Abstract
Purpose
The Clinical Practice Guidelines instruct physicians to ask their patients about smoking and to advise against tobacco use. Physicians are urged especially to attend to racial minorities and teens because of these groups' increased susceptibility to smoking. Research on race and physician advice against smoking has produced contradictory findings. The purpose of this study is to clarify the relationships between physician communication about tobacco, race, and smoking among adolescents.
Methods
This cross-sectional retrospective study explored (1) racial differences in rates of receiving physician communication and (2) whether the relationship between physician communication and smoking among adolescents was moderated by race. Multiple measures of smoking status were used (e.g., intentions to quit, quit attempts, quits, relapse status). We employed a large (N = 5,154), predominately African American (82.9%) sample of 11th graders.
Results
Regular smokers were more likely to be screened about smoking. African Americans were more frequently advised against tobacco than Caucasians. Among African Americans, nonsmokers were most likely to be both screened and advised; among Caucasians, regular were most likely to be screened and advised. Overall, physician intervention was associated with greater benefits for young African Americans, including fewer intentions to smoke, greater likelihood of quitting, and less relapse.
Conclusions
Physician communication about smoking may hold particular promise for African American teens, reducing health disparities due to racial differences in smoking-related mortality and morbidity. Physicians should be encouraged to screen and advise all young people about tobacco, regardless of race or smoking status.
Keywords: Physicians, communication, adolescent, smoking
Caucasian teens smoke at higher rates (15.4%) than their African American peers (9.6%) and begin smoking at a significantly earlier age [1,2]. Nonetheless, African Americans experience increased health consequences from smoking relative to Caucasians [3-7; see 7 for a review of tobacco-related health disparities]. Smoking among African Americans has been associated with an increased incidence of cardiovascular disease and disproportionate morbidity and mortality from lung cancer [6-10], low birth weight, respiratory disease, and infant death compared to Caucasians [6, 11]. Notably, African American smokers are 1.5 times more likely to want to quit than Caucasian smokers [3,4,6]. However, African American adults experience significantly more difficulty with cessation than Caucasians, and this difference in success rates extends to adolescents as well: Among high school daily smokers, more African Americans (68.1%) than Caucasians (62.5%) try to quit smoking, but African Americans are less likely to succeed, 8.7% vs. 12.2%, respectively [12].
Researchers have posited biological and psychosocial theories to explain why African Americans have lower cessation rates than Caucasians. Although African Americans smoke fewer cigarettes, they absorb 30% more nicotine and metabolize nicotine more slowly than Caucasian smokers [13,14]. In addition, about 75% of African Americans smoke menthol cigarettes, which may induce greater nicotine dependence [13]. Significant psychosocial factors may also reduce African Americans' cessation rate. The tobacco industry historically has targeted African Americans with tailored advertisements, heavy marketing, the portrayal of mentholated cigarettes as a healthier product, and strategic financial contributions [14,15]. This marketing pressure is thought to contribute to African Americans' lower quit rate [12,14,16]. In addition, difficulties with health care access may influence African Americans' cessation rates [6]. For example, African Americans as a group show diminished trust in health care providers [6] and less knowledge about medications and health effects [17-19]. African Americans are also less likely to be screened for smoking or advised by their health care provider (HCP) to quit smoking [6, 20]. Lastly, African Americans utilize fewer tobacco-cessation aids during quit attempts than Caucasian smokers [6, 20].
Nonetheless, for all teens, the healthcare system is an important venue for tobacco interventions [6, 21]. For example, those who have healthcare access show lower smoking prevalence and reduced smoking over time [22]. Further, behavioral interventions in healthcare systems have been shown to have an impact on an array of health behaviors [23-25]. Whereas HCP interventions tend to have less efficacy than intensive programs, across a population, their impact can be highly significant because of their greater reach [25].
The 2008 Clinical Practice Guidelines instruct physicians to intervene with all of their patients via the 5 A's: ask about smoking status, advise patients to quit smoking, assess whether patients are ready to quit, assist the patient with quitting, and arrange follow-up visits to avoid relapses [6]. Physician advice has been shown to produce a 1 to 3% increase in adult cessation above unassisted annual quitting rates of 2 to 3% [26], and to be effective for both African Americans and Caucasian adults [6].
Most research demonstrating the impact of physician advice on quitting has been conducted with adults. However, intervention with teens has been recommended [6], and if successful, it would greatly reduce the negative effects of smoking. In a cross-sectional study, physician advice to quit was associated with increased odds that teens would make at least one quit attempt in the following year [27]. Another cross-sectional study found that physician communication was associated with a variety of positive findings among adolescents: more negative attitudes about smoking, more accurate knowledge of tobacco-related health damage, fewer intentions to continue to smoke, more intentions to quit, and more quit attempts [28].
