ABSTRACT
Agriculture has undergone profound changes, and farmers face a wide variety of stressors. Our aim was to study the levels of anxiety and depression symptoms among Norwegian farmers compared with other occupational groups. Working participants in the HUNT3 Survey (The Nord-Trøndelag Health Study, 2006–2008), aged 19–66.9 years, were included in this cross-sectional study. We compared farmers (women, n = 317; men, n = 1,100) with HUNT3 participants working in other occupational groups (women, n = 13,429; men, n = 10,026), classified according to socioeconomic status. We used the Hospital Anxiety and Depression Scale (HADS) to measure anxiety and depression symptoms. Both male and female farmers had higher levels of depression symptoms than the general working population, but the levels of anxiety symptoms did not differ. The differences in depression symptom levels between farmers and the general working population increased with age. In an age-adjusted logistic regression analysis, the odds ratio (OR) for depression caseness (HADS-D ≥8) when compared with the general working population was 1.49 (95% confidence interval [CI]: 1.22–1.83) in men and 1.29 (95% CI: 0.85–1.95) in women. Male farmers had a higher OR of depression caseness than any other occupational group (OR = 1.94, 95% CI: 1.52–2.49, using higher-grade professionals as reference). Female farmers had an OR similar to men (2.00, 95% CI: 1.26–3.17), but lower than other manual occupations. We found that farmers had high levels of depression symptoms and average levels of anxiety symptoms compared with other occupational groups.
KEYWORDS: Agricultural workers, anxiety, cross-sectional studies, depression, socioeconomic factors
Introduction
Few occupations have undergone more profound changes over the past few decades than those experienced by farmers, and the number of Norwegian farmers has decreased. 1 Despite geographical and political differences, the same trends can be seen in most industrialized countries,2, 3 and the demands and stressors farmers face in a rapidly changing sector appear to be similar across borders. 4
Occupational stressors that are unique to farmers, such as physical environment, family structure, farm economy, bureaucracy, and other uncertainties associated with farming,5, 6 may have been aggravated in recent years because of the structural and economic changes in agriculture. 6 These stressors may be hazardous to mental health, but research has so far not provided a clear answer to the question of whether or not the mental health of farmers differs from that of the general working population. 7 Psychiatric disorders are commonly a contributing factor to suicide, 8 and farmers are at increased risk of suicide. 9 , 10 Mental illness appears to be particularly stigmatizing in farming communities, and farmers seem reluctant to contact the health care system for help for mental health problems. 5 , 6 Very limited research is available on the mental health of female farmers, but there is some evidence to suggest that female farmers experience more psychological distress than their male colleagues. 11 – 13
The HUNT Study (Helseundersøkelsen i Nord-Trøndelag, the Nord-Trøndelag Health Study) is one of the largest health studies ever performed. It has been undertaken in Nord-Trøndelag County, Norway, since the 1980s. Nord-Trøndelag County has a substantial agricultural production, and the HUNT Study represents a unique opportunity to study the mental health of farmers.
We wanted to answer the following research question: Do the levels of anxiety and depression symptoms in Norwegian farmers differ from those of other occupational groups?
Materials and methods
The HUNT Study includes large total population-based cohorts from Nord-Trøndelag County: HUNT1 (1984–1986), HUNT2 (1995–1997), and HUNT3 (2006–2008), with 125,000 participants in total. 14 – 16 The county is largely rural, the largest of the six main towns has a population of only 21,000.
All 93,860 residents of Nord-Trøndelag aged 20 years and above were invited to take part in HUNT3. In all, 50,805 (54.1%) participated. Information from the participants was gathered through various questionnaires, an interview at the health examination sites, and measurements such as weight and height. 16
The inclusion criteria of our study were (1) age 19–66.9 years at the time of participation in HUNT3; (2) being occupationally active; (3) having valid Hospital Anxiety and Depression Scale (HADS) scores, on both the anxiety (HADS-A) and depression (HADS-D) subscales; and (4) having an identifiable occupation (Figure 1). The statutory retirement age in Norway is 67 years. Being 66.9 years of age at the time of participation in HUNT3 was used as cutoff, yielding 40,257 persons aged 19–66.9 years.
Figure 1.
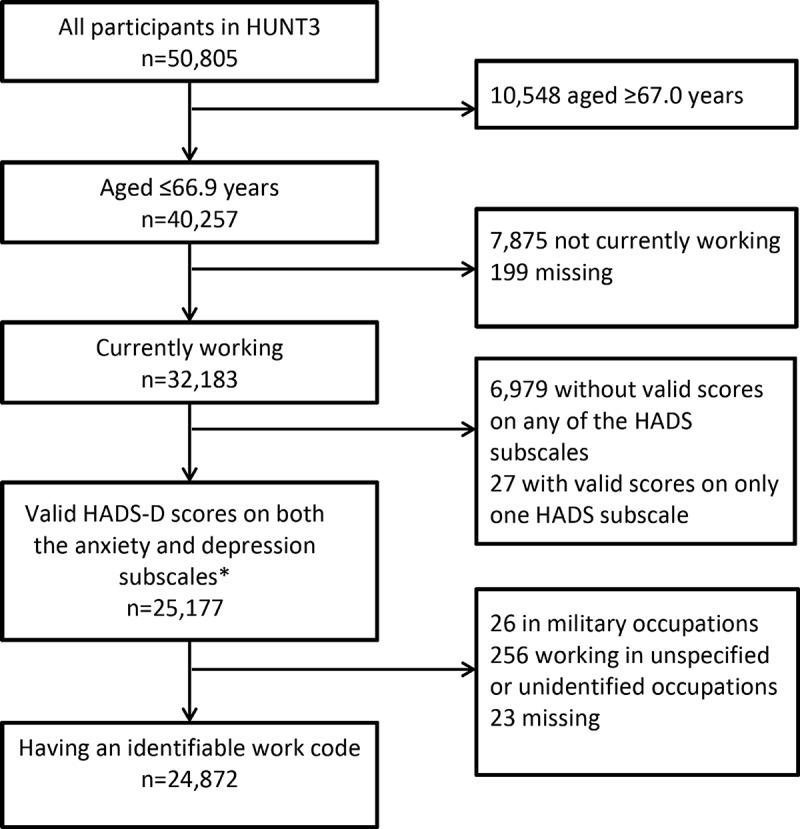
Flowchart showing the selection of study participants. HUNT3 (2006–2008). *Valid scores defined as having answered at least 5 out of 7 questions on both HADS subscales.
