Abstract
Background:
Most medical errors are preventable. The aim of this study was to compare the current execution of the 3 patient safety solutions with WHO suggested actions and standards.
Methods:
Data collection forms and direct observation were used to determine the status of implementation of existing protocols, resources, and tools.
Results:
In the field of patient hand-over, there was no standardized approach. In the field of the performance of correct procedure at the correct body site, there were no safety checklists, guideline, and educational content for informing the patients and their families about the procedure. In the field of hand hygiene (HH), although availability of necessary resources was acceptable, availability of promotional HH posters and reminders was substandard.
Conclusions:
There are some limitations of resources, protocols, and standard checklists in all three areas. We designed some tools that will help both wards to improve patient safety by the implementation of adapted WHO suggested actions.
Keywords: Hand hygiene, patient hand-over, patient safety, procedure errors
INTRODUCTION
Patient safety is an issue of global concern and it focuses on reducing medical errors.[1] Most medical errors that lead to serious injuries or death of a patient are preventable, but most of them transpire due to complexity of the healthcare system not because of individual errors.[2] A result of a study shows that the occurrence of unwanted events in hospitals was 11.1% for every 100 patients, from which 53.2% of these events were avoidable.[3] Based on a study in New York, 98,000 American patients lose their lives annually due to medical errors.[4] According to “The National Academy of Sciences Institute of Medicine,” the cost of preventable medical errors is estimated to be between 17 and 29 billion dollars annually.[5] Based on our research regarding this situation in Iran, we did not find suitable data pertaining to medical errors and its costs. However, a study conducted at a Pediatric Hospital in Khorramabad, showed that the frequency of medical errors was estimated to be 36%.[6] Due to the possibility of high medical error rates in Iranian hospitals, as well as insufficient data for patient safety, we decided to assess the present situations based on some patient safety standards. Since WHO has suggested nine solutions for reducing medical errors, a decision was made to assess the status of three of the nine patient safety solutions of WHO in 2 Intensive Care Unit (ICU) wards in Nemazi Hospital. Our three solutions were prioritized based on request and concern of each ward manager. We chose the ICU as our study environment because there is a higher possibility of medical errors as a result of prolonged hospitalization and different instruments used on the patients. The three safety solutions are as the following:
Communication during patient hand-overs
Communication problems were reported to be responsible for 11% of adverse events in Australian hospitals.[7] Poor communication between professional caregivers is also one of the most important contributory factors of adverse events in NHS hospital practices.[8] There is also a possibility of inaccurate or incomplete transfer of patient's information due to the lack of proper communication between healthcare providers. Therefore, an effective patient hand-over is the key element for improving patient safety. Different rules and regulations are recommended by professional organizations to ensure that patient hand-over will be performed in a proper way.[9,10,11,12,13] In a qualitative study conducted in the USA, the situation, background, assessment, and recommendation (SBAR) technique was found to be an appropriate and cost-effective tool for patient hand-over and improving patient safety.[14] The results of a study conducted by the Mashhad University of Medical Sciences in Iran revealed that implementing standardized shift hand-over protocols and techniques improved intershift information communication.[15]
Correct procedure at the correct body site
The rate of adverse events for surgical admissions is high, and it depends on many factors such as the type of procedure, age, etc.[16] The main cause of wrong-site procedure errors is a lack of standardized preoperative process that includes reviewing the patient's information.[17] A literature review and many other studies showed that surgical safety checklists are effective in reducing wrong-site surgery incidences and other medical errors.[18,19,20,21,22] A study conducted by the Shiraz University of Medical Sciences “(SUMS)” in Iran found that implementing safe surgery checklists decreased mortality and morbidity after procedures.[23] Some key strategies are provided for the proper use of these checklists.[24]
Promotion of hand hygiene
In American hospitals, Health care-associated Infections (HAIs) account for an estimated 1.7 million infections and 99,000 associated deaths each year.[25] According to the result of a systematic review and meta-analysis, pooled overall HAIs density in adult ICUs was 47.9/1000 patient days.[26] The risk of HAIs in developing countries is 2–20 times higher than in developed countries because of a larger number of risk factors associated with poor adherence to hand hygiene (HH) among health care workers.[27] Several guidelines and policies for the improvement of HH have been developed.[28,29] An interventional study in Africa that incorporated WHO HH improvement strategies displayed a significant advancement for the patient safety in the developing countries.[30] Many studies have been conducted in the field of HH in Iran, indicating that staff knowledge and compliance were very poor in HH. Therefore, providing staff with educational and training programs is necessary to reduce infection rates.[31,32,33]
The aim of this study was to investigate the infrastructures of resources, polices, and protocols in order to compare the current execution of the 3 patients safety solutions (communication during patient hand-over, correct procedure at the correct body site, improved HH) with WHO suggested actions and standards. The second aim of this study was to recognize the inadequacy and insufficiency of our tools so that we can design better tools for patient safety improvement by considering culture and current routine standards affiliated to our study setting.
