SUMMARY
The aim of this study is to investigate whether, in addition to intratympanic steroid therapy, additional hyperbaric oxygen therapy (HBOT) sessions per day (twice a day for 5 days) is more useful than one session per day for 10 days in patients affected by severe and profound idiopathic sudden sensorineural hearing loss (ISSNHL). A total of 55 patients affected by unilateral severe and profound ISSNHL were recruited. Two protocols were adopted. In the first, 27 patients (13 with profound and 14 with severe hearing loss) underwent one session of HBOT per day for 10 days, 6 days a week. An HBOT session comprised a period of 14 minutes air compression followed by 90 min at 2.4 atm absolute (ATA) followed by a decompression period of 15 min in oxygen. Patients breathed 100% oxygen through an appropriate mask checked for leaks. Patients were given 0.4 ml of 62.5 mg/ml of intratympanic prednisolone during the first three days of the protocol. In the second protocol, 28 patients (10 with profound and 18 with severe hearing loss) received 10 sessions of HBOT, twice a day for five days, 2.4 ATA 90 min 100% oxygen. The intratympanic injections of prednisolone were given between the two sessions of HBOT during the first three days of the protocol. Since there were no significant differences in hearing outcomes between the two protocols, the present study shows that the protocol of two sessions of HBOT per day is a valid treatment and equally effective as the one HBOT session per day, but with shorter treatment time.
KEY WORDS: Deafness, Prednisolone, Hypoxia, Pure-tone average, Cochlea, Inner ear
RIASSUNTO
La finalità dello studio è stata quella di investigare se, in pazienti affetti da ipoacusia improvvisa di grado severo e profondo, un numero maggiore di sedute giornaliere di ossigenoterapia iperbarica (due volte al giorno per 5 giorni) in associazione alla terapia steroidea intratimpanica, risulti più efficace della tradizionale sessione giornaliera di ossigenoterapia iperbarica effettuata per 10 giorni. 55 pazienti affetti da ipoacusia idiopatica unilaterale severa e profonda sono stati reclutati nello studio. Sono stati utilizzati due diversi protocolli terapeutici: il primo è consistito di 27 pazienti (13 con ipoacusia improvvisa profonda e 14 con ipoacusia improvvisa severa) che sono stati sottoposti ad una sessione di camera iperbarica giornaliera per un totale di 10 giorni (sei giorni a settimana). La sessione di camera iperbarica è consistita in un periodo di 14 minuti di compressione in aria seguiti da un periodo di trattamento a 2,4 atmosfere assolute (ATA) per 90 minuti e poi ad un successivo periodo di decompressione di 15 minuti in ossigeno. I pazienti hanno respirato ossigeno al 100% attraverso un'apposita maschera. Ai pazienti è stata somministrata una dose intratimpanica di 0.4 ml di prednisolone a 62,5 mg/ ml durante i primi tre giorni del protocollo. Il secondo protocollo è consistito di 28 pazienti (10 con ipoacusia profonde 18 con ipoacusia severa) che hanno ricevuto 10 trattamenti di camera iperbarica 2 volte al giorno 2,4 ATA, 90 minuti con ossigeno al 100%. Le infiltrazioni intratimpaniche di prednisolone sono state effettuate nel tempo intercorrente tra le due sessioni giornaliere di camera iperbarica durante i primi tre giorni del protocollo. Lo studio, non avendo evidenziato alcuna significativa differenza in termini di risultati uditivi tra i due protocolli sperimentali, permette di considerare il protocollo con la doppia sessione giornaliera di camera iperbarica una valida alternativa alla sessione unica giornaliera garantendo una significativa riduzione della durata complessiva della terapia.
Introduction
Idiopathic sudden sensorineural hearing loss (ISSNHL) is defined by the US National Institute for Deafness and Communication Disorders as a decline in hearing over 3 days or less, affecting three or more contiguous audiometric frequencies by 30 dB or more, with no identifiable aetiology 1. The treatment of patients with ISSNHL varies at different otological centres, but corticosteroids are considered the gold standard therapy 2.