In the interview, participants aged 70 or younger were asked the question: “Are you currently working, a student or working at home?” Each of the three had the response alternatives “yes” and “no.” According to the questionnaire guidelines, “working” included everyone who earned an income. “Working at home” included people who cared for children or others in their home, without earning an income. We defined everyone who answered “yes” to “working” (n = 32,183) as being occupationally active, regardless of whether they worked full-time or part-time. We excluded 7,875 who answered “no” and 199 missing.
The HADS is a screening tool, consisting of 14 questions on a self-administered questionnaire. There are seven questions related to anxiety and seven questions related to depression. Each question is scored on a scale of 0–3, yielding two subscales with a range of 0–21, with higher scores indicating higher levels of distress. 17 We defined valid HADS scores as having answered at least 5 out of the 7 questions on both HADS-A and HADS-D. If a respondent had answered 5 or 6 questions on a subscale, the respondent’s total score was multiplied by 7/5 or 7/6, respectively. We used a score of 8 or above as the cutoff for “caseness” on each subscale, indicating a possible and probable case of anxiety or depression. This cutoff gives an optimal balance between sensitivity and specificity, both of which are around 0.80 on both subscales. 18 We excluded 6,979 who did not have a valid score on any of the subscales, and 27 who had a valid score on only one subscale, leaving 25,177 participants.
The first questionnaire (Q1) was mailed to all residents of Nord-Trøndelag and was handed in at the health examination sites at the time of participation. The second questionnaire (Q2) was handed out at the health examination site and returned by mail, resulting in a lower response rate. The HADS questions were on Q2, and of the 7,006 without valid anxiety and depression scores, 6,749 (96.3%) had not returned Q2. The proportion of respondents with valid HADS scores was very similar in farmers and nonfarmers.
Information about a participant’s work title was gathered at the interview. If a participant had more than one job, only the main occupation was recorded. The work titles were classified manually by Statistics Norway according to the STYRK (Standard for yrkesklassifisering, Standard Classification of Occupations) work codes. 19 The STYRK is based on ISCO-88(COM), which is the European Union version of the International Standard Classification of Occupations (ISCO-88). 20 The STYRK work codes are hierarchal. The first number in the four-digit code provides information about the main occupational category, the second provides further subdivision, and so on. There were 1,168 working respondents (including respondents who were outside of the age range or without valid HADS scores), recorded with a work title, who had not been classified by Statistics Norway. They were classified manually into one of the nine main subgroups given by the first digit in the four-digit STYRK code. Work titles that could not be readily placed into one of the nine groups were coded as “unidentified.” We excluded 305 respondents who were in military occupations (n = 26), missing (n = 23), or in unspecified or unidentified occupations (n = 256), yielding a final study population of 24,872.
Using the first digit of the STYRK codes, the study population was classified into six groups based on a simplified version of the Erikson-Goldthorpe-Portocarero (EGP) social class scheme. 21 We defined the study group “farmers” (n = 1,598) as the following occupations with STYRK codes starting with 6 (“Occupation in farming, forestry and fisheries”): “6111 Field crop and vegetable growers” (n = 83), “6121 Dairy and livestock producers” (n = 664), “6122 Poultry producers” (n = 7), “6129 Animal producers and related workers not elsewhere classified” (n = 6), and “6130 Crop and animal producers” (n = 838). When going through the work titles of the farmers manually, several smaller subgroups were identified. Reindeer owners (n = 18), any work title that implied that the respondent was a farm worker and not a self-owning farmer (n = 133), and respondents with work titles suggesting that they were wrongly classified as farmers (n = 30) were reclassified. The remaining 1,417 respondents all had a variation of “farmer” as their work title.