METHODS
In our cross-sectional study, we invited 45 nurses and 15 physicians who worked in two ICUs of Nemazi Hospital for the past 12 months. Nemazi Hospital is the largest teaching hospital in the Southern Iran, affiliated to “SUMS.” One ICU had 14 beds and the second ICU had 10 beds, both of which admitted medical and surgical patients. This study was approved by the ethics committee of “SUMS” and was conducted from September 2013 to January 2014 in three phases:
Phase 1: Designing data collection forms
In order to design the three data collection forms, we used WHO actions.[9,17] We formed survey questions from WHO suggested actions, and some modifications were made due to the study setting's culture. We also used some of the questions from WHO HH framework survey due to existing conditions in our setting.[34] The data collection form consisted of demographic data, information on facilities, resources, basic organizational structures, and protocols which are available in the wards [Annexure 3, 4, 5]. The questions in the data collection form were assessed by a team of health care staff experts working within the wards, senior nurses, professors, and project partners to test its validity and relevance. The primary forms were given to 20% of the study population. Ten nurses and doctors piloted all three data collection forms after providing verbal consent. The pilot group members were asked if the questions in the survey forms were comprehensive. According to their opinions, minor changes were made to some of the questions. Moreover, the validity of the data collection forms was verified, and the final forms were created.
Phase 2: Baseline evaluation survey
The final data collection forms were distributed between the ICU ward staff members. After they provided verbal consent, they were asked to fill out the forms and return them within 2 weeks. In addition, unannounced systematic inspections of each clinical care area were performed every 2 weeks. 6 visits were made per ICU: Two morning visits, two evening visits, and two night visits. Data collection forms (as our observational checklist) were completed again by one of the authors (Sh. B) during the observation of the available documentation, resources, and opportunities in both wards. The results of the observations and the staffs’ reports identified any problems and shortcomings in the execution of the solutions. In order to make the results more tangible, we decided to change the responses of the participants from always to (optimal), often or sometimes to (acceptable) and rarely or never to (substandard) respectively.
Phase 3: Providing tools (protocols, checklists, posters, etc.)
After determining the key limitations and shortcomings from the analyzed data, we decided to design some tools to resolve them. By reviewing our results, the existing guidelines and protocols for each of the three issues in both wards, cultural perceptions, beliefs, and practices, we prepared new protocols and checklists for safe patient hand-overs and procedures. These protocols contain the necessary items that need to be communicated during patient hand-over and necessary items that need to be checked before and after invasive procedures.
For promoting HH and preventing HAIs, we provided the WHO recommended tools, which were not available previous to this study. For example, promotional HH reminders and posters were set in the workplace and alcohol-based hand rub bottles were attached to all beds, etc.[31] The content of protocols and checklists were assessed by heads of the wards, informed health care workers working within the wards, senior nurses, professors, and project partners to test for face validity and relevance.
Data analysis was performed by using SPSS statistical software version 21 (Chicago, IL, USA). We used descriptive analysis such as percentages, means, and standard deviations. We also calculated the coefficient of variation in each area, in order to check the agreement between observer and respondents.
RESULTS
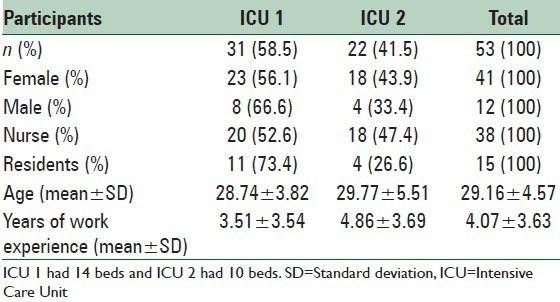
All 60 members were asked to complete the survey forms, but only 56 out of 60 individuals (93%) completed the forms. Participation in the survey was random and did not associate with a specific factor. None of the participants were more similar to each other. Three out of the 56 forms were excluded from evaluation since they were not completed. Demographic information of the participants is addressed in Table 1.
Table 1.
Demographic information of participants
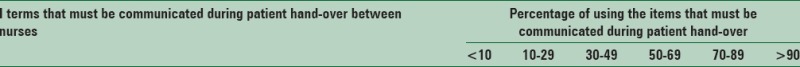
Communication during patient hand-over
The time spent for each patient hand-over between shift changes was reported to be <5 min in 13.9% (n = 5) of nurses and 26.7% (n = 4) of doctors, between 5 and 10 min in 66.7% (n = 24) of nurses and 60% (n = 9) of doctors and more than 10 min in 19.4% (n = 7) of nurses and 13.3% (n = 2) of doctors. According to our observations, hand-over time between shifts for each patient lasted, on average, 3 ± 1.2 min for nurses and 4 ± 1.5 min for doctors, respectively. Implementation of policies’ status, the availability of resources, and basic organizational structures for implementing “Communication during patient hand-over” solution is summarized in Table 2.
Table 2.