In the literature a number of different regimens have been proposed as therapy for ISSNHL including vasodilators, anticoagulants, antioxidants, plasma expanders, antiviral agents, H.E.L.P. apheresis, carbogen and corticosteroids 3-5. Hyperbaric oxygen therapy (HBOT) is also used in ISSNHL to increase the partial oxygen pressure and to improve the blood profile and microcirculation. Solubility of gases in liquids depends on pressure, and during HBOT, due to the increased external pressure, a much larger amount of oxygen enters the blood from the alveoli. Blood with a higher concentration of oxygen crossing from the thin alveolar walls is transported through the bloodstream to all parts of the body. The more dissolved oxygen is in the blood, the better it gets into the organs and tissues 6 7.
In 2002 Aslan et al. demonstrated the efficacy of one daily HBOT session in addition to conventional treatment modalities for ISSNHL 8. In 2012, the efficacy of one daily session of HBOT was demonstrated in association with short duration intratympanic steroid therapy (ITS) in patients affected by severe and profound ISSNHL known to be less responsive to systemic steroid treatment 9.
It is also known that an increase in hyperbaric sessions per day significantly improves soft tissue and bone recovery, wound healing, infection control, ulcers and compromised flap recovery 10 11. In 2011, Thom et al. demonstrated that HBOT can mobilize bone marrow stem cells by stimulating nitric oxide synthase. It was found that nitric oxide synthase activity is acutely increased in platelets following HBOT that remained elevated for at least 20 hours. HBOT stimulates vasculogenic stem cell mobilization from bone marrow of diabetics, and more cells are recruited to skin wounds 12.
The aim of this study is to investigate whether, in addition to ITS, a higher number of HBOT sessions per day (twice a day for 5 days) is more useful than one session per day for 10 days in patients affected by severe and profound ISSNHL.
Materials and methods
A total of 55 patients affected by unilateral severe and profound ISSNHL who were examined by the ENT Emergency Room staff of the Department of Sensory Organs of Sapienza Università di Roma from January 2012 to December 2013 were enrolled in this randomised pilot study. Severe ISSNHL is defined by a pure-tone average (PTA) between 70 and 90 dB and profound ISSNHL by a PTA > 90 dB. All patients met the following inclusion criteria: age between 19 and 85 years, time elapsed between the onset of ISSNHL and beginning of therapy not exceeding 15 days, no previous therapy for ISSNHL, no surgery affecting the ipsilateral ear and no retrocochlear disease, no acoustic trauma and no autoimmune or fluctuating hearing loss. The exclusion criteria were: chronic bronco-pulmonary obstructive syndrome, emphysema, sinusitis, seizure syndrome, pregnancy and claustrophobia in a hyperbaric environment. Informed written consent was obtained from each patient.
Treatment strategies
Two protocols were adopted. The first (HBOT1) consisted of 27 patients (13 with profound and 14 with severe sudden hearing loss) who underwent one session of HBOT per day for 10 days in a multi-place hyperbaric chamber, 6 days a week. A HBOT session comprised a period of 14 min compression in air followed by a treatment period at 2.4 atm absolute (ATA) for 90 min and then a decompression period of 15 min in oxygen. Patients breathed 100% oxygen through an appropriate mask checked for leaks. Patients were given 0.4 ml of 62.5 mg/ml of intratympanic prednisolone (Deltacortene Sol® Bruno Farmaceutici, Rome, Italy) before the HBOT session during the first three days of the protocol. The IT injection technique has been reported 13.
The second protocol (HBOT2) consisted of 28 patients (10 with profound and 18 with severe sudden hearing loss) who received 10 sessions of HBOT, twice a day for five days, 2.4 ATA 90 min 100% oxygen in a multi-place hyperbaric chamber. Intratympanic injections of prednisolone were given between the two sessions of HBOT during the first three days of the protocol. Within each protocol, patients were homogenous according to age, sex and PTA.