The Clinical Practice Guidelines urge physicians to attend to both minorities and children/adolescents because of their susceptibility to smoking [6]. Thus, one might expect that physicians would intervene more often with African American adolescents than Caucasians. In support of this idea, Shelley and colleagues found that African American adolescents were about 50% more likely to receive physician counseling than Caucasian teens [27]. However, research on disparities in physician advising is sparse and inconsistent, with some studies suggesting that Caucasian teens receive more advice [29] and others finding no racial differences [30].
Methodological differences across studies may account for some of this variability in results of studies examining the patient race and physician intervention against smoking. For example, in some studies youth have been asked about communication with HCPs during the past year [27], whereas other studies did not impose a time limit for the intervention. Some investigations have inquired about any interventions from HCPs, and others have asked specifically about physician communication [30]. Studies have also varied in how physician advice was measured, with some studies utilizing physician self-report [29] and others utilizing adolescents' self-reports [27, 30].
The current retrospective observational study extended previous literature by examining racial differences in the rates of receiving varying physician tobacco interventions (i.e., no intervention, screening alone, advising alone, or both) among a predominately African American sample of adolescents. The current study was also the first study to examine whether the relationship between physician-delivered interventions and smoking among adolescents was moderated by race.
Methods
Overview and Participants
Data were drawn from the Memphis Health Project, a longitudinal observational study of adolescent smoking [31]. All 39 eligible schools participated and all students enrolled in these schools were eligible. Surveys were administered in schools by teachers, using procedures that maximized student confidentiality. Parents notified the research team if they did not want their child to participate, and students provided assent. The study was approved by the University of Memphis Institutional Review Board. Procedures are detailed elsewhere [31].
The first survey was given to a cohort of 6,967 seventh graders (79% of those eligible) and repeated annually for 9 years [31]. The characteristics of these 6,967 responders who comprised our original cohort closely matched those of the target population in this school system. The study followed this cohort longitudinally, but also allowed new students to participate so the number of participants could increase over time. Our annualized loss over the course of the study was 11.4%, a rate that compares well with other studies of inner-city adolescents [32]. The current sample comprised 5,154 students assessed in the 11th grade.
Measures and Coding of Items of Interest
Demographic variables
Self-reported race was represented as a dichotomous variable (African American [1] vs. Caucasian [0]) due to small numbers of other races. Gender (male [1] vs. female [0]) was also self-reported. A proxy method was used to estimate socioeconomic status (SES) and education. Using the most recent census data, we assigned each student the average income and education level for their zip code. Thus, students were given proxy income and education levels representing the norms for their neighborhood.
Physician communication
Physicians' interventions were measured using adolescent self-reports of (1) physician screening for tobacco use (“Has your doctor ever asked you if you smoke?”) and (2) physician advice not to smoke (“Has your doctor ever told you not to smoke?”). These measures were used to create a multilevel measure of physician interventions with the following categories: neither screened nor advised (0); screened only (1); advised only (2); and both screened and advised (3). Higher numbers were associated with more intense intervention.
Intentions to smoke
Intention to smoke was measured among smokers and nonsmokers by two questions: “How likely is it that you will smoke cigarettes during the next year?” and “How likely is it that you will smoke cigarettes five years from now?” Responses ranged from “very likely” (0) to “very unlikely” (3). Higher scores indicated stronger intentions to smoke.
Tobacco use
The survey asked students to self-report smoking in a series of questions. An initial item screened for never smokers, former smokers, those who had smoked a few puffs only, those who smoked at least monthly but not weekly, and those who smoked at least weekly. Among weekly smokers, another question assessed the amount smoked: “I smoke from 1 to 6 cigarettes per week” (0), “Daily, but less than ½ pack per day (ppd)” (1), “Between ½ and 1 ppd” (2), and “I smoke more than a ppd” (3).
Intentions to quit were assessed among those who smoked weekly or more by asking “Are you seriously thinking about quitting smoking within the six months?” Another question assessed intentions to quit in the next month. Response options were “yes” (1) or “no” (0).
Students who reported smoking at least weekly were asked to report their number of previous quit attempts: “never tried to quit” (0), “one time” (1), “two times” (2), or “three times or more” (3).
Quitting status was constructed so that current quitters were coded “1” and those who smoked at least weekly were coded “0.”
Relapse status was also measured. Those who indicated they had quit were identified as quitters (1). Those who had quit but resumed smoking at least weekly were coded as relapsers (0).
Data Analysis
Gender and neighborhood education were covariates in all analyses (Table 1). Due to the high correlation (r = .72) between neighborhood income and education, only education was used.
