Abstract
Introduction
The 2011 IOM report stated that pain management in children is often lacking especially during routine medical procedures. The purpose of this review is to bring a developmental lens to the challenges in assessment and non-pharmacologic treatment of pain in young children.
Method
A synthesis of the findings from an electronic search of PubMed and the university library using the keywords pain, assessment, treatment, alternative, complementary, integrative, infant, toddler, preschool, young, pediatric, and child was completed. A targeted search identified additional sources for best evidence.
Results
Assessment of developmental cues is essential. For example, crying, facial expression, and body posture are behaviors in infancy that indicate pain: However in toddlers these same behaviors are not necessarily indicative of pain. Preschoolers need observation scales in combination with self-report while for older children self-report is the gold standard. Pain management in infants includes swaddling and sucking. However for toddlers, preschoolers and older children, increasingly sophisticated distraction techniques such as easily implemented non-pharmacologic pain management strategies include reading stories, watching cartoons, or listening to music.
Discussion
A developmental approach to assessing and treating pain is critical. Swaddling, picture books, or blowing bubbles are easy and effective when used at the appropriate developmental stage and relieve both physical and emotional pain. Untreated pain in infants and young children may lead to increased pain perception and chronic pain in adolescents and adults. Continued research in the non-pharmacological treatment of pain is an important part of the national agenda.
Introduction
Despite decades of research in the assessment and treatment of pain in pediatrics, infants and young children still suffer unnecessary pain. Moreover, despite intense research and education over the last decade, the assessment and treatment of pain in infants and young children remain challenging with potential long-term consequences (Fitzgerald & Walker, 2009; van Dijk, Peters, Bouwmeester, & Tibboel, 2002). Pain experiences in infancy and childhood may result in long-term changes in physiological and behavioral responses to pain (Anand & International Evidence-Based Group for Neonatal, 2001; Institute of Medicine, 2011). In fact, children who suffered traumatic pain were 1.5 times more likely to suffer chronic pain in adulthood while children who experienced frequent headaches were 2.2 times more likely to experience frequent headaches in adulthood (Fearon & Hotopf, 2001; Jones, Power, & Macfarlane, 2009). Unrelieved pain during infancy and childhood leads to a hypersensitivity to pain through a “rewiring” of the peripheral as well as central nervous system leading to life-long changes in pain perception (Fitzgerald & Walker, 2009; Woolf, 2007). One study of male infants circumcised within two days of birth indicated that they had higher pain scores when receiving two-month immunizations than male babies who had not been circumcised (Stevens, 2007). Relatedly, failure to control pain in infants with sickle cell disease has lifelong implications including poor coping strategies (Benjamin, 2008). Chronic pain in adults and children is a national and international challenge and results in suffering and increase healthcare costs. By improving the assessment and treatment of pain in early childhood, we may be able to address this challenge.
For children and infants, the pain experience often occurs during routine medical procedures such as heel sticks and vaccinations or during more severe instances of postoperative pain or pain from traumatic injuries. According to the International Association for the Study of Pain (IASP), the definition of pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage…” (2012, p. para. 5). IASP explains that the lack of ability to communicate using language does not mean that a child is not experiencing pain. In order to end unnecessary pain in childhood, and its long-term consequences, we must interpret infant and child communication including verbalizations such as crying, body movements such as kicking, and facial expressions such as a furrowed brow with our knowledge of child development.
The Institute of Medicine (IOM) states that pain is a national challenge and pain management in children is often lacking even in pediatric emergency departments (Institute of Medicine, 2011). Despite the fact that there are well-validated tools available for the assessment of children’s pain, more than half of hospitalized children experience severe unrelieved pain (Kortesluoma, Nikkonen, & Serlo, 2008; Twycross & Collis, 2012). This implies that either the tools are not being used to assess the pain or the pain is not being adequately treated. Hospitals in the United States are mandated to assess pain on a routine basis and hospital policies reflect that mandate. Studies conducted in Europe show that nurses may not be consistently assessing pain, may not always believe children when they report pain, and may not treat pain adequately (Kortesluoma et al., 2008; Twycross & Collis, 2012). Although we did not find a similar study from the United States, clinical experience of pain management specialists and the IOM report demonstrate that pediatric nurses in the United States have many of the same issues.
Similar issues also arise in the treatment of pain. A study in Canada examined whether pain was addressed during routine childhood vaccinations and found that although both pharmacological and non-pharmacological interventions are available and easy to use, these interventions were not done mainly due to lack of knowledge (Taddio et al., 2009). Non-pharmacological interventions such as music, hypnosis, distraction, and massage are often successful in decreasing pain during procedures such as venipuncture and lumbar puncture as well as general pain in pre-adolescent children (Nguyen, Nilsson, Hellstrom, & Bengtson, 2010; Post-White et al., 2009; Smith, Barabasz, & Barabasz, 1996). Simple techniques are very helpful for children during medical procedures but healthcare providers are often not introduced to these techniques during their formal education.
Factors that contribute to the difficulty in assessing and treating pain include a variety of dynamics from the child, their parents, and the health care providers. A child’s physical, emotional, and cognitive development modifies their response to pain. Other aspects include the child’s fear, anxiety, anger, lack of control or choice, underlying illness causing the pain, situational factors, and previous experiences with pain (McGrath & Brown, 2005). Parent and staff response to the child’s fear, anxiety, or anger can also alter the child’s response to pain (McGrath & Brown, 2005). Self-report remains the gold standard of assessing pain in adults, however infants, toddlers, preschool children, and non-verbal children are unable to report pain or are unable to do so reliably (Hunter, McDowell, Hennessy, & Cassey, 2000; von Baeyer, Forsyth, Stanford, Watson, & Chambers, 2009). Particularly in infants, proxy report in the form of parent report or healthcare provider observation are the common available sources of pain assessment (Buttner & Finke, 2000; Hartrick & Kovan, 2002; Pillai Riddell & Racine, 2009; Stevens, 2007). Given the large number of signs and symptoms presented by children related to their pain experience, the purpose of this article is to bring a developmental lens to the challenges of assessing and treating pain in young children.
