Abstract
Purpose:
To report the clinical outcomes with 24-month follow-up of transepithelial cross-linking using a combination of a d-alpha-tocopheryl polyethylene-glycol 1000 succinate (vitamin E-TPGS)-enhanced riboflavin solution and abbreviated low fluence UV-A treatment.
Methods:
In a nonrandomized clinical trial, 25 corneas of 19 patients with topographically proven, progressive, mild to moderate keratoconus over the previous 6 months were cross-linked, and all patients were examined at 1, 3, 6, 12, and 24 months. The treatments were performed using a patented solution of riboflavin and vitamin E-TPGS, topically applied for 15 minutes, followed by two 5-minute UV-A treatments with separate doses both at fluence below 3 mW/cm2 that were based on preoperative central pachymetry.
Results:
During the 6-month pretreatment observation, the average Kmax increased by +1.99 ± 0.29 D (diopter). Postoperatively, the average Kmax decreased, changing by −0.55 ± 0.94 D, by −0.88 ± 1.02 D and by −1.01 ± 1.22 D at 6, 12, and 24 months. Postoperatively, Kmax decreased in 19, 20, and 20 of the 25 eyes at 6 months, 12 months, and 24 months, respectively. Refractive cylinder was decreased by 3 months postoperatively and afterward, changing by −1.35 ± 0.69 D at 24 months. Best spectacle-corrected visual acuity (BSCVA) improved at 6, 12, and 24 months, including an improvement of −0.19 ± 0.13 logarithm of the minimum angle of resolution units at 24 months. There was no reduction in endothelial cell count. No corneal abrasions occurred, and no bandage contact lenses or prescription analgesics were used during postoperative recovery.
Conclusions:
Transepithelial cross-linking using the riboflavin-vitamin E solution and brief, low-dose, pachymetry-dependent UV-A treatment safely stopped keratoconus progression.
Key Words: corneal cross-linking, transepithelial cross-linking, keratoconus
Corneal collagen cross-linking (CXL) was first described in 1998 by Spoerl et al1 with first clinical results reported by Wollensak et al.2,3 Long-term treatment outcomes in keratoconus have been reported4–7 with results now out to 10 years postoperatively.8 Corneal curvature results have been reported using Scheimpflug photography9 and the Orbscan II (Bausch & Lomb, Bridgewater, NJ).10 The Dresden protocol, a current cross-linking standard treatment,2 involves the removal of corneal epithelium (epi-off technique) followed by 30 minutes of riboflavin corneal soaking and 30 minutes of UV-A irradiation at 3 mW/cm2.
Cross-linking with epithelium removed, although effective, is associated with postoperative discomfort, the risk of sterile corneal infiltrates, the typical use of a bandage contact lens for pain relief, and the risk of corneal ulcer formation.11–13 Attempted riboflavin/UVA cross-linking without removing the epithelium, so-called “transepithelial cross-linking” (TE-CXL), has not been effective because riboflavin barely passes any concentration into the corneal stroma.
Cross-linking using riboflavin with added chemical permeation enhancers to partially breakup the corneal epithelium to increase riboflavin penetration has met with only limited success.14,15 TE-CXL with riboflavin enhanced with trometamol (TRIS) and EDTA failed to stabilize keratoconus in a 24-month study.16 But adding an iontophoresis technique to the TRIS/EDTA-augmented riboflavin solution during the presoak period and using 10 mW/cm2 fluence UV-A irradiation have produced encouraging early cross-linking results.17 The iontophoresis technique still requires the use of a postoperative contact lens, with its attendant risks, and the use of analgesics.
We report in this TE-CXL clinical study the use of a patented riboflavin solution18 that is enhanced with d-alpha-tocopheryl polyethylene-glycol 1000 succinate (vitamin E-TPGS). Ostacolo et al19 reported in detail in vitro testing in which effective stromal concentrations of riboflavin occurred after just 15 minutes of topical application through intact epithelium. In the technique here reported, the presoak period was 15 minutes, and the UV-A treatment to the intact cornea was just 10 minutes with a fluence level at less than half the UV-A fluence of the original Dresden protocol. The precorneal riboflavin film was rinsed away before UV-A treatment. The results for a group of 25 consecutive eyes of 19 patients are reported with 2-year follow-up.
