Abstract
Biomechanical studies have shown that repair or plication of rotator interval (RI) ligamentous and capsular structures decreases glenohumeral joint laxity in various directions. Clinical outcomes studies have reported successful outcomes after repair or plication of these structures in patients undergoing shoulder stabilization procedures. Recent studies describing arthroscopic techniques to address these structures have intensified the debate over the potential benefit of these procedures as well as highlighted the differences between open and arthroscopic RI procedures. The purposes of this study were to review the structures of the RI and their contribution to shoulder instability, to discuss the biomechanical and clinical effects of repair or plication of rotator interval structures, and to describe the various surgical techniques used for these procedures and outcomes.
Keywords: rotator interval, shoulder instability, rotator interval plication, coracohumeral ligament
The rotator interval (RI) is a triangular space located in the anterosuperior aspect of the shoulder. First defined by Neer46 in 1970, the role of the RI in providing stability of the glenohumeral joint remains under debate. The structures of the RI have been shown to contribute to stability by maintaining negative glenohumeral joint intra-articular pressure30 and/or by resisting inferior glenohumeral translation.22,24,28,31,55,71 Many authors claim that the RI functions to prevent excessive inferior and/or posterior humeral head translation (not mutually exclusive).5 Others have argued that the RI is actually an area of tissue deficiency that can be injured in specific cases of shoulder instability, leading to chronic symptoms of shoulder instability.48,50,58 Specifically, some suggest that injuries to the RI are associated with increased glenohumeral translation and that surgical imbrication of the RI may augment the repair construct during multidirectional and posterior stabilization.12,17,24,31,43,54,71,78
Thus, while surgical plication of the RI has been advocated in cases of RI injury as well as in specific cases of shoulder instability,35,60,66,68 the true indications for these procedures remain controversial. One concern with performing RI plication, particularly in cases in which the procedure is unnecessary, is the potential for postoperative loss of external rotation.54,57,71,78 Historically, RI plication was performed via open surgical approaches; however, all-arthroscopic techniques for RI plication have more recently been described.10,12,16,32,35,44,66,69 Of note, open and arthroscopic RI closure are different surgical procedures and plicate different tissues, each in a different biomechanical vector. Thus, when evaluating the literature on RI closure, the specific technique used must be considered. The purposes of this study were to review the anatomy, function, and biomechanics of the RI; to discuss surgical closure in the setting of anterior, posterior, and multidirectional glenohumeral stabilization; and to review outcomes reported in the literature following RI closure.
Rotator Interval Anatomy
The triangular-shaped RI is bordered by the following (Figure 1):
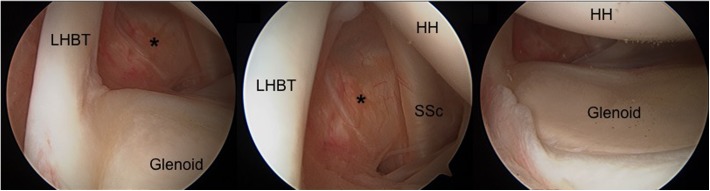
Figure 1.
The right shoulder during diagnostic arthroscopy performed in the lateral decubitus position (viewing from posterior) demonstrating the anatomy of the rotator interval from 3 different views. HH, humeral head; LHBT, long head of the biceps tendon; SSc, subscapularis; *rotator interval capsule.
Superior border: anterior border of the supraspinatus (SS)
Inferior border: superior border of the subscapularis (SSc)
Medial border: the base of the coracoid process
The anatomy of the RI is complicated due to the number of structures contained within a relatively small space, including the extra-articular coracohumeral ligament (CHL), the superior and middle glenohumeral ligaments (SGHL and MGHL, respectively), the long head of the biceps tendon (LHBT), and a thin layer of capsule that fills the capsular openings in the RI region.13,14,18,24,30,31,48,53
The CHL originates at the base of the coracoid and splits laterally into 2 bands. One band of the CHL inserts on the anterior edge of the SS tendon and greater tuberosity, while the other inserts on the SSc, the transverse humeral ligament, and the lesser tuberosity (Figure 2). Some authors have argued that the CHL is actually just a thickening of the anterosuperior glenohumeral capsule,24 while others maintain that the CHL is its own entity.47,50,51 Unlike the SGHL and the MGHL, the CHL is an extra-articular structure that is not visible during glenohumeral arthroscopy.
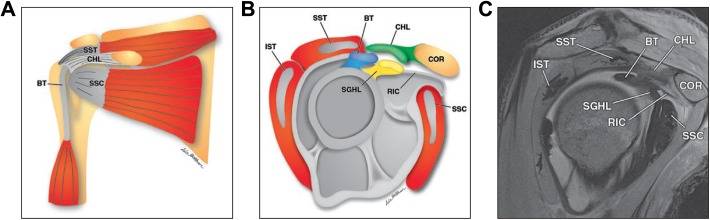
Figure 2.
Anatomy of the rotator interval, including illustrations in (A) coronal and (B) sagittal planes and (C) corresponding sagittal magnetic resonance proton density–weighted arthrogram show boundaries of the rotator interval, which are defined by the coracoid process (COR) at its base, superiorly by the anterior margin of supraspinatus tendon (SST), and inferiorly by the superior margin of the subscapularis tendon (SSc). Contents of the rotator interval include the long head of biceps tendon (BT), coracohumeral ligament (CHL), superior glenohumeral ligament (SGHL), and rotator interval capsule. The rotator interval capsule (RIC) is the anterosuperior aspect of the glenohumeral joint capsule, which merges with CHL and SGHL insertions medial and lateral to the bicipital groove. The CHL arises from the base of coracoid process, traverses through the subcoracoid fat, and inserts on the anterior humerus. IST, infraspinatus tendon. Reproduced with permission from Petchprapa et al.52
The SGHL is relatively smaller than the CHL, originating from the glenoid labrum adjacent to the supraglenoid tubercle, crossing the floor of the RI deep to the CHL, and inserting on the fovea capitis on the lesser tuberosity.24,49 The LHBT is located between the CHL and the SGHL.44 The SGHL is an intra-articular capsular ligament that can be visualized during glenohumeral arthroscopy.