Methods
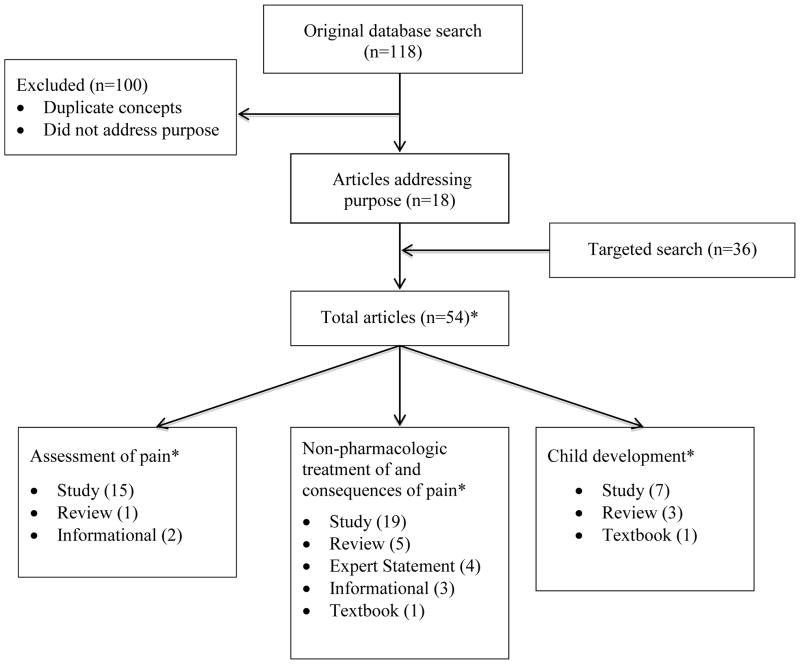
A synthesis of the findings from an electronic search of PubMed and the general non-medical library electronic resources for the years 1980 through 2014 using the keywords pain, assessment, treatment, alternative, complementary, integrative, infant, toddler, preschool, young, pediatric, and child in combination with a targeted search to identify additional sources for best evidence was completed. The general non-medical library resources were searched specifically for child development articles. After removing duplicates, the initial search resulted in 118 articles including 92 research studies, 5 informational articles, and 21 review articles. Articles that addressed the main purpose of this topic were used in this synthesis. Articles were excluded if they did not directly relate to the specific age groups of this synthesis (infant, toddler, preschooler, or early elementary schooler), or were not non-pharmacologic interventions. Additional supporting sources included those related to developmental issues, assessment tool validation, and position statements from experts and organizations such as the World Health Organization and the International Association for the Study of Pain (see Figure 1). The original search provided the direction of the article and main evidence for the synthesis. The first author (ST) conducted the initial search; all authors informally evaluated the studies and came to agreement about their inclusion, and contributed to the data synthesis. From the original search, 18 articles were used including 12 research studies, 5 reviews, and 1 informational survey. In addition, 36 research studies and review articles were found through a targeted search. In total, in-depth review of 54 articles was conducted.
Figure 1.
Article Flow Diagram
*Articles are not mutually exclusive. Many sources reported on more than one topic area.
Infants
Pain Assessment: Considering the Role of Attachment
There are a variety of pain tools available for the assessment of pain in infants. These tools rely mainly on observer report and consider a variety of infant behaviors including facial expression, cry, movement, tone, body posture, and consolability (Buttner & Finke, 2000; van Dijk et al., 2002). Some assessment tools also take into account physiologic signs such as respiratory and heart rate, oxygenation, or blood pressure (van Dijk et al., 2002). In an analysis of the most specific and reliable behaviors used by health care providers for the assessment of pain in infants, Buttner and Finke (2000) found that crying, facial expression, and body posture were the most sensitive cues to identifying pain.
The CRIES observational assessment tool is often used by hospitals during the neonatal period. This tool assesses the following attributes of the infant: Cry described as none, crying but consolable, high-pitched and inconsolable, Requires oxygen to maintain a saturation above 95%, Increased vital signs, facial Expression described as no grimace, grimace, or grimace and grunting, and Sleepless described as continuously asleep, frequently awake, constantly awake (Krechel & Bildner, 1995). An example of a popular observational assessment tool used by many hospitals for older infants is the FLACC (Face, Legs, Activity, Cry, and Consolability) measurement tool (Merkel, Voepel-Lewis, & Malviya, 2002). For both measures, each category is scored and then totaled and compared to established criteria such as the two-step approach recommended by World Health Organization (2012) for mild, moderate or severe pain.
Although both of these measures provide useful and observable information, neither takes into account the child’s attachment with an important adult in their lives the most salient developmental process in infancy (hereafter referred to as the parent although the adult may not be the biological parent). Infant reaction to painful stimuli is a bidirectional process between parent and infant (Pillai Riddell & Racine, 2009). Specifically, a parent who is sensitive to the infant’s pain cues will be more likely to provide soothing behaviors such as rocking, touching, or swaddling, to calm the infant more quickly (Jahromi, Putnam, & Stifter, 2004; Schechter et al., 2007). These parental soothing behaviors in turn result in the infant being more attentive to the parent, which strengthens the parent-child attachment. Understanding the degree of parent-child attachment may not change the amount of pain the child is experiencing, but it will provide important information for determining how to proceed with treatment. For example, if a child is experiencing pain but has a close attachment with a parent, then the child will likely receive relief from comforting by the parent, and may not need the same treatment as a child with the same amount of pain but no parent support.
Pain Treatment: Attachment, Swaddling, & the Sucking Response
Several non-pharmacologic methods have been shown to be effective in reducing pain in infants undergoing painful procedures. These methods may be effective in part because of their responsiveness to the developmental characteristics of infancy. For example, building on the infant’s need for attachment, Kangaroo Care (skin to skin contact with a parent) for 30 minutes prior to and during the painful procedure has been shown to decrease infant pain and distress (Stevens, 2007). In addition, studies on swaddling, which mimic the feeling of being held, suggest that infants’ vital signs recover more quickly when swaddled during a painful procedure (Fernandes, Campbell-Yeo, & Johnston, 2011; Spence et al., 2009). Other treatment methods capitalize on infants’ natural sucking response. Offering infants pacifiers, both with and without sucrose, and breastfeeding, have been shown to decrease pain during painful procedures including vaccinations and heel lancing (Marin Gabriel et al., 2013; Stevens, Yamada, & Ohlsson, 2010). A Cochrane review found that breastfeeding infants during painful procedures resulted in statistically lower heart rates and decreased total crying time when compared to swaddling, holding, and pacifier interventions (Shah, Herbozo, Aliwalas, & Shah, 2012). Bembich et al. (2013) used functional MRI to evaluate brain activity in infants during painful procedures using both sucrose solutions and breastfeeding: Breastfeeding stimulated cortical activation leading the authors to posit that breastfeeding is a multisensory experience leading to decreased pain perception.
