Abstract
Context:
Standardized nursing handovers have been known to improve outcome, reduce error, and enhance communication. Few, if any, studies on nursing handovers have been conducted in the India.
Aim:
The aim was to study nursing handover practices in a Neurosciences Center in India.
Subjects and Methods:
This study was conducted in a 200 bedded public sector Neurosciences Center in New Delhi, to assess nursing handover practices across five wards, all shifts, weekdays, and weekends using a pretested checklist. Ten elements were observed under the categories of time, duration, process, nurse interaction, and patient communication.
Statistical Analysis:
Analysis of variance, Z-test, and Spearman's correlation coefficient.
Results:
Totally, 525 nursing handovers revealed varying compliance levels among (63%) time, place (76%), process (82%), staff interaction (53%), and patient communication (44%) related elements. Poorer compliance was seen in morning shifts and weekends; the difference being statistically significant. Bedside handovers were more frequent during weekends and night shifts and were positively correlated with increased staff interaction and patient communication and negatively related to handover duration. Though nurses showed better adherence to process related elements, background patient information, and assessment was explained less frequently. Differences between wards were insignificant except in categories of nurse interaction and patient communication which was better in the neurosurgery than neurology wards.
Conclusion:
Study revealed a need for a system change and standardization of handovers. Greater administrative commitment, use of technology, training, and leadership development will aid in continuity of care, promote patient safety, and ensure better outcomes.
Keywords: Neurosciences Center, nursing handover, weekend shifts
Introduction
Nursing handover is a communication that occurs between two shifts of nurses where the purpose is to communicate information about patients under the care of nurses.[1,2]
Various researches have proven that standardized nursing handover protocols improve outcome, reduce error, enhance communication among nurses, and interaction with patients.[3,4] Some studies have observed a decrease in length of hospital stay and, therefore, the cost of individual medical visits and fewer referrals.[5]
Considering the heavier patient load in Indian public sector hospitals, the lack of standardized protocols, it was considered to undertake the study on nursing handover practices in the Neurosciences Center.
Subjects and Methods
This descriptive and cross-sectional study was conducted in a 200 bedded Neurosciences Center of an apex public sector Tertiary Care Referral Hospital in New Delhi, India from January 2014 to April 2014. The handover practices by the nursing staff during shift change in all five wards of the Neurosciences Center formed the sample for the process of nonparticipant observation time, duration, process, nurse interaction, and patient communication, through nonparticipant observation. Handovers in each ward were observed both during weekdays and weekends using a pretested checklist for a period of 1-week from the corresponding Monday of the week to the subsequent Monday. In each nursing shift, handover practices in relation to all the patients under the charge of one staff nurse was observed. Handover of all 30 beds was done over the week to overcome individual staff nurse variations. Administrative nurses, inter-hospital transfer handovers, Intensive Care Unit (ICU) to ward, and private ward beds handovers were excluded from the study.
The pretested checklist was adopted from the implementation toolkit: Standard Key Principles for Clinical Handover by the Australian Medical Association (2006) and the Safe Handover: Safe Patients’ Guideline by the United Kingdom National Patient Safety Agency (2004).[6,7] A triple shift, 1-week pilot test was carried out in all the wards. This modified, validated checklist was then used to carry out the study.
The nursing checklist consisted of 10 elements under five categories with 10 boxes corresponding to the elements under each category [Table 1]. The mean value of all the handovers for that shift were taken as representative for that shift. Wards, shifts, and weekends were also analyzed independently and as groups. One-way and two-way analysis of variance (ANOVA significant <0.05), Z-test for difference of proportions (significant <0.01), and Spearman's correlation was used to analyze the data using the SPSS software used was an Institute licensed, IBM SPSS-Version 22 software.
