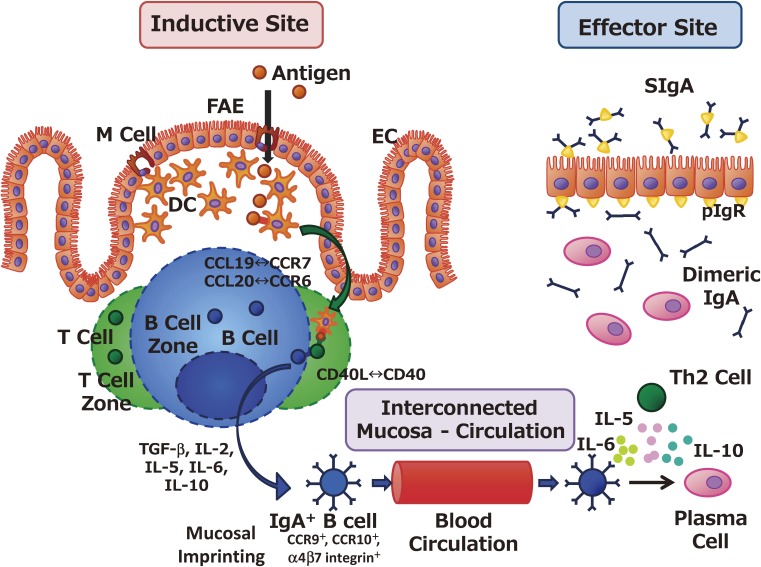
Figure 1.
Coordination between inductive and effector sites for the induction and regulation of antigen-specific mucosal immune responses. Antigens in the lumens of the gastrointestinal tract, nasal cavity, and tear ducts are endocytosed by M cells located on the follicle-associated epithelium (FAE) of the mucosa-associated lymphoid tissues. In the case of gut-associated lymphoid tissue or Peyer’s patches, M cells located in the FAE form the subepithelial dome structure, and antigen-presenting cells such as dendritic cells (DCs) lie immediately beneath the FAE. M-cell–endocytosed antigens are immediately processed by DCs, which transport antigens to underlying T cell zones through molecular interactions such as CCL19–CCR7 and CCL20–CCR6. Antigen-primed T cells support the induction of IgA-committed B cells (IgA+ B cells) owing to the biologic influences of transforming growth factor (TGF)-β, IL-2, IL-5, IL-6, IL-10, and the CD40–CD40 ligand (CD40L) interaction. In addition, IgA+ B cells acquire mucosal-imprinting molecules, such as CCR9, CCR10, and α4β7 integrin, and subsequently migrate to the effector sites. At the effector sites (e.g., the intestinal lamina propria), IgA+ B cells differentiate into plasma cells after stimulation by the IgA-enhancing cytokines IL-5, IL-6, and IL-10, which are secreted by antigen-specific Th2 cells. Dimeric or polymeric IgA secreted from plasma cells is transported to the mucosal surface as secretory IgA (SIgA) through the binding to polymeric Ig receptor expressed on the basal membrane of epithelial cells (ECs).