STYRK codes starting with 1 (“Legislators, senior officials and managers,” n = 1,963) and 2 (“Academia,” n = 2,636) were combined in a simplified EGP group labeled “Higher-grade professionals” (n = 4,599). STYRK codes starting with 3 (“Occupation with shorter education from college/university/tech. school,” n = 5,949) were labeled “Lower-grade professionals.” STYRK codes starting with 4 (“Office/service occupations,” n = 1,718) and 5 (“Sale/service/care occupations,” n = 5,613) were labeled “Routine non-manual employees” (n = 7,331). STYRK codes starting with 7 (“Trade/craft occupation,” n = 2,427) and 8 (“machine operator/transport worker,” n = 1,696) were labeled “Lower-grade technicians, supervisors of manual workers, skilled manual workers,” from here on referred to as “skilled manual workers.” In addition, “6112 Market gardeners” (n = 83) and “6310 Fish farmers” (n = 70) were included, yielding a total of 4,276 skilled manual workers. STYRK codes starting with 9 (“Occupation that doesn’t require education,” n = 1,047) were classified as “Unskilled manual workers.” In addition, “6411 Fishery workers” (n = 36), “6210 Forestry workers” (n = 66), as well as the previously mentioned farm workers (n = 133) and reindeer owners (n = 18) were classified as unskilled manual workers, making the total n = 1,300.
We compared farmers with the combined group of HUNT3 participants working in all other occupations (AOO), as well as dividing the AOO group according to the EGP scheme. We investigated the association between occupation and depression by using HADS-D caseness as the dependent variable in two different logistic regression models. HADS-A caseness was not tested, as no differences between farmers and the other occupational groups were found in the initial analyses. In the first model, we compared farmers with the AOO group by including being a farmer as a dichotomous variable. In the second model, we put farmers into a socioeconomic context by including EGP group as a categorical variable, using higher-grade professionals as the reference category.
We used directed acyclic graphs (DAGs) to identify possible confounders and mediators. 22 The analyses were stratified by sex to eliminate sex as a confounder and to allow investigation of possible sex differences. We considered age as a confounder and adjusted for it by entering age as a categorical variable in 10-year increments in both models. In the first model, we also adjusted for education, using data from the National Education Database that were matched with HUNT3 data by using the 11-digit unique national identification number. Education was classified according to the highest level of education completed: Higher education (≥3 years), secondary school, or not having graduated from secondary school. In the second model, we did not adjust for education, as we considered education to be a mediator in the relationship between the exposure variable occupation (as a measure of socioeconomic status) and the outcome variable depression. We also considered other variables, such as physical health, social background, and work-related variables, to be mediators and did not adjust for them.
The analyses were conducted using IBM SPSS Statistics 21 (IBM, Armonk, NY, USA). The forest plot was made using Metadata Viewer version 1.05. 23
Results
Characteristics of the study group and the AOO group are shown in Appendix 1. HADS-A and HADS-D mean scores and prevalences of anxiety and depression caseness are shown in Table 1. Farmers had a higher mean HADS-D score and a higher prevalence of depression caseness than the general working population, but the levels of anxiety symptoms did not differ. In the age-adjusted logistic regression analysis, male farmers (125 cases) had an odds ratio (OR) of depression caseness of 1.49 (95% confidence interval [CI]: 1.22–1.83) compared with the AOO group (1033 cases). The OR for female farmers (25 cases) was 1.29 (95% CI: 0.85–1.95) compared with the AOO group (828 cases). When adjusting for age and education, the ORs fell to 1.35 (95% CI: 1.10–1.65) in men and 1.21 (95% CI: 0.80–1.83) in women. Results of the logistic regression model with EGP groups are shown in Figure 2. Male farmers had the highest level of depression symptoms of any occupational group in our study.
Table 1.
HADS-A and HADS-D Means and Percentage of HADS Caseness, Working Participants of HUNT3 (2006–2008), Aged 19–66 Years.
| Men |
Women |
|||||||
|---|---|---|---|---|---|---|---|---|
| Profession | n | Mean | 95% CI | Caseness* | n | Mean | 95% CI | Caseness* |
| HADS-A | ||||||||
| Farmers | 1,100 | 3.6 | 3.5–3.8 | 11.4 | 317 | 4.4 | 4.0–4.8 | 16.4 |
| All other occupations | 10,026 | 3.6 | 3.5–3.6 | 10.3 | 13,429 | 4.2 | 4.1–4.3 | 15.9 |
| Higher-grade professionals | 2,456 | 3.5 | 3.4–3.6 | 9.5 | 2,143 | 3.8 | 3.7–3.9 | 11.9 |
| Lower-grade professionals | 2,063 | 3.4 | 3.3–3.6 | 10.0 | 3,886 | 3.8 | 3.7–3.9 | 13.2 |
| Routine nonmanual workers | 1,391 | 3.8 | 3.6–3.9 | 12.7 | 5,940 | 4.5 | 4.4–4.5 | 17.8 |
| Skilled manual workers | 3,737 | 3.6 | 3.6–3.7 | 10.1 | 539 | 4.8 | 4.5–5.1 | 22.6 |
| Unskilled manual workers | 379 | 3.7 | 3.4–4.0 | 10.0 | 921 | 4.7 | 4.5–4.9 | 19.9 |
| HADS-D | ||||||||
| Farmers | 1,100 | 3.8 | 3.7–4.0 | 11.4 | 317 | 3.3 | 3.0–3.6 | 7.9 |
| All other occupations | 10,026 | 3.1 | 3.1–3.2 | 7.7 | 13,429 | 2.7 | 2.7–2.7 | 6.2 |
| Higher-grade professionals | 2,456 | 2.8 | 2.7–2.9 | 6.2 | 2,143 | 2.4 | 2.3–2.5 | 4.1 |
| Lower-grade professionals | 2,063 | 2.9 | 2.8–3.0 | 6.6 | 3,886 | 2.4 | 2.3–2.5 | 5.3 |
| Routine nonmanual workers | 1,391 | 3.2 | 3.1–3.4 | 8.3 | 5,940 | 2.9 | 2.8–2.9 | 6.6 |
| Skilled manual workers | 3,737 | 3.4 | 3.3–3.5 | 9.2 | 539 | 3.4 | 3.2–3.7 | 10.4 |
| Unskilled manual workers | 379 | 3.3 | 3.1–3.6 | 7.1 | 921 | 3.2 | 3.0–3.4 | 9.3 |
Note. HADS = Hospital Anxiety and Depression Scale.