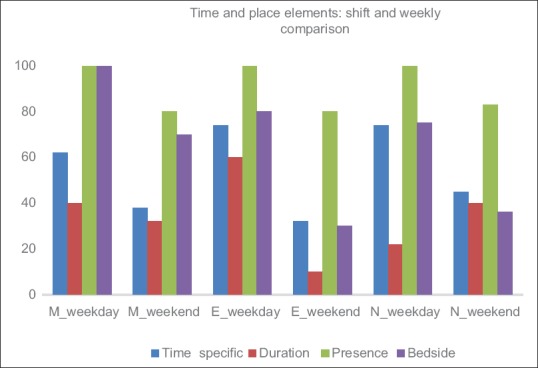
Table 1.
Nursing handover checklist used as tool
Results
The Neuroscience Center of the Tertiary Referral Center is a seven storied structure with 200 beds including general wards, ICU, and private wards. The inpatient wards which were included in the study comprised of five floors with 30 beds in each ward. Wards 1, 2, and 3 are Neurology wards and wards 4 and 5 are neurosurgery wards. The nursing shift handover occurs thrice in a day, morning shift (M), the evening shift (E), and the night shift (N) for the staff nurses.
Since each staff nurse is in-charge of five patients, in a 24 h period, 15 handover were observed. Thus, 105 handover (including 30 for the weekends) for a ward (corresponding to a week) and a total of 525 nursing handovers for the five wards were observed. Outcome was analyzed with regards to the parameters in each category against wards, shifts, weekdays, and over weekends:
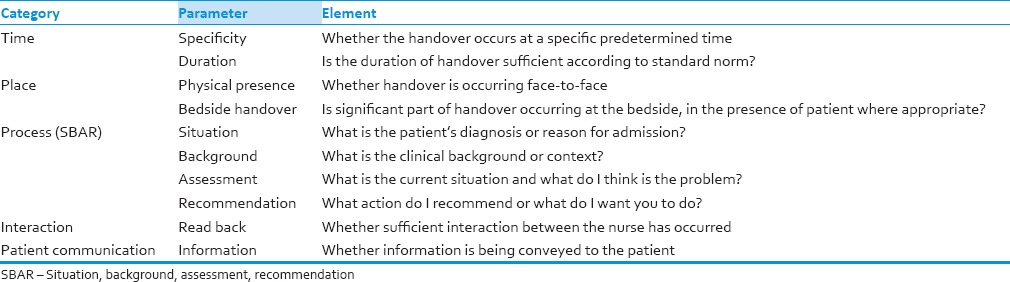
Time parameters
These included whether handover occurred at specific predetermined time and if the duration was sufficient. Weekday revealed a lower compliance during the morning shifts (62% and 40%) than in the evening (74% and 60%) and night shifts (45% and 40%), for both time specificity and duration [Figure 1]. The weekend compliance was lower in all the shifts in both parameters than their corresponding weekdays. The overall adherence was 63%. One-way ANOVA post-hoc test revealed that statistical difference was due to the morning shift, when all three shifts in all wards were analyzed (ANOVA significant = 0.023). Z-test for difference of proportions showed highly significant statistical difference between weekdays and weekends (Z-test significant = 0.004).
Figure 1.
The comparison between the “time” elements specificity and rtdduration of hand over across weekdays and weekends is shown. M represents morning shift, E represents evening shift, and N represents night shift. Weekend handovers were significantly deficient
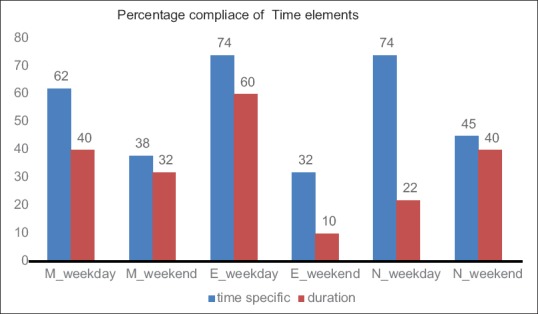
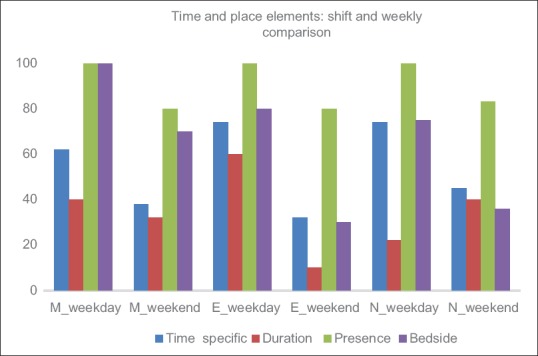
Place parameters
During weekdays, in all wards and in all shifts, nursing staff handover their charges in the physical presence of their colleague. Part of the handover occurred at bedside (83%). Overall compliance was 76%. Handovers that occurred in bedside had shorter duration. In addition, weekend and night shift staff had a higher propensity to do bedside handover [Figure 2]. One-way ANOVA test did not reveal statistically significant difference. However, two-way ANOVA test revealed a significant difference between time and place elements (two-way ANOVA significant = 0.03).