Although these developmentally-informed non-pharmacologic pain treatment strategies show promise individually, recent research suggests that a combination of techniques such as breastfeeding, pacifiers, swaddling, and rocking may be more effective than one technique used alone (Harrington et al., 2012). As evidenced in this research on infancy, taking advantage of developmental characteristics may be an effective approach to decreasing the pain and suffering attached to common medical procedures.
Toddlers
Pain Assessment: Beyond Physiology
The assessment of pain in toddlers presents similar issues as infants. Toddlers are venturing toward autonomy, but still look to their parents for security in new situations and when things are frightening or painful. Toddlers cannot conceptualize pain in terms of location or intensity. Most hospitals and providers use the same tools to measure pain in toddlers as they do in infants (e.g., FLACC mentioned above). Other pain scales used with toddlers includes Children’s and Infants’ Postoperative Pain Scale (CHIPPS) and Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS). The CHIPPS scale assesses crying (none, moaning, screaming), facial expression (relaxed, wry mouth, grimacing), posture of the trunk (neutral, variable, rear up), posture of the legs (neutral, kicking, tightened), and motor restlessness (none, moderate, restless). The CHEOPS scale tested on children ages one to five is more complex: This scale assesses cry (no cry, moaning, crying), facial expression (smiling, composed, grimace), child verbalizations (positive, none, complaints other than pain, pain complaints, both pain and non-pain complaints), torso (neutral, shifting, tense), touch (not touching, reach, touch, grab, restrained), legs (neutral, squirming kicking, drawn up tensed, standing, restrained). Although some of these such as FLACC are still useful, research suggests that those that have a physical measure such as heart rate are not effective for this developmental stage. For example, Buttner and Finke (2000) found that for toddlers, physiological indicators such as heart rate, respiratory rate, and blood pressure were not good indicators for pain. Instead, observational assessments such as those used in FLACC or CHIPPS were both specific and sensitive measures of pain in toddlers. In a prospective study involving 150 children and four observers, both FLACC and CHIPPS were found to be homogeneous, have good face and construct validity, sensitivity, and specificity to pain whereas the psychometric properties of CHEOPS was not as consistent because the category “touch” has a low score for reliability and internal validity (Bringuier et al., 2009). This suggests that behavioral indicators may need more careful consideration. Stressful situations may result in variable pain scores depending on parental attachment, parental stress, experience level of the observer, and temperament of the child (Frank, Blount, Smith, Manimala, & Martin, 1995; Hartrick & Kovan, 2002; Schechter et al., 2007).
Pain Treatment: The Emergence of Cognitive Skills
Toddlerhood can be a demanding age group for parents and nurses who are attempting to soothe these young children during and after painful procedures. This is in part because their cognitive abilities are still emerging and, as such, non-painful situations such as taking a temperature may seem just as distressing as receiving an injection. Moreover, at this stage parental empathetic attention may cause the toddler to react in an especially distressed way (McMurtry, Chambers, McGrath, & Asp, 2010).
One positive outcome of toddlers’ cognitive advances is that distraction is now more effective than before, and is more effective than common techniques such as parental empathetic attention (Schechter et al., 2007). Thus, treating toddler pain can be easier than in infancy as toddlers are increasingly inclined to take their behavioral cues from parents and other adults. Specifically, techniques such as playing peek-a-boo, blowing bubbles, or looking at books are easily implemented distractions for toddlers when parents or other adults join in the game (Jay, Elliott, Fitzgibbons, Woody, & Siegel, 1995; Manne et al., 1990).
Preschoolers
Pain Assessment: Emerging Self-Awareness and Language Skills
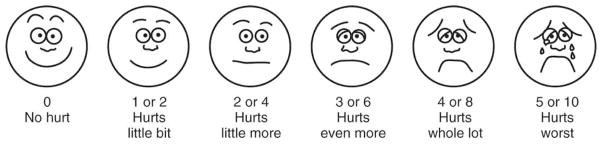
Beginning in preschool, children are developing the ability to use self-report tools such as a faces-type pain scale with varying degrees of precision (Hunter et al., 2000; von Baeyer et al., 2009).
Children in this age group often lack the ability to describe their pain although often they are at the very least able to point to the area that hurts (von Baeyer et al., 2009). In a study of healthy children ages three to five years old, von Bayer et al. found that three year old children show a response bias by choosing either the high or low end of the scale consistently and are not always able to put a faces-type of pain scale in the correct order, from low to high pain level. By the age of five, however, the children had developed a higher level of self-awareness and language that translated into more nuanced and useful responses (von Baeyer et al., 2009). Based on this study, von Bayer et al. recommend using a proxy pain assessment, such as the FLACC scale mentioned above, in conjunction with self-report for children younger than five years of age.
Because preschoolers are just beginning to development sufficient self-awareness and language skills to effectively use self-report assessments, observational pain assessment tools are still used for this age group in situations such as trauma or post-surgically. Hesselgard, Larsson, Romner, Stromblad, and Reinstrup (2007) felt that most observational scales were too complicated for fast and accurate pain measurement, especially in the post-surgical setting. Thus the Behavioral Observational Pain Scale (BOPS) was created to be a fast and accurate observational measure of pain for children ages one to seven, assessing facial expression, verbalization, and body position separately on a scale of zero to two for a total possible pain score of zero to six (Hesselgard et al., 2007). In psychometric testing, the scale achieved a high inter-rater reliability (0.93), a high correlation with the CHEOPS pain scale (r=0.87), and a high construct validity and sensitivity to measuring pain and pain relief with preschool children (Hesselgard et al., 2007). When testing the FLACC pain scale in post-operative children, Malviya, Voepel-Lewis, Burke, Merkel, and Tait (2006) found a high intra-class correlation coefficient (ICC) for total pain scores (ICC=0.90). In sum, observational pain assessment such as the BOPS and FLACC may be valid and useful at this stage, but self-report may also be effective as self-awareness and language skills emerge.