Rotator Interval Function
In their classic cadaveric study, Harryman et al24 reported that the overall function of the RI was to (1) act as a restraint against extreme flexion, extension, adduction, and external rotation; (2) stabilize the humeral head against inferior translation while in adduction; and (3) stabilize the humeral head against posterior translation while in flexion or external rotation with abduction. Notably, Harryman et al came to these conclusions by either sectioning or imbricating the extra-articular CHL (which the authors labeled the “rotator interval capsule”) without altering the other RI capsuloligamentous structures.
Superior Glenohumeral Ligament
The importance of the SGHL in resisting inferior translation of the shoulder has been emphasized by some authors, while others argue that both the SGHL and CHL ligaments work together as a unit to prevent inferior and posterior translation of the humeral head.49,73 In an anatomic study, Warner et al73 determined that the SGHL was the primary restraint to inferior translation of the adducted shoulder, and that the anterior and posterior portions of the inferior glenohumeral ligament became more involved in preventing translation with increasing amounts of abduction.
Coracohumeral Ligament
Several investigators have suggested that the CHL is also an important stabilizer to inferior humeral head translation.8,50 Specifically, some authors consider the CHL to be the most important structure preventing downward translation of the adducted arm, while, as noted above, others consider the SGHL as the most important structure in preventing inferior translation.5,8,49,73 Certainly, while there is no consensus as to the most critical individual structure, as a whole, the RI prevents inferior translation of the adducted arm.
Capsule/Synovial Layer
The capsule or synovial layer of the RI is only 0.06 to 0.1 mm thick,53 and its role in overall joint stability is unclear. While the contribution of the capsular tissue to the RI can be difficult to quantify, it is thought that the thin layer of tissue creates a barrier for the joint that may contribute to maintaining the joint’s negative intra-articular pressure.25,29,30
Long Head of the Biceps Tendon
One final function of the RI is its contribution to the stability of the LHBT. Specifically, the CHL, SGHL, and SSc tendon are components of the biceps pulley system, which is responsible for the normal anatomic position of the biceps tendon.26,27,64,79
Biomechanical Considerations for Open Versus Arthroscopic Rotator Interval Closure
Open Rotator Interval Closure
As mentioned, Harryman et al24 analyzed the role of the RI in shoulder stability by assessing glenohumeral motion and translation in 3 different testing conditions: (1) intact RI, (2) sectioned CHL in the RI, and (3) CHL imbricated in a medial to lateral direction by 1 cm. The authors found that transverse sectioning of the CHL led to an increase in both inferior and posterior translation as well as increases in passive flexion, adduction, external rotation, and extension. Following CHL imbrication, motion and translation were substantially reduced, and the authors concluded that the RI “capsule” (in actuality, the CHL) was an important restraint to translation and excessive motion.
While the work of Harryman et al24 has been used to support the routine plication of RI structures in cases of posterior and multidirectional instability, the surgical approach (open or arthroscopic) and specific technique utilized must be carefully evaluated. Notably, while the open RI closure technique is typically described as medial-lateral plication, as described by Harryman et al, and while the arthroscopic technique is typically described as superior-inferior plication, a superior-inferior RI plication can also be performed via an open approach. For the purposes of the subsequent sections, open RI closure will refer to the technique described by Harryman et al (medial to lateral imbrication). A recent biomechanical comparison of open and arthroscopic RI plication techniques performed by Provencher et al57 found that the open technique as described by Harryman et al was not the same biomechanically as the arthroscopic technique in which the MGHL is sutured to the SGHL. Specifically, in their study, Provencher et al found that arthroscopic RI plication did not reduce posterior or inferior humeral head translation, whereas open CHL plication, performed in a medial to lateral direction, improved both anterior and inferior translation. Contrary to the results reported by Harryman et al, Provencher et al did not find a reduction in posterior translation of the humeral head following open RI plication. As will be discussed, the open medial-lateral CHL plication technique utilized by Harryman et al is not the same as the arthroscopic superior-inferior (SGHL to MHGL) plication technique (Figure 3).
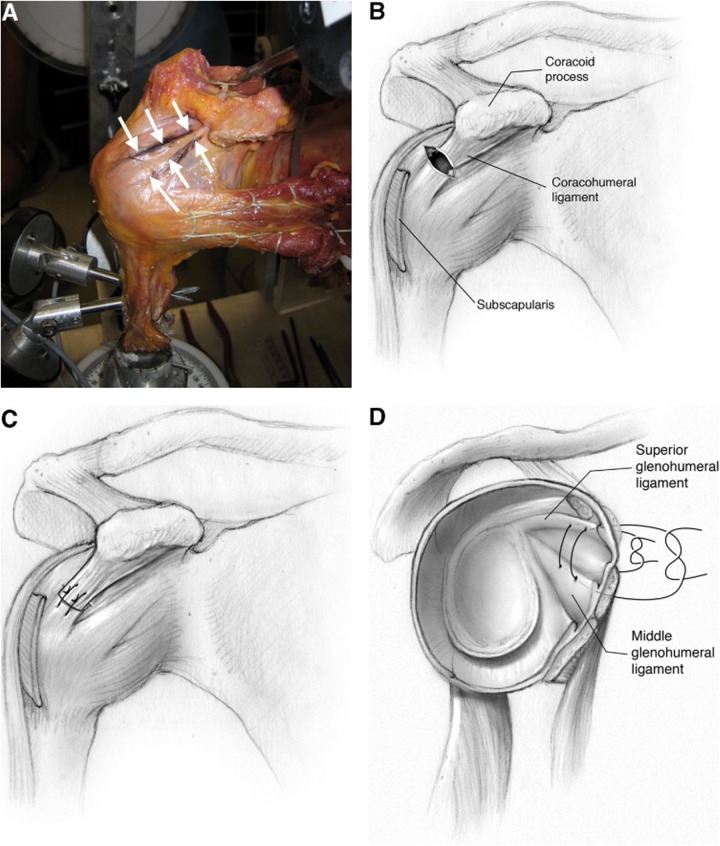
Figure 3.