Figure 2.
Comparison between the elements of time and place categories over the weekdays and weekends shows a negative correlation between duration of handover and weekends. The compliance was poorer during morning and weekends
Process parameters
Situation, background, assessment, recommendation (SBAR) process elements were followed the best among all the five categories studied (aggregate 82%). Among the four elements, in all wards and across all shift, situation (86%) and recommendation (82%) had higher adherence among nurses than background (79%) and assessment (80.4%) [Figure 3]. However, the difference between all five wards statistically insignificant (two-way ANOVA signification = 0.454).
Figure 3.
Percentage compliance level between wards on the four elements of process category. The overall high compliance level among process elements did not show significant difference between wards
Staff interaction
The overall interaction among all nursing staff during handovers was low (52.8%), however, it was higher in the neurosurgery wards (wards 4 and 5) [Figure 4]. The difference was statistically significant (Z-test significant = 0.006). The task of “read back’’ or “repeat back” by the incoming nurse was being followed less often during the night shifts and weekends, but were not statistically significant.
Figure 4.
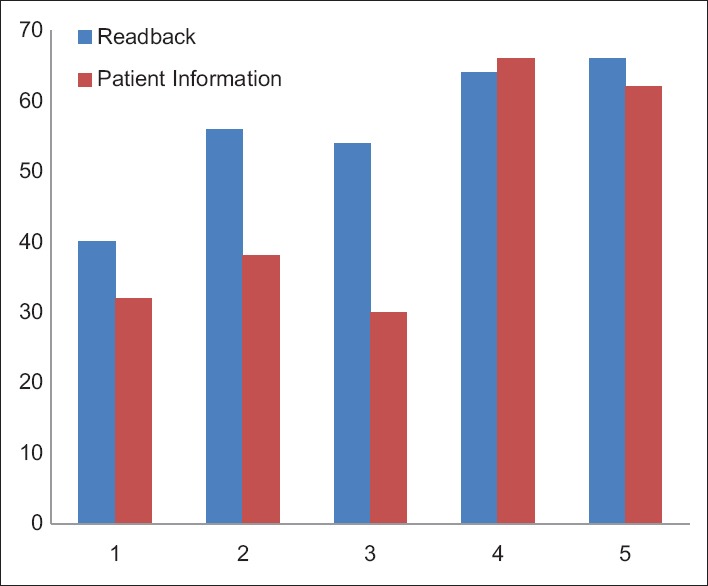
Comparison of staff interaction (read back) and patient information between wards. 1, 2, 3, 4, and 5 represent the respective wards. Neurosurgery wards (4 and 5) fared better than neurology wards with regards to nurse interaction and patient communication
Patient communication
Among all categories, patient communication was given the least priority (44.4%). However, the nursing staff working in the neurosurgery ward fared significantly better than their colleagues in the neurology ward [Figure 4]. (Z-test significant = 0.004). Although, communication was observed to be higher in the weekends, it may have been a chance finding. Overall compliance with respect to all the categories between specialties offered similar trends over shifts and days [Figure 5].
Figure 5.