Pain Treatment: Increases in Cognition and the Complexity of Distractions
Like toddlerhood, the use of distraction techniques is a way to help preschoolers decrease the perception of pain and cope with painful procedures (Weiss, Dahlquist, & Wohlheiter, 2011). One example of the effectiveness of distraction is seen in a study with 120 healthy three to five year old children who kept their non-dominant hands in a cooler filled with water maintained at 50ºF and experienced either an active or passive distraction (Weiss et al., 2011). Interactive distraction consisted of playing a video game with a joystick. Passive distraction involved watching the game output without actually playing it. Results indicated that both passive and interactive distraction conditions worked equally well to increase pain tolerance in the experimental groups when compared to the control group (Weiss et al., 2011). In another study on distraction, Yoo, Kim, Hur, and Kim (2011) used a three-minute animated cartoon intervention shown on a laptop computer for three to five year olds during a blood draw procedure. In this quasi-experimental intervention, (Yoo et al., 2011) found that when comparing the intervention group with the control group, the intervention group had significantly lower cortisol and glucose levels indicating lower stress levels, and a lower self-reported pain score. These results suggest that distractions may be effective at this stage, although the form of distractions is notably more complex than in toddlerhood (peek-a-boo, bubble blowing, etc.). Since preschoolers are now mastering increasingly complex cognitive skills such as using symbols, manipulating whole numbers, and engaging in more elaborate pretend play scenarios; it is understandable that their need for more complex distractions increases as well.
It is also important to note that the timing of the distraction is an important consideration. In contrast to the above interventions, Dixey, Seiler, Woodie, Grantham, and Carmon (2008) studied the child’s response after a procedure using stickers, which are sometimes given to children as a reward following a procedure. They found that giving a child a cartoon sticker following a finger stick blood test procedure did not decrease child self-report of pain when compared to children who did not receive a sticker. This suggests that interventions during a procedure work better to decrease pain than those interventions completed after a procedure.
Early Elementary Schoolers
Pain Assessment: Burst in Vocabulary Development Aids Self-Report
By the time a typically developing child reaches kindergarten, they are not only able to report their pain but also point to the painful area and describe their pain using descriptive terms such as stabbing or burning, (Hicks, von Baeyer, Spafford, van Korlaar, & Goodenough, 2001). Specifically, a substantial burst in vocabulary at this stage increases early elementary schoolers’ ability to express themselves and communicate nuanced aspects of pain. The Faces Pain Scale has been validated over time and found highly correlated with a visual analog scale (VAS) for this age group (Garra et al., 2010; Hicks et al., 2001). The Faces Pain Scale or a visual numerical scale is appropriate for assessing pain in this age group. In addition to pointing to the face associated with their pain level, early elementary schoolers may be able to describe their pain to a nurse with more nuance and detail.
Simultaneously, cultural and social norms have been observed by the child and reinforced by the parents and the community. The end result becomes the child’s ability to control their expression making proxy pain report difficult and self-report of pain the only reliable measure (Chen & French, 2008; Huguet, Stinson, & McGrath, 2010). Western societies, for example, often value autonomy and individual decision-making relatively more than self-regulation and control (MacCoby & Martin, 1983). On the other hand, for cultures that value group orientation and group harmony (e.g., many East Asian and Latin American families), self-control is more highly valued and lack of self-regulation may be considered a significant problem (Zhou, Eisenberg, Wang, & Reiser, 2004). As a result, it may be easier to assess pain cues of children from Western cultures, because they show their pain relatively more freely without being trained to enact as much restraint as their peers. Understanding cultural norms may increase nurse’s attunement to variation in self-report responses and make this a more valid approach to pain assessment.
Pain Treatment: Reading Relational Cues
As in earlier stages, studies have shown that distractions provided by caregivers, not verbal reassurance, can be useful for treating pain in early elementary schoolers, but their effectiveness is dependent on the type of relational cues the child gets from the adult. For example, in one study by Frank et al. (1995), 77 children receiving routine vaccinations were examined and researchers found that children’s coping behaviors were accounted for mainly as a result of parents and staff promoting coping behavior. Furthermore, parental distress-promoting behaviors, such as punishment, criticism, empathic comments, apologies, and reassurance were significant predictors of child distress. Children at this stage are often quite skilled at observing and interpreting adult behavior, and these cues influence their experience of pain (Blount et al., 1989). This is exemplified in McMurtry et al. (2010) study examining parental facial expression and tone of voice and found that children rated parents as more fearful when giving reassurances in general but particularly when either fearful facial expression or falling tone of voice accompanied the words of reassurance. These children were picking up nuances in relational cues.
Distractions that are perceived as more authentically calm and positive, however, convey to children that it is acceptable to lower their reaction to the pain. This type of distraction technique may include talking to the child about something other than the procedure or the child’s illness. Furthermore, when children perceived a happy expression and a rising tone of voice as parental happiness, they believed that the parent was neither fearful nor distressed (McMurtry et al., 2010). In sum, children’s heightened ability to read the intentions behind adult cues during distractions make it increasingly important for adults to manage their own concerns and express genuine calmness.
Discussion
Pain assessment and treatment in young children presents special challenges to healthcare providers and parents. Based on current research, pain assessment is not an exact science in any age group. While health care providers understand that self-report is the gold standard for older children, adolescents, and adults; toddlers and preschoolers and even early elementary schoolers benefit from the addition of observational assessment tools such as FLACC, CHIPPS, CHEOPS, or BOPS depending on the situation (Bringuier et al., 2009; Frank et al., 1995; Hartrick & Kovan, 2002; Malviya et al., 2006; von Baeyer et al., 2009). Full term infants express their pain through cry, facial expression, and body movements and are not influenced by culture or social norms. Physiological signs may be reasonable indicators of pain in infancy when combined with observation of cry, facial expression and body movements. However, even at this age, pain expression is a bidirectional process between infant and parent or caregiver (Pillai Riddell & Racine, 2009). Assessment and treatment of pain during infancy should include the important influence of parents and their role in the child’s pain management. Sensitive caregivers who have well-attached infants are better able and more likely to provide appropriate soothing behaviors allowing infants to cope with stressful or painful situations (Jahromi et al., 2004; Schechter et al., 2007).