Schematic figures demonstrating the 2 described methods of rotator interval plication. (A) The coracohumeral ligament (CHL) is shown, originating at the base of the coracoid and inserting laterally on the humerus, outlined in ink (arrows). The CHL is made more visible with sulcus translation of the glenohumeral joint, placing the CHL under tension and isolating the structure as a consistent cord-like band of tissue. (B) Open rotator interval (RI) closure as described by Harryman et al.24 An open repair of the RI is performed, and the CHL is imbricated by 1 cm (C) in the medial-to-lateral direction, with the arm in 30° of external rotation. (D) Arthroscopic RI repair is performed using 2 no. 2 nonabsorbable sutures (1 medial and 1 lateral), with the arm in 30° of external rotation. Reproduced with permission from Provencher et al.57
Arthroscopic Rotator Interval Closure
The biomechanical data supporting arthroscopic RI capsuloligamentous plication are controversial, with several authors reporting conflicting results. Most biomechanical studies on arthroscopic RI capsular plication procedures have demonstrated consistent decreases in anterior translation as well as minimal to no decreases in inferior or posterior translation. The majority of arthroscopic techniques involve a superior-inferior shift of the MGHL or SSc tendon to the SGHL. Of note, many authors describing this technique utilize the term “rotator interval closure” in describing such procedures. We prefer to reserve this term for historical procedures that actually close the interval by suturing the SS tendon to the SSc tendon. We advocate avoiding this terminology in favor of describing the actual anatomic procedure performed (ie, capsular plication of SGHL to MGHL) and recommend that in the future, such anatomic descriptions be used to enhance the ability of the orthopaedic community to compare techniques appropriately.
Overall, the implications of arthroscopic RI capsular plication are variably reported in the literature, with conflicting results with respect to stabilization and postoperative stiffness. In 2008, Shafer et al63 found that capsular plication alone was able to adequately limit range of motion to that of the intact shoulder, but that in some positions, reducing glenohumeral translation required concomitant RI closure performed in a superior to inferior direction. Notably, the addition of RI capsular plication to capsular plication resulted in a significant decrease in external rotation, potentially implying that such a procedure could lead to postoperative stiffness. Also in 2008, Mologne et al44 found that arthroscopic RI capsulolabral plication did not improve posterior labral repair stability in a cadaver model; however, the addition of this procedure after anterior labral repair did result in decreased anterior translation. Similar to Shafer et al, Mologne et al reported loss in external rotation after RI capuloligamentous plication, especially in adduction (28° loss) and abduction (5°). Interestingly, a 2009 biomechanical study by Farber et al16 described a medial-lateral shift in an attempt to arthroscopically replicate the work by Harryman et al.24 The authors found that the medial-lateral RI procedure was significantly more effective at reducing posterior translation than the superior-inferior RI procedure and that in 60° of abduction, only the medial-lateral repair restored range of motion to the intact state.
Classification of Rotator Interval Pathologic Changes
There is no accepted classification system for the description of pathologic changes within the RI region, although a few systems have been suggested. The available systems describe the RI on the basis of mechanical strength48,49 as well as on the basis of the involvement of other glenohumeral structures, including the RI capsule, CHL, SGHL, SS tendon, SSc tendon, and/or the LHBT.18 Overall, these classification systems provide a way to describe RI pathology, but to date, have not been helpful in guiding treatment decisions.
Diagnosis of Rotator Interval Pathology
A multifaceted workup, including a complete history, physical examination, advanced imaging studies, and often, diagnostic arthroscopy, is necessary to accurately diagnose the patient with suspected RI pathology. Certainly, the diagnosis of any pathology in addition to lesions to the RI is crucial for preoperative planning and appropriate surgical management.
History
Patients with RI pathology do not necessarily present with a classic injury mechanism. Some patients may report a history of an acute traumatic event to the shoulder, while others may also describe a history of chronic, overuse injuries that have resulted in a sensation of soft tissue insufficiency about the shoulder. It should be noted that an isolated RI lesion is probably quite rare and that RI pathology is usually seen with concomitant primary instability conditions of the shoulder.61 As suggested by Ho,26 injuries to the RI usually occur as part of a spectrum of glenohumeral pathology as opposed to a separate, isolated lesion, and surrounding structures including the labrum, CHL, LHBT, and rotator cuff are often injured along with an RI lesion. Thus, patients with RI lesions may also present with complaints related to one or more of these concomitant injuries. In a patient complaining of shoulder instability, it may become necessary to utilize advanced imaging modalities as well as diagnostic arthroscopy2 findings to support a clinical suspicion for RI pathology to arrive at an accurate diagnosis.
Physical Examination
Isolated pathology of the RI is difficult to assess on physical examination, as findings may be vague and representative of other shoulder lesions, including anterior, posterior, and/or multidirectional instability. It is imperative to perform a complete examination of the shoulder paying particular attention to signs for instability as well as glenohumeral pathology, including rotator cuff tears, impingement, and biceps pathology. As in any shoulder examination, the appearance, motion, neurological status, and stability of the injured shoulder should be compared with the opposite shoulder. Loss of motion should alert the clinician to pathology other than RI pathology, and if significant stiffness is noted, range of motion must be optimized prior to any operative stabilization procedure to avoid progressive loss of motion. Asymmetrical loss of external rotation at the side may indicate overconstraint of the subscapularis, the RI, or the superior capsule (SGHL, MGHL), while asymmetrical loss of external rotation in abduction may identify nonanatomic overconstraint of the inferior ligaments. Some authors advocate that increased external rotation at the side or a sulcus in external rotation is an indication for RI plication. Strength in all planes should also be assessed, and weakness may indicate the possible presence of concomitant pathology such as rotator cuff tear or suprascapular nerve palsy. Shoulder stability testing should also be addressed with focus on the various glenohumeral ligaments as the direction and degree may change the surgical plan. Symptomatic instability and laxity in the inferior direction that does not disappear in external rotation with the arm at the side as well as significant symptomatic capsular laxity in the setting of multidirectional instability are indicative of pathology to the RI.