*Percentage of the total. Caseness was defined as a score of ≥8 on the HADS-A or HADS-D subscale.
Figure 2.
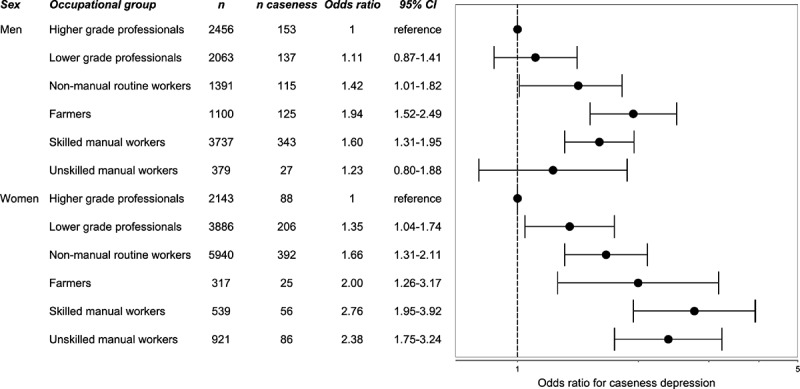
Odds ratios for caseness of depression (HADS-D ≥8), stratified by sex and adjusted for age. The HUNT3 Survey (2006–2008).
The results of age-stratified analyses are shown in Figure 3. The absolute differences in mean HADS-A scores between farmers and the AOO group were minor for men and women, as well as in all age groups (Figure 3A). The absolute differences in mean HADS-D scores between farmers and the AOO group increased with increasing age (Figure 3B).
Figure 3.
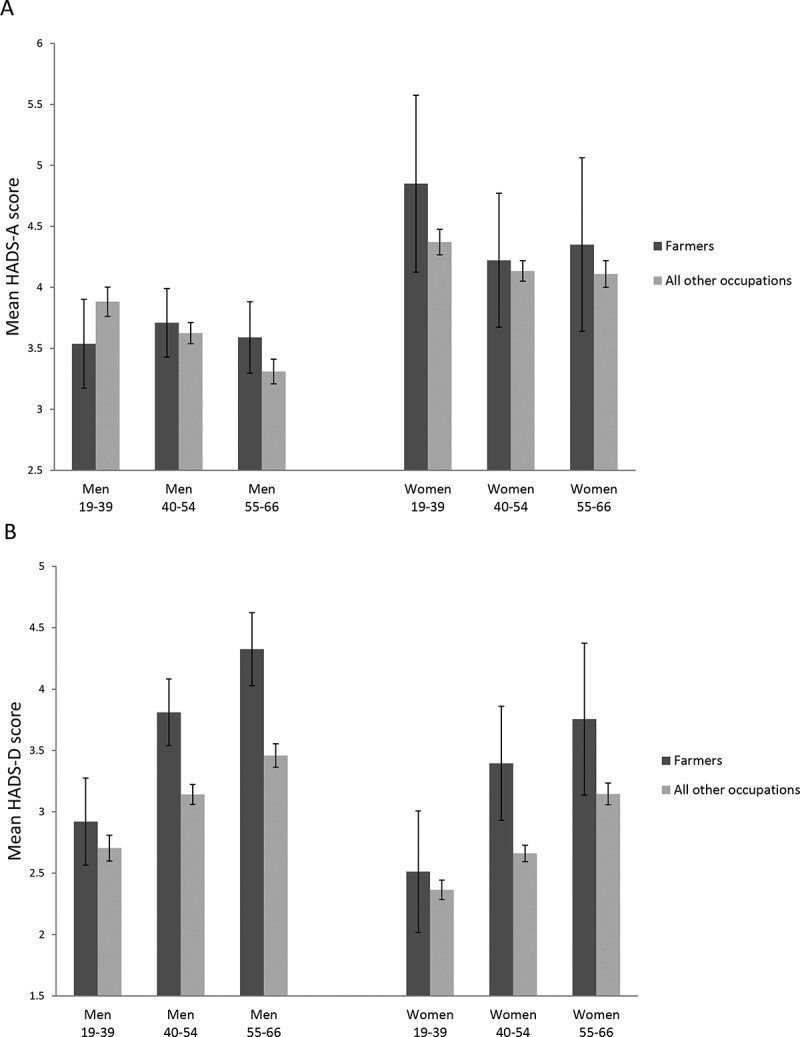
(A) Mean HADS-A scores stratified by sex and age group. (B) Mean HADS-D scores stratified by sex and age group. The HUNT3 Survey (2006–2008). Error bars represent 95% confidence intervals.
Discussion
We found that farmers had a higher prevalence of depression symptoms than the general working population. Although we cannot infer causality in a cross-sectional study, this may be an indication of the structural pressure farmers are under.