Toddlers continue to rely on their parents and other important adults, and considering this while treating pain may mean consciously incorporating adults for distraction and connection. Suggesting appropriate distractions for caregivers to employ during painful procedures such as playing peek-a-boo or blowing bubbles not only helps the child cope but gives the caregiver something positive to help their child and avoids empathetic behaviors such as parental apology or exaggerated reassurance (Jay et al., 1995; Schechter et al., 2007). Additionally, toddlers have a growing sense of self yet still emerging cognitive abilities, thus rendering temperature taking as upsetting as receiving a vaccination. Because of this quandary, physiological signs are not a good indicator of pain in this age group.
Preschoolers are able to begin reliably telling practitioners that they have pain. However some observation is still necessary as this age group may still be developing the language skills needed to express nuances especially regarding moderate pain levels. Allowing preschoolers to self-report pain will give them practice in using these tools although their ratings may not always reflect the child’s perceived pain; for this reason using an observational tool in addition to self report will yield a more reliable pain report (Hunter et al., 2000; von Baeyer et al., 2009). It is important for young children through elementary school to use a visual scale such as either a FACES-type of pain scale or other visual scale: Visual tools are helpful for young children who may not be able to visualize numbers and rate their pain accordingly (Garra et al., 2010; Hicks et al., 2001).
By school age, self-report is the most reliable method of pain assessment for typically developing children. School-age children have learned to self-regulate not only their actions but also their facial expressions based on cultural norms. Therefore, health care providers cannot use only observation to determine a child’s pain level validly or reliably.
Poor assessments and under treatment of infant and child pain remains a challenge for health care providers and caregivers (Kortesluoma et al., 2008; Twycross & Collis, 2012). The biggest asset in the assessment and treatment of pain in young children is parents: Children who have a relationship with parents or caregivers may be much more amenable to being assessed and are able to benefit from non-pharmacologic treatments. The use of non-pharmacological methods for procedures such as heel lancing, vaccinations, and even more painful procedures such as lumbar punctures have demonstrated effectiveness in decreasing infant and child pain and increasing coping (Harrington et al., 2012; Marin Gabriel et al., 2013; Smith et al., 1996; Taddio et al., 2009; Yoo et al., 2011). The consideration of developmental stage for the selection of assessment tools and non-pharmacologic treatment of pain will decrease children’s suffering during painful procedures. Educational awareness coupled with institutional changes resulting in system-wide cultural transformations could lead to a significant reduction in childhood suffering from pain.
Limitations
This narrative was not meant to be an exhaustive review of the literature. While every effort was made to include only well-designed studies and reviews, no formal rating of the quality of the studies or study design was carried out. While this review considered peer-reviewed studies and textbook sources, we did not consider grey literature, which may have given us additional, updated information. We only considered sources published in English. This exclusion may have eliminated a rich source of child development studies and non-pharmacologic interventions. However, cultural norms including child self-regulation can vary significantly and would deserve separate treatment beyond the scope of this synthesis. Use of cultural awareness when using interventions mentioned in this synthesis is important.
Recommendations for Health Care Providers
Use of an evidence-based approach is the key recommendation for practitioners. Research has created reliable and valid measurement tools for assessing pain in infants and young children. Practitioners and the institutions they work in must make it a priority to choose an appropriate tool for each age group, educate practitioners in its use, and learn to assess according to evidence and institutional policy. Studies have shown that when measurement tools are used as intended within institutional guidelines, infant and child pain and suffering can be well managed. Commitment to pain management is crucial and an institutional culture shift to the regular assessment, documentation, and management of pain must happen. With the growing number of studies showing solid evidence for both assessment and treatment of pain at each child developmental level, practitioners need an evidence-based approach and institutional commitment to make the practice changes necessary to treat children’s pain.
Recommendations for Researchers
A heartening number of studies have been performed in relation to the assessment and treatment of infant and child pain management strategies. A plethora of studies have examined various assessment tools for each age group. Future efforts to develop infant pain assessments may consider including observations of the strength of the parent-child attachment, or the apparent sensitivity of the parent to the infant as a way to ensure a more contextualized, and ecologically valid approach (Olds, 2008). One possible direction for researchers is to study nurses’ and other health care providers during pain assessment to identify barriers in using the assessment as it was intended. Moreover, it is essential to educate nurses regarding developmentally informed pain management both pharmacologic and especially non-pharmacologic. Simple non-pharmacologic methods are unknown to many healthcare providers thus their use is typically limited.
Recommendations for Policy-Makers
Recommendations for policy-makers are clear: (a) support research exploring the best treatment options for each developmental level, including both pharmacologic and non-pharmacological options, (b) support research investigating healthcare providers skill when implementing pain assessment and treatment practices, (c) mandate education programs for providers on the best practice for both assessment and treatment of pain, and (d) mandate the use of evidence-based practices in the assessment and treatment of pain in infants and children. Research has shown that untreated and undertreated pain in infancy leads to increased pain perception in children and an increased risk of chronic pain in adulthood. From a monetary perspective, chronic pain conditions are expensive not only in healthcare dollars spent in treatment but also in lost work productivity. In adolescents alone, chronic pain is estimated to cost $19.5 billion yearly, taking into account direct and indirect patients costs including hospital admissions, emergency and primary care visits, diagnostic costs, and lost parental work productivity (Groenewald, Essner, Wright, Fesinmeyer, & Palermo, 2014). For adults, Gaskin and Richard (2012) calculated that the total cost for pain including lost work productivity is between $560 to $635 billion dollars and is more than heart disease ($309 billion) and cancer ($243 billion) combined. Research and education are vital to decrease pain and suffering in infants, young children, and ultimately in adults resulting in a savings in healthcare costs from current levels.