Advanced Imaging Studies
Radiographic studies are typically unremarkable in patients with RI pathology, and the utility of advanced imaging modalities in the diagnosis of RI pathologic changes is limited, as distinguishing between so-called RI “lesions” and nonpathologic variants of normal anatomy can be challenging. Modalities such as magnetic resonance imaging (MRI) and/or arthrography (MRA) are the most helpful in discriminating between normal anatomy and pathologic changes associated with the RI.38,49,72 MRA is the most sensitive of all imaging studies, and typical signs of RI injury include contrast fluid in the subacromial and/or subdeltoid bursa through the RI as well as contrast under the coracoid on oblique sagittal images.6,7,11,38,49,72 Improper MRA technique can result in contrast fluid being injected into the soft tissues as opposed to intra-articularly, making RI pathologic changes extremely difficult to define.11,45 The presence of normal rotator interval capsular openings (RICOs)15,76 can also lead to contrast extravasation into these areas, further complicating image interpretation (Figure 4). Cole et al13 demonstrated that RICOs are present in fetal cadaveric specimens, suggesting that these openings may not represent damage suffered in an injury but rather are normal developmental variations in how the anterior capsule is formed.13 The variability of the RI on MRI in patients with clinical evidence of glenohumeral instability has been described by several authors with conflicting results. When comparing the size of the RI on MRI in 202 patients with shoulder instability to that of 50 control patients without instability, Kim et al33 reported a significantly increased RI size (both height and area) in instability patients. Similarly, Lee et al37 studied the MRA findings of 47 patients with atraumatic multidirectional shoulder instability and 50 patients without instability and reported that RI width and depth were significantly greater in the multidirectional instability group compared with the control group. In contrast, using MRA, Provencher et al56 demonstrated no enlargement of RI dimensions in patients with glenohumeral instability.
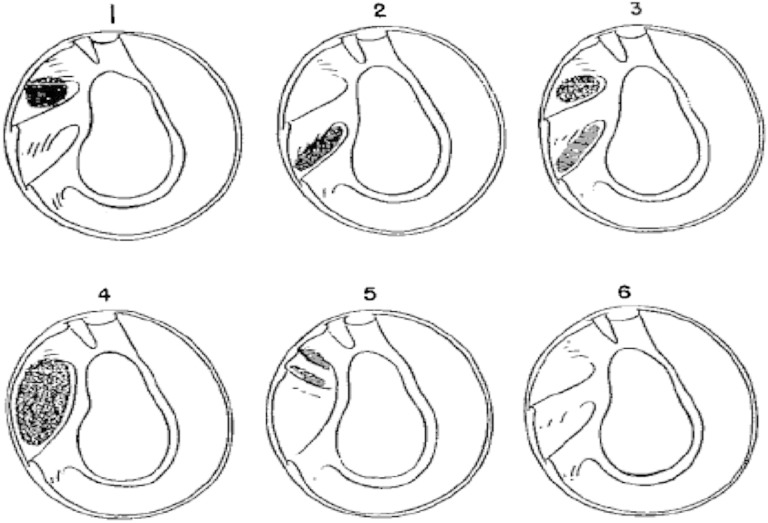
Figure 4.
Schematic representation of the 6 subtypes of variants of the rotator interval capsular opening (RICO) as described by DePalma et al15 based on their cadaveric dissection. Reproduced with permission from Wilson et al.76
Because of the difficulty in interpreting imaging studies, in addition to history and physical examination, the diagnosis of RI pathology is often made at the time of surgery, aided by findings from the examination under anesthesia as well as the diagnostic arthroscopy.2,18,66 Specifically, the senior authors (D.T., N.N.V., A.A.R., T.S.M., and M.T.P.) define injury based on the arthroscopic or open evidence of disruption of labral, ligamentous, tendinous (subscapularis), or cartilaginous tissue. To be able to make that determination, one must be aware of the anatomic variations in the RI. Certainly, patients can have symptomatic instability without structural injury and with a normal appearing lax capsule that can be treated with a variety of procedures to tighten up the capsule.
Treatment Options, Indications for Surgery, and Decision Making
Indications for rotator interval surgery remain controversial. While clinical and biomechanical studies demonstrate decreased anterior translation with arthroscopic plication of the MGHL to the SGHL, the outcomes are not as clear with respect to posterior and/or inferior stability. Furthermore, the potential for postoperative stiffness, particularly in external rotation, is concerning.65 Based on the clinical experience and biomechanical analyses of the senior author (M.T.P.), RI capsuloligamentous plication may be considered in patients with the following conditions: (1) symptomatic instability and laxity in the inferior direction that does not disappear in external rotation with the arm at the side and (2) significant symptomatic capsular laxity in the setting of multidirectional instability.23 It should be noted that it is exceedingly rare to operate on the RI capsular structures in isolation, and currently, there are no long-term clinical studies regarding the outcomes of RI plication procedures.
Once a patient is deemed to be a candidate for an RI procedure, open and/or arthroscopic surgical techniques can be considered. From biomechanical studies, it is thought that arthroscopic RI capsular plication may better improve anterior stability whereas open RI capsular plication, when performed in a medial to lateral direction, may improve both posterior and inferior stability. When considering RI closure in the setting of instability, it is important to consider the “circle concept” of the shoulder, as elegantly described by Warren et al.74 The “circle concept” centers on the idea that capsular injuries on both sides of the capsule occur in the setting of a glenohumeral dislocation, such that in order for a shoulder to dislocate posteriorly, there must be capsuloligamentous damage on the anterior side (ie, the rotator interval). In light of this concept, it would follow that during surgery, if other portions of the capsule are tensioned/imbricated, the “gap” within the RI may open even further if not concomitantly repaired. The “circle concept” has been challenged, however, by findings from several cadaveric studies that did not describe injuries to anterior structures, including the RI, in a posteriorly dislocated shoulder, and thus, the decision to close the RI concomitantly with a posterior stabilization procedure must be evaluated on a case-by-case basis.44,57,75
Regardless of whether the procedure is performed open or arthroscopically, it is important to consider the position of the shoulder during the procedure to avoid overtightening the capsule and potentially causing postoperative loss of external rotation.44,57 Currently, there is no consensus on arm position, with a variety of authors recommending varying degrees of abduction and external rotation at the time of RI plication.18,21,49,55,66,78
Surgical Technique
Various open and arthroscopic surgical techniques for plication of RI structures have been described.¶ Regardless of the technique used, appropriate indications for surgery as well as experience of the surgeon with the technical aspects of the procedure are probably the most significant factors in predicting the success of any RI procedure. In general, the vast majority of published studies describe open RI closure as a medial to lateral plication of RI tissue and arthroscopic RI closure as a superior to inferior plication of RI tissue. An important difference between open and arthroscopic RI closure is that the adjoining capsule is adherent to the subscapularis and supraspinatus muscle-tendon units when arthroscopic closure is performed. In contrast, the capsule can be freed from these attachments via an open technique. In addition, when interpreting the available studies discussing open and arthroscopic management of RI “pathology,” it is important to differentiate between true pathologic changes to the RI and anatomic variants of normal, or RICOs. Several authors describe “closure” of the RI as a suture repair incorporating the MGHL to the SGHL, which other authors consider akin to closure of the RICO.67 Certainly, it is important to understand that there is likely a continuum between normal openings and pathologic laxity, and differentiating between normal RI openings and true capsular laxity is extremely challenging.
