Abstract
Purpose: The purpose of this study was to identify the influence of pelvic incidence (PI) on spinopelvic parameters in patients with degenerative lumbar scoliosis (DLS) and compare them with those of a normal population. Methods: There were two groups in this study. One group was composed by 136 patients with DLS and another was composed by 120 participants free of spinal disease. In each group there were three subgroups according to PI, which were low (PI less than 45°), middle (PI between 45° and 60°) and high PI group (PI more than 60°). Sagittal spinopelvic parameters were compared between the DLS patients and asymptomatic participants in each PI group. Results: The number of DLS patients with low, middle, and high PI were 38 (27.9%), 50 (36.8%), and 48 (35.3%), respectively. In the control group, the number of low, middle, and high PI participants were 52 (43.3%), 41 (34.2%), and 27 (22.5%), respectively. There were significant difference in PT, SS, LL, SVA and TLJ between the three subgroups in the DLS patients. Patients with high PI showed large TLJ, LL, PT, SS and small SVA. In the Control group and DLS group, PI determined pelvic orientation (PT, SS) and sagittal spinal parameters (LL, TLJ). In terms of correlation between SS and LL, between SS and TLJ, both DLS and Control groups showed significant correlations. In terms of correlation between PT and SVA, between PT and TLJ, only the DLS group showed a significant correlation. Compared with the asymptomatic participants, DLS patients showed a high PT and low SS as well as kyphotic TLJ, lumbar hypolordosis and thoracic hypokyphosis in all PI groups. Conclusions: The changes in spinopelvic parameters and pelvic compensatory mechanisms differ according to PI in patients with DLS, restoration of LL based on individual PI could help in accomplishing a balanced spinopelvic alignment.
Keywords: Pelvic incidence, spinopelvic parameters, degenerative lumbar scoliosis
Introduction
Pelvic incidence (PI), first described by Duval-Beaupere, is unique to each individual, not affected by posture [1]. Since PI is a summation of the sacral slope (SS) and pelvic tilt (PT), it is a useful descriptor of the global shape of the pelvis and of the position of the sacrum within the pelvic unit [2]. Previous reports demonstrate that PI regulates the sagittal alignment of the spine and pelvis in normal populations [3-6]. It is also reported that PI would maintain constant even if spinal deformity occurred [7]. Legaye J [8] proved that PI played an important role in regulating the sagittal curve of spine including the variety of SS and lordosis curve in adult scoliotic women. Bae JS [2] confirmed that PI regulates spinopelvic parameters in patients with sagittal imbalance due to lumbar degenerative kyphosis (LDK) and in normal population, spinopelvic parameters and pelvic compensatory mechanisms in LDK patients differ according to PI.
Degenerative lumbar scoliosis (DLS) is characterized as three-dimensional deformity, including axial rotation, coronal and sagittal vertebral tilting, and presents not only the scoliotic deformity in coronal plane, but also the lumbar hypo-lordosis in sagittal plane. Progression of scoliosis can verticalize the sacrum and displace the hip joint anteriorly, suggesting that a coronal deformity could affect both the pelvic orientation and sagittal spinal alignment [9]. The sagittal balance reconstruction is more important than scoliosis correction in relation to the health-related quality of life scores postoperatively. Proper knowledge of sagittal balance including spinal alignment and pelvic orientation is indispensable for spine surgeons to achieve successful outcomes in spinal operative procedures [10-12]. Realization of the correlation between the pelvic orientation (especially the PI) and degenerative scoliosis would be useful for decision making and surgical planning.
To the best of our knowledge, this study is the first to analyze the spinopelvic parameters in terms of PI in a large number of DLS patients. This study evaluates the influence of PI on spinopelvic parameters in patients with DLS and compares them with those of a normal population.
Materials and methods
Subjects
The study was performed retrospectively after Institutional Review Board approval in the Third Hospital of Hebei Medical University (2014-01-025). We declared that we had no financial and personal relationships with other people or organizations that can inappropriately influence this work. The inclusion criteria for recruitment were as follows: availability of Posterior-Anterior (PA) and Lateral (LAT) X-rays of spine and pelvis, visibility of both femoral heads on the LAT radiographs, age older than 50 years. The exclusion criteria: leg length discrepancy of more than 1 cm, subjects with a history or clinical signs of compression fractures, hip joint disease, or an obvious radiographic abnormality, such as spondylolysis, spondylolisthesis, or Scheuermann kyphosis.