Implementation status of policies, the availability of resources and basic organizational structures in the ward according to nurses’ (N) and doctors’ (D) opinion
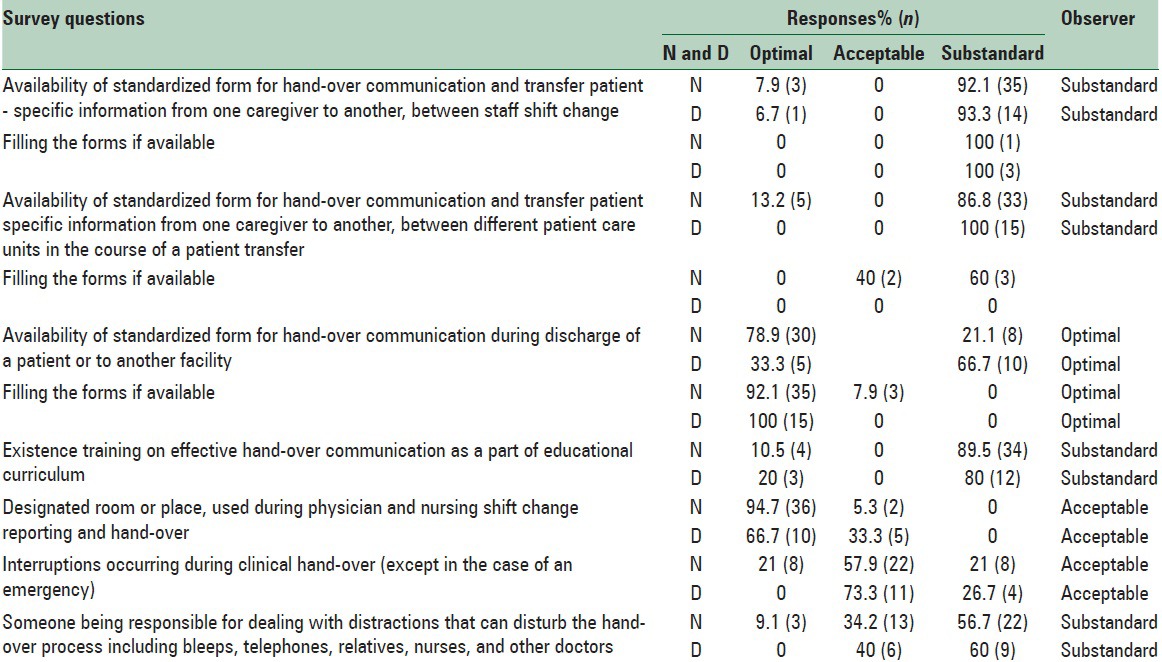
However, we did not observe any data collection form for hand-over communication between staff when changing shifts or between different patient care units in the course of a patient transfer. Hence, there was an imperfect form for hand-over communication during discharge of a patient or transfer to another facility. Hand-over was usually performed at the bedside by nurses and doctors, but access to radiology and pathology results was possible only at the nursing station.
Our study shows none of the items in the time of hand-over between caregivers were completed by nurses or doctors. There was also not a single case where information was transferred completely. However, most of the important information such as patient identification, primary and secondary diagnoses, changes in patient condition, patient condition assessment, plans, concerns, and recommendations were transferred by caregivers half of the time. Coefficient of variation in this area was 4.64% (<5%), so the agreement between observer and respondents was good and acceptable.
Performance of correct procedure at correct body site
Implementation status of policies, availability of resources, and basic organizational structures for implementation of “Performance of correct procedure at correct body site” solution is summarized in Table 3. According to our observation, there was no guideline or educational content for informing the patients and their families about procedure rationale, plans, options, and risks in both wards. However, 9.4% of the staff reported the presence of such forms. It is worth mentioning that there were some discrepancies between observations and reports, which is discussed later.
Table 3.