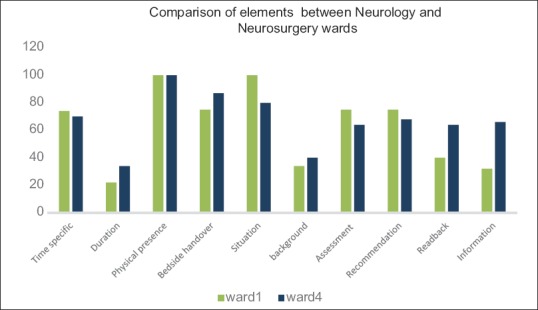
Inter specialty comparison is shown in percentage, overall 10 elements of handover showed largely similar trends across both, neurology and neurosurgery wards with significant difference only the categories of readback and patient information
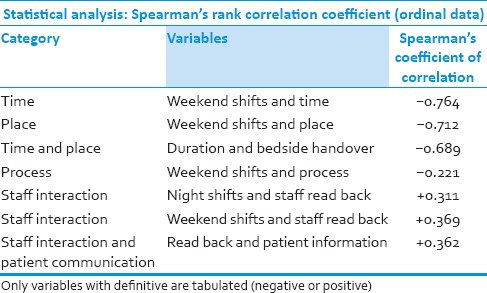
Strong negative correlation was observed between weekend shift and elements related to time (Spearman's coefficient of correlation: −0.764) and place (Spearman's coefficient of correlation: −0.712). Strong negative relationship was also observed between bedside handovers and duration of handover (Spearman's correlation coefficient: −0.689). Weak negative correlation was observed between weekend shifts and process (Spearman coefficient: −0.221) elements. Weekends and night shifts were found to be positively related to staff interaction (Spearman coefficient: +0.311) [Table 2]. Positive correlation was observed with staff interaction and patient information (Spearman coefficient: +0.362). However, no correlation was observed between elements and wards.
Table 2.
Correlation between various variables and categories
Discussion
Nursing shift handovers are essential, not only for maintaining the continuity and quality of care but also are important in planning.[8,9]
This study of nursing handover practices at the Neurosciences Center was conducted with the knowledge that nursing handover at the center had evolved on a need-based manner over a prolonged period. However, a validated tool provided an opportunity to assess the gaps in a system with unstructured handovers.
Studies indicate the importance of duration and specific time for handovers.[10] Yet, significant deficiencies were found, especially during the morning shifts and weekends. The findings collaborate with those of other studies. Sexton et al. (2004) observed 23 handovers by time of the day in one general medical ward. Handovers frequency was 3 times/24 h (07:00 am, 14:30 pm, 22:45 pm). At 07:00 am there were observed seven handovers, with a mean length of 18 min and their range between 15 and 22 min. However, the other handovers (afternoon and night) had more mean length (39 and 33 min respectively).[11] The low morning compliance probably reflects the delay in arrival of the morning shift oncoming practitioner, busy morning duty corresponding with doctors rounds, and nurse fatigue factor due to night duty. The weekend fall of compliance may be a result of lack of supervision (absence of administrative nurses) and generalized fall in diligence observed in other studies as well. That there was no variation between other shifts, and the trend was similar between wards, point to a more systemic deficiency rather than factors such as specialty-specific or individual variations.