The data of two population groups were analyzed. The first group comprised 136 patients with DLS. There were 117 women and 19 men, with a mean age of 59.6 years (SD 5.8 years; range 51-74 years). The second group comprised a normal population of 120 adults free of spinal disease. There were 104 women and 16 men, with a mean age of 60.5 years (SD 5.2 years; range 51-72 years). The 120 adults constituted the Control group for assessing the relationship between spine and pelvis for a normal population.
Radiographic evaluation
All radiograph were taken by the same technician, using the same X-ray machine with a constant cassette-to-X ray source distance of 200 cm. First, a full spine PA radiograph was taken, followed by a 30×90 cm LAT radiograph from the base of the skull to the femoral heads in a standardized freestanding position. Participants were made to stand up straight in a relaxed posture with their knees extended as much as possible, hips straight, and hands placed on a height-adjustable bar so that the arms were flexed at 30 degrees from the shoulder. Radiographic measurements were done in PACS (Picture Archiving Communications System).
The angular measurements were expressed in degrees, the spinopelvic parameters are listed below (Figure 1): 1. Scoliotic angle (SA) was measured between the most tilted vertebrae in PA X-ray. 2. Sagittal balance was determined by measuring the sagittal vertical axis (SVA) with a plumb line from center of C7 vertebral body to the posterior sacral prominence on LAT radiograph. 3. Thoracic kyphosis (TK) was measured from T5 superior endplate to T12 inferior endplate. 4. Thoracolumbar junction (TLJ) was measured from T10 superior endplate to L2 inferior endplate. 5. Lumbar lordosis (LL) was measured from T12 inferior endplate to S1 superior endplate by the Cobb method. 6. PI is defined as the angle between the line perpendicular to the sacral plate and the line connecting the midpoint of the sacral plate to the bicoxofemoral axis. 7. SS is the angle between the S1 superior endplate and a horizontal line. 8. PT is defined as the angle between a vertical line originating at the center of bi-coxofemoral axis and a line drawn between the same point and the middle of the superior endplate of S1.
Figure 1.
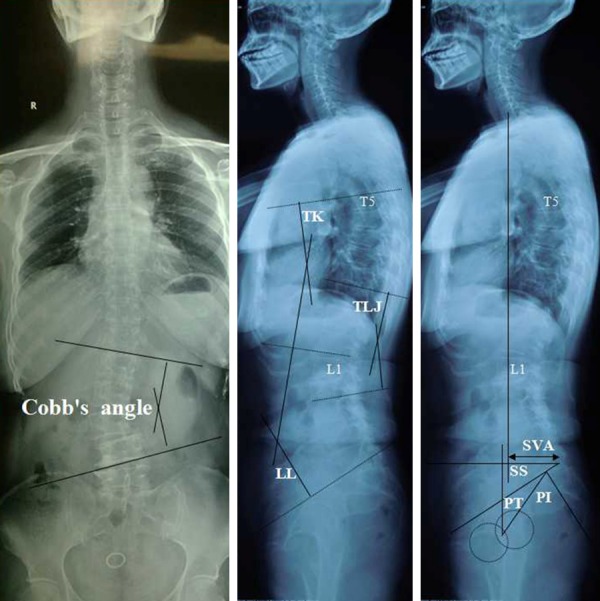
Scoliotic angle (SA) was measured in whole spine Postero-Anterior view (Left). Sagittal spinal parameters including lumbar lordosis (LL), thoracic kyphosis (TK), thoracolumbar junction (TLJ) were measured in whole spine Lateral view (Middle). Pelvic parameters including pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT) and sagittal vertical axis (SVA) were measured in whole spine Lateral view (Right).
In terms of PI, the DLS patients and asymptomatic adults were divided into three groups: low (PI less than 45°), middle (PI between 45° and 60°), and high PI groups (PI more than 60°) [13]. Sagittal spinopelvic parameters were compared between the DLS patients and asymptomatic adults in each PI group.