Implementation status of policies and availability of resources and basic organizational structures in the wards
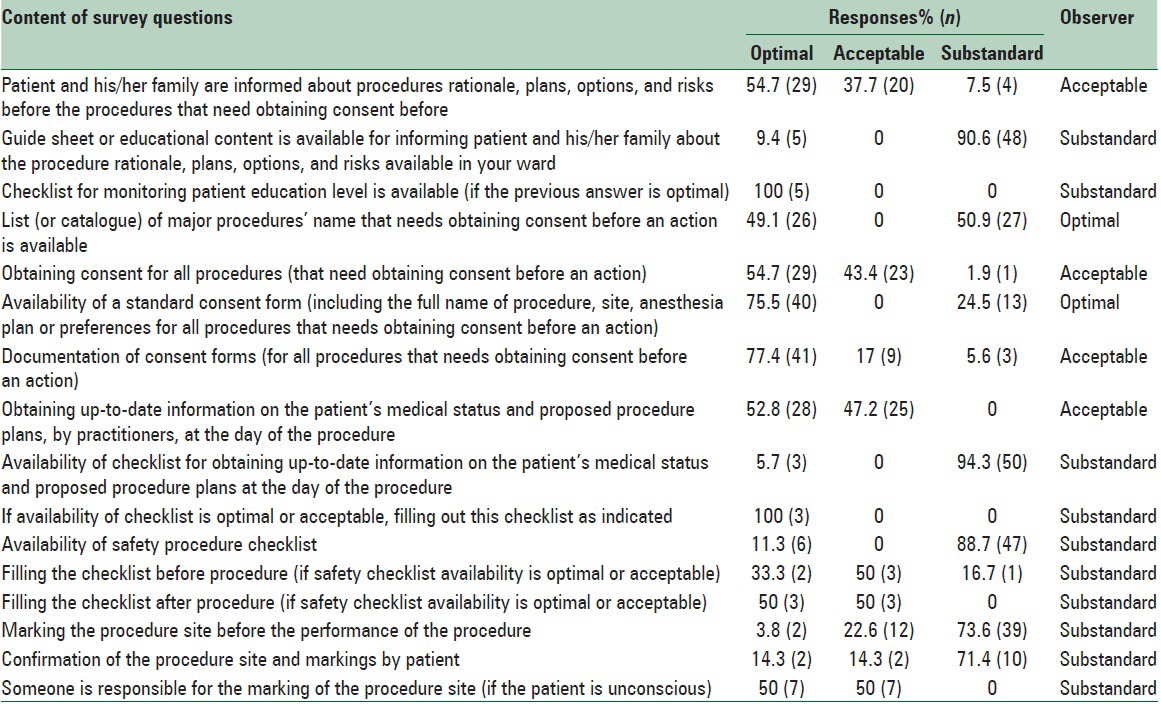
The investigator observed a list of major procedures that required obtaining consent forms before the specific procedure was performed in the wards. The majority of the staff reported that they verbally obtain the consent for the required procedures, as well as information about patient's medical status and procedure plans. Thus, in most cases they did not fill out any checklist. The investigator also realized that there was no checklist available in both wards to ensure performance of safe procedures. Coefficient of variation in this area was 3.78% (<5%), so the agreement between observer and respondents was good and acceptable.
Hand hygiene
Implementation status of policies, availability of resources, and basic organizational structures for implementing “Hand hygiene” solution is summarized in Table 4. According to our observations, foot operated taps were available in all points of care, as well as hand rub wall dispensers. On the other hand, few members of the staff (5.7%) reported the usage of hand-operated taps in both wards because staffs used hand-operated taps in their resting rooms. As for the types of hand rub dispensers that are available in the ward, all 53 staff reported the use of wall dispensers, but no one reported the availability of other types of hand rub dispensers such as pocket bottles, bottles affixed to trolleys/trays, bottles attached to beds, and dispensers located on the bedside of tables/trolleys. Thirty members of staff (56.6%) reported the availability of wall dispensers at the point of care, and the remaining percentage (43.4%) reported the availability of the wall dispensers but not at each point of care. About 69.2% of the staff did not know how frequently the audits on HH compliance were performed in the ward, 17.9% reported that it was performed at least once a year, 2.6% stated that it was done at least once every 2 years, and 10.3% said it was performed rarely.
Table 4.
Implementation status of policies and availability of resources and basic organizational structures in the wards for HH
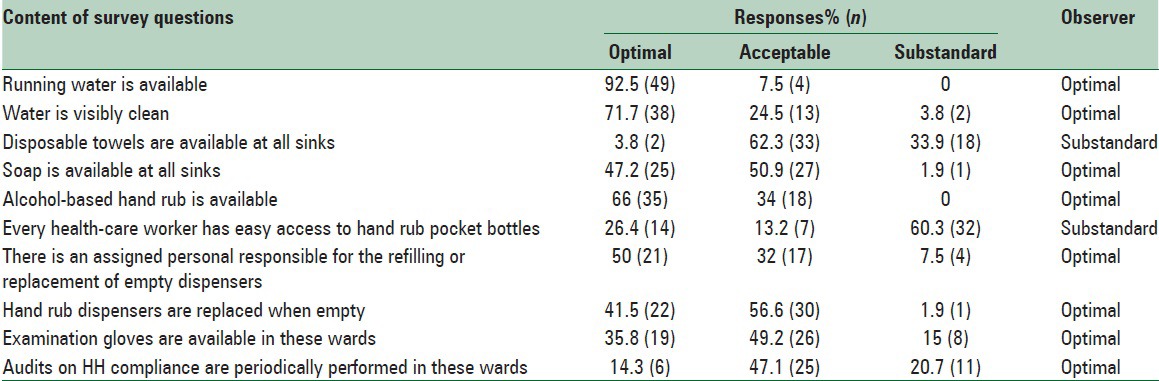
According to our observations, posters illustrating hand wash and hand rub techniques were not displayed beside all the sinks, close to dispensers or in multiple areas of both wards. However, posters illustrating indications for HH were displayed in multiple areas of both wards thus; no other type of reminders was available in these wards. All the staff reported that running water and alcohol-based hand rubs were always or often available, and 96.2% of the staff reported that water was always or often visibly clean. 88.7% of the staff reported that hand rub dispensers were always or often replaced when empty, and 84.9% of them stated that examination gloves were always or often available in these wards. Coefficient of variation in this area was 5.8% (<5%), so the agreement between observer and respondents was almost acceptable.