Standard assessment
The standard assessment includes audiometric testing PTA and impedance audiometry, vestibular tests, routine serological test, coagulation, high resolution CT of temporal bone and MRI of the brain (specifically of the cerebellopontine angle with gadolinium).
Audiological evaluation and hearing improvement
All patients underwent evaluation of PTA immediately before the beginning of the treatment and one day after the last session of HBOT (11 days after HBOT1 treatment and 6 days after HBOT2). The results were compared. PTA was calculated as the mean of thresholds at the six frequencies (250, 500, 1000, 2000, 4000 and 8000 Hz).
Thresholds that could not be measured due to the limit of the audiometric equipment were "dummy coded" with the highest test level of audiometric equipment, as suggested in a recent study 14 15. In these cases they were set at 130 dB.
Criteria adopted for evaluating audiological improvement were based on those used by Furuhashi et al. 16 who classified the outcomes as complete recovery, marked improvement, partial improvement, or non-recovery. Successful treatment is defined as complete recovery or marked improvement in PTA at six frequencies (250, 500, 1000, 2000, 4000 and 8000 Hz) (Table I).
Table I.
Criteria used to define audiological improvement.
| Hearing Outcome | Furuhashi's criteria |
| Complete recovery* | PTA ≤ 25 dB or identical to the contralateral, non-affected ear |
| Marked improvement* | PTA improvement > 30 dB |
| Slight improvement | PTA improvement between 10 and 30 dB |
| No recovery | PTA improvement < 10 dB |
Successful treatment: complete recovery and marked recovery.
Statistical analysis
Statistical analysis on PTA values was performed using ANOV A two-way repeated measurements. Bonferroni post-hoc test was performed for the analysis of statistically significant interactions. Unpaired t-test was performed in the comparison between the two groups in the pre-treatment phase. Fisher's exact test was performed in the comparison of treatment outcomes between and within groups (HBOT1 and HBOT2 severe and profound hearing loss).
Results
PTA
The frequency averages of patients treated with the two protocols, before and after the therapy, is shown in Figure 1.
Fig. 1.
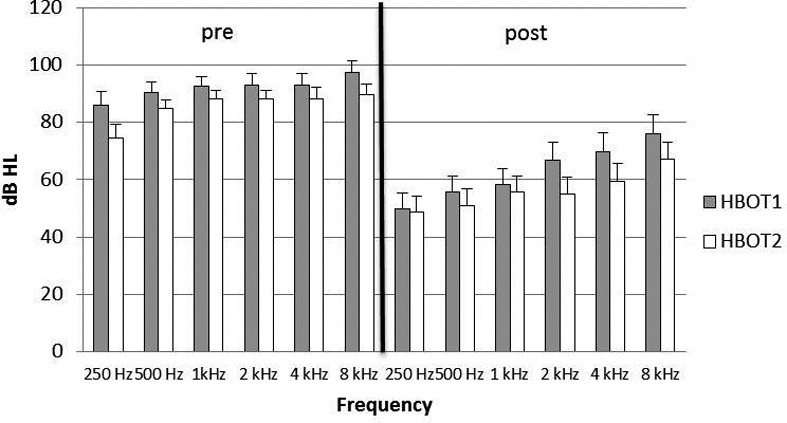
Threshold average of frequencies in the patients treated with the two protocols. Pre: before therapy; post: at the end of therapy.
Any statistically significant difference of PTA values was observed comparing the pre-treatment phase between the two groups HBOT1 and HBOT2 (p = 0.17).
In all patients the comparison of PTA before and after treatment showed a statistically significant reduction (p < 0.0001). The average PTA decreased for HBOT1 from 92.04 ± 18.6 to 62.65 ± 29.14, and for HBOT2 from 85.53 ± 16.3 to 56.07 ± 29.19 with a statistical significance of p < 0.001 for each protocol (Fig. 2). Comparing the results within the severe and profound hearing loss group a statistically significant reduction of PTA was observed, while no significant difference regarding the two protocols was seen (p = 0.27) (Fig. 3).