Statistical analysis
Data were analyzed using Statistical Product and Service Solutions software (version 13; SPSS, Chicago, IL). Independent two-sample t test and Mann-Whitney U test were used to compare the variables between DLS patients and asymptomatic adults. Kruskal-Wallis test and one-way analysis of variance were used to compare the variables among the three PI groups. The correlations between spinopelvic parameters were determined using the Pearson correlation coefficient. Statistical significance was accepted at the 0.05 alpha level.
Results
The number of DLS patients with low, middle, and high PI were 38 (27.9%), 50 (36.8%), and 48 (35.3%), respectively. In the control group, the number of low, middle, and high PI participants were 52 (43.3%), 41 (34.2%), and 27 (22.5%), respectively. Table 1 showed radiographic results of spine and pelvic parameters in DLS patients and the asymptomatic participants, the DLS patients demonstrated a lower TK, LL, SS, TLJ and a higher SVA, PT, PI.
Table 1.
Comparison of spine and pelvic parameters between DLS and Control group
| DLS | Control | P value | |
|---|---|---|---|
| TK | 20.5±3.0 | 27.7±3.4 | 0.006 |
| TLJ | -4.0±3.4 | 17.9±2.1 | <0.001 |
| LL | -33.1±3.6 | -41.6±5.8 | <0.001 |
| SVA (mm) | 39.8±4.3 | 11.9±1.4 | <0.001 |
| PI | 58.6±5.2 | 51.2±5.6 | 0.008 |
| PT | 35.3±3.1 | 21.1±2.4 | <0.001 |
| SS | 22.5±3.3 | 30.1±3.5 | <0.001 |
There were significant differences in PT, SS, and LL according to the PI group in the asymptomatic participants, participants with high PI presented with large LL, PT, SS (Table 2). There were significant differences in PT, SS, LL, SVA and TLJ according to the PI group in DLS patients, patients with high PI presented with large TLJ, LL, PT, SS and small SVA (Table 3).
Table 2.
Comparison of spine and pelvic parameters according to the PI in Control participants
| Low PI | Middle PI | High PI | P value | |
|---|---|---|---|---|
| TK | 26.4±3.0 | 28.3±2.7 | 29.3±2.8 | 0.341 |
| TLJ | 16.4±1.8 | 15.6±2.0 | 11.9±1.2 | 0.285 |
| LL | -34.4±3.6 | -43.9±5.1 | -51.8±5.7 | <0.001 |
| SVA (mm) | 12.6±1.8 | 11.9±1.0 | 10.4±1.1 | 0.287 |
| PT | 17.9±2.3 | 20.4±3.0 | 28.3±4.8 | <0.001 |
| SS | 23.7±3.5 | 31.7±4.1 | 39.4±4.3 | <0.001 |
Table 3.
Comparison of spine and pelvic parameters according to the PI group in DLS patients
| Low PI | Middle PI | High PI | P value | |
|---|---|---|---|---|
| TK | 18.4±2.3 | 20.6±3.2 | 22.1±3.1 | 0.208 |
| TLJ | 8.5±1.1 | -4.6±0.9 | -13.4±2.7 | <0.001 |
| LL | -24.8±2.4 | -32.2±4.6 | -40.7±3.8 | <0.001 |
| SVA (mm) | 52.4±5.1 | 38.9±4.0 | 30.7±4.6 | <0.001 |
| PT | 27.9±2.3 | 29.4±3.9 | 47.3±5.2 | <0.001 |
| SS | 14.7±2.5 | 24.8±3.1 | 26.4±3.3 | <0.001 |
| SA | 19.8±2.2 | 22.2±2.5 | 24.1±3.0 | 0.332 |
Table 4 showed the correlation coefficients between the parameters. In the Control group and DLS group, PI determined pelvic orientation (PT, SS) and sagittal spinal parameters (LL, TLJ). In terms of correlation between SS and LL, between SS and TLJ, both DLS and Control groups showed significant correlations. In terms of correlation between PT and SVA, between PT and TLJ, only the DLS group showed a significant correlation.
Table 4.