DISCUSSION
As previously mentioned, most medical errors that result in death or serious injuries to patients can be prevented. As our baseline surveys showed, there were some limitations, such as resources, tools, and protocols, for implementing WHO solutions in both wards. Therefore, we made a decision to develop some tools (checklists, reminders, and posters) and protocols for successful implementation of WHO suggested actions in each area.
Communication during patient hand-over
Standardized approach to hand-over communication is required in order to minimize the risk of adverse events due to lost information, misinterpretation, and missed actions.[9,10,11,12,13] An interventional study showed that safety environment improved significantly over time in an intervened group after implementing SBAR tool, and the proportion of incidences reported due to communication errors decreased significantly in the intervened group, from 31% to 11%.[35,12] Therefore, we believe that a standardized hand-over checklist like SBAR is vital in both wards for the improvement of this routine process. We designed a checklist similar to SBAR by considering culture and current routine standards affiliated to our study setting [Annexure 1].
An effective hand-over communication is not part of staff educational curriculum. So, development and implication of an appropriate educational program can significantly improve this process. An experimental study evaluated the undergraduate nursing students’ performance using the standardized communication tool SBAR. The study found that continuing education and training in hospitals can considerably improve their learning abilities.[36] It is logical to create some guidelines and protocols to standardize this process like many other countries do.[11,12,13] Standardization can help us improve this routine process because information can be conveyed more efficiently and with a higher rate of reliability.[12]
Correct procedure at the correct body site
Several types of surgical checklists have been created to control the risks during invasive procedures.[37,38,39] These checklists are applicable for procedures performed in wards or in all settings in which invasive procedures are performed. Using such safety checklists is useful to ensure that all relevant documents and special equipment are available prior to the start of the procedure and accurately match each patient. It is also useful when verifying the procedure and for correct site marking.[40] According to the results of other studies, adverse events were diminished due to using a safety checklist during interventional procedures.[41] According to the results of a review, benefits from these checklists will be of particular value in developing countries, where resources and surgical practice are behind compared to developed countries.[42] In our setting, the risk of error during an invasive procedure is high due to workload pressure. We believe checklists would be particularly useful in other settings of developing countries. Therefore, we designed a safety procedure checklist similar to WHO safety surgery checklist with some modifications [Annexure 2].
On the other hand, a proper consent form (one of the six important surgical safety program factors) is required to eliminate preventable surgical harms.[43] According to our observation, a list of major procedures that required obtaining consent forms before being performed, as well as standard consent forms, were also available in both wards. Nonetheless, some of the respondents were not aware of the existence of such a list or form. This could indicate that a consent form was not filled out in the required situations, as well as the absence of a proper educational program for staff.
It is vital for the patient to be personally involved in their care process in order to improve the quality of care and patient safety, so proper implementation of the consent form is an important component for all invasive procedures and needs to be improved in both wards by training staff and providing proper tools.[17] There were some differences between what was observed and what was reported by the staff that can only be interpreted as a sign of unavailability of proper guidelines or a misunderstanding of the questions. Some staff also informed their patients verbally about the procedures.
Hand hygiene
Our results in this cross-sectional study indicated that basic HH facilities had some limitations in these wards. Several factors can influence the HH compliance among health care workers, and its promotion is particularly complex in the developing countries where limited resources can strongly influence practices.[44,45,46,47,48] Evidence indicated that when basic HH apparatuses, such as alcohol-based hand rubs, were available and easily accessible at the points of care, usage among healthcare workers increased.[49] A study in a large hospital in Ghana found that limited access to HH facilities was one of the primary recognized causes of low HH compliance.[50] Another study in Africa showed that although severe deficiencies in the infrastructure of HH were identified, the improvement was observed after implementing WHO multimodal HH improvement strategy.[30] However, studies that were conducted in Iran in recent years showed that there was no significant evidence of the availability of necessary resources for HH promotion in hospitals.[31,32,33] Even though necessary resources were available, few staff members were aware of the current status, according to their reports. Perhaps this is because they were not using the existing resources, or they lacked motivation or attention when completing the survey forms. However, for the promotion of HH, we should first provide resources and then consider cultural perceptions, beliefs, and practices.
In order to promote HH in our setting, it is essential to provide alcohol-based hand rub packs in different sizes and set them in various places where staff can easily access them. Disposable towels should also be placed beside sinks, and hand washing reminders should be placed wherever possible. According to the results of a major survey in the USA, alcohol-based hand rubs were continuously available at each point of care in 77.5% of health care facilities. The great majority of facilities displayed posters explaining HH indications and correct techniques for hand rubbing and hand washing (89.9%, 80.6%, and 85.3%, respectively). Other workplace reminders, such as screen savers, were used in 78.3% of facilities.[51] Another infrastructure survey conducted in a teaching hospital in Ghana showed that basic equipment for HH, such as liquid soap dispensers, was not available in some wards. Overall, no single service provision center in that hospital had all the basic facilities needed for effective HH.[52]
CONCLUSIONS
By using data collection forms that were designed according to the WHO suggested actions; we compared “what we have” and “what we should have” in order to successfully implement the three mentioned WHO solutions. We found many shortcomings and limitations, and we overcame them by providing some tools such as protocols, safety procedure checklists, safety hand off checklists, and some resources like hand rubs and reminders. We recommend evaluation of the currently implemented status of patient safety solutions of other Iranian hospitals by comparing them to WHO suggested actions. We also recommend designing another study for comparing the status of some patient safety indexes before and after using designated tools to ensure that practice changes lead to improvements in patient safety.