Table 1. Descriptive Statistics for Participants by Race.
| Caucasian | African American | Statistic | |
|---|---|---|---|
| Gender [n(%)] | χ2(1, N =4,787) = 10.75*** | ||
| Male | 403 (49.3%) | 1,710 (43.1%) | |
| Female | 414 (50.7%) | 2,260 (56.9%) | |
|
| |||
| Neighborhood Education [n(%)] | χ2(4, N =4,763) = 535.62*** | ||
| 9-12th grade, no degree | 0 (0%) | 73 (1.8%) | |
| High school degree or GED | 279 (34.4%) | 2,810 (71.1%) | |
| Some college/post high school | 506 (62.4%) | 1,069 (27.0%) | |
| Bachelor's degree | 24 (3.0%) | 0 (0%) | |
| Grad/professional school | 2 (0.2%) | 0 (0%) | |
|
| |||
| Neighborhood Income [M(SD)] | $41,065 ($13,582) | $26,043 ($8,605) | F(1,4761) = 1,635.44*** |
|
| |||
| Smoking history [n(%)] | χ2 (6, N =4,589) = 603.29*** | ||
| Never smoked | 243 (30.1%) | 2,237 (59.2%) | |
| Tried smoking (just a puff) | 180 (22.3%) | 1,026 (27.1%) | |
| Quit smoking | 99 (12.3%) | 181 (4.8%) | |
| Smoke < monthly | 32 (4.0%) | 88 (2.3%) | |
| Smoke < weekly | 18 (2.2%) | 47 (1.2%) | |
| Smoke weekly | 41 (5.1%) | 66 (1.7%) | |
| Smoke daily | 195(24.1%) | 136 (3.6%) | |
|
| |||
| History of quit attempt [n(%)] | χ2 (1, N = 2,109) = 1.82 | ||
| No | 75 (13.3%) | 172 (11.1%) | |
| Yes | 490 (86.7%) | 1,372 (88.9%) | |
Note. Where percentages do not total to 100%, it is due to missing data.
p < .001
First, differences in the amount of physician communication provided to the African Americans vs. Caucasians were examined via multinomial logistic regression. Race, smoking status [nonsmoker, light smoker (smokes < weekly), and regular smoker (smokes at least weekly] and their interaction were examined as predictors of physician communication. Odds ratios were interpreted.
Next, the analysis focused on examining if the relationships between physician communication and the dependent variables were moderated by race. When the dependent variable was binary, logistic regression was employed, using race, physician communication, and their interaction as predictors. When the dependent variable was continuous, analysis of variance (ANOVA) was used. Alpha was set at .05.
Results
Participant Characteristics
This sample was similar in race to students in the larger school system and included 82.9% African American and 17.1% Caucasian youth. African Americans lived in neighborhoods with lower income and education and were more likely to be female and nonsmokers (Table 1). Overall, 54% of the adolescents reported never smoking, 39.9% smoked some amount, and 6.2% had quit smoking. Among those who smoked, 88.2% had made a quit attempt.
Overall, 43.2% of youth were neither screened nor advised about smoking (n = 2,185), 14.6% were only screened (n = 736), 13.3% were only advised (n = 674), and 28.9% were both screened and advised (n = 1,458). All remaining analyses included gender and neighborhood education as covariates.
Rates of Physician Communication by Race and Smoking Status
A multinomial logistic regression examined race, smoking status (nonsmoker, light smoker, regular smoker), and their interaction as predictors of physician communication. When comparing no communication (referent) to screening, regular smokers were 1.73 times more likely than nonsmokers to be screened about smoking (95% CI [1.08, 2.77]). The main effect of race and its interaction were not significant predictors of being screened.
When predicting no communication (referent) vs. advice against smoking, African Americans were 1.53 times more likely than Caucasians to be advised (95% CI [1.11, 2.11]). The smoking status main effect and its interaction with race were nonsignificant.
When predicting those who were both screened and advised, regular smokers were 2.62 times more likely than nonsmokers to be both screened and advised about smoking (95% CI [1.81, 3.79]). The race main effect was nonsignificant. The interaction was significant: Among African Americans, nonsmokers were 1.72 times more likely than light smokers to be screened and advised. Among Caucasians, regular smokers were 2.60 times more likely than nonsmokers to be screened and advised.