The size of HUNT3 made it possible to look at the mental health of farmers from a socioeconomic perspective. Numerous studies suggest a stepwise social gradient in health, 24 including depression, 25 with groups of low socioeconomic status being at higher risk. Farmers are an occupational group that is not immediately easy to put into a socioeconomic context. Farming is a manual occupation without a formal education requirement, and farmers are commonly exposed to a number of work conditions that are generally considered unfavorable, such as long working hours, monotonous tasks, and a dangerous physical work environment. 26 In addition to physically demanding work, farming requires diverse skills, such as administration and economy. Farmers do, however, have a great deal of autonomy at work. 26 Norwegian farms are generally family-owned, and farmers are almost always self-employed. Control has been shown to be crucial for health, 24 and in Karasek’s job demand-control model, the interaction between high job demands and low decision latitude predicts mental distress. 27 Even though farmers may face high demands, they also have high job decision latitude. However, insecurity related to future employment can have negative effects on workers’ health,28, 29 and we propose that working in agriculture during a period of major changes may have led to a perceived lack of control and a feeling of job insecurity.
A Norwegian study from the Health Survey of Hordaland found that male agricultural workers (ISCO-88(COM) 6.1, which includes the STYRK codes defined as “farmers” in our study) had the highest HADS-D level of all the occupational groups in the study, 30 and our results support their finding. The causes of the high depression level of in particular male farmers cannot be identified in a cross-sectional study and cannot be readily explained. A perceived lack of control or job insecurity may be two of many possible explanations. Using a screening tool instead of diagnoses of anxiety and depression may be another. The HADS is not a diagnostic tool, and high scores on the depression scale could be caused by transient factors such as physical illness or going through divorce and not a diagnosis of depression. However, we did not find any evidence of farmers having more problems related to physical health, family problems, or lack of social network than the skilled or unskilled manual workers (results not shown). The farmers in our study had comparable education levels to the skilled and unskilled manual workers, and farmers had more favorable lifestyle indicators, such as smoking and alcohol consumption (results not shown).
Comparing farmers with other occupational groups in a cross-sectional study is particularly challenging because the selection out of the occupation is probably higher than in most other occupations and may also be related to the outcome in our study. The number of farmers in Nord-Trøndelag County decreased by more than 30 % between 1999 and 2008 alone. 1 The high proportion of farmers who reported working more than 40 hours per week is an indication that being in good health is crucial to be able to stay in farming, and it is also an indicator of the general pressure the occupational group is under. Farmers who left farming in favor of an off-farm job may have had a different health status than the ones who stayed in the profession, creating a selection bias of unknown direction and magnitude. We found that the differences in depression levels between farmers and the AOO group increased with age. Young, healthy, well-educated farmers may have found it easier to find an off-farm job than older colleagues with higher depression and anxiety levels. Factors such as aging making physically challenging tasks more difficult, insecurity relating to farm succession, or a lack of other options but to stay on the farm 31 may also play a role, but we do not have data available on them. The increasing depression levels with age could also be a reflection of a cohort effect. Another premature way out of the farming profession is disability pension. One might hypothesize that the selection process of farmers with depressive symptoms being awarded disability pensions might differ from other occupations, because of factors such as the previously mentioned insecurity related to farm succession, their status as self-employed, or other reasons, but this is not known.
The mean levels of depression found in our study were well below the cutoff for caseness, as would be expected in a working cohort. The absolute differences in mean levels between the different occupational groups were relatively modest. Farmers reported having the same quality of life as the AOO group, which could be an indication that a higher level of depression symptoms is not perceived as a medical problem. However, unipolar depressive disorders are estimated to be the leading cause of burden of disease in high-income countries (measured by disability-adjusted life years [DALYs]), and number three behind ischemic heart disease and cerebrovascular disease in the European region, 32 indicating both the prevalence of unipolar depressive disorders and the impact they have on individuals. Our findings indicate that there could be a considerable number of excess cases of depression among farmers compared with other occupational groups.
Norway is a welfare state with universal health care, including for mental illness. 33 In addition, the national occupational health care organization for farmers gives its members access to occupational health care. 34 However, despite universal health care access and having a higher prevalence of depression symptoms, we found that a lower proportion of farmers reported having sought help for mental health problems than in the AOO group. Even though “mental health problems” includes a wide range of conditions in addition to depression, our findings support the existing literature in that farmers may be more reluctant to seek help for mental health problems.5,6 The help-seeking behavior of farmers appears to differ for physical health conditions as well, as a smaller proportion of farmers had visited a doctor in the last 12 months than in the AOO group, even though more farmers reported having chronic pain or a long-lasting illness or injury. In a study of workers from all the 27 EU states, participants working in the agricultural sector reported the highest impact of work on health of any of the sectors in the study, 26 and this apparent discrepancy between the help-seeking behavior of farmers and their needs for health services constitutes a challenge for the health care system.
The population of Nord-Trøndelag County follows Norwegian trends in disability 35 and cause-specific mortality 36 closely, and our results should be generalizable to other parts of Norway. The international trends in agriculture are similar to those seen in Norway, 3 but the extent to which our results are generalizable to farming populations outside Norway is unknown. However, we believe our results could be of interest internationally.
