Abstract
Patient: Female, 62
Final Diagnosis: Gossypiboma
Symptoms: Abdominal discomfort
Medication: —
Clinical Procedure: Surgery
Specialty: Surgery
Objective:
Challenging differential diagnosis
Background:
Gossypiboma is the term for a surgical complication resulting from foreign materials such as a surgical sponge or gauze that was accidentally left inside a patient’s body.
Case Report:
Here, we report the case of a 62-year-old woman with gossypiboma. She underwent surgery due to an abdominal mass that was preoperatively considered a tumor. Intra-postoperatively, it was diagnosed as gossypiboma.
Conclusions:
For the prevention of gossypiboma during the pre-operative and post-operative periods, counting sponges and surgical equipment must be done very carefully. If there is any doubt postoperatively, direct abdominal imaging may be helpful.
MeSH Keywords: Abdomen, Diagnostic Errors, Gossypium
Background
Gossypiboma is the term for a surgical complication resulting from foreign materials such as a surgical sponge or gauze that was accidentally left inside a patient’s body. Although not frequent, major intra-abdominal operations are the procedure in which this most often occurs. This situation appears more often in developing countries that have low socioeconomic levels, and is a rare occurrence in developed countries. The situation may give rise to complications contributing to morbidity and mortality. A simple solution to prevent this mistake is to properly count the materials that are used during and at the end of the operation [1], but methods other than having the nurses count these items are necessary to prevent this rare but real complication. Gossypiboma may cause severe morbidity and even mortality in some cases. If there is a doubt postoperatively, direct abdominal imaging may be helpful.
Case Report
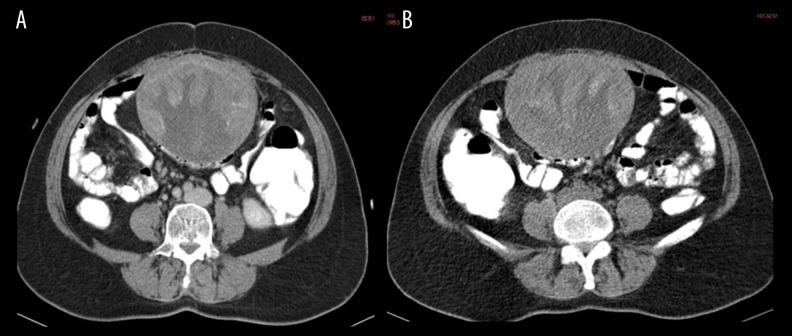
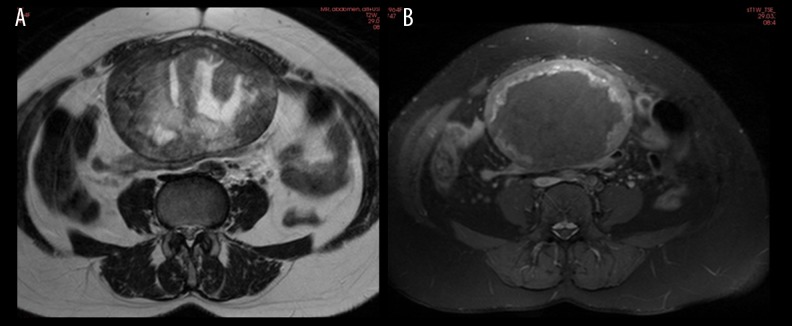
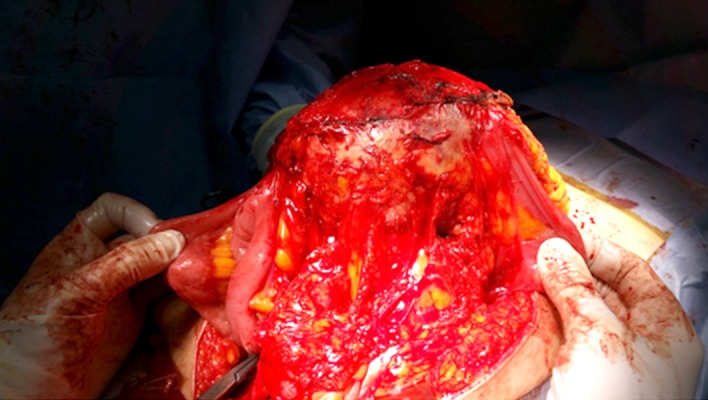
A 62-year-old woman was admitted to our hospital with the complaints of stomachache, distention, and constipation for the last 5 years. During physical examination her vital signs were normal, but a bulk at the abdominal midline and under the umbilicus was found and there was tenderness at the epigastrium of the abdomen. She had a medical history of myomectomy and a Pfannenstiel incision scar was observed. She had been operated on 20 years ago and there were no postoperative complications. As a comorbidity, she had hypertension. A well-circumscribed solid bulky lesion, 12×11.5×9 cm in size, was located via computed tomography (CT) scan at the abdominal midline, near the abdominal wall (Figure 1). Using contrast-unenhanced abdominal CT, a heterogeneous bulky lesion that consisted of hypodense cystic and hyperdense solid components was detected. After the introduction of the contrast agent, no significant contrast agent uptake by the bulk lesion was detected. It was suspected that the patient had a malign mesenchymal tumor. A heterogeneous non-specific solid bulky lesion with hypointense and hyperintense components, as well as cystic degenerative components at its center, was detected via magnetic resonance imaging (MRI) (Figure 2). After the introduction of contrast agent, some of the peripheral contrast uptake was seen in arterial-phase images. In the late-phase venous images, a bulky lesion was observed homogenously with enhancing contrast agent. Laparotomy was performed and there was a high level of intra-abdominal adhesion. Adhesions were separated via obtuse and sharp dissections. The bulk, which was approximately 10 cm in size, was located at the abdominal midline and was highly adhered to the segments of the small intestine (Figure 3). The bulk was resected with 40 cm of the small intestine (Figure 4) and sent to the Pathology Department for diagnosis (Figure 5). It was reported to be a textiloma at pathological examination.
