improving palliative care outcomes. Future studies, powered to detect clinically and statistically significant results will be needed to consider widespread implementation.
Acknowledgments
This study was supported by NIA/Paul Beeson Career Development Award 5K23AG028957-04 (Fischer, PI).
The authors wish to acknowledge Linda M. Martinez who served as the compassionate and dedicated patient navigator for this project.
Footnotes
Disclosures
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and ethnic differences in end-of-life costs: why do minorities cost more than whites? Arch Intern Med. 2009;169:493–501. doi: 10.1001/archinternmed.2008.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. 2009;10:1187–1204. doi: 10.1016/j.jpain.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Portenoy RK, Ugarte C, Fuller I, Haas G. Population-based survey of pain in the United States: differences among white, African American, and Hispanic subjects. J Pain. 2004;5:317–328. doi: 10.1016/j.jpain.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Anderson KO, Richman SP, Hurley J, et al. Cancer pain management among underserved minority outpatients: perceived needs and barriers to optimal control. Cancer. 2002;94:2295–2304. doi: 10.1002/cncr.10414. [DOI] [PubMed] [Google Scholar]
- 5.Lewis ET, Combs A, Trafton JA. Reasons for under-use of prescribed opioid medications by patients in pain. Pain Med. 2010;11:861–871. doi: 10.1111/j.1526-4637.2010.00868.x. [DOI] [PubMed] [Google Scholar]
- 6.Cleeland CS, Gonin R, Baez L, Loehrer P, Pandya KJ. Pain and treatment of pain in minoritiy patients with cancer. Ann Intern Med. 1997;127:813–816. doi: 10.7326/0003-4819-127-9-199711010-00006. [DOI] [PubMed] [Google Scholar]
- 7.Anderson KO, Mendoza TR, Valero V, et al. Minority cancer patients and their providers: pain management attitudes and practice. Cancer. 2000;88:1929–1938. [PubMed] [Google Scholar]
- 8.Cohen LL. Racial/ethnic disparities in hospice care: a systematic review. J Palliat Med. 2008;11:763–768. doi: 10.1089/jpm.2007.0216. [DOI] [PubMed] [Google Scholar]
- 9.Smith AK, Earle CC, McCarthy EP. Racial and ethnic differences in end-of-life care in fee-for-service Medicare beneficiaries with advanced cancer. J Am Geriatr Soc. 2009;57:153–158. doi: 10.1111/j.1532-5415.2008.02081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Born W, Greiner KA, Sylvia E, Butler J, Ahluwalia JS. Knowledge, attitudes, and beliefs about end-of-life care among inner-city African Americans and Latinos. J Palliat Med. 2004;7:247–256. doi: 10.1089/109662104773709369. [DOI] [PubMed] [Google Scholar]
- 11.Duffy SA, Jackson FC, Schim SM, Ronis DL, Fowler KE. Racial/ethnic preferences, sex preferences, and perceived discrimination related to end-of-life care. J Am Geriatr Soc. 2006;54:150–157. doi: 10.1111/j.1532-5415.2005.00526.x. [DOI] [PubMed] [Google Scholar]
- 12.Smith AK, McCarthy EP, Paulk E, et al. Racial and ethnic differences in advance care planning among patients with cancer: impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol. 2008;26:4131–4137. doi: 10.1200/JCO.2007.14.8452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tellez-Giron P. Providing culturally sensitive end-of-life care for the Latino/a community. WMJ. 2007;106:402–406. [PubMed] [Google Scholar]
- 14.Taylor T, Serrano E, Anderson J, Kendall P. Knowledge, skills, and behavior improvements on peer educators and low-income Hispanic participants after a stage of change-based bilingual nutrition education program. J Community Health. 2000;25:241–262. doi: 10.1023/a:1005160216289. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine. Unequal treatment. Washington, DC: National Academies Press; 2003. [Google Scholar]
- 16.Freiere P. Pedagogy of the oppressed. New York: Continuum; 1930. [Google Scholar]
- 17.Swider SM. Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs. 2002;19:11–20. doi: 10.1046/j.1525-1446.2002.19003.x. [DOI] [PubMed] [Google Scholar]
- 18.Romero LJ, Lindeman RD, Koehler KM, Allen A. Influence of ethnicity on advance directives and end-of-life decisions [letter] JAMA. 1997;277:298. [PubMed] [Google Scholar]