Open Rotator Interval Techniques
For open RI capsular plication, several clinical studies have described RI lesions repaired without concomitant shoulder stabilization by all-suture techniques. These lesions likely represent RICOs. After repair of the capsular opening with nonabsorbable sutures, the CHL is typically sutured over the top by imbricating the inferior border of the RI defect margin with the superior border of the RICO in a “pants-over-vest” fashion, with good to excellent results reported in most patients.17,36,48 The authors describing these techniques position the shoulder in external rotation prior to the repair; however, the amount of external rotation is variable.
Arthroscopic Rotator Interval Techniques
Multiple arthroscopic surgical techniques for RI capsuloligamentous plication have been described; however, only a small subset of these reports describe clinical outcomes.# Furthermore, the vast majority of these studies include patients undergoing concomitant procedures, and thus, it is difficult to assess the effectiveness of the RI procedure relative to the other procedures being performed. Several of the more recent studies describing arthroscopic techniques have intensified the debate over the potential benefit (or lack thereof) of these procedures.
Of note, inadvertent damage to the RI capsule, especially during capsulolabral reconstruction, may be encountered during arthroscopic instability repair. The very placement of the anterior portal may leave a large defect in the RI capsule once the cannula is removed, which may contribute to glenohumeral instability recurrence. In 2002, Karas32 noted that the RI lesion described in the study by Harryman et al24 closely resembled the type of defect created in the RI capsule after standard anterior portal placement, and subsequently, Karas described a technique for RI capsular defect closure that does not require an interval portal. The reported advantages of this 1-portal technique are that there is direct visualization of the interval capsule, it can be performed repeatedly until the plication is deemed adequate, the subacromial space is not compromised, and the spinal needle and suture retriever are introduced through the same anterior portal, thus eliminating the need for accessory portals.
In 2004, Taverna et al69 described an “all-inside” arthroscopic technique for repair of RI pathologic structures. In this technique, the arm is positioned in 30° of external rotation and abduction to decrease the possible postoperative loss of external rotation. A superior to inferior RI “closure” is performed, plicating the superior capsule adjacent to the anterior border of the SS to the MGHL. Currently, no studies reporting on the short- or long-term clinical outcomes after stabilization of the RI with this technique are available.
Clinical Outcomes Studies After Shoulder Stabilization Incorporating Rotator Interval Stabilization
Multiple open and arthroscopic stabilization studies describing the incorporation of RI procedures are available in the literature. Furthermore, no studies have compared stabilization procedures with and without RI plication/closure. The utilization of a concomitant RI plication procedure in addition to the main stabilization procedure has been described; however, the indications for plication of any of the RI capsuloligamentous tissues remain loosely defined.19 Plication of the RI structures in cases of anterior instability has been described to improve recurrence rates; however, this has not been fully evaluated, and concerns regarding postoperative loss of external rotation remain. During cases of posterior and/or multidirectional instability repair, the RI has been described as being plicated with both thermal and suture capsulorrhaphy techniques with varying results. Certainly, additional biomechanical and clinical studies are necessary to clearly define the role of RI procedures as an augment to anterior, posterior, or multidirectional instability repair.
Postoperative Management
The postoperative protocol for RI capsuloligamentous plication follows the primary procedure repair guidelines (ie, for anterior, posterior, or multidirectional stabilization). Typically, patients will be placed into a sling for 4 to 6 weeks, and the primary procedure (as opposed to the RI procedure) will dictate the postoperative regimen. Of note, it is advised to avoid more than 30° of external rotation for the first 5 to 6 weeks to protect the RI plication. After the sling is removed, active and active-assisted exercises and terminal range of motion stretching is begun. Gradual return to activity is then begun with a goal of full activity at 6 months.
Conclusion
The pathoanatomy of the RI remains a controversial topic among shoulder specialists treating shoulder instability. Overall, an improved understanding of RI pathology, better means of diagnosing symptomatic RI pathology, and higher quality studies evaluating the effectiveness of RI capsular plication are necessary. While surgical plication of RI structures may be indicated in a select group of instability procedures, the biomechanical and clinical evidence for routine plication is inconclusive. The majority of the available literature is based on cadaveric studies of open RI procedures, and the findings of these studies cannot and should not necessarily be applied to procedures performed arthroscopically. Current arthroscopic RI cadaveric studies suggest that the most significant changes associated with RI capsulolabral plication are decreased anterior translation and decreased external rotation. A prospective clinical trial regarding the utility of RI procedures in arthroscopic shoulder stabilization procedures is needed to better identify the potential clinical benefits and cost-effectiveness of these procedures. Overall, additional studies are needed to clarify the role of the RI and its associated structures in the setting of shoulder instability to better define indications and improve surgical techniques.
Footnotes
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government. No sources of support in the forms of grants, equipment, or other items were received for this study.
One or more of the authors has declared the following potential conflict of interest: N.N.V. receives royalties from Smith & Nephew; is a paid consultant for Minivasive and Smith & Nephew; has stock/stock options in Cymedica, Minivasive, and Omeros; and receives research support from Arthrex, Smith & Nephew, Athletico, ConMed Linvatec, Miomed, Mitek, Arthrosurface, and DJ Orthopaedics. A.A.R. is a consultant for Arthrex and Saunders/Mosby-Elsevier; receives royalties from Arthrex and Saunders/Mosby-Elsevier; receives speaking fees from Arthrex; and receives research funding from Arthrex, DJO Surgical, Smith & Nephew, and Ossur.