Fig. 2.
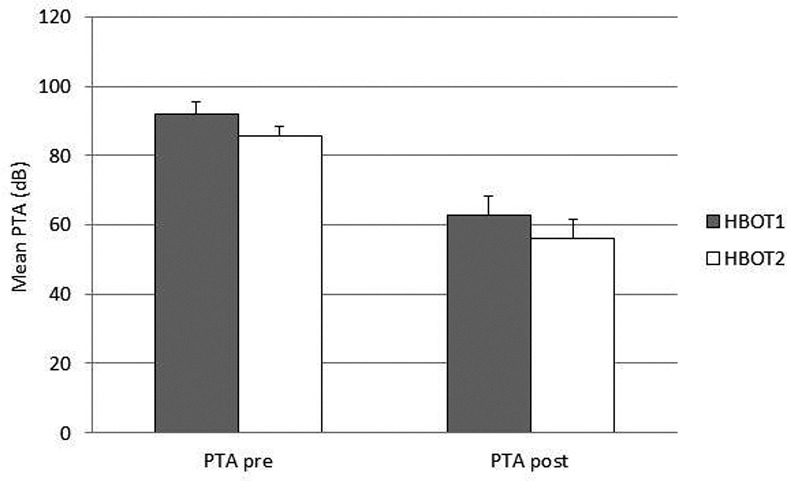
Average PTA for each protocol before and after treatment.
Fig. 3.
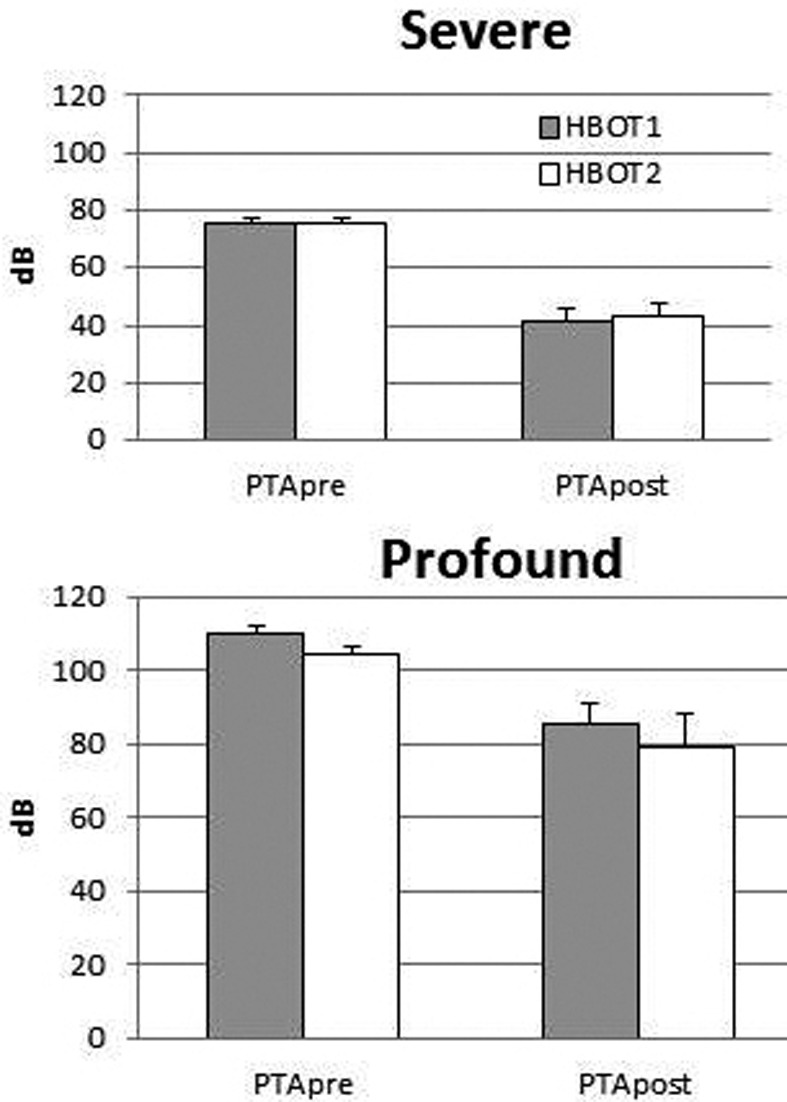
Mean PTA based on the two protocols in profound and severe hearing loss.