MATERIALS AND METHODS
This clinical, prospective, nonrandomized study was conducted according to the ethical standards of the Declaration of Helsinki (revised in 2000). The patients were informed about the nature and the aim of experimentation, and they signed an informed consent. Institutional Review Board (IRB)/Ethics Committee approval was obtained (authorization no. 1269).
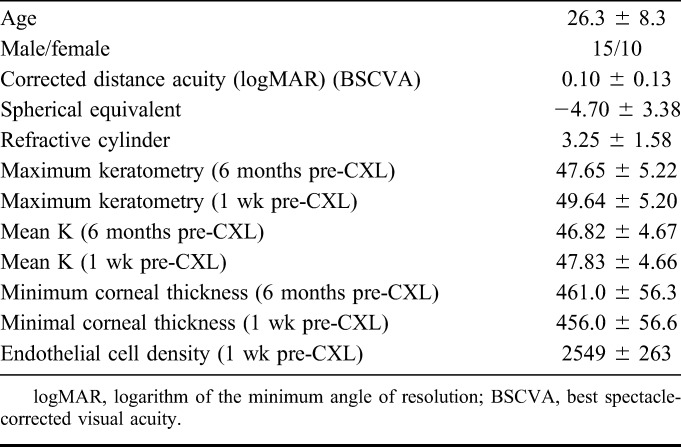
Nineteen patients (11 male, 8 female), were enrolled for treatment, for a total of 25 eyes (13 right eyes, 12 left eyes, 15 eyes of males, 10 eyes of females). The mean patient age was 26.7 ± 7.4 years. Patient demographics along with mean clinical parameters are reported in Table 1.
TABLE 1.
Patient Demographics (n = 25)
All eyes were affected by keratoconus and were selected for treatment because of proven Orbscan IIz topographic progression during the 6 months before treatment based on an increase in Kmax of over 1.5 D (diopter). Exclusion criteria included any of the following (1) age below 16 years or above 45 years, (2) evidence of clinical and instrumental stability of keratoconus in the last 6 months, (3) thinnest corneal point less than 350 μm, (4) corrected visual acuity worse than 0.5, (5) evidence of subepithelial or mid-anterior stromal scars or opacities, (6) evidence of marked Vogt striae, (7) associated corneal diseases, (8) previous ocular surgical procedures, (9) wearing of contact lenses in the 4 weeks before examination, (10) pregnancy or breast feeding, and (11) poor compliance.
Clinical observations were recorded and are reported for 6 months before and 1 week before TE-CXL and at 1, 3, 6, 12, and 24 months after treatment.
Examinations included the following: uncorrected visual acuity and best spectacle-corrected distance visual acuity, measured in mesopic condition with a logarithm of the minimum angle of resolution chart, refraction, Orbscan IIz corneal topography with measured sim K at the 3 mm optical zone—Kmax, Kmin, Kmean, slit-lamp examination of the anterior and posterior segment, Goldmann tonometry, endothelial corneal cell count (Tomey EM-3000; Tomey Corp, Japan), and central corneal thickness measured with ultrasound (Quantel Medical, Clermont-Ferrand, France). Three days before treatment, 1 drop of preservative-free norfloxacin 0.3% solution was instilled into the operative eye every 6 hours. Twenty minutes before treatment, the anesthetic oxybuprocaine hydrochloride 0.2% (Minims—Bausch & Lomb, London), a single-use, preservative-free, sterile topical solution, was instilled at the rate of 2 drops every 5 minutes. One drop of norfloxacin 0.3% (Naflox 0.3%; Farmigea, Italy) single-use, preservative-free, sterile topical solution was instilled every 3 minutes for antibiotic prophylaxis, and 2 drops of pilocarpine 1% (pilocarpine hydrochloride 1%; Allergan, Dublin, Ireland) were instilled.