References
- 1. Almazán A, Ruiz M, Cruz F, Pérez FX, Ibarra C. Simple arthroscopic technique for rotator interval closure. Arthroscopy. 2006;22:230.e1–230.e4. [DOI] [PubMed] [Google Scholar]
- 2. Anbar A, Emad Y, Zeinhom F, Ragab Y. Shoulder arthroscopy remains superior to direct MR arthrography for diagnosis of subtle rotator interval lesions. Eur J Orthop Surg Traumatol. 2015;25:689–697. [DOI] [PubMed] [Google Scholar]
- 3. Antoniou J, Duckworth DT, Harryman DT., 2nd Capsulolabral augmentation for the the management of posteroinferior instability of the shoulder. J Bone Joint Surg Am. 2000;82:1220–1230. [DOI] [PubMed] [Google Scholar]
- 4. Barnes CJ, Getelman MH, Snyder SJ. Results of arthroscopic revision anterior shoulder reconstruction. Am J Sports Med. 2009;37:715–719. [DOI] [PubMed] [Google Scholar]
- 5. Basmajian JV, Bazant FJ. Factors preventing downward dislocation of the adducted shoulder joint. J Bone Joint Surg Am. 1959;41-A:1182–1186. [PubMed] [Google Scholar]
- 6. Beall DP, Morag Y, Ly JQ, et al. Magnetic resonance imaging of the rotator cuff interval. Semin Musculoskelet Radiol. 2006;10:187–196. [DOI] [PubMed] [Google Scholar]
- 7. Bigoni BJ, Chung CB. MR imaging of the rotator cuff interval. Magn Reson Imaging Clin N Am. 2004;12:61–73. [DOI] [PubMed] [Google Scholar]
- 8. Boardman ND, Debski RE, Warner JJ, et al. Tensile properties of the superior glenohumeral and coracohumeral ligaments. J Shoulder Elbow Surg. 1996;5:249–254. [DOI] [PubMed] [Google Scholar]
- 9. Bottoni CR, Franks BR, Moore JH, DeBerardino TM, Taylor DC, Arciero RA. Operative stabilization of posterior shoulder instability. Am J Sports Med. 2005;33:996–1002. [DOI] [PubMed] [Google Scholar]
- 10. Calvo A, Martínez AA, Domingo J, Herrera A. Rotator interval closure after arthroscopic capsulolabral repair: a technical variation. Arthroscopy. 2005;21:765. [DOI] [PubMed] [Google Scholar]
- 11. Chung C, Dwek J, Cho G, Lektrakul N, Trudell D, Resnick D. Rotator cuff interval: evaluation with MR imaging and MR arthrography of the shoulder in 32 cadavers. J Comput Assist Tomogr. 2000;24:738–743. [DOI] [PubMed] [Google Scholar]
- 12. Cole BJ, Mazzocca AD, Meneghini RM. Indirect arthroscopic rotator interval repair. Arthroscopy. 2003;19:E28–E31. [DOI] [PubMed] [Google Scholar]
- 13. Cole BJ, Rodeo SA, O’Brien SJ, et al. The anatomy and histology of the rotator interval capsule of the shoulder. Clin Orthop Relat Res. 2001;390:129–137. [DOI] [PubMed] [Google Scholar]
- 14. Cooper DE, O’Brien SJ, Arnoczky SP, Warren RF. The structure and function of the coracohumeral ligament: an anatomic and microscopic study. J Shoulder Elbow Surg. 1993;2:70–77. [DOI] [PubMed] [Google Scholar]
- 15. DePalma AF, Callery G, Bennett GA. Variational anatomy and degenerative lesions of the shoulder joint. Instr Course Lect. 1949;6:255–281. [Google Scholar]
- 16. Farber AJ, Elattrache NS, Tibone JE, McGarry MH, Lee TQ. Biomechanical analysis comparing a traditional superior-inferior arthroscopic rotator interval closure with a novel medial-lateral technique in a cadaveric multidirectional instability model. Am J Sports Med. 2009;37:1178–1185. [DOI] [PubMed] [Google Scholar]
- 17. Field LD, Warren RF, O’Brien SJ, Altchek DW, Wickiewicz TL. Isolated closure of rotator interval defects for shoulder instability. Am J Sports Med. 1995;23:557–563. [DOI] [PubMed] [Google Scholar]
- 18. Fitzpatrick M, Powell S, Tibone J, Warren R. Instructional course 106: the anatomy, pathology, and definitive treatment of rotator interval lesions: current concepts. Arthroscopy. 2003;19(10 suppl 1):70–79. [DOI] [PubMed] [Google Scholar]
- 19. Forsythe B, Frank RM, Ahmed M, et al. Identification and treatment of existing copathology in anterior shoulder instability repair. Arthroscopy. 2015;31:154–166. [DOI] [PubMed] [Google Scholar]
- 20. Garofalo R, Mocci A, Moretti B, et al. Arthroscopic treatment of anterior shoulder instability using knotless suture anchors. Arthroscopy. 2005;21:1283–1289. [DOI] [PubMed] [Google Scholar]
- 21. Gartsman GM, Taverna E, Hammerman SM. Arthroscopic rotator interval repair in glenohumeral instability: description of an operative technique. Arthroscopy. 1999;15:330–332. [DOI] [PubMed] [Google Scholar]
- 22. Gaskill TR, Braun S, Millett PJ. Multimedia article. The rotator interval: pathology and management. Arthroscopy. 2011;27:556–567. [DOI] [PubMed] [Google Scholar]
- 23. Gaskill TR, Taylor DC, Millett PJ. Management of multidirectional instability of the shoulder. J Am Acad Orthop Surg. 2011;19:758–767. [DOI] [PubMed] [Google Scholar]
- 24. Harryman DT, 2nd, Sidles JA, Harris SL, Matsen FA., 3rd The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74:53–66. [PubMed] [Google Scholar]
- 25. Helmig P, Sojbjerg JO, Sneppen O, Loehr JF, Ostgaard SE, Suder P. Glenohumeral movement patterns after puncture of the joint capsule: an experimental study. J Shoulder Elbow Surg. 1993;2:209–215. [DOI] [PubMed] [Google Scholar]
- 26. Ho CP. MR imaging of rotator interval, long biceps, and associated injuries in the overhead-throwing athlete. Magn Reson Imaging Clin N Am. 1999;7:23–37. [PubMed] [Google Scholar]