ACKNOWLEDGEMENTS
We thank the faculty members, residents and staff of Nemazi Hospital Intensive Care Units who participated in this study. The vice-chancellor for research at Shiraz University of Medical Sciences funded this project. This research was performed by Sheida Banihashemi in partial fulfillment of the requirements for certification as a specialist in community medicine at Shiraz University of Medical Sciences in Shiraz, Iran.
ANNEXURE. Annexure 1: Hand-over checklist
Situation
□ Care giver 1 (name and job):
□ Care giver 2 (name and job):
□ Ward:
□ Bed number:
□ Patient name:
□ Patient's diagnosis:
□ Personal history (like allergies):
□ Family history:
□ New complaints, wants, or needs:
Background
□Patient's current medication:
□ Recent changes and response to treatment:
□ Recent changes in vital signs:
□ Recent changes in whole body exam:
□ Recent changes in lab data (critical lab values):
□ Recent changes in tests:
Assessment
-
□ Current assessment:
□ Your best judgment/anticipations:
Recommendation
□ Pending tests or lab results:
□ Things should be done of the next few hours:
□ Current recommendation for future care:
□ Plan of action:
□ Prioritization of actions:
□ Your concerns:
□ Other questions and answers:
Annexure 2: Safety procedure checklist
Patient name: Ward: Date:
Team member names Role
1
2
3
4
5
6
Before procedure
□ Confirmation of patient identity (by himself or his family)
□ Confirmation of procedure site and position (by himself or his family)
□ Confirmation of filling the consent form (by himself or his family)
□ Marking the procedure site (if it is applicable)
□ Review the patient history (allergies, risks for blood loss, etc.):
□ Any new concern about the current patient status:
□ Introducing the team members (name and role)
□ Confirmation of required equipment's for procedure, by practitioner
□ Anticipating critical events or concerns by team members (specific equipment requirements, sterility of the instrumentation, special investigations, etc.):
□ Availability of the required test or imaging
□ Indication for surgical site infection bundle (prophylactic antibiotic, hair removal, etc.)
□ Other questions and answers:
After procedure
□ Confirmation of recorded procedure name
□ Confirmation of counting the instruments, swabs, and sharp (if applicable)
□ Confirmation of labeling the specimens
□ Any problems that need to be addressed
□ Key concerns for management of this patient:
□ Items that must be followed:
□ Other questions and answers:
Name:
Signature of registered practitioner:
Annexure 3: “Hand-over” data collection form:
-
Is a standardized form available for hand-over communication and passing patient specific information from one caregiver to another, between staff change of shift?
- □ Yes
- □ No
- □ Don’t Know
-
If the form is available, is it filled out?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is a standardized form available for hand-over communication and passing patient specific information from one caregiver to another, between different patient care units in the course of a patient transfer?
- □ Yes
- □ No
- □ Don’t know
-
If the form is available, is it filled out?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is a standardized form available for hand-over communication during discharge of the patient back home or to another facility?
- □ Yes
- □ No
- □ Don’t know
-
If the form is available, is it filled out?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is training on effective hand-over communication, part of the educational curriculum?
- □ Yes
- □ No
- □ Do’t know
-
Is any specified room or place, used during physician and nursing change-of-shift reporting and hand-over?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Except in the case of an emergency, are any interruptions occurring during clinical hand-over?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is anyone responsible for dealing with distractions that can disturb the hand-over process including bleeps, telephones, relatives, nurses, and other doctors?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
How much time do you spent for patients hand-over between changes of shifts?
- □ <30 min
- □ 30-60 min
- □ More than 60 min
-
How much time do you spent for each patient hand-over between changes of shifts?
- □ <5 min
- □ 5-10 min
- □ More than 10 min
-
Please fill out the below table
Admitting diagnosis
Secondary diagnosis
Consultations that has been done in the previous shift
Complications that has occurred for the patient in the previous shift
Recently changes in medication or fluid therapy
Abnormal labs
Recently changes in vital signs
Recently changes in drains/tubes/wounds/dressings
Recently changes in clinical status/physical examination
Any concerns about this patient
Care/issues/orders/pending treatment/tests/items left undone requiring follow-up
Annexure 4: “Correct procedure at correct body site” data collection form
-
Are the patient and his/her family informed about procedure rationale, plans, options, and risks before the procedures that need obtaining consent before the performance?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is any guide sheet or educational content for informing the patient and his/her family about the procedure rationale, plans, options and risks, and available in your ward?
- □ Yes
- □ No
- □ Don’t know
-
If yes, is any checklist for monitoring of patient education, available in your ward?
- □ Yes
- □ No
- □ Don’t know
-
Is there any list (or catalogue) of major procedures’ name that needs obtaining consent before the performance, available in your ward?