Intentions to smoke
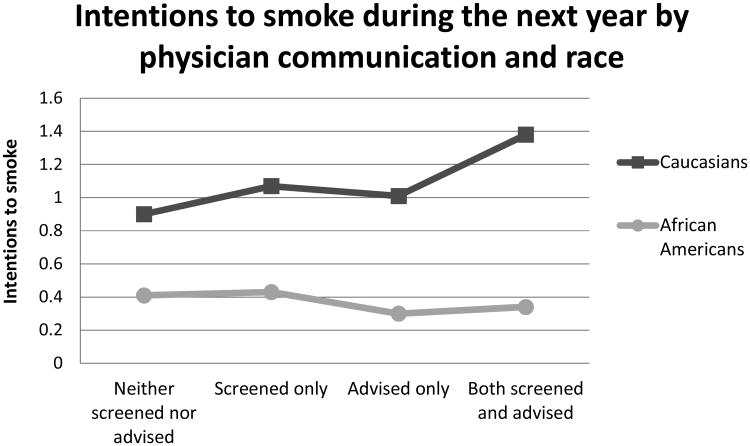
Intentions to smoke during the next year
A series of ANOVAs were conducted on the entire sample of both smokers and nonsmokers to determine the relations of race and physician communication to intentions to smoke. African Americans reported fewer intentions to smoke during the next year than Caucasians (F(1, 4525) = 291.12, p < .001; Table 2). The main effect of physician communication was significant (F(3, 4525) = 9.11, p < .001): Teens who were both screened and advised reported more intentions to smoke than those who received any other intervention, p's < .05.
Table 2. Estimated Marginal Means by Physician Communication and Race, Controlling for Gender and Estimated Neighborhood Education.
| Physician Communication | ||||
|---|---|---|---|---|
|
| ||||
| Neither Screened nor Advised | Screened only | Advised only | Both screened and advised | |
|
|
|
|
|
|
| Full Sample | M (SE) | M (SE) | M (SE) | M (SE) |
| Intentions to smoke a | ||||
|
| ||||
| Intentions to smoke during the next year | 0.66 (0.03) | 0.75 (0.05) | 0.66 (0.05) | 0.86 (0.03) |
|
| ||||
| Caucasian | 0.90 (0.05) | 1.07 (0.08) | 1.01 (0.10) | 1.38 (0.06) |
| African American | 0.41 (0.02) | 0.43 (0.04) | 0.30 (0.04) | 0.34 (0.03) |
|
| ||||
| Intentions to be a smoker in five years | 0.50 (0.02) | 0.63 (0.04) | 0.45 (0.05) | 0.70 (0.03) |
|
| ||||
| Caucasian | 0.64 (0.04) | 0.87 (0.07) | 0.64 (0.09) | 1.06 (0.05) |
| African American | 0.37 (0.02) | 0.39 (0.04) | 0.26 (0.04) | 0.33 (0.03) |
|
| ||||
| Subsample of smokers | ||||
|
| ||||
| Current amount smoked a | 0.76 (0.06) | 1.04 (0.09) | 0.99 (0.12) | 1.07 (0.06) |
|
| ||||
| Caucasian | 0.96 (0.10) | 1.38 (0.15) | 1.20 (0.19) | 1.48 (0.09) |
| African American | 0.56 (0.08) | 0.70 (0.11) | 0.78 (0.15) | 0.68 (0.09) |
|
| ||||
| Number of quit attempts b | 1.29 (0.07) | 1.72 (0.11) | 1.53 (0.14) | 1.44 (0.07) |
|
| ||||
| Caucasian | 1.34 (0.12) | 1.75 (0.18) | 1.88 (0.22) | 1.57 (0.10) |
| African American | 1.24 (0.08) | 1.68 (0.12) | 1.18 (0.16) | 1.31 (0.10) |
Note. M = mean. SE = standard error.
The n's for physician communication differed across analyses due to missing data. Full sample analyses: neither screened nor advised (n range = 1,936-1,948), screened only (n range = 651-656), advised only (n range = 603-611), and both screened and advised (n range = 1,318-1,320). Subsample of smokers: neither screened nor advised (n range = 250-308), screened only (n range = 107-136), advised only (n range = 64-75), and both screened and advised (n range = 213-265).
Lower scores represent better outcomes.
Higher scores represent better outcomes.
However, these main effects should be interpreted in light of a significant interaction, F(3,4525) = 14.83, p < .001 (see Figure 1). Physician communication had different effects for Caucasians (F(3, 4525) = 14.06, p < .001) vs. African Americans (F(3, 4525) = 2.95, p = .03). Caucasians who were screened and advised reported more intentions to smoke than those who received less intensive interventions, p < .01. Among African Americans, youth who were advised had fewer intentions to smoke than those who received no intervention (p = .02) or were only screened (p = .03).
Figure 1.
Interaction effects of physician communication with race on intentions to smoke during the next year, controlling for gender and estimated neighborhood education.