- 27. Hsu SH, Miller SL, Curtis AS. Long head of biceps tendon pathology: management alternatives. Clin Sports Med. 2008;27:747–762. [DOI] [PubMed] [Google Scholar]
- 28. Hunt SA, Kwon YW, Zuckerman JD. The rotator interval: anatomy, pathology, and strategies for treatment. J Am Acad Orthop Surg. 2007;15:218–227. [DOI] [PubMed] [Google Scholar]
- 29. Itoi E, Berglund LJ, Grabowski JJ, Naggar L, Morrey BF, An KN. Superior-inferior stability of the shoulder: role of the coracohumeral ligament and the rotator interval capsule. Mayo Clin Proc. 1998;73:508–515. [DOI] [PubMed] [Google Scholar]
- 30. Itoi E, Berglund LJ, Grabowski JJ, Naggar L, Morrey BF, An KN. Superior-inferior stability of the shoulder: role of the coracohumeral ligament and the rotator interval capsule. Mayo Clin Proc. 1998;73:508–515. [DOI] [PubMed] [Google Scholar]
- 31. Jost B, Koch PP, Gerber C. Anatomy and functional aspects of the rotator interval. J Shoulder Elbow Surg. 2000;9:336–341. [DOI] [PubMed] [Google Scholar]
- 32. Karas SG. Arthroscopic rotator interval repair and anterior portal closure: an alternative technique. Arthroscopy. 2002;18:436–439. [DOI] [PubMed] [Google Scholar]
- 33. Kim KC, Rhee KJ, Shin HD, Kim YM. Estimating the dimensions of the rotator interval with use of magnetic resonance arthrography. J Bone Joint Surg Am. 2007;89:2450–2455. [DOI] [PubMed] [Google Scholar]
- 34. Kim SH, Kim HK, Sun JI, Park JS, Oh I. Arthroscopic capsulolabroplasty for posteroinferior multidirectional instability of the shoulder. Am J Sports Med. 2004;32:594–607. [DOI] [PubMed] [Google Scholar]
- 35. Krych AJ, Shindle MK, Baran S, Warren RF. Isolated arthroscopic rotator interval closure for shoulder instability. Arthrosc Tech. 2014;3:e35–e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Le Huec JC, Schaeverbeke T, Moinard M, et al. Traumatic tear of the rotator interval. J Shoulder Elbow Surg. 1996;5:41–46. [DOI] [PubMed] [Google Scholar]
- 37. Lee HJ, Kim NR, Moon SG, Ko SM, Park JY. Multidirectional instability of the shoulder: rotator interval dimension and capsular laxity evaluation using MR arthrography. Skeletal Radiol. 2013;42:231–238. [DOI] [PubMed] [Google Scholar]
- 38. Lee JC, Guy S, Connell D, Saifuddin A, Lambert S. MRI of the rotator interval of the shoulder. Clin Radiol. 2007;62:416–423. [DOI] [PubMed] [Google Scholar]
- 39. Lewicky YM, Lewicky RT. Simplified arthroscopic rotator interval capsule closure: an alternative technique. Arthroscopy. 2005;21:1276. [DOI] [PubMed] [Google Scholar]
- 40. Mazzocca AD, Brown FM, Jr, Carreira DS, Hayden J, Romeo AA. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33:52–60. [DOI] [PubMed] [Google Scholar]
- 41. McIntyre LF, Caspari RB, Savoie FH., 3rd The arthroscopic treatment of multidirectional shoulder instability: two-year results of a multiple suture technique. Arthroscopy. 1997;13:418–425. [DOI] [PubMed] [Google Scholar]
- 42. McIntyre LF, Caspari RB, Savoie FH., 3rd The arthroscopic treatment of posterior shoulder instability: two-year results of a multiple suture technique. Arthroscopy. 1997;13:426–432. [DOI] [PubMed] [Google Scholar]
- 43. Millett P, Clavert P, Warner J. Arthroscopic management of anterior, posterior, and multidirectional shoulder instability: pearls and pitfalls. Arthroscopy. 2003;19(10 suppl 1):86–93. [DOI] [PubMed] [Google Scholar]
- 44. Mologne TS, Zhao K, Hongo M, Romeo AA, An KN, Provencher MT. The addition of rotator interval closure after arthroscopic repair of either anterior or posterior shoulder instability: effect on glenohumeral translation and range of motion. Am J Sports Med. 2008;36:1123–1131. [DOI] [PubMed] [Google Scholar]
- 45. Morag Y, Jacobson JA, Shields G, et al. MR arthrography of the rotator interval, long head of the biceps brachii, and biceps pulley of the shoulder. Radiology. 2005;235:21–30. [DOI] [PubMed] [Google Scholar]
- 46. Neer CS. 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 47. Neer CS, 2nd, Satterlee CC, Dalsey RM, Flatow EL. The anatomy and potential effects of contracture of the coracohumeral ligament. Clin Orthop Relat Res. 1992;280:182–185. [PubMed] [Google Scholar]
- 48. Nobuhara K, Ikeda H. Rotator interval lesion. Clin Orthop Relat Res. 1987;223:44–50. [PubMed] [Google Scholar]
- 49. Nottage WM. Rotator interval lesions: physical exam, imaging, arthroscopic findings, and repair. Tech Shoulder Elbow Surg. 2003;4:175–184. [Google Scholar]
- 50. Ovesen J, Nielsen S. Stability of the shoulder joint. Cadaver study of stabilizing structures. Acta Orthop Scand. 1985;56:149–151. [DOI] [PubMed] [Google Scholar]
- 51. Ozaki J, Nakagawa Y, Sakurai G, Tamai S. Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J Bone Joint Surg Am. 1989;71:1511–1515. [PubMed] [Google Scholar]
- 52. Petchprapa CN, Beltran LS, Jazrawi LM, Kwon YW, Babb JS, Recht MP. The rotator interval: a review of anatomy, function, and normal and abnormal MRI appearance. AJR Am J Roentgenol. 2010;195:567–576. [DOI] [PubMed] [Google Scholar]
- 53. Plancher KD, Johnston JC, Peterson RK, Hawkins RJ. The dimensions of the rotator interval. J Shoulder Elbow Surg. 2005;14:620–625. [DOI] [PubMed] [Google Scholar]