- □ Yes
- □ No
- □ Don’t know
-
Is consent obtained for all procedures (that need obtaining consent before the performance)?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is there any consent form including the full name of the procedure, site, anesthesia plan or preferences for all procedures that need obtaining consent before the performance, available in your ward?
- □ Yes
- □ No
- □ Don’t know
-
Are consents documented for all procedures that need obtaining consent before the performance in your ward?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is the current information on the patient's medical status and proposed procedure plans obtained by practitioners at the day of the procedure?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is any checklist available for obtaining the current information on the patient's medical status and proposed procedure plans at the day of the procedure?
- □ Yes
- □ No
- □ Do’t know
-
If yes, is this checklist filled out when needed?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is any checklist available to ensure the performance of correct procedure at the correct body site?
- □ Yes
- □ No
- □ Don’t know
If yes, answer the next three questions:
-
Is any part of the checklist questions completed before induction of anesthesia as “Sign in”?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is any part of the checklist questions completed before start of surgical intervention as “Time out”?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is any part of the checklist questions, completed before any member of the team leaves the procedure room as “Time out”?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is the procedure site marked before the performance of the procedure?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
If yes, answer the next two questions:
-
Does the patient confirm the procedure site and markings?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is anyone responsible for the marking of the procedure site if the patient is not conscious?
- □ Yes
- □ No
- □ Dont’ Know
Annexure 5: “Hand hygiene” data collection form
-
Is running water available?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is water visibly clean?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
What kind of taps is available?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Are disposable towels available at all sinks?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is soap available at all sinks?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is an alcohol-based hand rub available?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
If yes, what type of hand rub dispensers are available? (select all applicable answers)
- □ Pocket bottle
- □ Bottle affixed to trolley/tray
- □ Bottle affixed to bed
- □ Wall dispenser
- □ Dispenser located on bedside table/trolley
-
If wall dispensers are available, are they placed at the point of care*?
- □ Yes
- □ Yes but not at each point of care
- □ No
-
Does every health-care worker have easy access to hand rub pocket bottles?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Is there an assigned person responsible for the refilling or replacement of empty dispensers?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Are hand rub dispensers replaced when empty?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Are posters illustrating hand wash technique displayed beside each sink?
- □ Yes
- □ No
-
Are posters illustrating hand rub technique displayed close to the dispensers and in multiple areas of the ward?
- □ Yes
- □ No
-
Are posters illustrating indications for HH displayed in multiple areas of the ward?
- □ Yes
- □ No
-
Is any other type of reminder on HH displayed/available on this ward?
- □ Yes
- □ No
-
Are examination gloves available on this ward?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
Are audits on HH compliance periodically performed on this ward?
- □ Always
- □ Often
- □ Sometimes
- □ Rarely
- □ Never
-
If yes, how frequently?
- □ At least once a year
- □ At least once every 2 years
- □ Less frequently
HH=Hand hygiene
Footnotes
Source of Support: Shiraz University of Medical Sciences.
Conflict of Interest: None declared.
REFERENCES
- 1.Geneva: World Health Organization; 2014. [Last accessed on 2014 Sep 03]. World Health Organization. 10 Facts on Patient Safety. Available from: http://www.who.int/features/factfiles/patient_safety/en/index.html . [Google Scholar]
- 2.Emanuel L, Berwick D, Conway J, Combes J, Hatlie M, Leape L, et al. 1: Assessment. Rockville (MD): Agency for Healthcare Research and Quality; 2008. [Last accessed on 2014 Sep 03]. Advances in Patient Safety: New Directions and Alternative Approaches. Available from: http://www.ahrq.gov/downloads/pub/advances2/vol1/advances-emanuel-berwick_110.pdf . [Google Scholar]
- 3.Sousa P, Uva AS, Serranheira F, Nunes C, Leite ES. Estimating the incidence of adverse events in Portuguese hospitals: A contribution to improving quality and patient safety. BMC Health Serv Res. 2014;14:311. doi: 10.1186/1472-6963-14-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kohn L, Corrigan J, Donaldson M, editors. Washington, DC: Institute of Medicine – National Academy Press; 1999. [Last accessed on 2014 Sep 04]. To Err is Human: Building a Safer Health System. Available from: http://www.nap.edu/books/0309068371/html/ [Google Scholar]
- 5.Thomas EJ, Studdert DM, Newhouse JP, Zbar BI, Howard KM, Williams EJ, et al. Costs of medical injuries in Utah and Colorado. Inquiry. 1999;36:255–64. [PubMed] [Google Scholar]
- 6.Mohsenzadeh A, Rezapour S, Birjandi M. Frequency of medical errors in hospitalized children in Khorramabad Madani hospital during six months in 2008. Yafteh. 2010;11:31–8. [Google Scholar]
- 7.Zinn C. 14,000 preventable deaths in Australian hospitals. BMJ. 1995;310:1487. doi: 10.1136/bmj.310.6993.1487. [DOI] [PubMed] [Google Scholar]
- 8.Neale G, Woloshynowych M, Vincent C. Exploring the causes of adverse events in NHS hospital practice. J R Soc Med. 2001;94:322–30. doi: 10.1177/014107680109400702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Communication during Patient Hand-Overs. Geneva: World Health Organization; 2007. [Last accessed on 2014 Sep 02]. World Health Organization. WHO Collaborating Centre for Patient Safety Solutions. Available from: http://www.who.int/patientsafety/solutions/patientsafety/PS-Solution3.pdf . [Google Scholar]
- 10.Manser T, Foster S. Effective handover communication: An overview of research and improvement efforts. Best Pract Res Clin Anaesthesiol. 2011;25:181–91. doi: 10.1016/j.bpa.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 11.Department of Health, Victoria, Australia. Clinical handover tools (November 2006). Suggested content for CH Protocol or Guidelines; November. 2006. [Last accessed on 2013 Sep 03]. pp. 1–2. Available from: http://www.health.vic.gov.au/qualitycouncil/downloads/ch_policy_guidelines_content.pdf .