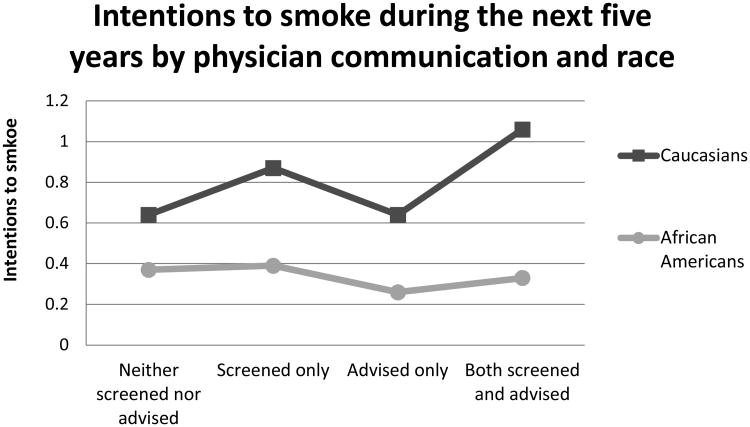
Intentions to smoke within five years
ANOVA using the entire sample revealed that African Americans had fewer intentions to smoke during the next five years than Caucasians (F(1, 4498) = 152.93, p < .001). Physician communication was associated with teens' intentions to smoke in five years (F(3, 4498) = 12.47, p < .001). Youth who were advised against smoking had fewer intentions to smoke than teens only screened or who were both screened and advised, p's < .05. Teens who were only screened or were screened and advised reported more intentions than teens who received no intervention.
There was a significant interaction (F(3, 4498) = 13.66, p < .001; Figure 2). Physician communication was related to intentions to smoke among both Caucasians (F(3, 4498) = 15.38, p < .001) and African Americans (F(3, 4498) = 3.23, p = .02). Again, the direction of the relationship differed. Caucasians who received the most intensive intervention endorsed more intentions to smoke than those who received less intervention, p's < .05. Alternatively, African Americans who were advised not to smoke had fewer intentions to smoke than peers who received less intervention, p's < .05.
Figure 2.
Interaction effects of physician communication with race on intentions to smoke in five years, controlling for gender and estimated neighborhood education.
Smoking vs. Quitting
Logistic regression was used to determine whether race and physician communication were related to quitting vs. continued smoking. The results revealed a trend (p = .08), such that among African Americans, teens who were screened and advised by physicians were 1.53 times more likely to have quit smoking than those who received no physician intervention (95% CI [0.95, 2.48]). Neither main effect was significant.
Amount smoked
All of the subsequent analyses were conducted only with participants who smoked. The interaction was nonsignificant (F(3, 624) = 2.02, p = .11), but both main effects were significant (Table 2). Teens who received the most intensive physician intervention smoked more than teens who received no intervention and teens who were screened smoked more than those not intervened with at all (F(3, 624) = 4.79, p = .003; follow-ups, p's < .05). African Americans smoked less than Caucasians (F(1, 624) = 36.98, p < .001).
Intentions to quit
Logistic regressions examined the relations between physician communication (referent category = neither screened nor advised), race (referent category = Caucasian), their interaction, and intentions to quit smoking vs. no such intentions.
Intentions to quit in one month
African Americans were 3.01 times more likely than Caucasians to intend to quit within one month (95% CI [1.72, 5.27]). In addition, physician communication was a predictor of intentions to quit: Teens asked about smoking and advised not to smoke were 1.83 times more likely to plan to quit in the next month compared to teens who did not receive intervention (95% CI [1.03, 3.26]). The interaction was nonsignificant.
Intentions to quit in six months
The interaction term and main effects were nonsignificant.
Quit history
Quit attempts
Caucasians reported more quit attempts than African Americans (F(1, 774) = 6.97, p = .008). Teens who were asked about smoking reported more quit attempts than those who received no intervention (F(3, 774) = 4.01, p = .008; follow-ups, p's < .05; Table 2). No significant interaction emerged.
Relapse status
Among adolescents who had quit, logistic regression was employed to examine relapse rates. Caucasians were 5.25 times more likely than African Americans to be quit vs. relapsed (95% CI [1.56, 17.68]). The communication main effect was nonsignificant. The interaction was significant: Among teens who received no communication, Caucasians were 8.83 times more likely than African Americans to avoid relapsing (95% CI [2.17, 35.87]). Among minority adolescents, those who were advised not to smoke were 7.27 times more likely to stay quit than adolescents who received no intervention (p = .06; 95% CI [0.90, 58.60]).
Discussion
Previous studies have found inconsistencies in the focus of physician advice against smoking, with some showing that physicians are more likely to advise young African Americans against tobacco and others suggesting that Caucasian youth are more often the target of physician intervention [27,29]. Our study moves one step further, suggesting that the smoking status of the adolescents under study is critical in this regard. A significant interaction emerged between race and smoking status: Among African Americans, nonsmokers were most likely to receive the most intensive physician intervention about smoking while among Caucasians regular smokers were more likely to get the most intensive intervention. Further, regular smokers were more likely to be screened and African Americans were more likely to be advised against smoking. It seems likely that physicians are targeting youth at risk for tobacco-related consequences—African Americans and regular smokers; however, they appear to be missing an opportunity for intervention among African American smokers and Caucasian nonsmokers. It may be that physicians are aware of the different trajectories of smoking among youth (e.g., later initiation among African Americans and earlier initiation among Caucasians) and are focusing the limited time they have with adolescents on risk behaviors that are most salient at that time [1,2]. However, further research is needed to determine why physicians offer different types of intervention to adolescents.