- 54. Plausinis D, Bravman JT, Heywood C, Kummer FJ, Kwon YW, Jazrawi LM. Arthroscopic rotator interval closure: effect of sutures on glenohumeral motion and anterior-posterior translation. Am J Sports Med. 2006;34:1656–1661. [DOI] [PubMed] [Google Scholar]
- 55. Pradhan RL, Itoi E. Rotator interval lesions of the shoulder joint. Orthopedics. 2001;24:798–801. [DOI] [PubMed] [Google Scholar]
- 56. Provencher MT, Dewing CB, Bell SJ, et al. An analysis of the rotator interval in patients with anterior, posterior, and multidirectional shoulder instability. Arthroscopy. 2008;24:921–929. [DOI] [PubMed] [Google Scholar]
- 57. Provencher MT, Mologne TS, Hongo M, Zhao K, Tasto JP, An KN. Arthroscopic versus open rotator interval closure: biomechanical evaluation of stability and motion. Arthroscopy. 2007;23:583–592. [DOI] [PubMed] [Google Scholar]
- 58. Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Joint Surg Am. 1984;66:159–168. [PubMed] [Google Scholar]
- 59. Savoie FH. The use of rotator interval closure in the arthroscopic treatment of posterior shoulder instability. Arthroscopy. 2009;25:110–111. [DOI] [PubMed] [Google Scholar]
- 60. Savoie FH, 3rd, Holt MS, Field LD, Ramsey JR. Arthroscopic management of posterior instability: evolution of technique and results. Arthroscopy. 2008;24:389–396. [DOI] [PubMed] [Google Scholar]
- 61. Schenk TJ, Brems JJ. Multidirectional instability of the shoulder: pathophysiology, diagnosis, and management. J Am Acad Orthop Surg. 1998;6:65–72. [DOI] [PubMed] [Google Scholar]
- 62. Selecky MT, Tibone JE, Yang BY, McMahon PJ, Lee TQ. Glenohumeral joint translation after arthroscopic thermal capsuloplasty of the rotator interval. J Shoulder Elbow Surg. 2003;12:139–143. [DOI] [PubMed] [Google Scholar]
- 63. Shafer BL, Mihata T, McGarry MH, Tibone JE, Lee TQ. Effects of capsular plication and rotator interval closure in simulated multidirectional shoulder instability. J Bone Joint Surg Am. 2008;90:136–144. [DOI] [PubMed] [Google Scholar]
- 64. Slatis P, Aalto K. Medial dislocation of the tendon of the long head of the biceps brachii. Acta Orthop Scand. 1979;50:73–77. [DOI] [PubMed] [Google Scholar]
- 65. Sodl JF, McGarry MH, Campbell ST, Tibone JE, Lee TQ. Biomechanical effects of anterior capsular plication and rotator interval closure in simulated anterior shoulder instability [published online February 9, 2014]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-2878-8. [DOI] [PubMed] [Google Scholar]
- 66. Stokes DA, Savoie FH, 3rd, Field LD, Ramsey JR. Arthroscopic repair of anterior glenohumeral instability and rotator interval lesions. Orthop Clin North Am. 2003;34:529–538. [DOI] [PubMed] [Google Scholar]
- 67. Svoboda SJ, Taylor DC, Magnussen RA. The anatomic variability of the “rotator interval capsule”: a comparison of arthroscopic and open investigations. Duke Orthop J. 2013;3:54–60. [Google Scholar]
- 68. Taverna E, Sansone V, Battistella F. Arthroscopic rotator interval repair: the three-step all-inside technique. Arthroscopy. 2004;20:105–109. [DOI] [PubMed] [Google Scholar]
- 69. Taverna E, Sansone V, Battistella F. Arthroscopic rotator interval repair: the three-step all-inside technique. Arthroscopy. 2004;20(suppl 2):105–109. [DOI] [PubMed] [Google Scholar]
- 70. Treacy SH, Field LD, Savoie FH. Rotator interval capsule closure: an arthroscopic technique. Arthroscopy. 1997;13:103–106. [DOI] [PubMed] [Google Scholar]
- 71. Van der Reis W, Wolf E. Arthroscopic rotator cuff interval capsular closure. Orthopedics. 2001;24:657–661. [DOI] [PubMed] [Google Scholar]
- 72. Vinson EN, Major NM, Higgins LD. Magnetic resonance imaging findings associated with surgically proven rotator interval lesions. Skeletal Radiol. 2007;36:405–410. [DOI] [PubMed] [Google Scholar]
- 73. Warner JJ, Deng X-H, Warren RF, Torzilli PA. Static capsuloligamentous restraints to superior-inferior translation of the glenohumeral joint. Am J Sports Med. 1992;20:675–685. [DOI] [PubMed] [Google Scholar]
- 74. Warren RF, Kornblatt IB, Marchand R. Static factors affecting posterior shoulder stability. Orthop Trans. 1984;8:89. [Google Scholar]
- 75. Weber SC, Caspari RB. A biomechanical evaluation of the restraints to posterior shoulder dislocation. Arthroscopy. 1989;5:115–121. [DOI] [PubMed] [Google Scholar]
- 76. Wilson WR, Magnussen RA, Irribarra LA, Taylor DC. Variability of the capsular anatomy in the rotator interval region of the shoulder. J Shoulder Elbow Surg. 2013;22:856–861. [DOI] [PubMed] [Google Scholar]
- 77. Wolf R, Zheng N, Iero J, Weichel D. The effects of thermal capsulorrhaphy and rotator interval closure on multidirectional laxity in the glenohumeral joint: a cadaveric biomechanical study. Arthroscopy. 2004;20:1044–1049. [DOI] [PubMed] [Google Scholar]
- 78. Yamamoto N, Itoi E, Tuoheti Y, et al. Effect of rotator interval closure on glenohumeral stability and motion: a cadaveric study. J Shoulder Elbow Surg. 2006;15:750–758. [DOI] [PubMed] [Google Scholar]
- 79. Zappia M, Reginelli A, Russo A, et al. Long head of the biceps tendon and rotator interval. Musculoskelet Surg. 2013;97(suppl 2):S99–S108. [DOI] [PubMed] [Google Scholar]