Figure 1.
A well-circumscribed solid bulky lesion 12×11.5×9 cm in size, was located at the abdominal midline, near the abdominal wall, via computed tomography (CT) scan. (A) Using contrast-unenhanced abdominal CT, a heterogeneous bulky lesion consisting of hypodense cystic and hyperdense solid components was detected. (B) After the introduction of the contrast agent, no significant contrast agent uptake at the bulky lesion was detected.
Figure 2.
A heterogeneous non-specific solid bulky lesion that has hypointense and hyperintense components and also cystic degenerative components at its center was seen in contrast-enhanced dynamic superior and inferior MRI scan images [fat-suppressed (A) coronal and (B) sagittal T2A scan images].
Figure 3.
Intraoperative view of gossypiboma.
Figure 4.

Macroscopic view of gossypiboma.
Figure 5.

Macroscopic view of gossypiboma.
Discussion
Because surgeons hide these types of situations, the frequency of gossypiboma is not exactly known. Gossypiboma also creates a legal problem for surgeons, since these situations can result in mortality and morbidity [1]. The most common complications of gossypiboma are adhesions, abscesses, and fistulas. Gossypiboma may give rise to 2 types of pathologic reactions: (i) exudative response, which may cause abscess formation; and (ii) granuloma formation, which may occur as a response to foreign material [2]. The exudative response is generally seen during the early postoperative period. Persistent intraabdominal abscess after treatment helps the physician to diagnose gossypiboma. Granuloma formation is generally seen during the late postoperative period, even years and decades later, as seen in our case. It mimics malignancy. As observed from the radiologic analysis, our case had similarities with a mesenchymal tumor [3–5]. CT is the most common method for the diagnosis of gossypiboma [6] and resection of the lesion via laparoscopic procedure or open surgery is the classical treatment method [7].
Conclusions
For the prevention of gossypiboma at the pre-operative and post-operative periods, counting sponges and surgical equipment must be done very carefully, and the universal rules that were published by American College of Surgeons in 2005 must be strictly followed [8]. If there is a doubt postoperatively, direct abdominal imaging may be helpful [9].
References:
- 1.Malhotra MK. Migratory surgical gossypiboma-cause of iatrogenic perforation: Case report with review of literature. Niger J Surg. 2012;18:27–29. doi: 10.4103/1117-6806.95486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Srivastava KN, Agarwal A. Gossypiboma posing as a diagnostic dilemma: A case report and review of the literature. Case Rep Surg. 2014;2014:713428. doi: 10.1155/2014/713428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Isik A, Okan I, Firat D, Idiz O. A rare complication of colorectal surgery and its management: Chylous leakage. Cir Esp. 2015;93:118–20. doi: 10.1016/j.ciresp.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 4.Isik A, Firat D, Peker K, et al. A case report of esophageal perforation: Complication of nasogastric tube placement. Am J Case Rep. 2014;15:168–71. doi: 10.12659/AJCR.890260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Işik A, Deniz Firat Y, Peker K, et al. How could such a wide piece of tree root pass through the narrow pyloric orifice? An extremely rare case. Am J Case Rep. 2014;15:284–87. doi: 10.12659/AJCR.890713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aminian A. Gossypiboma: a case report. Cases J. 2008;1:220. doi: 10.1186/1757-1626-1-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karahasanoglu T, Unal E, Memisoglu K, et al. Laparoscopic removal of a retained surgical instrument. J Laparoendosc Adv Surg Tech A. 2004;14:241–43. doi: 10.1089/lap.2004.14.241. [DOI] [PubMed] [Google Scholar]
- 8.American College of Surgeons, authors Statement on the prevention of retained foreign bodies after surgery. Bull Am Coll Surg. 2005;90:15–16. [PubMed] [Google Scholar]
- 9.Kreis BE, de Mol van Otterloo AJ, Kreis RW. Open abdomen management: A review of its history and a proposed management algorithm. Med Sci Monit. 2013;19:524–33. doi: 10.12659/MSM.883966. [DOI] [PMC free article] [PubMed] [Google Scholar]