Besides the all important bedside handovers, several researchers have also identified the nursing station as an appropriate location of handovers, to avoid disturbance or interruption, but suggest caution in changing from office based to bedside handover.[12] Bedside handover has been known to facilitate a partnership model in medication communication bring nursing team, together, promoting medication review, providing a patient centered dimension of handovers, with an additional advantage of patients providing key essential information, and an opportunity to participate actively in the process of their treatment.[13,14] Our study revealed that bedside handovers were paradoxically more frequent during weekends and night shifts. Interestingly, bedside handovers had a negative correlation with the duration of handover this may be the reason for a subconscious nursing adaptation by nurses to save time on weekends and night shifts. This also validates the findings of other studies, which suggest that bedside handover takes less time. Bradley and Mott 2012 observed that in exclusive nursing station handovers, the mean total time taken was 0.44 h and after the implementation of bedside handovers, it was 0.22 h. No shift wise or ward wise variation was seen.[15]
Several authors have studied the content of hand over. The findings of a qualitative case study in two hospitals indicate that SBAR may aid in schema development that allows rapid decision making by nurses, provide social capital and legitimacy for less tenured nurses, and reinforce a move toward standardization in the nursing profession.[4] A prospective interventional study reveals that SBAR improves communication and safety climate and decreases incident reports due to communication errors.[16] However, our study revealed that although process based elements had an overall better compliance, nurses had a greater propensity to explain the situation and the recommendation and much less about the background and their own assessment of the patient, relying more or records. This ritualized handover has been studied to be ineffective and a discourse of anxiety among nurses.[17] Authors have given various modification to support flexible adaptation such as the standardized protocols identify–situation–observations–background–agreed plan–read back (iSoBAR), or more recently the “HAND ME AN ISOBAR.”[18,19] No localized modification was observed in any of the handovers in our study.
Importantly, there was no statistically significant difference between wards. This probably reveals the understanding among the nursing staff of the SBAR being the core of the handover process, and thus greater diligence regarding the same may have been habituated. However, a weak negative correlation between weekend shift and SBAR continues to point toward the possibility of the weekend effect. Detail analysis of the content was beyond the scope of the study.
The importance of nursing personnel interaction is especially read back is emphasized by World Health Organization.[20] However, this study revealed a poor level of compliance with read backs (52.8%) though a positive relationship exists between night shifts and staff interaction. Further, handovers were formulaic, partial, cryptic, given at high speed, used abbreviations, and jargon. This has been observed in others studies, which suggest that nursing interaction often required socialized knowledge to interpret.[21]
An interesting finding was that the staff interaction was significantly higher among the neurosurgery staff than among the neurology staff. It is unclear whether it is an adaptive response to the nature of the specialty itself, or a result of better administrative leadership in the neurosurgery. Nevertheless, it brings out the importance of leadership in the implementation of better handover practices, as enumerated in several studies.[22]
The patient and family are the only constant and are thus in a position to play a critical role in ensuring continuity of care.[23,24] Engaging patients is sometimes made more difficult due to low health literacy.[25] This is especially true in the Indian context where healthcare workers have a paternalistic view of patients and inequalities in levels of empowerment and opportunity affect medical decision making.[26] Our study reflected the least compliance with patient communication during handovers. Encouragingly though, greater staff interaction was found to be directly related to better patient communication. Surprisingly, observation of weekend shift revealed greater nurse-patient interaction, a possible outcome of a less hectic schedule, fewer transfers, non-outpatient department days and fewer surgeries. A study of neurosurgery residents concludes that there needs to be more focused education devoted to learning effective patient care handoffs in neurosurgical training programs.[27] The same may be extrapolated to nurses as well.
The study had certain limitation including that of Hawthorne effect on the nursing staff performing handovers in the presence of the author. Further, the role of content of handover and patients and family members was not included in the study. Moreover, the large influence of extraneous factors, such as the type of clinical environment, experience, culture of leadership, specialty, case mix, technology, and local policies, cannot be underestimated.
Conclusion
This study was undertaken to assess the nursing handover practices in an apex Neurosciences Center in India. Relatively inferior weekend and morning shift handover practices across all wards, in all categories, except bedside handovers and patient communications, calls for a systems approach, and greater administrative commitment. Decreased interaction among nurses and poor communication with patients, needs to be addressed. Since the two showed a direct relation with bedside handovers, promoting the latter is likely to result in overall improvement. Better performance regarding process elements across the spectrum is encouraging. However, nurses continued to lay less emphasis on handing over their own assessment and recommendation to the incumbent, further emphasizing the need for standardized handovers.