Periocular skin was then disinfected with povidone iodine 10% solution. For the corneal presoaking, a Landers vitrectomy silicone ring (12 mm diameter, 3 mm height Ocular Instruments Inc., Bellevue, WA) was placed on the corneoscleral limbus (Fig. 1) to retain the riboflavin solution, composed of riboflavin-dextran 0.1 g/100 g and vitamin E-TPGS 500 mg/100 mL, (IROS, Naples, Italy). Drops of this solution were delivered into the silicone ring to completely cover the cornea. Filled with solution, the ring was maintained in place for 15 minutes. Further drops were added as necessary to maintain corneal coverage with the solution. After the corneal presoak, a slit-lamp examination was then performed to observe the complete yellow dying of corneal tissue and the greenish Tyndall effect in the anterior chamber with a blue filter, indicating adequate passage of the riboflavin solution.
FIGURE 1.

Silicone ring during corneal presoak.
The power of the emitter used to irradiate the corneas (Vega CBM X-Linker; CSO, Italy) was lowered from the usual 3 mW/cm2 fluence with partially absorbing UV-filters (Knight Optical LTD, United Kingdom), to achieve a customized-delivered power, according to the nomogram from our mathematical model described by Barbaro et al.20 That nomogram specifies a UV-A fluence that is pachymetry dependent and at a level lower than that specified in the Dresden protocol. The intraoperative UV fluence measurements were performed with a LaserMateQ, (Coherent Inc, Santa Clara, CA). The treatment diameter was 8 mm at a distance of 5 cm from the corneal apex. During the first 5 minutes, the average UV-A fluence applied was 1.67 ± 0.08 mW/cm2; during the second 5 minutes, the average UV-A fluence applied was 1.45 ± 0.08 mW/cm2. There was no time break between the first UV-A treatment and the second treatment except for the time necessary to change the UV-A fluence level.
No more riboflavin solution was applied during the UV-A exposure. Rather, the corneal surface was washed with balanced salt solution to remove the superficial riboflavin film before irradiation. Drops of balanced salt solution were delivered onto the corneal surface during UV exposure to maintain adequate moisture. Norfloxacin 0.3% eye drops were administered at the end of the treatment.
The patients returned home with topical antibiotic and lubricant therapy (norfloxacin 0.3% and hyaluronate 0.15% eye drops every 6 hours), and these drops were used just until the following day. No analgesics were prescribed. There was no use of a bandage contact lens postoperatively.
RESULTS
Patient discomfort did not require the use of prescription pain relievers. There were no corneal abrasions. We noticed 1 case of transient corneal haze and 2 cases of transient stromal edema; these were managed with topical corticosteroid therapy, with complete clinical resolution after a few weeks. Mild epithelial edema was sometimes present soon after the treatment but disappeared in all cases within a few days. The clinical outcomes of the TE-CXL treatment are reported in Table 2.
TABLE 2.
Clinical Outcomes of Transepithelial Corneal Collagen Cross-linking With Riboflavin–Vitamin E-TPGS
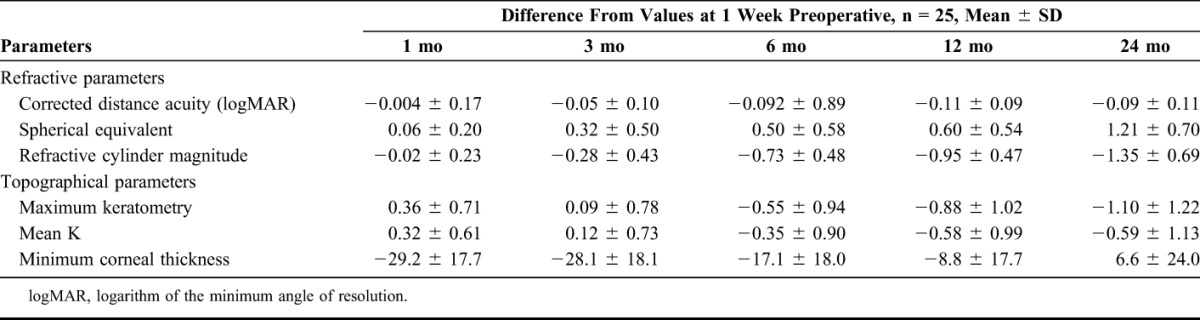
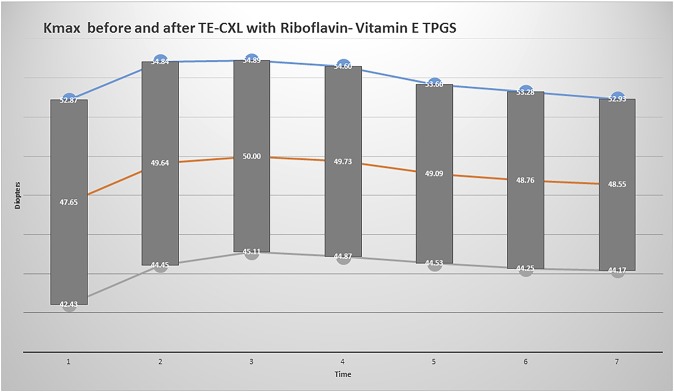