Correlation coefficients between the spine and pelvic parameters
| Spino-pelvic parameters | DLS group | Control group | ||
|---|---|---|---|---|
|
| ||||
| R | P | R | P | |
| PI-SS | 0.549 | <0.001 | 0.775 | <0.001 |
| PI-PT | 0.510 | <0.001 | 0.812 | <0.001 |
| PI-LL | 0.462 | <0.001 | 0.413 | 0.010 |
| PI-TLJ | 0.427 | <0.001 | 0.371 | 0.029 |
| PI-TK | 0.211 | 0.124 | 0.158 | 0.213 |
| PI-SVA | -0.357 | 0.001 | -0.189 | 0.114 |
| PI-SA | 0.268 | 0.092 | - | - |
| SS-LL | -0.510 | <0.001 | -0.714 | <0.001 |
| SS-TLJ | -0.403 | <0.001 | -0.357 | 0.032 |
| SS-TK | 0.259 | 0.098 | 0.212 | 0.102 |
| SS-PT | -0.230 | 0.107 | -0.387 | 0.026 |
| SS-SVA | -0.238 | 0.098 | -0.218 | 0.111 |
| SS-SA | 0.200 | 0.128 | - | - |
| PT-LL | 0.277 | 0.089 | 0.274 | 0.082 |
| PT-TLJ | -0.282 | 0.087 | -0.181 | 0.127 |
| PT-TK | 0.135 | 0.221 | 0.203 | 0.109 |
| PT-SVA | -0.485 | <0.001 | 0.136 | 0.215 |
| PT-SA | 0.228 | 0.102 | - | - |
| LL-TK | -0.179 | 0.165 | -0.427 | 0.009 |
| LL-SVA | -0.288 | 0.083 | -0.252 | 0.091 |
| LL-SA | -0.368 | 0.001 | - | - |
| TLJ-SVA | -0.248 | 0.114 | 0.284 | 0.071 |
| TLJ-SA | -0.116 | 0.252 | - | |
| TK-SVA | 0.157 | 0.239 | 0.132 | 0.351 |
| TK-SA | 0.186 | 0.161 | - | - |
| SVA-SA | 0.293 | 0.072 | - | - |
Compared with the asymptomatic adults, DLS patients showed a high PT and low SS as well as kyphotic TLJ, lumbar hypolordosis and thoracic hypokyphosis in all PI groups (Table 5).
Table 5.
Comparison of spine and pelvic parameters between DLS patients and control participants in low, middle, and high PI groups
| Low PI | Middle PI | High PI | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| DLS | Control | P value | DLS | Control | P value | DLS | Control | P value | |
| TK | 18.4±2.3 | 26.4±3.0 | 0.002 | 20.6±3.2 | 28.3±2.7 | 0.007 | 22.1±3.1 | 29.3±2.8 | 0.012 |
| TLJ | 8.5±1.1 | 16.4±1.8 | <0.001 | -4.6±0.9 | 15.6±2.0 | <0.001 | -13.4±2.7 | 11.9±1.2 | <0.001 |
| LL | -24.8±2.4 | -34.4±3.6 | <0.001 | -32.2±4.6 | -43.9±5.1 | <0.001 | -40.7±3.8 | -51.8±5.7 | <0.001 |
| SVA | 52.4±5.1 | 12.6±1.8 | <0.001 | 38.9±4.0 | 11.9±1.0 | <0.001 | 30.7±4.6 | 10.4±1.1 | <0.001 |
| PT | 27.9±2.3 | 17.9±2.3 | <0.001 | 29.4±3.9 | 20.4±3.0 | <0.001 | 47.3±5.2 | 28.3±4.8 | <0.001 |
| SS | 14.7±2.5 | 23.7±3.5 | <0.001 | 24.8±3.1 | 31.7±4.1 | <0.001 | 26.4±3.3 | 39.4±4.3 | <0.001 |
Discussion
In the asymptomatic participants, a high PI is associated with a long curved LL, and a low PI is associated with a short flat LL (Figure 2), the lumbar curve is appropriate for one individual as it is assigned to the morphological shape of pelvis, consistent with previous literatures [13,14]. While in the DLS group, a high PI is associated with relatively preserved lordosis in the lumbar region with a flat or lordotic TLJ, and a low PI is associated with a pronounced hypo-lordosis in the lumbar region with a flat or kyphotic TLJ (Figure 3). In comparison with the asymptomatic adults, TK in DLS group was observed to be significantly decreased in all PI groups, all spino-pelvic parameters except TK were shown to have a significant correlation with PI. In other words, TK is independent of the value of PI, but it is significantly changed by DLS.