Clinical evaluation of hearing outcomes
According to the audiological criteria of Furuhashi, there was no significant difference between the two protocols (p = 0.58) (Table II).
Table II.
Audiological results according to Furuhashi's criteria.
| Hearing outcomes (Furuhashi's criteria) | Severe SSNHL | Profound SSNHL | ||
|---|---|---|---|---|
| HBOT1 n = 14 |
HBOT2 n = 18 |
HBOT1 n = 13 |
HBOT2 n = 10 |
|
| Successful treatment | 10 | 14 | 6 | 5 |
| Unsuccessful treatment | 4 | 4 | 7 | 5 |
No significant differences were observed in the audiometric division in severe or profound hearing loss (severe p = 0.7; profound p = 1) and between the two experimental groups (HBOT1 p = 0.25; HBOT2 p = 0.21) (Fig. 4).
Fig. 4.
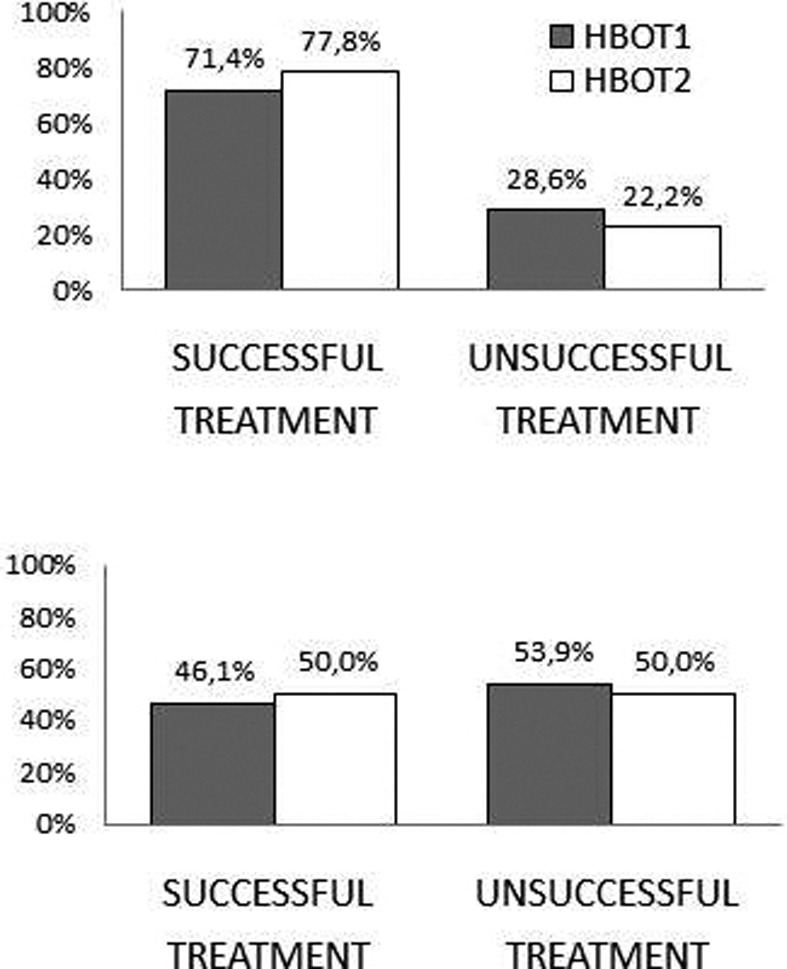
Hearing outcomes following Furuhashi's criteria based on the two protocols in severe (top) and profound (bottom) hearing loss.