A statistically significant improvement of corneal, refractive, and visual acuity parameters was evident after treatments (P < 0.05 calculated with the Student t test, using the pretreatment values as reference) in best spectacle-corrected visual acuity at 6, 12, and 24 months (P = 0.01, P < 0.01, and P = 0.02, respectively) and in refractive cylinder at 12 and 24 months (P = 0.03, P < 0.01, and P = 0.02, respectively), compared with pretreatment values. There was also a statistically significant decrease of the Kmean at 12 and 24 months compared with pretreatment values. There was stabilization of Kmax. During the 6-month pretreatment observation, all 25 eyes had keratoconus progression with increased Kmax. The average pretreatment Kmax increase was 1.99 ± 0.29 D. After TE-CXL treatment, Kmax decreased compared with the 1-week preoperative value in 19, 20, and 20 of the 25 eyes at 6 months, 12 months, and 24 months (P = 0.04, 0.03, and 0.03, respectively). A graph showing the behavior of Kmax is depicted in Figure 2.
FIGURE 2.
Average Kmax value ± 1 SD over time 6 months and 1 week before corneal cross-linking and then at follow-up examinations at 1 month, 3 months, 6 months, 1 year, and 2 years postoperatively.
A stabilization of corneal and refractive parameters was observed in all cases. Average best spectacle-corrected visual acuity was 0.79 at 1 week preoperatively, 0.79 at 1 month postoperatively (P = 0.91), and 0.97 (P = 0.02) at 2 years postoperatively. The average preoperative endothelial cell count was 2549 ± 263; at 2 years postoperatively it was 2548 ± 270 (P = 0.97). Average refractive cylinder was reduced (P < 0.01) from a preoperative value of 3.25 ± 1.58 D to 2-year postoperative value of 1.90 ± 1.51 D. Spherical equivalent decreased (P < 0.01) from −4.70 ± 3.38 D preoperatively to −3.50 ± 3.10 D at 2 years postoperatively. Kmax averaged 47.6 ± 5.2 D at 6 months preoperatively, progressed to 49.6 ± 5.2 D at 1 week postoperatively, and was 48.5 ± 4.4 D at 2 years postoperatively (P = 0.03).
Average central corneal thickness, 456 ± 56.6 μm at 1 week preoperative, decreased to a minimum of 427.9 ± 54.9 μm at 3 months postoperative and increased to 462.6 ± 46.8 μm at 24 months postoperatively (P = 0.61). Further pachymetry data appear in Table 2.
Intraocular pressure was unchanged (P = 0.808) at 1 year postoperatively (15.6 ± 1.6 mm Hg) as compared with preoperative levels (15.6 ± 2.0 mm Hg).
DISCUSSION
The results of this clinical trial are encouraging, considering that clinical stabilization of keratoconus progression was obtained in all cases and lasted for 24 months without remarkable side effects.
The treatment yielded significant improvement in corneal topography and visual acuity although the study involved relatively mild cases of keratoconus. Generally, cross-linking induces less effect in cases of mild keratoconus than in the more advanced cases.21 The eyes treated in this study were topographically proven cases of keratoconus, but at a much milder stage (Average preoperative Kmax = 49.64 D) when compared with more typical cross-linking study populations reported, such as Caporossi et al4 (average preoperative Kmax = 51.72 D), Coskunseven5 (Average preoperative Kmax = 54.02 D), Raiskup et al8 (Average preoperative Kmax = 53.2 D), and Vinciguerra et al17 (Average preoperative Kmax = 59.02 D). We look forward to further testing of this new technique in more advanced keratoconus cases.