Figure 2.
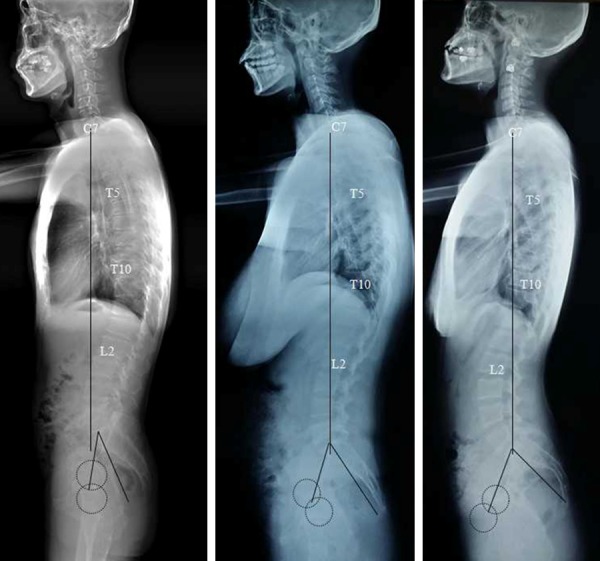
Whole spine Lateral radiographs of the asymptomatic participants in terms of low PI (Left), middle PI (Middle), and high PI (Right). Note the relatively flat, short lumbar lordosis in low PI and long curved lumbar lordosis extending to thoracolumbar junction in high PI.
Figure 3.

Whole spine Lateral radiographs of DLS in terms of low PI (Left), middle PI (Middle), and high PI (Right). Note the hypo-lordotic lumbar curve in low PI and relatively preserved lumbar lordosis in high PI.
Berthonnaud [5] put forward the theory that spine as a chain connects the head and pelvis with a group of segments which mechanically coordinate with each other to maintain a stable posture with minimum energy expenditure. Any change in one segment may cause the cascade affection on the adjacent level [15,16]. In the DLS group, pelvic parameters closely correlated with LL, there was negative correlation between PT and LL, both SS and SA positively correlated with LL. Progression of lumbar scoliosis is followed by a decrease in LL in terms of sagittal spinal parameter, a decrease in SS and increase in PT in terms of pelvic parameters.
It is well known that pelvis plays an important role in compensation mechanism to keep sagittal balance in normal people. The higher PI value, the greater ability of compensation for the pelvis. The compensatory pelvic retroversion for lumbar hypo-lordosis is important to prevent the forward inclination of the upper body and to maintain the spino-pelvic sagittal balance [17,18]. However, if the pelvic compensation is inadequate or reaches maximal, the patients may develop sagittal trunk imbalance and mostly characterized by forward leaning of the trunk with positive sagittal imbalance of the spine. In the DLS group, patients with low PI showed significant flattened SS and non-significant low PT than those with a middle PI, PT was shown to have a strong negative correlation with SVA, indicating that DLS patients with low PI were more inclined to suffer from sagittal imbalance due to the limitation of pelvic retroversion. Therefore, a flattened SS in low PI is the main compensatory mechanism for lumbar hypo-lordosis and the compensatory pelvic retroversion (increase of PT) in response to the aggravation of hypo-lordosis is limited when compared with that in middle PI. While patients with high PI showed non-significant steep SS and significant high PT than those with a middle PI. The high PI value means large range of retroversion capability of pelvis to lean backward for regaining the sagittal balance. Moreover, the TLJ in high PI is lordosis, contrary to the physiological alignment (neural or kyphosis, range from 0 degree to 20 degrees), and is also an important compensatory mechanism for the positive sagittal trunk imbalance.