In a number of cases the relation of physician communication to outcomes did not differ by racial group. For example, regardless of teens' race, physician interventions were associated with increased intentions to quit in one month and quit attempts. However, physician communication was also associated with higher levels of smoking. Because of the cross-sectional nature of this study, the directionality of this finding is unclear. This pattern of results may suggest that physicians are able to identify adolescent tobacco users and intensify their intervention for these youth accordingly; especially given the congruence of our findings with research that found that physician communication was associated with both higher levels of smoking (selection of at-risk adolescents) and increased quit attempts (intervention benefits; [27]).
Physician communication was moderated by race in a pattern that suggests important benefits for African American teens. Physician communication with young African Americans was associated with fewer intentions to smoke. Further, among African American smokers, those who received physician intervention were 53% more likely to quit smoking than their peers who received no intervention. Finally, African American teens who were advised not to smoke were over seven times as likely to report a successful quit (i.e., without relapse) than African Americans who received no intervention.
These findings are particularly promising, given that smoking-related morbidity and mortality is higher among African Americans [3-5] and that cessation is less common than among Caucasians [3,12,33-35]. African Americans start smoking at a later age, usually in late adolescence or young adulthood [2], providing a longer window for preventive interventions. Physicians could take advantage of this window by continuing to reinforce to young African Americans the importance of avoiding tobacco and the benefits of quitting if one is already a smoker.
Despite its contributions, there are limitations. Given the large-scale nature of the study, biochemical verification of smoking was not possible. However, research has indicated that youth self-reports of smoking are valid when confidentiality is ensured [36, 37]. Our measure of physician communication assessed a history of ever talking to a physician about smoking. Youth may have underreported this construct due to recall bias; however, research has supported the validity of adolescent recall of preventive services [38]. Other contextual factors that could influence physician-adolescent communication, such as healthcare access, were not assessed. However, a previous study found that among adolescents who had seen a HCP in the past year, rates of physician intervention during the past year (64%) were similar to those obtained in our study (57%) [39]. Although our cross-sectional design allowed us to maximize sample size, it also hindered our ability to draw conclusions about directionality. Randomized controlled trials exploring the relations between physician communication and tobacco use would allow for clearer interpretations of causal directions.
Our research has identified important relationships between race and physicians' advising against smoking. Physicians seem to be targeting youth at risk for tobacco-related consequences—African Americans and regular smokers; however, they may be missing an opportunity for intervention among African American smokers and Caucasian nonsmokers. Importantly, African American teens appeared to benefit more from the physician tobacco interventions. These findings are particularly promising, given that smoking-related morbidity and mortality is higher among African Americans [3-5] and cessation is less common [3,12,33-35]. Overall, these findings reiterate the necessity for consistent tobacco surveillance and interventions for all youth.
Implications and Contribution.
Physician interventions were associated with increased adolescent intentions to quit and quit attempts. Physicians seem to be targeting youth at risk for tobacco-related consequences—African Americans and regular smokers; there are opportunities for increased intervention among African American smokers and Caucasian nonsmokers. African Americans benefited more from physician interventions.
Acknowledgments
The study was supported by National Heart, Lung, and Blood Institute grant HL050723 and a Centers of Excellence grant awarded by the State of Tennessee to the Department of Psychology, University of Memphis. This study was also supported by a training grant 5 T32 HL076134-09 (R. Wing, PI).
Abbreviations
- HCP
Health care provider
Footnotes
Declaration of Interests: Neither of the authors has any competing interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Leslie A. Robinson, Email: Lrobinso@memphis.edu.
Jeanelle S. Ali, Email: jsali@memphis.edu.
References
- 1.Centers for Disease Control and Prevention. Tobacco Product Use Among Middle and High School Students — United States, 2011 and 2012. MMWR Morb Mortal Wkly Rep. 2013;62(45):893–97. [PMC free article] [PubMed] [Google Scholar]
- 2.National Cancer Institute. Phenotypes and endophenotypes: Foundations for genetic studies of nicotine use and dependence. [Accessed October 21, 2013]; Available at: http://cancercontrol.cancer.gov/brp/tcrb/monographs/20/ Published March 13, 2012.