In contrast to the Dresden protocol, in this study, the excess of riboflavin solution, derived from the corneal presoaking, was washed off before UV-A irradiation, thus avoiding superficial UV-A shielding. In this way, the UV-A fluence could be reduced almost to 1.5 mW/cm2, maintaining efficacy. This approach was suggested by our in vitro studies and is currently submitted for publication. The same studies revealed that the endothelial shielding effect of intracorneal riboflavin rapidly fades, with time, during UV-A irradiation, at a typical rate. Thus, lower UV-A fluence during the second 5-minute treatment period was used.
The UV-A fluence was also modulated on the average corneal thickness determined by pachymetry measured 1 week preoperatively. In this way, the UV-A rays reaching the endothelium were more easily maintained below the endothelial toxicity levels as described by Wollensak.22
It must be also considered how this approach makes the cross-linking technique more reproducible in comparison with standard techniques, where riboflavin is continually placed during UV-A irradiation. The periodic application of undefined amounts of riboflavin during treatments, in fact, could be responsible for a different superficial UV-A filtering and, finally, for a different efficacy.
Total treatment time was reduced to 25 minutes (15 minutes of presoak and 10 minutes of UV-A treatment) versus 60 minutes (30 minutes of presoak and 30 minutes of UV-A treatment) in the Dresden protocol, and the decreased power of UV-A irradiation led to rapid recovery of corneal epithelium with no detectable damage to the corneal endothelium.
The total applied UV-A energy over the treatment period in this study was approximately 1.5 mW/cm2 for 10 minutes or only 0.9 J/cm2 in our clinical trial. This compares with 5.4 J/cm2 in the Dresden protocol. We believe that, in addition to the increased efficiency of light transmission to the cornea in our study achieved by eliminating the precornea riboflavin film, it is likely that riboflavin entered the cornea more efficiently because of the use of the Landers vitrectomy silicone ring. That increased riboflavin penetration achieved by continuous soaking was studied and reported by Schumacher et al.23
In our study, patients were prudently treated with antibiotic drops before treatment because the chance of corneal epithelial breaks was unpredictable. Based on the experience gained during this study and on the here reported absence of epithelial damage, we would now eliminate preoperative topical antibiotic treatment.
Importantly, keratoconus stabilization with cross-linking has been achieved in this study without removal or disturbance of the corneal epithelium. This has led to a more rapid and comfortable visual recovery with lower risk of complications.
The results obtained are further encouraging in light of the evidence that inadequate cross-linking effect can be augmented by further treatment.24 Thus, it becomes increasingly important to produce a cross-linking treatment characterized by minimal risk and maximal compliance.
The correct diagnosis of keratoconus progression depends on the reproducibility of topographic measurements. Menassa et al25 found that the variance in Kmax measurements in normal subjects, measured using the Orbscan II, was equal to that obtained by the Scheimpflug system of the Galilei topographer. Nuñez et al26 found that the Orbscan II had less variance in determining the point of maximal corneal elevation than the Pentacam. Kim and Joo27 studied keratoconus patients with the Orbscan every 6 months, assessing as nonprogressive the changes in average keratometry within +0.15 ± 0.15 D per 6-month period. Epstein et al28 found that the 95% confidence level of true change in maximal anterior corneal curvature, Kmax, based on single measurements at each session was 1.51 D using the Pentacam HR. Based on these topographer reproducibility findings, a conservative estimate of the 95% confidence level of keratoconus progression using the Orbscan II could be set at 1.51 D, that of the Pentacam HR, because the articles cited here tended to indicate that the Orbscan II is as reproducible as Scheimpflug topography. Hence, all 25 eyes in our study reached the 95% confidence level of true keratoconus progression before treatment and none reached 95% confidence of further progression at 2 years postoperatively. In fact, 20 of the 25 eyes in the study showed a decrease in Kmax at 2 years postoperatively as compared with the 1 week preoperative Kmax value.