Conclusion
Assessment and treatment of pain in infants and young children is challenging. While it is now recognized that infants feel pain from the moment they are born, healthcare has not yet completely come to terms with that fact in either the assessment or treatment of newborn pain. Traditional medical approaches often result in unnecessary pain when non-pharmacologic interventions such as swaddling or breastfeeding may soothe infants more quickly with fewer side effects. Toddlers may be the most challenging developmental stage for assessment although sample distraction techniques work well for treatment as increased awareness of self leads to indiscriminate distress from strange people and benign procedures as well as legitimately painful events. Preschool and early school age children are very open to non-pharmacological interventions such as video games, cartoons, stories, or counting which serve to focus the mind on something other than the painful event, thus decreasing the perception of pain and decreasing stress. Previous research on implementation suggests that institutional commitment and support is necessary for change to take place (Struder, 2003). Using a developmental approach to assessment and non-pharmacological treatment can lead to better outcomes. Cooperation between policy makers, institutions, and healthcare providers can result in less pain and suffering in infants and children.
Figure 2.
Wong-Baker FACES Pain Scale (From Hockenberry, M. J., Wilson, D., Winkelstein, M.L. (2005). Wong’s Essentials of Pediatric Nursing, 7th Ed., St. Louis, MO:Mosby, p. 1259. Used with permission. Copyright Mosby).
Table 1.
| Age Group (years) | Assessment Tools | Evidence-Based Non-Pharmacological Intervention |
|---|---|---|
| Infant (0–1) | CRIES, FLACC |
|
| Toddler (1–3) | FLACC, CHIPPS, CHEOPS |
|
| Pre-School (3–5) | FACES, FLACC, CHEOPS, BOPS |
|
| Early School Age (5–10) | FACES, VAS, VNS |
|
Assessment Tools and Non-Pharmacologic Interventions by Developmental Level
Highlights.
Pain is often untreated during routine medical procedures in pediatric patients
Using a developmental approach to assessment and non-pharmacological treatment can lead to better outcomes
Parental attachment is an important consideration when treating infants
Use of developmental stage is crucial for non-pharmacologic treatment in children
Acknowledgments
Funding: This work was supported by Interdisciplinary Training for Nurse Scientists In Cancer Survivorship Research (T32 NR011972) and NINR Ruth L. Kirschstein National Research Service Awards for Individual Predoctoral Fellows In Nursing Research (F31NR014762)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Susan E. Thrane, Email: thrane.2@osu.edu, Assistant Professor, College of Nursing, Ohio State University, 322 Newton Hall, 1585 Neil Avenue, Columbus, OH 43210.
Shannon Wanless, Email: swanless@pitt.edu, Assistant Professor, School of Education, University of Pittsburgh, 5937 Wesley W. Posvar Hall, 230 South Bouquet Street, Pittsburgh, PA 15260.
Susan M. Cohen, Email: cohensu@pitt.edu, Associate Professor, School of Nursing, University of Pittsburgh, 440 Victoria Building, 3500 Victoria Street, Pittsburgh, PA 15261.
Cynthia A. Danford, Email: danfordc@pitt.edu, Assistant Professor, School of Nursing, University of Pittsburgh, 458 Victoria Building, 3500 Victoria Street, Pittsburgh, PA 15261.
References
- Anand KJ International Evidence-Based Group for Neonatal P. Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med. 2001;155(2):173–180. doi: 10.1001/archpedi.155.2.173. [DOI] [PubMed] [Google Scholar]
- Bembich S, Davanzo R, Brovedani P, Clarici A, Massaccesi S, Demarini S. Functional neuroimaging of breastfeeding analgesia by multichannel near-infrared spectroscopy. Neonatology. 2013;104(4):255–259. doi: 10.1159/000353386. [DOI] [PubMed] [Google Scholar]
- Benjamin L. Pain management in sickle cell disease: palliative care begins at birth? American Society of Hematology Educational Program. 2008:466–474. doi: 10.1182/asheducation-2008.1.466. [DOI] [PubMed] [Google Scholar]
- Blount RL, Corbin SM, Sturges JW, Wolfe VV, Prater JM, James D. The relationship between adults’ behavior and chil coping and distress during BMA/LP procedures: A sequential analysis. Behavior Therapy. 1989;20(4):585–601. doi: 10.1016/S0005-7894(89)80136-4. [DOI] [Google Scholar]
- Bringuier S, Picot MC, Dadure C, Rochette A, Raux O, Boulhais M, Capdevila X. A prospective comparison of post-surgical behavioral pain scales in preschoolers highlighting the risk of false evaluations. Pain. 2009;145(1–2):60–68. doi: 10.1016/j.pain.2009.05.012. [DOI] [PubMed] [Google Scholar]
- Buttner W, Finke W. Analysis of behavioural and physiological parameters for the assessment of postoperative analgesic demand in newborns, infants and young children: a comprehensive report on seven consecutive studies. Paediatr Anaesth. 2000;10(3):303–318. doi: 10.1046/j.1460-9592.2000.00530.x. [DOI] [PubMed] [Google Scholar]
- Chen X, French DC. Children’s social competence in cultural context. Annu Rev Psychol. 2008;59:591–616. doi: 10.1146/annurev.psych.59.103006.093606. [DOI] [PubMed] [Google Scholar]
- Dixey P, Seiler J, Woodie JA, Grantham CH, Carmon MC. Do cartoon stickers given after a hemoglobin finger stick influence preschoolers’ pain perception? J Pediatr Health Care. 2008;22(6):378–382. doi: 10.1016/j.pedhc.2008.04.014. [DOI] [PubMed] [Google Scholar]