- 19.Morrison RS, Morrison EW, Glickman DF. Physician reluctance to discuss advance directives. An empiric investigation of potential barriers. Arch Intern Med. 1994;154:2311–2318. [PubMed] [Google Scholar]
- 20.McKinley ED, Garrett JM, Evans AT, Danis M. Differences in end-of-life decision making among black and white ambulatory cancer patients. J Gen Intern Med. 1996;11:651–656. doi: 10.1007/BF02600155. [DOI] [PubMed] [Google Scholar]
- 21.Shepardson LB, Younger SJ, Speroff J, et al. Variation in the use of do-not-resuscitate orders for patients with a stroke. Arch Intern Med. 1997;157:1841–1847. [PubMed] [Google Scholar]
- 22.Wenger NS, Pearson ML, Desmond KA, et al. Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race,a nd functional impairment. Arch Intern Med. 1995;155:2056–2062. [PubMed] [Google Scholar]
- 23.Garrett JM, Harris RP, Norburn JK, Patrick DL, Danis M. Life sustaining treatments during terminal illness:who wants what? J Gen Intern Med. 1993;8:361–368. doi: 10.1007/BF02600073. [DOI] [PubMed] [Google Scholar]
- 24.Gramelspacher GP, Zhou XH, Hanna MP, Tierney WM. Preferences of physicians and thier patients for end-of-life care. J Gen Intern Med. 1997;12:346–351. doi: 10.1046/j.1525-1497.1997.00058.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haas JS, Weissman JS, Cleary PD, et al. Discussion preferences for life-sustaining care by persons with AIDS. Arch Intern Med. 1993;153:1241–1248. [PubMed] [Google Scholar]
- 26.Weiss SC, Emanuel LL, Fairclough DL, Emanuel EJ. Understanding the experience of pain in terminally ill patients. Lancet. 2001;357:1311–1315. doi: 10.1016/S0140-6736(00)04515-3. [DOI] [PubMed] [Google Scholar]
- 27.McNeill JA, Reynolds J, Ney ML. Unequal quality of cancer pain management: disparity in perceived control and proposed solutions. Oncol Nurs Forum. 2007;34:1121–1128. doi: 10.1188/07.ONF.1121-1128. [DOI] [PubMed] [Google Scholar]
- 28.American Geriatrics Society Panel on Chronic Pain in Older Persons. Clinical practice guideline: the management of chronic pain in older persons. J Am Geriatr Soc. 1998;46:635–651. doi: 10.1111/j.1532-5415.1998.tb01084.x. [DOI] [PubMed] [Google Scholar]
- 29.Chiauzzi E, Black RA, Frayjo K, et al. Health care provider perceptions of pain treatment in Hispanic patients. Pain Pract. 2011;11:267–277. doi: 10.1111/j.1533-2500.2010.00421.x. [DOI] [PubMed] [Google Scholar]
- 30.Morrison RS, Wallenstein S, Natale DK, Senzel RS, Huang LL. “We don’t carry that”-failure of pharmacies in predominantly nonwhite neighborhoods to stock opioid analgesics. N Engl J Med. 2000;342:1023–1026. doi: 10.1056/NEJM200004063421406. [DOI] [PubMed] [Google Scholar]
- 31.Ng B, Dimsdale JE, Shragg GP, Deutsch R. Ethnic differences in analgesic consumption for post-operative pain. Psychosom Med. 1996;58:125–129. doi: 10.1097/00006842-199603000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Montague L, Green CR. Cancer and breakthrough pain’s impact on a diverse population. Pain Med. 2009;10:549–561. doi: 10.1111/j.1526-4637.2009.00564.x. [DOI] [PubMed] [Google Scholar]
- 33.Green CR, Montague L, Hart-Johnson TA. Consistent and breakthrough pain in diverse advanced cancer patients: a longitudinal examination. J Pain Symptom Manage. 2009;37:831–847. doi: 10.1016/j.jpainsymman.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 34.Im EO, Chee W, Guevara E, et al. Gender and ethnic differences in cancer pain experience: a multiethnic survey in the United States. Nurs Res. 2007;56:296–306. doi: 10.1097/01.NNR.0000289502.45284.b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jayadevappa R, Johnson JC, Chhatre S, Wein AJ, Malkowicz SB. Ethnic variation in return to baseline values of patient-reported outcomes in older prostate cancer patients. Cancer. 2007;109:2229–2238. doi: 10.1002/cncr.22675. [DOI] [PubMed] [Google Scholar]
- 36.Castel LD, Saville BR, Depuy V, et al. Racial differences in pain during 1 year among women with metastatic breast cancer: a hazards analysis of interval-censored data. Cancer. 2008;112:162–170. doi: 10.1002/cncr.23133. [DOI] [PubMed] [Google Scholar]
- 37.National Hospice and Palliative Care Organization. NHPCO facts and figures. Alexandria, VA: NHPCO; 2002. [Google Scholar]
