Summary
In 2012 Quebec limited continuous in-hospital duty to 16 consecutive hours for all residents regardless of postgraduate (PGY) level. The new restrictions in Quebec appeared to have a profound, negative effect on the quality of life of surgical residents at McGill University and a perceived detrimental effect on the delivery of surgical education and patient care. Here we discuss the results of a nationwide survey that we created and distributed to general surgery residents across Canada to capture and compare their perceptions of the changes to duty hour restrictions.
In 2012 Quebec limited continuous in-hospital duty to 16 consecutive hours for all residents regardless of postgraduate (PGY) level.1 The new regulations were different from rules in the United States, which limited 24-hour duty only in the PGY-1 year, and in the rest of Canada.1 The new restrictions in Quebec appeared to have a profound, negative effect on the quality of life of surgical residents at McGill University and a perceived detrimental effect on the delivery of surgical education and patient care.1
We administered a nationwide survey to capture and compare the perception of general surgery residents about the changes to duty hour restrictions. We expected that Quebec residents working under the current restricted duty hour model would report less satisfaction with their quality of life and education than their counterparts in other provinces.
Survey
We developed our survey based on scales measuring quality of life and sleep, perception of future competency, satisfaction with education and relationship with attending surgeons, and perception of ability to provide safe patient care. The survey included parts of the World Health Organization’s WHOQOL-BREF for quality of life, the Pittsburgh Sleep Quality Index, and a previously published survey to assess education and patient care issues.1 The survey (Appendix 1, available at canjsurg.ca) was distributed to general surgery residents across Canada via the online tool SurveyMonkey. Participants completed the survey anonymously, selecting their level of agreement with various statements using a 5-point Likert scale, between January and March 2013.
In Canada, general surgery residency is a 5-year postgraduate program leading to Royal College certification. Each of the 17 programs accept 3–14 residents per year. The sex distribution of residents in these programs is 55% male and 45% female. The average age of residents in Quebec who responded to our survey was 23.6 ± 6.2 years, compared with 28.2 ± 8.2 years nationally. The response rate in Quebec was 37%, compared with 17.6% nationally (Table 1).
Table 1.
Characteristics of survey respondents
| Characteristic | Group; no. (%)* | p value | |
|---|---|---|---|
| Quebec (n = 61)† | Rest of Canada (n = 122)‡ | ||
| Age, yr, mean ± SD | 23.6 ± 6.2 | 28.2 ± 8.2 | < 0.001 |
| PGY level | — | — | — |
| PGY-1 | 15 (24.9%) | 32 (26.2%) | — |
| PGY–2 | 17 (27.5%) | 23 (18.9%) | — |
| PGY–3 | 11 (17.7%) | 33 (27.1%) | — |
| PGY–4 | 7 (11.3%) | 17 (13.9%) | — |
| PGY–5 | 8 (12.9%) | 17 (13.9%) | — |
| PGY–6 | 3 (5.7%) | — | — |
| Plan to pursue fellowship training | 53 (87.6%) | 76 (62.3%) | — |
PGY = postgraduate year; SD = standard deviation.
Unless indicated otherwise.
Restricted duty hour model (12-hour shifts at McGill University and night float at the other Quebec universities).
24-hour duty model.
How do residents in Quebec compared with those in the rest of Canada feel about the duty hour model?
In Quebec 13.1% of residents felt that they knew their patients well compared with 80.3% of national respondents. Quebec residents felt less able than residents in other provinces to diagnose and manage their patients effectively (11.9% v. 77.9%).
Quebec residents reported an average of 5.5 ± 1.3 hours of sleep every night compared with an average of 6.5 ± 1.9 hours for residents in other provinces. The weekly sleep average for both Quebec residents and national residents was about 42 hours. The majority (89.6%) of Quebec residents felt sleep-deprived, compared with just over half (53.2%) of residents from other provinces.
Morale differed between residents in Quebec and those in the rest of Canada despite them having similar overall weekly duty hours (71.8 ± 16.7 hours in Quebec v. 75.9 ± 22.3 hours nationally). Only 19.6% of residents working under the limited duty hours felt that morale was good in the program compared with 51.6% of residents nationally.
There were differences in residents’ perceptions of their ability to provide safe and continuous care to patients. Only 16.3% of Quebec respondents (compared with 59.8% of respondents in the rest of Canada) felt that they would be able to master the necessary surgical skills needed for practice.
A more detailed breakdown of the residents’ responses (Quebec v. rest of Canada) are available in Appendix 1, Tables S1–S4. To control for the differences inherent to each program in Quebec as well as the different duty hour models at McGill University compared with the other 3 general surgery residency programs in Quebec, we conducted a subgroup analysis by program in Quebec (Fig. 1, Fig. 2 and Appendix 1).
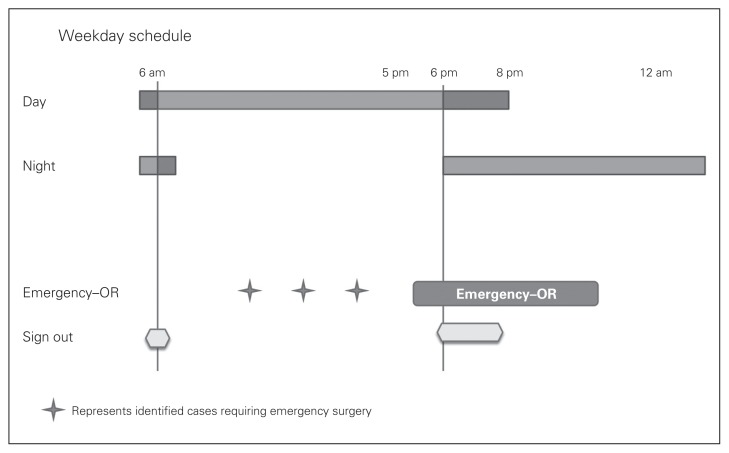
Fig. 1.