While this contextual study revealed an urgent need for the administration to undertake a system-based approach for a standardized handover protocol, the use of technology such as electronic handovers, role of leadership, and training cannot be overemphasized.[28] Future studies need to focus on the postinterventional analysis, content of handovers, perception of nursing staff, and the role of leadership in handovers. This will assist in continuity of care, promote patient safety, and ensure better outcomes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lamond D. The information content of the nurse change of shift report: A comparative study. J Adv Nurs. 2000;31:794–804. doi: 10.1046/j.1365-2648.2000.01349.x. [DOI] [PubMed] [Google Scholar]
- 2.Commission on Safety and Quality in Health Care – Clinical Handover. ACSQHC. 2012. [Last accessed on 2013 Dec 18]. Available from: http://www.safetyandquality.gov.au/our-work/clinical-communications/clinical-handover .
- 3.Oakbrook, IL: Joint Commission; 2006. [Last accessed on 2013 Sep 12]. Root Causes of Sentinel Events, All Categories. Available from: http://www.jointcommission.org/NR/rdonlyres/FA465646-5F5F-4543-AC8F-E8AF6571E372/0/root_cause_se.jpg . [Google Scholar]
- 4.Vardaman JM, Cornell P, Gondo MB, Amis JM, Townsend-Gervis M, Thetford C. Beyond communication: The role of standardized protocols in a changing health care environment. Health Care Manage Rev. 2012;37:88–97. doi: 10.1097/HMR.0b013e31821fa503. [DOI] [PubMed] [Google Scholar]
- 5.Chiò A, Montuschi A, Cammarosano S, De Mercanti S, Cavallo E, Ilardi A, et al. ALS patients and caregivers communication preferences and information seeking behaviour. Eur J Neurol. 2008;15:55–60. doi: 10.1111/j.1468-1331.2007.02000.x. [DOI] [PubMed] [Google Scholar]
- 6.Implementation Toolkit: Standard Key Principles for Clinical Handover. [Last accessed on 2013 Nov 26]. Available from: http://www.archi.net.au/documents/resources/qs/clinical/clinical-handover/implementation-toolkit.pdf .
- 7.Safe Handover: Safe Patients’ Guideline by the United Kingdom National Patient Safety Agency. 2004. [Last accessed on 2013 Dec 12]. Available from: http://www.bma.org.uk/media/files/pdfs/practical%20advice%20at%20work/contracts/safe%20 handover%20safe%20 patients.pdf .
- 8.Philpin S. Handing over: Transmission of information between nurses in an intensive therapy unit. Nurs Crit Care. 2006;11:86–93. doi: 10.1111/j.1362-1017.2006.00157.x. [DOI] [PubMed] [Google Scholar]
- 9.Liukkonen A. The content of nurses’ oral shift reports in homes for elderly people. J Adv Nurs. 1993;18:1095–100. doi: 10.1046/j.1365-2648.1993.18071095.x. [DOI] [PubMed] [Google Scholar]
- 10.Randell R, Wilson S, Woodward P. The importance of the verbal shift handover report: A multi-site case study. Int J Med Inform. 2011;80:803–12. doi: 10.1016/j.ijmedinf.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Sexton A, Chan C, Elliott M, Stuart J, Jayasuriya R, Crookes P. Nursing handovers: Do we really need them? J Nurs Manag. 2004;12:37–42. doi: 10.1111/j.1365-2834.2004.00415.x. [DOI] [PubMed] [Google Scholar]
- 12.McMurray A, Chaboyer W, Wallis M, Fetherston C. Implementing bedside handover: Strategies for change management. J Clin Nurs. 2010;19:2580–9. doi: 10.1111/j.1365-2702.2009.03033.x. [DOI] [PubMed] [Google Scholar]