Discussion
In the last few years, ITS injection has been considered a good treatment for ISSNHL as it permits the greatest possible intra-cochlear concentration of cortisone, without the risk of adverse systemic effects, although the exact mechanism in still unclear. In the literature, ITS injection is favoured not also as a first line therapy, but also as salvage therapy 17.
The logical basis for the use of HBOT in ISSNHL is linked to the pathogenetic hypothesis. Whatever the aetiology – vascular, viral, autoimmune, or metabolic – the final event triggering cochlear damage is always the same: hypoxia. Accumulation of CO2 leads to anaerobic glycolysis, acidosis, tissue oedema, a further reduction of blood flow and ultimately to increasingly serious oxygen debt, with evident consequences on homeostasis of inner and outer hair cells and labyrinthine fluids. Furthermore, HBOT has been shown to provide a significant additional effect when used in combination with a steroid therapy for ISSNHL 9.
To improve hearing outcomes in patients affected by ISSNHL, the present study proposed an increase in the frequency of HBOT sessions per day, as in the treatment of some other pathologies (crush syndrome, soft tissue infections, burns, etc.).
Regardless of the severity of the hearing loss, the results obtained show that patients with severe or profound hearing loss respond similarly to both protocols of ITS injection associated with one or two HBOT sessions per day. Considering the two protocols individually, both demonstrated the efficacy of the treatment for ISSNHL. The percentages of recovery and the values of PTA do not show any different effects with one session of HBOT per day or two, in combination with ITS.
Possible complications during HBOT include barotraumatic lesions (middle ear, nasal sinuses, inner ear, lung, teeth), oxygen toxicity (central nervous system, lung), confinement anxiety and ocular effects (myopia, cataract growth) 18. There are also some potential disadvantages to ITS such as otitis media, transient vertigo, otomycosis, perforations of tympanic membrane, myringitis 19 and pneumolabyrinth 20. In our study, no patient experienced these side effects.
Since there were no significant differences in hearing outcomes between the two regimens, the present study demonstrates that a protocol of two sessions of HBOT per day is a valid treatment and equally effective as the one HBOT session per day, with a shorter duration, and that it may also be less stressful and more acceptable for the patient. The protocol of two HBOT sessions per day could be more flexible and adaptable to the needs of patients.
References
- 1. National Institute of Health , author. Sudden deafness. Bethesda, MD: National Institute of Health NH publication; 2000. pp. 4757–4757. [Google Scholar]
- 2.Jarvis SJ, Giangrande V, John G, et al. Management of acute idiopathic sensorineural hearing loss: a survey of UK ENT consultants. Acta Otorhinolaryngol Ital. 2011;31:85–89. [PMC free article] [PubMed] [Google Scholar]
- 3.Schreiber BE, Agrup C, Haskard DO, et al. Sudden sensorineural hearing loss. Lancet. 2010;375:1203–1211. doi: 10.1016/S0140-6736(09)62071-7. [DOI] [PubMed] [Google Scholar]
- 4.Bianchin G., Russi G., Romano N., et al. Role of H.E.L.P.- apheresis in the treatment of sudden sensorineural hearing loss in a group of 230 patients. Acta Otorhinolaryngol Ital. 2011;31:395–398. [PMC free article] [PubMed] [Google Scholar]
- 5.Filipo R, Attanasio G, Russo FY, et al. Oral versus Short- Term Intratympanic Prednisolone Therapy for Idiopathic Sudden Hearing Loss. Audiol Neurotol. 2014;19:225–233. doi: 10.1159/000360069. [DOI] [PubMed] [Google Scholar]