Strengths and limitations
The HUNT3 survey is a large, total population-based cross-sectional study with a relatively high participation rate, and we used a validated screening instrument to measure anxiety and depression symptoms. Our study included a high number of farmers compared with other studies in the field, including women. The questions on occupation and mental health symptoms were included in a large general health survey, ruling out reporting bias for the relationship between being a farmer and symptom levels. Reports of psychological stress are higher in occupational than in population studies, suggesting that participants may overreport measures of psychological stress when they know they have been recruited to a study based on their occupation. 37
We relied on self-report data, which may be a potential weakness of our study. An alternative approach would be to use psychiatric diagnoses given by a physician. However, if the help-seeking behavior of farmers differs from other occupational groups,5, 6 using primary care or hospital data could have resulted in an underestimation of the true prevalence of anxiety and depression in farmers. Another weakness of our study is the inability to separate full-time from part-time farmers. We do not know if the farmers in our study had another job outside the farm, as we only have information on the self-reported main occupation of the HUNT3 participants.
The EGP scheme classifies occupations by using characteristics of the employment relation, such as levels of of independence, delegated authority, and job control. There is not, however, an explicit hierarchical rank in the EGP scheme; thus, it may not capture a social gradient in health. 38
A HUNT3 nonparticipation study found that nonparticipants had lower socioeconomic status than participants, as well as a higher prevalence of psychiatric disorders. There are indications that depression may be a more important restricting factor for participation in HUNT3 than anxiety. 39 Selection bias is likely to result in an underestimation of the differences between socioeconomic groups, but the magnitude cannot be assessed.
Conclusion
Our hypothesis for this study was that working in an industry that has been under long-term structural and economic pressure may be detrimental to mental health. Our results indicate that this might be the case, although we cannot infer causality in a cross-sectional study. More studies of longitudinal and qualitative design are needed to investigate the effects changes in agricultural policy-making, economy, and technology may have on the mental health of farmers. Our results also emphasize the continued need for preventive occupational health strategies in agriculture, as well as finding ways to address the apparent difference in the healthcare-seeking behavior of farmers compared with the general population, especially for mental illness.
Acknowledgments
The Nord-Trøndelag Health Study (HUNT) is a collaboration between HUNT Research Center (Faculty of Medicine, Norwegian University of Science and Technology NTNU), Nord-Trøndelag County Council, Central Norway Health Authority, and the Norwegian Institute of Public Health.
Funding
The project was funded by the Research Levy on Agricultural Products/the Agricultural Agreement Research Fund, Norway. The funders had no involvement in study design, data collection and analysis, preparation of the manuscript, or the decision to publish.
Ethics approval: All participants of HUNT3 provided written informed consent. The HUNT Study was approved by the Regional Committee for Medical and Health Research Ethics (REC Central), as was the present study (2012/1359).
Appendix 1.
Characteristics of the study participants. Working participants of HUNT3 (2006-2008) aged 19-66 years. [SD = standard deviation; BMI = body mass index].
| Men |
Women |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Farmers |
All other occupational groups |
Farmers |
All other occupational groups |
|||||||||||||||||
| n | %* | mean | SD | range | n | %* | mean | SD | range | n | %* | mean | SD | range | n | %* | mean | SD | range | |
| Number of study participants | 1100 | 10026 | 317 | 13429 | ||||||||||||||||
| Age, mean (+/- SD) | 1100 | 50.0 | 9.8 | 21.7 – 66.8 | 10026 | 48.1 | 10.8 | 19.2 – 66.9 | 317 | 48.0 | 10.3 | 20.9 – 66.5 | 13429 | 46.5 | 11.0 | 19.2 – 66.9 | ||||
| Education | ||||||||||||||||||||
| Not graduated from secondary school | 684 | 62.2 | 3257 | 32.5 | 185 | 58.4 | 4988 | 37.1 | ||||||||||||
| Secondary school graduate | 339 | 30.8 | 4472 | 44.6 | 94 | 29.7 | 4272 | 31.8 | ||||||||||||
| College/university graduate, three years or more | 77 | 7.0 | 2297 | 22.9 | 38 | 12.0 | 4169 | 31.0 | ||||||||||||
| Health | ||||||||||||||||||||
| Quality of life - “very satisfied”, “satisfied” or “somewhat satisfied” | 940 | 87.4 | 8886 | 89.4 | 274 | 87.8 | 11676 | 87.8 | ||||||||||||
| Self-reported health - “not so good” or “poor” | 188 | 17.7 | 1530 | 15.5 | 74 | 24.0 | 2408 | 18.4 | ||||||||||||
| Having a long-lasting illness or injury (physical or mental) which impairs daily life functioning** | 282 | 26.7 | 2328 | 23.8 | 85 | 28.0 | 3148 | 24.1 | ||||||||||||
| Long-lasting impairment because of physical illness (slight, moderate, severe)** | 174 | 15.8 | 1510 | 15.1 | 60 | 18.9 | 2317 | 17.3 | ||||||||||||
| Long-lasting impairment because of mental health problems (slight, moderate, severe)** | 37 | 3.4 | 451 | 4.5 | 11 | 3.5 | 634 | 4.7 | ||||||||||||
| Current physical pain which has lasted more than six months | 379 | 35.4 | 3057 | 31.0 | 124 | 40.3 | 4702 | 35.9 | ||||||||||||
| Sick leave certificate by a doctor in the last 12 months | 331 | 30.7 | 2727 | 27.5 | 109 | 34.9 | 5056 | 38.1 | ||||||||||||