- 13.Liu W, Manias E, Gerdtz M. Medication communication between nurses and patients during nursing handovers on medical wards: A critical ethnographic study. Int J Nurs Stud. 2012;49:941–52. doi: 10.1016/j.ijnurstu.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Chaboyer W, McMurray A, Johnson J, Hardy L, Wallis M, Sylvia Chu FY. Bedside handover: Quality improvement strategy to transform care at the bedside. J Nurs Care Qual. 2009;24:136–42. doi: 10.1097/01.NCQ.0000347450.90676.d9. [DOI] [PubMed] [Google Scholar]
- 15.Bradley S, Mott S. Handover: Faster and safer? Aust J Adv Nurs. 2012;30:23–32. [Google Scholar]
- 16.Randmaa M, Mårtensson G, Leo Swenne C, Engström M. SBAR improves communication and safety climate and decreases incident reports due to communication errors in an anaesthetic clinic: A prospective intervention study. BMJ Open. 2014;41:E004268. doi: 10.1136/bmjopen-2013-004268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evans AM, Pereira DA, Parker JM. Discourses of anxiety in nursing practice: A psychoanalytic case study of the change-of-shift handover ritual. Nurs Inq. 2008;15:40–8. doi: 10.1111/j.1440-1800.2008.00387.x. [DOI] [PubMed] [Google Scholar]
- 18.Porteous JM, Stewart-Wynne EG, Connolly M, Crommelin PF. iSoBAR – A concept and handover checklist: The National Clinical Handover Initiative. Med J Aust. 2009;190:S152–6. doi: 10.5694/j.1326-5377.2009.tb02625.x. [DOI] [PubMed] [Google Scholar]
- 19.Yee KC, Wong MC, Turner P. HAND ME AN ISOBAR: A pilot study of an evidence-based approach to improving shift-to-shift clinical handover. Med J Aust. 2009;190:S121–4. doi: 10.5694/j.1326-5377.2009.tb02617.x. [DOI] [PubMed] [Google Scholar]
- 20.WHO Collaborating Center International Steering Committee. 11-12, June 2006, Meeting. Also London Declaration, Patients for Patient Safety, WHO World Alliance for Patient Safety, 29 March. 2006. [Last accessed on 2014 Dec 24]. Available from: http://www.who.int/patientsafety/information_center/London_Declaration_May06.pdf .
- 21.Payne S, Hardey M, Coleman P. Interactions between nurses during handovers in elderly care. J Adv Nurs. 2000;32:277–85. doi: 10.1046/j.1365-2648.2000.01474.x. [DOI] [PubMed] [Google Scholar]
- 22.Meissner A, Hasselhorn HM, Estryn-Behar M, Nézet O, Pokorski J, Gould D. Nurses’ perception of shift handovers in Europe: Results from the European Nurses’ Early Exit Study. J Adv Nurs. 2007;57:535–42. doi: 10.1111/j.1365-2648.2006.04144.x. [DOI] [PubMed] [Google Scholar]
- 23.Cahill J. Patient's perceptions of bedside handovers. J Clin Nurs. 1998;7:351–9. doi: 10.1046/j.1365-2702.1998.00149.x. [DOI] [PubMed] [Google Scholar]
- 24.Whale Z. The participation of hospital nurses in the multidisciplinary ward round on a cancer-therapy ward. J Clin Nurs. 2004;2:155–63. [Google Scholar]
- 25.Chicago: American Medical Association; [Last accessed on 2014 Jan 11]. The ABCs of Health Literacy. Chicago, American Medical Association. Available from: http://www.ama-assnorg/ama1/pub/upload/mm/15/health_ literacy.doc . [Google Scholar]
- 26.Seetharam S, Zanotti R. Patients’ perceptions on healthcare decision making in rural India: A qualitative study and ethical analysis. J Clin Ethics. 2009;20:150–7. [PubMed] [Google Scholar]
- 27.Babu MA, Nahed BV, Heary RF. Investigating the scope of resident patient care handoffs within neurosurgery. PLoS One. 2012;7:e41810. doi: 10.1371/journal.pone.0041810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Govier M, Medcalf P. Living for the weekend: Electronic documentation improves patient handover. Clin Med. 2012;12:124–7. doi: 10.7861/clinmedicine.12-2-124. [DOI] [PMC free article] [PubMed] [Google Scholar]


