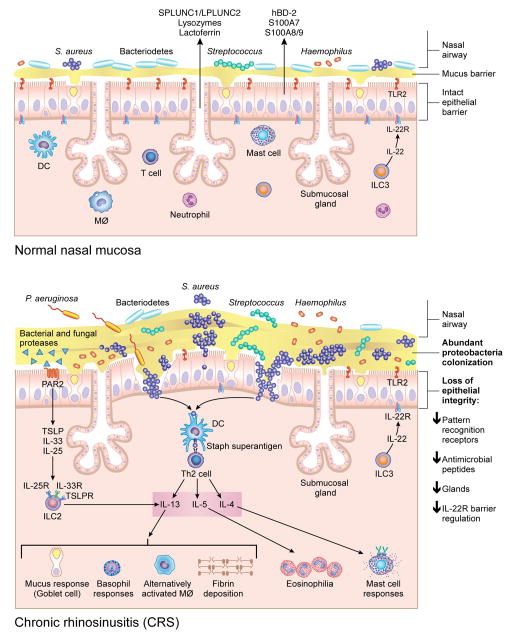
Figure 1. A Model for changes in the nasal microbiome and mucosal immune response in CRSwNP.
Although multiple microorganisms colonize healthy nasal mucosa membranes, as shown in the top figure, there are changes that occur in the microbiome in patients with CRSwNP, including increased S. aureus abundance, decreased Bacteriodetes and decreased diversity, as shown in the bottom figure. These changes, along with loss of epithelial integrity, decreased pattern recognition molecules, decreased mucosal glands and decreased antimicrobial peptide production in the nasal polyp and sinus tissue, can potentially provide an environment that promotes invasion of microorganisms across the mucosal barrier. Enterotoxins produced by S. aureus can act as superantigens and promote Th-2 inflammation, resulting in production of cytokines such as IL-13, IL-4 and IL-5 that further recruit and activate inflammatory cells such as eosinophils, mast cells, basophils and alternatively activated macrophages. Bacterial and fungal proteases can induce production of thymic stromal lymphopoietin (TSLP) through Protease-Activated Receptor-2(PAR-2)[151], which will subsequently result in activation of innate lymphoid type 2 cells (ILC-2) that further produce IL-5 and IL-13.