| Visited a doctor in the last 12 months*** | 570 | 64.4 | 5629 | 68.0 | 190 | 76.6 | 8815 | 81.5 | ||||||||||||
| Consultation at a psychiatric outpatient clinic in the last 12 months | 12 | 1.4 | 152 | 1.9 | 5 | 2.0 | 274 | 2.6 | ||||||||||||
| Have or have had mental health problems which you have sought help for | 77 | 7.2 | 880 | 9.0 | 40 | 13.1 | 1981 | 15.1 | ||||||||||||
| Lifestyle | ||||||||||||||||||||
| BMI | 1099 | 27.3 | 3.6 | 17.2 – 44.3 | 10013 | 27.5 | 3.6 | 16.7 – 48.9 | 317 | 27.3 | 5.0 | 18.6 – 46.1 | 13406 | 26.5 | 4.6 | 12.1 – 54.3 | ||||
| Daily smoker | 100 | 9.1 | 1364 | 13.6 | 45 | 14.2 | 2505 | 18.7 | ||||||||||||
| Exercise at least once a week | 653 | 60.8 | 7315 | 73.6 | 242 | 77.5 | 11362 | 85.3 | ||||||||||||
| May have an alcohol problem**** | 114 | 10.4 | 1593 | 15.9 | 7 | 2.2 | 577 | 4.3 | ||||||||||||
| Work | ||||||||||||||||||||
| Work part time | 59 | 5.4 | 872 | 8.7 | 70 | 22.1 | 7096 | 52.9 | ||||||||||||
| Work full time (up to 40 hours a week) | 140 | 12.7 | 5070 | 50.6 | 98 | 30.9 | 4614 | 34.4 | ||||||||||||
| Work >40 hours a week | 901 | 81.9 | 4078 | 40.7 | 149 | 47.0 | 1712 | 12.8 | ||||||||||||
* Percentage of participants who reported the indicated response alternative (s). The total number on individual variables may not add up to the total number of study participants because of missing data
** of at least one year duration
*** general practictioner, specialist outside of a hospital, hospital outpatient clinic (except psychiatric)
**** CAGE (Cut down Annoyed Guilty Eye-opener) questionnaire score ≥2 (Ewing, JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252(14):1905–07.)
Funding Statement
The project was funded by the Research Levy on Agricultural Products/the Agricultural Agreement Research Fund, Norway. The funders had no involvement in study design, data collection and analysis, preparation of the manuscript, or the decision to publish. Ethics approval: All participants of HUNT3 provided written informed consent. The HUNT Study was approved by the Regional Committee for Medical and Health Research Ethics (REC Central), as was the present study (2012/1359).
References
- Statistics Norway [Accessed Jun 25;, 2014];Structure of agriculture. Oslo-Kongsvinger: Statistics Norway. 2014 https://www.ssb.no/statistikkbanken/selecttable/hovedtabellHjem.asp?KortNavnWeb=stjord&CMSSubjectArea=jord-skog-jakt-og-fiskeri&PLanguage=1&checked=true Available at.
- Donham KJ, Thelin A. Agricultural Medicine: Occupational and Environmental Health for the Health Professions. Ames, IA: Blackwell Publishing; 2006. [Google Scholar]
- Food And Agriculture Organization of the United Nations . The State of Food and Agriculture. Rome: Food And Agriculture Organization of the United Nations; 2012. [Accessed Apr 9;, 2014]. http://www.fao.org/docrep/017/i3028e/i3028e.pdf Available at. [Google Scholar]
- Kolstrup CL, Kallioniemi M, Lundqvist P, Kymalainen HR, Stallones L, Brumby S. International perspectives on psychosocial working conditions, mental health, and stress of dairy farm operators. J Agromedicine. 2013;18:244–255. doi: 10.1080/1059924X.2013.796903. [DOI] [PubMed] [Google Scholar]
- Kallioniemi MK, Simola A, Kinnunen B, Kymäläinen HR. Stress in farm entrepreneurs. In: Langan-Fox J, Cooper CL, editors. Handbook of Stress in the Occupations. Cheltenham, UK: Edward Elgar; 2011. pp. 381–402. [Google Scholar]
- Gregoire A. The mental health of farmers. Occup Med (Lond) 2002;52:471–476. doi: 10.1093/occmed/52.8.471. [DOI] [PubMed] [Google Scholar]
- Fraser CE, Smith KB, Judd F, Humphreys JS, Fragar LJ, Henderson A. Farming and mental health problems and mental illness. Int J Soc Psychiatry. 2005;51:340–349. doi: 10.1177/0020764005060844. [DOI] [PubMed] [Google Scholar]
- Hawton K, van Heeringen K. Suicide. Lancet. 2009;373:1372–1381. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- Stallones L, Doenges T, Dik BJ, Valley MA. Occupation and suicide: Colorado, 2004–2006. Am J Ind Med. 2013;56:1290–1295. doi: 10.1002/ajim.22228. [DOI] [PubMed] [Google Scholar]
- Kennedy AJ, Maple MJ, McKay K, Brumby SA. Suicide and accidental death in Australia’s rural farming communities: a review of the literature. Rural Remote Health. 2014;14:2517. [PubMed] [Google Scholar]
- Kallioniemi MK, Simola AJK, Kymalainen HR, Vesala HT, Louhelainen JK. Mental symptoms among Finnish farm entrepreneurs. Ann Agric Environ Med. 2009;16:159–168. [PubMed] [Google Scholar]
- Thomas HV, Lewis G, Thomas DR. Mental health of British farmers. Occup Environ Med. 2003;60:181–185. doi: 10.1136/oem.60.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth NJ, Lloyd K. Stress in farmers. Int J Soc Psychiatry. 2000;46:67–73. doi: 10.1177/002076400004600108. [DOI] [PubMed] [Google Scholar]
- Holmen J, Midthjell K, Forsen L, Skjerve K, Gorseth M, Oseland A. Helseundersøkelsen i Nord-Trøndelag 1984–86. Fremmøtet og sammenlikning av dem som møtte og dem som ikke møtte [A health survey in Nord-Trøndelag 1984-86. Participation and comparison of attendants and non-attendants] Tidsskr Nor Lægeforen. 1990;110:1973–1977. [PubMed] [Google Scholar]
- Holmen J, Midthjell K, Krüger Ø et al. The Nord-Trøndelag Health Study 1995–97 (HUNT2): objectives, contents, methods and participation. Norsk Epidemiol. 2003;13:19–32. [Google Scholar]
- Krokstad S, Langhammer A, Hveem K. Cohort profile: the HUNT Study, Norway. Int J Epidemiol. 2012;42:968–977. doi: 10.1093/ije/dys095. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Norway Statistics. [Accessed Apr 9;, 2014];Standard Classification of Occupations. Oslo-Kongsvinger: Statistics Norway. 1998 http://www.ssb.no/a/publikasjoner/pdf/nos_c521/nos_c521.pdf Available at.
