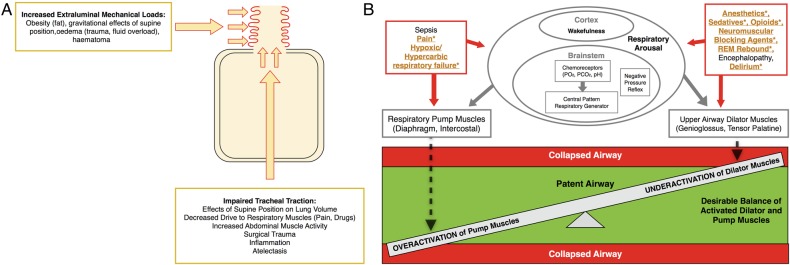
Figure 1.
Pathophysiology of perioperative obstructive sleep apnoea. (A) Pathological anatomy. This schematic of the respiratory system demonstrates the anatomical forces (red arrows) increasing collapsibility of the upper airway (red curly lines). Caudal tracheal traction stabilises the upper airway such that it is less vulnerable to collapse. CPAP treatment can evoke caudal tracheal traction and increase end-expiratory lung volume. Collapsing physical forces are those that increase the mechanical load on the upper airway (haematoma, oedema, fat) and those that reduce caudal tracheal traction (atelectasis, supine, flat position). (B) Pathological physiology. The vulnerable perioperative upper airway physiology is illustrated as a scale, demonstrating the fragile balance between activation of respiratory pump muscles and upper airway dilator muscles (green zone). When activated, pump muscles generate negative inspiratory pressure and tip the balance to upper airway collapse (red zone). In normal physiology, upper airway dilator muscles activate to counterbalance the negative inspiratory pressure and dilate the upper airway. Underactivation of airway dilator muscles, such as the tongue muscle, will result in collapse (red zone). A variety of perioperative events affect respiratory arousal, which can impair airway patency by overactivating pump or underactivating dilator muscles, respectively. Patients with OSA are at higher vulnerability towards collapse, and the specific pathophysiological mechanism of the increased perioperative vulnerability to collapse in OSA are emphasised in yellow colour and denoted with an asterisk. CPAP, continuous positive airway pressure; OSA, obstructive sleep apnoea.