- 6.Stachler RJ, Chandrasekhar SS, Archer SM, et al. Clinical practice guideline: sudden hearing loss. Otolaryngol Head Neck Surg. 2012;146(3 Suppl):S1–S35. doi: 10.1177/0194599812436449. [DOI] [PubMed] [Google Scholar]
- 7.Goto F, Fujita T, Kitani Y, et al. Hyperbaric oxygen and stellate ganglion blocks for idiopathic sudden hearing loss. Acta Otolaryngol. 1979;88:335–342. doi: 10.3109/00016487909137177. [DOI] [PubMed] [Google Scholar]
- 8.Vincey P, Mechineau Y, Lafond P, et al. Treatment of acute acoustic trauma. Comparative results of normovolemichemodilution. Rev Laryngol Otol Rhinol (Bord) 1987;108:339–341. [PubMed] [Google Scholar]
- 9.Aslan I, Oysu C, Veyseller B, et al. Does the addition of hyperbaric oxygen therapy to the conventional treatment modalities influence the outcome of sudden deafness? Otolaryngol Head Neck Surg. 2002;126:121–126. doi: 10.1067/mhn.2002.121915. [DOI] [PubMed] [Google Scholar]
- 10.Filipo R, Attanasio G, Viccaro M, et al. Hyperbaric oxygen therapy with short duration intratympanic steroid therapy for sudden hearing loss. Acta Otolaryngol. 2012;132:475–481. doi: 10.3109/00016489.2011.647360. [DOI] [PubMed] [Google Scholar]
- 11.Smolle-Jüttner FM, Pinter H, Neuhold KH, et al. Hyperbaric surgery and oxygen therapy in clostridial myonecrosis. Wien Klin Wochenschr. 1995;107:739–741. [PubMed] [Google Scholar]
- 12.Gustilo SJ, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures:a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Thom SR, Milovanova TN, Yang M, et al. Vasculogenic stem cell mobilization and wound recruitment in diabetic patients: increased cell number and intracellular regulatory protein content associated with hyperbaric oxygen therapy. 2011;19:149–161. doi: 10.1111/j.1524-475X.2010.00660.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Filipo R, Covelli E, Balsamo G, et al. Intratympanic prednisolone therapy for sudden sensorineural hearing loss: A new protocol. Acta Otolaryngol. 2010;130:1209–1213. doi: 10.3109/00016481003793766. [DOI] [PubMed] [Google Scholar]
- 15.Plontke SK, Löwenheim H, Mertens J, et al. Randomized, double blind, placebo controlled trial on the safety and efficacy of continuous intratympanic dexamethasone delivered via a round window catheter for severe to profound sudden idiopathic sensorineural hearing loss after failure of systemic therapy. Laryngoscope. 2009;119:359–369. doi: 10.1002/lary.20074. [DOI] [PubMed] [Google Scholar]
- 16.Chen CY, Halpin C, Rauch SD. Oral steroid treatment of sudden sensorineural hearing loss: a ten year retrospective analysis. Otol Neurotol. 2003;24:728–733. doi: 10.1097/00129492-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Furuhashi A, Matsuda K, Asahi K, et al. Sudden deafness: long term follow-up and recurrence. Clin Otolaryngol. 2002;27:458–463. doi: 10.1046/j.1365-2273.2002.00612.x. [DOI] [PubMed] [Google Scholar]
- 18.Plaza G1, Herráiz C. Intratympanic steroids for treatment of sudden hearing loss after failure of intravenous therapy. Otolaryngol Head Neck Surg. 2007;137:74–78. doi: 10.1016/j.otohns.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 19.Plafki C, Peters P, Almeling M, et al. Complications and side effects of hyperbaric oxygen therapy. Aviat Space Environ Med. 2000;71:119–124. [PubMed] [Google Scholar]
- 20.Covelli E, Attanasio G, Cagnoni L, et al. Pneumolabyrinth after intratympanic steroid injection in patient with prosthesis of the stapes: a case report. Am J Otolaryngol. 2013;34:759–761. doi: 10.1016/j.amjoto.2013.06.002. [DOI] [PubMed] [Google Scholar]


