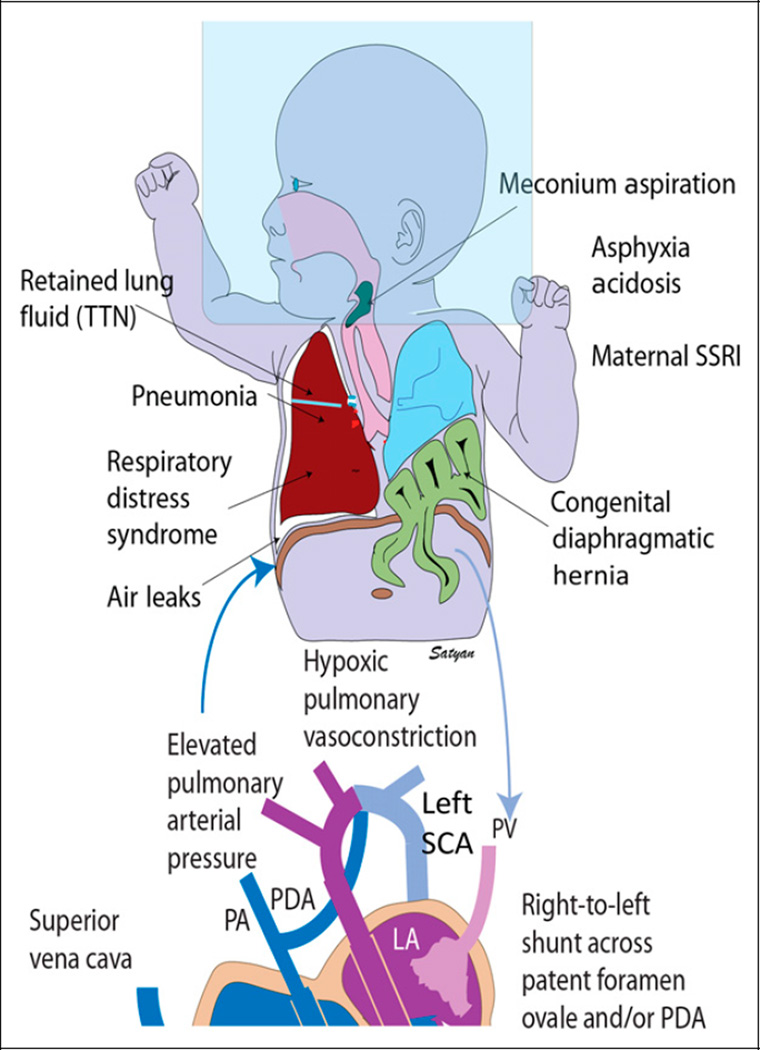
Figure 2.
Etiology and pathophysiology of persistent pulmonary hypertension of the newborn (PPHN). Secondary PPHN can be due to various lung diseases, such as retained lung fluid or transient tachypnea of newborn (TTN), pneumonia, aspiration syndromes, respiratory distress syndrome (RDS), and congenital diaphragmatic hernia with lung hypoplasia. Use of high concentrations of inspired oxygen (approximately 100%) without positive pressure (oxygen hood) can lead to absorption atelectasis and worsening of ventilation-perfusion mismatch. Lung disease and V/Q mismatch result in hypoxemia. Increased pulmonary vascular resistance results in reduced pulmonary blood flow and right-to-left shunt through patent ductus arteriosus (PDA) and/or patent foramen ovale (PFO). Pulmonary hypertension is often associated with systemic hypotension with deviation of the interventricular septum to the left. The right subclavian artery (SCA) (and blood flowing to the right upper extremity) is always preductal. The left SCA may be preductal, juxtaductal, or postductal. Hence, preductal oxygen saturations should be obtained from the right upper extremity and compared with lower extremity to assess differential cyanosis.
LA = left atrium; LV = left ventricle; PA = pulmonary artery; RA = right atrium RV = right ventricle; TR = tricuspid regurgitation. Copyright Satyan Lakshminrusimha.