- 3.Richardson TL. African-American smokers and cancers of the lung and of the upper respiratory and digestive tracts. Is menthol part of the puzzle? West J Med. 1997;166:189–94. [PMC free article] [PubMed] [Google Scholar]
- 4.Royce JM, Hymowitz N, Corbett K, Hartwell TD, Orlandi MA. Smoking cessation factors among African Americans and Whites. Am J Public Health. 1993;83(2):220–226. doi: 10.2105/AJPH.83.2.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; [Accessed on October 21, 2013]. Tobacco use among U.S racial/ethnic minority groups-African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, Hispanics: A Report of the Surgeon General. http://profiles.nlm.nih.gov/ps/retrieve/ResourceMetadata/NNBBFQ. Published 1998. [Google Scholar]
- 6.Fiore MC, Jaén CR, Baker TB, et al. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; [Accessed October 21, 2013]. Treating tobacco use and dependence 2008 update - Clinical practice guideline. http://www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/tobacco/clinicians/update/treating_tobacco_use08.pdf. Published May, 2008. [Google Scholar]
- 7.Moolchan ET, Fagan P, Fernander AF, et al. Addressing tobacco-related health disparities. Addiction. 2007;102:30–42. doi: 10.1111/j.1360-0443.2007.01953. [DOI] [PubMed] [Google Scholar]
- 8.Harris RE, Zang EA, Anderson JI, Wynder EL. Race and sex differences in lung cancer risk associated with cigarette smoking. Int J Epidemiol. 1993;22(4):592–599. doi: 10.1093/ije/22.4.592. [DOI] [PubMed] [Google Scholar]
- 9.Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17(1):143–52. [PubMed] [Google Scholar]
- 10.Pérez-Stable EJ, Herrera B, Jacob P, III, Benowitz NL. Nicotine Metabolism and Intake in Black and White Smokers. JAMA. 1998;280(2):152–156. doi: 10.1001/jama.280.2.152. [DOI] [PubMed] [Google Scholar]
- 11.Headley AJ. Generations of loss: contemporary perspectives on black infant mortality. J Natl Med Assoc. 2004;96(7):987–994. [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. High school students who tried to quit smoking cigarettes--United States, 2007. MMWR Morb Mortal Wkly Rep. 2009;58(16):428–431. [PubMed] [Google Scholar]
- 13.Benowitz NL. Clinical pharmacology of nicotine: implications for understanding, preventing, and treating tobacco addiction. Clin Pharmacol Ther. 2008;83(4):531–541. doi: 10.1038/clpt.2008.3. [DOI] [PubMed] [Google Scholar]
- 14.Primack BA, Bost JE, Land SR, et al. Volume of tobacco advertising in African American markets: Systematic review and meta-analysis. Health Rep. 2007;122(5):607–615. doi: 10.1177/003335490712200508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gardiner PS. The African Americanization of menthol cigarette use in the United States. Nicotine Tob Res. 2004;6(Suppl 1):S55–S65. doi: 10.1080/14622200310001649478. [DOI] [PubMed] [Google Scholar]
- 16.Anderson SJ. Marketing of menthol cigarettes and consumer perceptions: A review of tobacco industry documents. Tob Control. 2011;20(Suppl 2):ii20–ii28. doi: 10.1136/tc.2010.041939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fu SS, Burgess D, van Ryn M, et al. Views on smoking cessation methods in ethnic minority communities: A qualitative investigation. Prev Med. 2007;44(3):235–240. doi: 10.1016/j.bbr.2011.03.031. [DOI] [PubMed] [Google Scholar]
- 18.Klesges RC, Somes G, Pascale RW, et al. Knowledge and beliefs regarding the consequences of cigarette smoking and their relationships to smoking status in a biracial sample. Health Psychol. 1998;7(5):387–401. doi: 10.1037/0278-6133.7.5.387. [DOI] [PubMed] [Google Scholar]
- 19.Reimer RA. Racial disparities in smoking knowledge among current smokers: Data from the Health Information National Trends Surveys. Psychology & Health. 2010;25(8):943–959. doi: 10.1080/08870440902935913. [DOI] [PubMed] [Google Scholar]
- 20.Cokkinides VE, Halpern MT, Barbeau EM, et al. Racial and ethnic disparities in smoking-cessation interventions: Analysis of the 2005 National Health Interview Survey. Am J Prev Med. 2008;34(5):404–412. doi: 10.1016/j.amepre.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 21.Lawrence D, Graber JE, Mills SL, et al. Smoking cessation interventions in U.S. racial/ethnic minority populations: an assessment of the literature. Prev Med. 2003;36(2):204–216. doi: 10.1016/S0091-7435(02)00023-3. [DOI] [PubMed] [Google Scholar]