- 38.Greiner KA, Perera S, Ahluwalia JS. Hospice usage by minorities in the last year of life:results from the national mortality feedback survey. J Am Geriatr Soc. 2003;51:970–978. doi: 10.1046/j.1365-2389.2003.51310.x. [DOI] [PubMed] [Google Scholar]
- 39.Gordon AK. Deterrents to access and service for blacks and Hispanics: the Medicare Hospice Benefit, healthcare utilization, and cultural barriers. Hosp J. 1995;10:65–83. doi: 10.1080/0742-969x.1995.11882792. [DOI] [PubMed] [Google Scholar]
- 40.Freeman HP, Chu KC. Determinants of cancer disparities: barriers to cancer screening, diagnosis, and treatment. Surg Oncol Clin N Am. 2005;14:655–669. v. doi: 10.1016/j.soc.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 41.Freeman HP. Patient navigation: a community centered approach to reducing cancer mortality. J Cancer Educ. 2006;21:S11–S14. doi: 10.1207/s15430154jce2101s_4. [DOI] [PubMed] [Google Scholar]
- 42.Freeman HP. Patient navigation: a community based strategy to reduce cancer disparities. J Urban Health. 2006;83:139–141. doi: 10.1007/s11524-006-9030-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Freeman HP, Muth BJ, Kerner JF. Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Pract. 1995;3:19–30. [PubMed] [Google Scholar]
- 44.Paskett ED, Harrop JP, Wells KJ. Patient navigation: an update on the state of the science. CA Cancer J Clin. 2011;61:237–249. doi: 10.3322/caac.20111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Calhoun EA, Whitley EM, Esparza A, et al. A national patient navigator training program. Health Promot Pract. 2010;11:205–215. doi: 10.1177/1524839908323521. [DOI] [PubMed] [Google Scholar]
- 46.Wells KJ, Battaglia TA, Dudley DJ, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113:1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Steinberg ML, Fremont A, Khan DC, et al. Lay patient navigator program implementation for equal access to cancer care and clinical trials: essential steps and initial challenges. Cancer. 2006;107:2669–2677. doi: 10.1002/cncr.22319. [DOI] [PubMed] [Google Scholar]
- 48.Fischer SM, Sauaia A, Kutner JS. Patient navigation: a culturally competent strategy to address disparities in palliative care. J Palliat Med. 2007;10:1023–1028. doi: 10.1089/jpm.2007.0070. [DOI] [PubMed] [Google Scholar]
- 49.Fischer SM, Gozansky W, Sauaia A, et al. A practical tool to identify patients who may benefit from a palliative approach: the CARING criteria. J Pain Symptom Manage. 2005;31:285–292. doi: 10.1016/j.jpainsymman.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 50.Youngwerth J, Min SJ, Statland B, Allyn R, Fischer S. Caring about prognosis: a validation study of the CARING criteria to identify hospitalized patients at high risk for death at 1 year. J Hosp Med. 2013;8:696–701. doi: 10.1002/jhm.2107. [DOI] [PubMed] [Google Scholar]
- 51.Sudore RL, Landefeld CS, Barnes DE, et al. An advance directive redesigned to meet the literacy level of most adults: a randomized trial. Patient Educ Couns. 2007;69:165–195. doi: 10.1016/j.pec.2007.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fischer SM, Sauaia A, Kutner JS. Patient navigation: a culturally competent strategy to address disparities in palliative care. J Palliat Med. 2007;10:1023–1028. doi: 10.1089/jpm.2007.0070. [DOI] [PubMed] [Google Scholar]
- 53.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129–138. [PubMed] [Google Scholar]
- 54.Guadagnolo BA, Dohan D, Raich P. Metrics for evaluating patient navigation during cancer diagnosis and treatment: crafting a policy-relevant research agenda for patient navigation in cancer care. Cancer. 2011;117:3565–3574. doi: 10.1002/cncr.26269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lupu D. Estimate of current hospice and palliative medicine physician workforce shortage. J Pain Symptom Manage. 2010;40:899–911. doi: 10.1016/j.jpainsymman.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 56.Quill TE, Abernethy AP. Generalist plus specialist palliative care--creating a more sustainable model. N Engl J Med. 2013;368:1173–1175. doi: 10.1056/NEJMp1215620. [DOI] [PubMed] [Google Scholar]