- Fearon P, Hotopf M. Relation between headache in childhood and physical and psychiatric symptoms in adulthood: national birth cohort study. BMJ. 2001;322(7295):1145. doi: 10.1136/bmj.322.7295.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes A, Campbell-Yeo M, Johnston CC. Procedural pain management for neonates using nonpharmacological strategies: Part 1: sensorial interventions. Adv Neonatal Care. 2011;11(4):235–241. doi: 10.1097/ANC.0b013e318225a2c2. [DOI] [PubMed] [Google Scholar]
- Fitzgerald M, Walker SM. Infant pain management: a developmental neurobiological approach. Nat Clin Pract Neurol. 2009;5(1):35–50. doi: 10.1038/ncpneuro0984. [DOI] [PubMed] [Google Scholar]
- Frank NC, Blount RL, Smith AJ, Manimala MR, Martin JK. Parent and staff behavior, previous child medical experience, and maternal anxiety as they relate to child procedural distress and coping. J Pediatr Psychol. 1995;20(3):277–289. doi: 10.1093/jpepsy/20.3.277. [DOI] [PubMed] [Google Scholar]
- Garra G, Singer AJ, Taira BR, Chohan J, Cardoz H, Chisena E, Thode HC., Jr Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med. 2010;17(1):50–54. doi: 10.1111/j.1553-2712.2009.00620.x. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- Groenewald CB, Essner BS, Wright D, Fesinmeyer MD, Palermo TM. The economic costs of chronic pain among a cohort of treatment-seeking adolescents in the United States. J Pain. 2014;15(9):925–933. doi: 10.1016/j.jpain.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington JW, Logan S, Harwell C, Gardner J, Swingle J, McGuire E, Santos R. Effective analgesia using physical interventions for infant immunizations. Pediatrics. 2012;129(5):815–822. doi: 10.1542/peds.2011-1607. [DOI] [PubMed] [Google Scholar]
- Hartrick CT, Kovan JP. Pain assessment following general anesthesia using the Toddler Preschooler Postoperative Pain Scale: a comparative study. J Clin Anesth. 2002;14(6):411–415. doi: 10.1016/s0952-8180(02)00389-6. [DOI] [PubMed] [Google Scholar]
- Hesselgard K, Larsson S, Romner B, Stromblad LG, Reinstrup P. Validity and reliability of the Behavioural Observational Pain Scale for postoperative pain measurement in children 1–7 years of age. Pediatr Crit Care Med. 2007;8(2):102–108. doi: 10.1097/01.PCC.0000257098.32268.AA. [DOI] [PubMed] [Google Scholar]
- Hicks CL, von Baeyer CL, Spafford PA, van Korlaar I, Goodenough B. The Faces Pain Scale-Revised: toward a common metric in pediatric pain measurement. Pain. 2001;93(2):173–183. doi: 10.1016/S0304-3959(01)00314-1. [DOI] [PubMed] [Google Scholar]
- Huguet A, Stinson JN, McGrath PJ. Measurement of self-reported pain intensity in children and adolescents. J Psychosom Res. 2010;68(4):329–336. doi: 10.1016/j.jpsychores.2009.06.003. [DOI] [PubMed] [Google Scholar]
- Hunter M, McDowell L, Hennessy R, Cassey J. An evaluation of the Faces Pain Scale with young children. J Pain Symptom Manage. 2000;20(2):122–129. doi: 10.1016/s0885-3924(00)00171-8. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Relieving pain in America: A blueprint for transforming prevention, care, education and research. 2011 Retrieved April 23, 2012, 2012, from http://books.nap.edu/openbook.php?record_id=13172&page=1. [PubMed]
- International Association for the Study of Pain. IASP Taxonomy. 2012 Retrieved October 14, 2012, from http://www.iasp-pain.org/Content/NavigationMenu/GeneralResourceLinks/PainDefinitions/default.htm - Pain.
- Jahromi LB, Putnam SP, Stifter CA. Maternal regulation of infant reactivity from 2 to 6 months. Dev Psychol. 2004;40(4):477–487. doi: 10.1037/0012-1649.40.4.477. [DOI] [PubMed] [Google Scholar]
- Jay S, Elliott CH, Fitzgibbons I, Woody P, Siegel S. A comparative study of cognitive behavior therapy versus general anesthesia for painful medical procedures in children. Pain. 1995;62(1):3–9. doi: 10.1016/0304-3959(94)00216-2. [DOI] [PubMed] [Google Scholar]
- Jones GT, Power C, Macfarlane GJ. Adverse events in childhood and chronic widespread pain in adult life: Results from the 1958 British Birth Cohort Study. Pain. 2009;143(1–2):92–96. doi: 10.1016/j.pain.2009.02.003. [DOI] [PubMed] [Google Scholar]
- Kortesluoma RL, Nikkonen M, Serlo W. “You just have to make the pain go away”--children’s experiences of pain management. Pain Manag Nurs. 2008;9(4):143–149. 149 e141–145. doi: 10.1016/j.pmn.2008.07.002. [DOI] [PubMed] [Google Scholar]
- Krechel SW, Bildner J. CRIES: a new neonatal postoperative pain measurement score. Initial testing of validity and reliability. Paediatr Anaesth. 1995;5(1):53–61. doi: 10.1111/j.1460-9592.1995.tb00242.x. [DOI] [PubMed] [Google Scholar]
- MacCoby EE, Martin CN. Socialization in the context of the family: Parent-child interaction. In: Hetherington EM, editor. Handbook of Child Psychology. Socialization, Personality and Social Development. Vol. 4. New York: Wiley; 1983. pp. 1–102. [Google Scholar]
- Malviya S, Voepel-Lewis T, Burke C, Merkel S, Tait AR. The revised FLACC observational pain tool: improved reliability and validity for pain assessment in children with cognitive impairment. Paediatr Anaesth. 2006;16(3):258–265. doi: 10.1111/j.1460-9592.2005.01773.x. [DOI] [PubMed] [Google Scholar]
- Manne SL, Redd WH, Jacobsen PB, Gorfinkle K, Schorr O, Rapkin B. Behavioral intervention to reduce child and parent distress during venipuncture. J Consult Clin Psychol. 1990;58(5):565–572. doi: 10.1037//0022-006x.58.5.565. [DOI] [PubMed] [Google Scholar]