- 22.Kiefe CI, Williams OD, Greenlund KJ, et al. Health care access and seven-year change in cigarette smoking: The CARDIA study. Am J Prev Med. 1998;15(2):146–159. doi: 10.1016/S0749-3797(98)00044-0. [DOI] [PubMed] [Google Scholar]
- 23.Chapman S. The role of doctors in promoting smoking cessation. BMJ. 1993;307(6903):518–519. doi: 10.1136/bmj.307.6903.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whitlock EP, Orleans CT, Pender N, et al. Evaluating primary care behavioral counseling interventions: An evidence-based approach. Am J Prev Med. 2002;22(4):267–284. doi: 10.1016/S0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 25.Robinson LA, Emmons KM, Moolchan ET, et al. Developing smoking cessation programs for chronically ill teens: Lessons learned from research with healthy adolescent smokers. J Pediatr Psychol. 2008;33(2):133–144. doi: 10.1093/jpepsy/jsm112. [DOI] [PubMed] [Google Scholar]
- 26.Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database of Syst Rev. 2008;(2):CD000165. doi: 10.1002/14651858.CD000165.pub3. 2008. [DOI] [PubMed] [Google Scholar]
- 27.Shelley D, Cantrell J, Faulkner D, et al. Physician and dentist tobacco use counseling and adolescent smoking behavior: Results from the 2000 National Youth Tobacco Survey. Pediatrics. 2005;115(3):719–725. doi: 10.1542/peds.2004-0873. [DOI] [PubMed] [Google Scholar]
- 28.Hum AM, Robinson LA, Jackson AA, et al. Physician communication regarding smoking and adolescent tobacco use. Pediatrics. 2011;127(6):e1368–e1374. doi: 10.1542/peds.2010-1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thorndike AN, Ferris TG, Stafford RS, et al. Rates of U.S. physicians counseling adolescents about smoking. J Natl Cancer Inst. 1999;91(21):1857–1862. doi: 10.1093/jnci/91.21.1857. [DOI] [PubMed] [Google Scholar]
- 30.Alfano CM, Zbikowski SM, Robinson LA, et al. Adolescent reports of physician counseling for smoking. Pediatrics. 2002;109(3):e47. doi: 10.1542/peds.109.3.e47. [DOI] [PubMed] [Google Scholar]
- 31.Robinson LA, Klesges RC, Zbikowski SM, et al. Predictors of risk for different stages of adolescent smoking in a biracial sample. J Consult Clin Psychol. 1997;65(4):653–662. doi: 10.1037/0022-006X.65.4.653. [DOI] [PubMed] [Google Scholar]
- 32.Siddiqui O, Hedeker D, Flay BR, Hu FB. Intraclass correlation estimates in a school-based smoking prevention study. Am J Epidemiol. 1996;144:425–433. doi: 10.1093/oxfordjournals.aje.a008945. [DOI] [PubMed] [Google Scholar]
- 33.Gandhi KK, Foulds J, Steinberg MB, et al. Lower quit rates among African American and Latino menthol cigarette smokers at a tobacco treatment clinic. Int J Clin Pract. 2009;63(3):360–367. doi: 10.1111/j.1742-1241.2008.01969. [DOI] [PubMed] [Google Scholar]
- 34.Gundersen DA, Delnevo CD, Wackowski O. Exploring the relationship between race/ethnicity, menthol smoking, and cessation, in a nationally representative sample of adults. Prev Med. 2009;49(6):553–557. doi: 10.1016/j.ypmed.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 35.Harris KJ, Okuyemi KS, Catley D, et al. Predictors of smoking cessation among African-Americans enrolled in a randomized controlled trial of bupropion. Prev Med. 2004;38(4):498–502. doi: 10.1016/j.bbr.2011.03.031. [DOI] [PubMed] [Google Scholar]
- 36.Dolcini MM, Adler NE, Lee P, et al. An assessment of the validity of adolescent self-reported smoking using three biological indicators. Nicotine Tob Res. 2003;5(4):473–483. doi: 10.1080/1462220031000118586. [DOI] [PubMed] [Google Scholar]
- 37.Post A, Gilljam H, Rosendahl I, et al. Validity of self reports in a cohort of Swedish adolescent smokers and smokeless tobacco (snus) users. Tob Control. 2005;14(2):114–117. doi: 10.1136/tc.2004.008789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Klein JD, Graff CA, Santelli JS, et al. Developing quality measures for adolescent care: Validity of adolescents' self-reported receipt of preventive services. Health Serv Res. 1999;34(1):391–404. [PMC free article] [PubMed] [Google Scholar]
- 39.Schauer GL, Agaku IT, King BA, Malarcher AM. Health care provider advice for adolescent tobacco use: results from the 2011 national youth tobacco survey. Pediatrics. 2014;134(3):446–55. doi: 10.1542/peds.2014-0458. http://doi.org/10.1542/peds.2014-0458. [DOI] [PubMed] [Google Scholar]