- International Labour Organization ISCO-88. 2014 Apr 9; http://www.ilo.org/public/english/bureau/stat/isco/isco88/ Available at. Published. 2004. Accessed.
- Erikson R, Goldthorpe JH. The Constant Flux. A Study of Class Mobility in Industrial Societies. Oxford, UK: Clarendon Press; 1992. [Google Scholar]
- Glymour MM, Greenland S. Modern Epidemiology, third edition (by: Rothman, KJ. Greenland, S. Lash, TL.) Philadelphia, PA: Lippincott Williams & Wilkins; 2008. Causal Diagrams; pp. 183–209. [Google Scholar]
- Boyles AL, Harris SF, Rooney AA, Thayer KA. Forest Plot Viewer: a new graphing tool. Epidemiology. 2011;22:746–747. doi: 10.1097/EDE.0b013e318225ba48. [DOI] [PubMed] [Google Scholar]
- Marmot M. The Status Syndrome: How Social Standing Affects Our Health and Longevity. New York: Henry Holt and Company; 2005. [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Parent-Thirion A, Macías EF, Hurley J, Vermeylen G . Fourth European Working Conditions Survey. Dublin: European Foundation for the Improvement of Living and Working Conditions; 2007. [Google Scholar]
- Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Admin Sci Q. 1979;24:285–308. [Google Scholar]
- Sverke M, Hellgren J, Naswall K. No security: a meta-analysis and review of job insecurity and its consequences. J Occup Health Psychol. 2002;7:242–264. [PubMed] [Google Scholar]
- Ferrie JE, Shipley MJ, Marmot MG, Stansfeld S, Smith GD. Health effects of anticipation of job change and non-employment: longitudinal data from the Whitehall II study. BMJ. 1995;311:1264–1269. doi: 10.1136/bmj.311.7015.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanne B, Mykletun A, Dahl AA, Moen BE, Tell GS. Occupational differences in levels of anxiety and depression: the Hordaland Health Study. J Occup Environ Med. 2003;45:628–638. doi: 10.1097/01.jom.0000069239.06498.2f. [DOI] [PubMed] [Google Scholar]
- Rogers M, Barr N, O’Callaghan Z, Brumby S, Warburton J. Healthy ageing: farming into the twilight. Rural Soc. 2013;22:251–262. [Google Scholar]
- Organization World Health. The Global Burden of Disease: 2004. Geneva: World Health Organization; 2008. Update. [Google Scholar]
- Esping-Andersen G. The Three Worlds of Welfare Capitalism. Princeton, NJ: Princeton University Press; 1990. [Google Scholar]
- Norsk Landbruksrådgivning HMS. [Accessed Dec 23;, 2014];Ås: Norsk Landbruksrådgivning HMS. 2014 http://www.lhms.no/ Available at: Published.
- Krokstad S, Johnsen R, Westin S. Social determinants of disability pension: a 10-year follow-up of 62 000 people in a Norwegian county population. Int J Epidemiol. 2002;31:1183–1191. doi: 10.1093/ije/31.6.1183. [DOI] [PubMed] [Google Scholar]
- Statistics Norway. Causes of death. Oslo-Kongsvinger: Statistics Norway . 2013. Jun 23, https://www.ssb.no/statistikkbanken/selecttable/hovedtabellHjem.asp?KortNavnWeb=dodsarsak&CMSSubjectArea=helse&PLanguage=1&checked=true Available at. Accessed. 2014. [Google Scholar]
- Goodwin L, Ben-Zion I, Fear NT, Hotopf M, Stansfeld SA, Wessely S. Are reports of psychological stress higher in occupational studies? A systematic review across occupational and population based studies. PLoS ONE. 2013;8:e78693. doi: 10.1371/journal.pone.0078693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakes JM, Kaufman JS. Methods in Social Epidemiology. San Francisco: Jossey-Bass; 2006. [Google Scholar]
- Langhammer A, Krokstad S, Romundstad P, Heggland J, Holmen J. The HUNT study: participation is associated with survival and depends on socioeconomic status, diseases and symptoms. BMC Med Res Methodol. 2012;12:143. doi: 10.1186/1471-2288-12-143. [DOI] [PMC free article] [PubMed] [Google Scholar]


