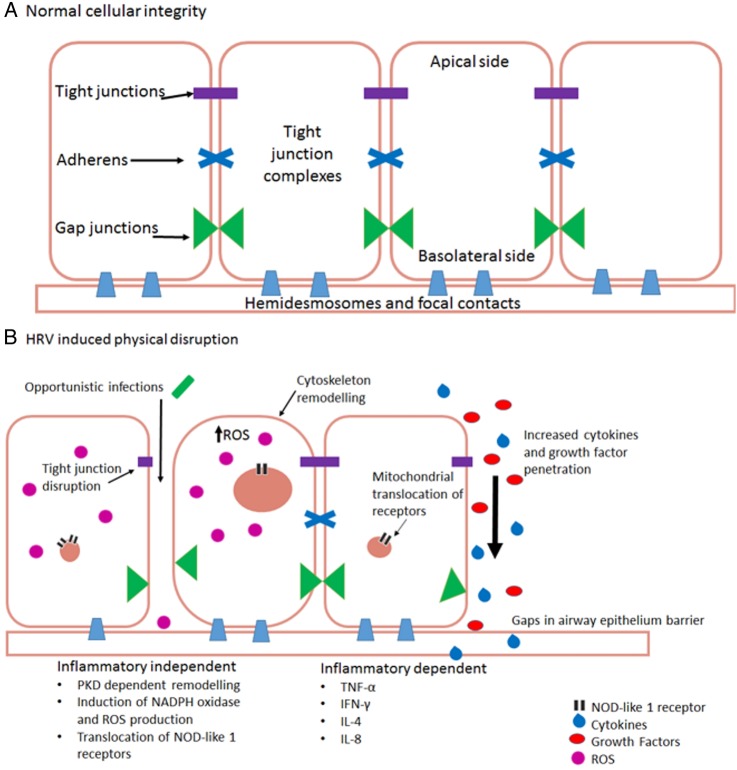
Figure 1.
(A) Normal healthy airway barrier. In a healthy airway, cells are connected together by tight junction complexes including tight junctions, adherens and gap junctions. Cells are attached to basement membranes by hemidesmosomes and focal contacts. Barrier permeability is minimal and tightly regulated to prevent the excessive release of essential molecules, ions and proteins. The barrier is protective against infection. (B) Human rhinovirus infection in airway epithelial cells. There are two main ways that HRV causes physical disruption of airway barriers, inflammatory-dependent and independent. Both replicating and non-replicating viruses can interfere with airway membrane integrity by disrupting tight junction complexes. This causes a reduction of transepithelial resistance with the potential consequence of contracting a secondary infection. Cytoskeletal remodelling mediated by protein kinase D (PKD) causes an actin reorganisation within infected cells, altering their structure and integrity, further allowing cells to lose their adjoining contacts. Replicating HRV produces a dsRNA intermediate structure which can interact and activate NOD-like receptor X-1 ultimately producing reactive oxygen species. These alone are capable of reducing transepithelial resistance and barrier disruption. Loss of gap junctions and cells leaves gaps within epithelial layers. These allow cytokines, growth factors, immune cells and further viral particles to penetrate deeper layers within the airways, causing dysregulation of cellular signalling. This dysregulation causes further upregulation of various molecules including growth factors, which, in turn, can lead to an increase of receptor expression, such as transient receptor potential channels which have a prolific effect to cause cough (TNF, tumour necrosis factor; IFN, interferon; IL, interleukin).