The statistical power of our experimental model was challenged by a matched, paired Student t test. We took the data from the left eye of each patient who had 2 eyes cross-linked and the data from each patient who had only 1 eye cross-linked. The population was composed of 19 patients. The null hypothesis was that the proposed cross-linking treatment was ineffective, not determining a stop in Kmax increase. The post hoc power of our model to correctly reject the null hypothesis with 95% confidence, 19 independent variables and average decreases in measured Kmax of 0.8816 at 1 year and 1.1395 at 2 years, is 90.25% and 95.3%, respectively.
One shortcoming of the present clinical study is the lack of a placebo group. Nevertheless, other important cross-linking clinical studies in the published literature, such as those by Caporossi et al16 and Vinciguerra et al,17 have not included a placebo group.
A prospective randomized, double masked, placebo-controlled clinical trial of cross-linking using riboflavin–vitamin E-TPGS under the US Food and Drug Administration monitoring is in progress. The Food and Drug Administration-monitored clinical trial is in 2 parts. The first study is to test the effectiveness of TE-CXL with riboflavin–vitamin E-TPGS with presoaking times and UV-A exposure times equal to those of the Dresden protocol. The second study is to test the effect of shortened UV-A exposure times and presoaking times as described in this article.
Footnotes
The work described here was entirely self-funded by I.R.O.S.
R. L. Epstein has received consultation fees from I.R.O.S. in the past, although not for the preparation of this article. C. Caruso and S. Troisi are owners of patent EP 2459 186B1 concerning the vitamin E-TPGS–enhanced riboflavin solution used in this work. The remaining authors have no conflicts of interest to disclose.
REFERENCES
- 1.Spoerl E, Huhle M, Seiler T. Induction of cross-links in corneal tissue. Exp Eye Res. 1998;66:97–103. [DOI] [PubMed] [Google Scholar]
- 2.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen cross-linking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–627. [DOI] [PubMed] [Google Scholar]
- 3.Wollensak G, Spörl E, Seiler T. Treatment of keratoconus by collagen cross linking. Ophthalmologe. 2003;100:44–49. [DOI] [PubMed] [Google Scholar]
- 4.Caporossi A, Mazzotta C, Baiocchi S, et al. Long-term results of riboflavin ultraviolet-A corneal collagen cross-linking for keratoconus in Italy: the Siena eye cross study. Am J Ophthalmol. 2010;149:585–593. [DOI] [PubMed] [Google Scholar]
- 5.Coskunseven E, Jankov MR, II, Hafezi F. Contralateral eye study of corneal collagen cross-linking with riboflavin and UVA irradiation in patients with keratoconus. J Refract Surg. 2009;25:371–376. [DOI] [PubMed] [Google Scholar]
- 6.Vinciguerra P, Albè E, Trazza S, et al. Intraoperative and postoperative effects of corneal collagen cross-linking on progressive keratoconus. Arch Ophthalmol. 2009;127:1258–1265. [DOI] [PubMed] [Google Scholar]
- 7.Vinciguerra R, Romano MR, Camesasca FI, et al. Corneal cross-linking as a treatment for keratoconus: four-year morphologic and clinical outcomes with respect to patient age. Ophthalmology. 2013;120:908–916. [DOI] [PubMed] [Google Scholar]
- 8.Raiskup F, Theuring A, Pillunat LE, et al. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. J Cataract Refract Surg. 2015;41:41–46. [DOI] [PubMed] [Google Scholar]
- 9.Koller T, Iseli HP, Hafezi F, et al. Scheimpflug imaging of corneas after collagen cross-linking. Cornea. 2009;28:505–510. [DOI] [PubMed] [Google Scholar]
- 10.Tu KL, Aslanides IM. Orbscan II anterior elevation changes following corneal collagen cross-linking treatment for keratoconus. J Refract Surg. 2009;25:715–722. [DOI] [PubMed] [Google Scholar]