- Marin Gabriel MA, del Rey Hurtado de Mendoza B, Jimenez Figueroa L, Medina V, Iglesias Fernandez B, Vazquez Rodriguez M, Medina Malagon L. Analgesia with breastfeeding in addition to skin-to-skin contact during heel prick. Arch Dis Child Fetal Neonatal Ed. 2013;98(6):F499–503. doi: 10.1136/archdischild-2012-302921. [DOI] [PubMed] [Google Scholar]
- McGrath PA, Brown SC. Paediatric palliative medicine. In: Doyle D, Hanks G, Cherny N, Calman K, editors. Oxford textbook of palliative medicine. 3. New York: Oxford University Press; 2005. [Google Scholar]
- McMurtry CM, Chambers CT, McGrath PJ, Asp E. When “don’t worry” communicates fear: Children’s perceptions of parental reassurance and distraction during a painful medical procedure. Pain. 2010;150(1):52–58. doi: 10.1016/j.pain.2010.02.021. [DOI] [PubMed] [Google Scholar]
- Merkel S, Voepel-Lewis T, Malviya S. Pain assessment in infants and young children: the FLACC scale. Am J Nurs. 2002;102(10):55–58. doi: 10.1097/00000446-200210000-00024. [DOI] [PubMed] [Google Scholar]
- Nguyen TN, Nilsson S, Hellstrom AL, Bengtson A. Music therapy to reduce pain and anxiety in children with cancer undergoing lumbar puncture: a randomized clinical trial. J Pediatr Oncol Nurs. 2010;27(3):146–155. doi: 10.1177/1043454209355983. [DOI] [PubMed] [Google Scholar]
- Olds DL. Preventing Child Maltreatment and Crime with Prenatal and Infancy Support of Parents: The Nurse-Family Partnership. J Scand Stud Criminol Crime Prev. 2008;9(S1):2–24. doi: 10.1080/14043850802450096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillai Riddell R, Racine N. Assessing pain in infancy: the caregiver context. Pain Res Manag. 2009;14(1):27–32. doi: 10.1155/2009/410725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post-White J, Fitzgerald M, Savik K, Hooke MC, Hannahan AB, Sencer SF. Massage therapy for children with cancer. J Pediatr Oncol Nurs. 2009;26(1):16–28. doi: 10.1177/1043454208323295. [DOI] [PubMed] [Google Scholar]
- Schechter NL, Zempsky WT, Cohen LL, McGrath PJ, McMurtry CM, Bright NS. Pain reduction during pediatric immunizations: evidence-based review and recommendations. Pediatrics. 2007;119(5):e1184–1198. doi: 10.1542/peds.2006-1107. [DOI] [PubMed] [Google Scholar]
- Shah PS, Herbozo C, Aliwalas LL, Shah VS. Breastfeeding or breast milk for procedural pain in neonates. Cochrane Database Syst Rev. 2012;12:CD004950. doi: 10.1002/14651858.CD004950.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JT, Barabasz A, Barabasz M. Comparison of hypnosis and distraction in severely ill children undergoing painful medical procedures. Journal of Counseling Psychology. 1996;43(2):187–195. [Google Scholar]
- Spence K, Henderson-Smart D, New K, Evans C, Whitelaw J, Woolnough R. Evidenced-based clinical practice guideline for management of newborn pain. Journal of Paediatrics and Child Health. 2009;46:184–192. doi: 10.1111/j.1440-1754.2009.01659.x. [DOI] [PubMed] [Google Scholar]
- Stevens B. Pain assessment and management in infants with cancer. Pediatr Blood Cancer. 2007;49(7 Suppl):1097–1101. doi: 10.1002/pbc.21347. [DOI] [PubMed] [Google Scholar]
- Stevens B, Yamada J, Ohlsson A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev. 2010;(1):CD001069. doi: 10.1002/14651858.CD001069.pub3. [DOI] [PubMed] [Google Scholar]
- Struder Q. Hardwiring Excellence. Gulf Breeze, FL: Fire Starter Publishing; 2003. [Google Scholar]
- Taddio A, Chambers CT, Halperin SA, Ipp M, Lockett D, Rieder MJ, Shah V. Inadequate pain management during routine childhood immunizations: the nerve of it. Clin Ther. 2009;31(Suppl 2):S152–167. doi: 10.1016/j.clinthera.2009.07.022. [DOI] [PubMed] [Google Scholar]
- Twycross A, Collis S. How well is acute pain in children managed? A snapshot in one English hospital. Pain Management Nursing, in press. 2012 doi: 10.1016/j.pmn.2012.01.003. [DOI] [PubMed] [Google Scholar]
- van Dijk M, Peters JW, Bouwmeester NJ, Tibboel D. Are postoperative pain instruments useful for specific groups of vulnerable infants? Clin Perinatol. 2002;29(3):469–491. x. doi: 10.1016/s0095-5108(02)00015-5. [DOI] [PubMed] [Google Scholar]
- von Baeyer CL, Forsyth SJ, Stanford EA, Watson M, Chambers CT. Response biases in preschool children’s ratings of pain in hypothetical situations. Eur J Pain. 2009;13(2):209–213. doi: 10.1016/j.ejpain.2008.03.017. [DOI] [PubMed] [Google Scholar]
- Weiss KE, Dahlquist LM, Wohlheiter K. The effects of interactive and passive distraction on cold pressor pain in preschool-aged children. J Pediatr Psychol. 2011;36(7):816–826. doi: 10.1093/jpepsy/jsq125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf CJ. Central sensitization: uncovering the relation between pain and plasticity. Anesthesiology. 2007;106(4):864–867. doi: 10.1097/01.anes.0000264769.87038.55. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO guidelines on the pharmacological treatment of persisting pain in children with medical illnesses. 2012:172. Retrieved from http://whqlibdoc.who.int/publications/2012/9789241548120_Guidelines.pdf. [PubMed]
- Yoo H, Kim S, Hur HK, Kim HS. The effects of an animation distraction intervention on pain response of preschool children during venipuncture. Appl Nurs Res. 2011;24(2):94–100. doi: 10.1016/j.apnr.2009.03.005. [DOI] [PubMed] [Google Scholar]
- Zhou Q, Eisenberg N, Wang Y, Reiser M. Chinese children’s effortful control and dispositional anger/frustration: Relations to parenting styles and children’s social functioning. Dev Psychol. 2004;40(3):352–366. doi: 10.1037/0012-1649.40.3.352. [DOI] [PubMed] [Google Scholar]