Historically, surgical treatment for DLS patients always focused on correction of coronal plane deformity and less on the sagittal realignment [16]. Poor integration of the spino-pelvic relationship can lead to suboptimal correction and iatrogenic pathology such as a flat back [19,20]. Therefore, if the clinical symptoms develop and surgery is required in DLS patients, sagittal realignment should be paid more attention than the scoliosis correction, and the surgery planning should fulfill the ideal LL acceptable for their PI [21]. The mean value of PI in the DLS group was significantly higher than the Control group, suggesting that high PI is more prone to the development of DLS, and more restoration of LL is required during deformity correction surgery.
Considering the pelvic compensatory mechanism for lumbar hypo-lordosis varies according to the PI value, differences should be taken into consideration during the surgical planning for the DLS patients. The flattened SS is the main compensatory mechanism for lumbar hypo-lordosis in low PI, and significant correlation between SS and LL was detected in the DLS group. Accordingly, internal instrumentation within the lumbar region to realign the lumbar lordosis is enough to relieve the pelvic compensation in low PI. While high PT is the main compensatory mechanism for lumbar hypo-lordosis in high PI, however, the DLS group did not show a significant correlation between PT and LL, but showed a significant correlation between PT and TLJ, indicating that restoration of LL alone is inadequate for the release of compensatory pelvic retroversion, and the TLJ should be realigned from lordosis to neural or kyphosis by surgical intervention. Therefore, long-segment instrumentation involving the thoracolumbar region (the upper instrumented level in T10 or above) is necessary in high PI.
This study included a large number of subjects with strict criteria in both groups and with homogenous characters, the similar age and sex composition in the same ethnic background could reduce compounding factors. However, there were several limitations in this study. First, only Chinese Han individuals were included in this study and Ethnic variation was not covered. Second, multicenter study should be conducted in the further study. In summary, the changes in spinopelvic parameters and pelvic compensatory mechanisms differ according to PI in patients with DLS, restoration of LL based on individual PI could help in accomplishing a balanced spinopelvic alignment.
Disclosure of conflict of interest
None.
References
- 1.Duval-Beaupere G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20:451–62. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 2.Bae JS, Jang JS, Lee SH, Kim JU. Radiological analysis of lumbar degenerative kyphosis in relation to pelvic incidence. Spine J. 2012;12:1045–51. doi: 10.1016/j.spinee.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 3.Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Pélissier J. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–22. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:346–53. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 5.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–7. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 6.Mac-Thiong JM, Berthonnaud E, Dimar JR, Betz RR, Labelle H. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976) 2004;29:1642–7. doi: 10.1097/01.brs.0000132312.78469.7b. [DOI] [PubMed] [Google Scholar]
- 7.Lafage V, Schwab F, Skalli W, Hawkinson N, Gagey PM, Ondra S, Farcy JP. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine (Phila Pa 1976) 2008;33:1572–8. doi: 10.1097/BRS.0b013e31817886a2. [DOI] [PubMed] [Google Scholar]
- 8.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hong JY, Suh SW, Modi HN, Hur CY, Yang JH, Song HR. Correlation of Pelvic Orientation with Adult Scoliosis. J Spinal Disord Tech. 2010;23:461–6. doi: 10.1097/BSD.0b013e3181bf1a85. [DOI] [PubMed] [Google Scholar]
- 10.Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Roger B. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawakami M, Tamaki T, Ando M, Yamada H, Hashizume H, Yoshida M. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976) 2002;27:59–64. doi: 10.1097/00007632-200201010-00014. [DOI] [PubMed] [Google Scholar]
- 12.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024–9. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 13.Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–22. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007;16:1459–67. doi: 10.1007/s00586-006-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hresko MT, Labelle H, Roussouly P, Berthonnaud E. Classification of high grade spondylolisthesis based on pelvic version and spinal balance: possible rationale for reduction. Spine (Phila Pa 1976) 2007;32:2208–13. doi: 10.1097/BRS.0b013e31814b2cee. [DOI] [PubMed] [Google Scholar]
- 16.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224–31. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 17.Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007;61:981–6. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 18.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599–E606. doi: 10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 19.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024–9. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 20.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828–33. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 21.Bae JS, Jang JS, Lee SH, Kim JU. Radiological analysis of lumbar degenerative kyphosis in relation to pelvic incidence. Spine J. 2012;12:1045–51. doi: 10.1016/j.spinee.2012.10.011. [DOI] [PubMed] [Google Scholar]