- 11.Goldich Y, Marcovich AL, Barkana Y, et al. Safety of corneal collagen cross-linking with UV-A and riboflavin in progressive keratoconus. Cornea. 2010;29:409–411. [DOI] [PubMed] [Google Scholar]
- 12.Spoerl E, Mrochen M, Sliney D, et al. Safety of UVA-riboflavin cross-linking of the cornea. Cornea. 2007;26:385–389. [DOI] [PubMed] [Google Scholar]
- 13.Dhawan S, Rao K, Natrajan S. Complications of corneal collagen cross-linking. J Ophthalmol. 2011;2011:869015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kissner A, Spoerl E, Jung R, et al. Pharmacological modification of the epithelial permeability by benzalkonium chloride in UVA/Riboflavin corneal collagen cross-linking. Curr Eye Res. 2010;35:715–721. [DOI] [PubMed] [Google Scholar]
- 15.Leccisotti A, Islam T. Transepithelial corneal collagen cross-linking in keratoconus. J Refract Surg. 2010;26:942–948. [DOI] [PubMed] [Google Scholar]
- 16.Caporossi A, Mazzotta C, Paradiso AL, et al. Transepithelial corneal collagen crosslinking for progressive keratoconus: 24-month clinical results. J Cataract Refract Surg. 2013;39:1157–1163. [DOI] [PubMed] [Google Scholar]
- 17.Vinciguerra P, Randleman JB, Romano V, et al. Transepithelial iontophoresis corneal collagen cross-linking for progressive keratoconus: initial clinical outcomes. J Refract Surg. 2014;30:746–753. [DOI] [PubMed] [Google Scholar]
- 18.Caruso C, Troisi S: U.S. patent 9192594 pending for publication November 24, 2015; E.P 2459186B1 Bulletin 2013/41 November 10, 2013.
- 19.Ostacolo C, Caruso C, Tronino D, et al. Enhancement of corneal permeation of riboflavin-5'-phosphate through vitamin E TPGS: a promising approach in corneal trans-epithelial cross linking treatment. Int J Pharm. 2013;440:148–153. [DOI] [PubMed] [Google Scholar]
- 20.Barbaro G, Caruso C, Troisi S, et al. A Mathematical Model of Corneal UV-A Absorption After Soaking With a Riboflavin Solution During Transepithelial Cross-Linking. Paper presented at: 1st Joint International Congress Refractive online and SICSSO; July 7–9, 2011; Grosseto, Italy. Available at: http://www.irosrc.it/wp-content/uploads/Iros_Art.6.pdf; www.irosrc.it/research. Accessed November 15, 2015. [Google Scholar]
- 21.Koller T, Pajic B, Vinciguerra P, et al. Flattening of the cornea after collagen crosslinking for keratoconus. J Cataract Refract Surg. 2011;37:1488–1492. [DOI] [PubMed] [Google Scholar]
- 22.Wollensak G, Spörl E, Reber F, et al. Corneal endothelial cytotoxicity of riboflavin/UVA treatment in vitro. Ophthalmic Res. 2003;35:324–328. [DOI] [PubMed] [Google Scholar]
- 23.Schumacher S, Mrochen M, Wernli J, et al. Optimization model for UV-riboflavin corneal cross-linking. Invest Ophth Vis Sci. 2012;53:762–769. [DOI] [PubMed] [Google Scholar]
- 24.Hafezi F, Tabibian D, Richoz O. Additive effect of repeated corneal collagen cross-linking in keratoconus. J Refract Surg. 2014;30:716–718. [DOI] [PubMed] [Google Scholar]
- 25.Menassa N, Kaufmann C, Goggin M, et al. Comparison and reproducibility of corneal thickness and curvature readings obtained by the Galilei and the Orbscan II analysis systems. J Cataract Refract Surg. 2008;34:1742–1747. [DOI] [PubMed] [Google Scholar]
- 26.Nuñez MX, Blanco C. Efficacy of Orbscan II and Pentacam topographers by a repeatability analysis when assessing elevation maps in candidates to refractive surgery. Biomedica. 2009;29:362–368. [PubMed] [Google Scholar]
- 27.Kim H, Joo CK. Measure of keratoconus progression using orbscan II. J Refract Surg. 2008;24:600–605. [DOI] [PubMed] [Google Scholar]
- 28.Epstein RL, Chiu YL, Epstein GL. Pentacam HR criteria for curvature change in keratoconus and postoperative LASIK ectasia. J Refract Surg. 2012;28:890–894. [DOI] [PubMed] [Google Scholar]