The current duty hour model used at McGill University, Montreal, Que., consists of 2 12-hour shifts — a daytime shift from 6 am to 6 pm and a night shift from 6 pm to 6 am. Owing to emergency surgeries and sign-outs it is difficult to work efficiently within these limits, and there is often overlap of the day team and night team. OR = operating room.
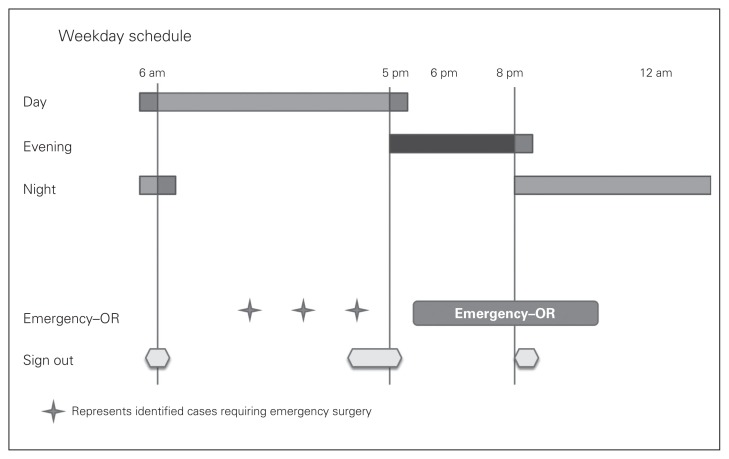
Fig. 2.
The duty model used at Université de Montréal, Université Laval and Université de Sherbrooke require a resident from the daytime to take a longer shift until 8 pm. During the period from 5 pm to 8 pm, this resident covers all surgical services and then signs out all services to another person covering the night shift. There are 3 sign-out periods in this system. Owing to this setup the resident covering the evening shift cannot attend any emergency surgeries. The medium-grey bars represent necessary overlap otherwise unaccounted for. On the weekend all programs revert to a 12-hour shift model like the one used at McGill University. OR = operating room.
What should educators take away from our survey results?
Quebec is the first jurisdiction in North America to implement very restrictive duty hour limits without examining the possible effects on surgical training.1 Compared with residents in the rest of Canada, those in Quebec report a decreased quality of life and a decreased sense of ownership of patients in their care. The results of our national survey reveal that the protection of residents and patients is an issue that is not simply addressed by mandating reduced duty hours in a “one size fits all” approach.2
Most surgical programs in Canada still function within the framework of an apprenticeship model, where experiential learning is central to skill acquisition and the development of competent and safe surgeons.2,3 The Quebec ruling effectively equates the training needs — procedural or not — of all specialties. Unlike in specialties such as emergency medicine, where duty hour restrictions exist and are necessary,4 residents in general surgery are not in a perpetual state of concentration or subjected to assessing a constant stream of patients during call.
Programs across Quebec have started to think of unique ways to ensure quality of life beyond duty hours. These include hiring physician extenders, protected nap times, mindfulness meditation programs, and an application to the medical union in Quebec to give general surgery residents an exemption to allow overnight call that lasts 16 hours instead of 12 hours.1,2
Quantifying medical errors or actual operating case volumes was beyond the scope of our survey, and we were not able to control for several confounders, including number of residents in each program and pressures to provide coverage; weather conditions; nature of patients and services in each program; resident salary, noting that this is lower in Quebec; and number of fellows or physician extenders. Despite these confounders and the low response rate from residents outside Quebec, it is increasingly apparent that the problems posed by the new duty hour restrictions go beyond the number of hours worked or spent in the hospital. Studies to measure objective patient outcomes under the new duty hour restrictions are needed. Without other significant changes to the system, we have only added additional pressure to our trainees, expecting them to perform the same amount of work in less time.1,2,5
Footnotes
Competing interests: None declared.
Contributors: All authors contributed substantially to the conception, writing and revision of this commentary and approved the final version for publication.
References
- 1.Hamadani FT, Deckelbaum D, Sauvé A, et al. Abolishment of 24-hour continuous medical call duty in Quebec: a quality of life survey of general surgical residents following implementation of the new work-hour restrictions. J Surg Educ. 2013;70:296–303. doi: 10.1016/j.jsurg.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed N, Devitt KS, Keshet I, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. 2014;259:1041–53. doi: 10.1097/SLA.0000000000000595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jamal MH, Rousseau MC, Hanna WC, et al. Effect of the ACGME duty hours restrictions on surgical residents and faculty: a systematic review. Acad Med. 2011;86:34–42. doi: 10.1097/ACM.0b013e3181ffb264. [DOI] [PubMed] [Google Scholar]
- 4.Collins JP. International consensus statement on surgical education and training in an era of reduced working hours. Surgeon. 2011;9(Suppl 1):S3–5. doi: 10.1016/j.surge.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 5.Aminazadeh N, Farrokhyar F, Naeeni A, et al. Is Canadian surgical esidency training stressful? Can J Surg. 2012;55:S145–51. doi: 10.1503/cjs.002911. [DOI] [PMC free article] [PubMed] [Google Scholar]