- 12.Australian Commission on Safety and Quality in Health Care. Guide to Clinical Handover Improvement. 2010. [Last accessed on 2014 Sep 04]. pp. 33–5. Available from: http://www.safetyandquality.gov.au/wp-content/uploads/2012/01/ossie.pdf .
- 13.National Health Service. Institute for Innovation and Improvement. Acute SBAR Communication Tool. [Last accessed on 2014 Sep 04]. Available from: http://www.institute.nhs.uk/images//documents/SaferCare/SBAR/Cards/Acute__SBARv4.pdf .
- 14.Vardaman JM, Cornell P, Gondo MB, Amis JM, Townsend-Gervis M, Thetford C. Beyond communication: The role of standardized protocols in a changing health care environment. Health Care Manage Rev. 2012;37:88–97. doi: 10.1097/HMR.0b013e31821fa503. [DOI] [PubMed] [Google Scholar]
- 15.Malekzadeh J, Mazluom SR, Etezadi T, Tasseri A. A standardized shift handover protocol: Improving nurses’ safe practice in intensive care units. J Caring Sci. 2013;2:177–85. doi: 10.5681/jcs.2013.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kable AK, Gibberd RW, Spigelman AD. Adverse events in surgical patients in Australia. Int J Qual Health Care. 2002;14:269–76. doi: 10.1093/intqhc/14.4.269. [DOI] [PubMed] [Google Scholar]
- 17.Geneva: World Health Organization; 2007. [Last accessed on 2014 Sep 02]. World Health Organization. WHO Collaborating Centre for Patient Safety Solutions. Available from: http://www.who.int/patientsafety/solutions/patientsafety/PS-Solution4.pdf . [Google Scholar]
- 18.Collins SJ, Newhouse R, Porter J, Talsma A. Effectiveness of the surgical safety checklist in correcting errors: A literature review applying Reason's Swiss cheese model. AORN J. 2014;100:65–79.e5. doi: 10.1016/j.aorn.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 19.Kasatpibal N, Senaratana W, Chitreecheur J, Chotirosniramit N, Pakvipas P, Junthasopeepun P. Implementation of the World Health Organization surgical safety checklist at a university hospital in Thailand. Surg Infect (Larchmt) 2012;13:50–6. doi: 10.1089/sur.2011.043. [DOI] [PubMed] [Google Scholar]
- 20.Semel ME, Resch S, Haynes AB, Funk LM, Bader A, Berry WR, et al. Adopting a surgical safety checklist could save money and improve the quality of care in U.S. hospitals. Health Aff (Millwood) 2010;29:1593–9. doi: 10.1377/hlthaff.2009.0709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor B, Slater A, Reznick R. The surgical safety checklist effects are sustained, and team culture is strengthened. Surgeon. 2010;8:1–4. doi: 10.1016/j.surge.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 22.Treadwell JR, Lucas S, Tsou AY. Surgical checklists: A systematic review of impacts and implementation. BMJ Qual Saf. 2014;23:299–318. doi: 10.1136/bmjqs-2012-001797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Askarian M, Kouchak F, Palenik CJ. Effect of surgical safety checklists on postoperative morbidity and mortality rates, Shiraz, Faghihy Hospital, a 1-year study. Qual Manag Health Care. 2011;20:293–7. doi: 10.1097/QMH.0b013e318231357c. [DOI] [PubMed] [Google Scholar]
- 24.Spruce L. Back to basics: Implementing the surgical checklist. AORN J. 2014;100:465–73. doi: 10.1016/j.aorn.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 25.Klevens RM, Edwards JR, Richards CL, Jr, Horan TC, Gaynes RP, Pollock DA, et al. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007;122:160–6. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allegranzi B, Bagheri Nejad S, Combescure C, Graafmans W, Attar H, Donaldson L, et al. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet. 2011;377:228–41. doi: 10.1016/S0140-6736(10)61458-4. [DOI] [PubMed] [Google Scholar]
- 27.Geneva: World Health Organization; 2005. World Health Organization. The Global Patient Safety Challenge. 2005-2006 “Clean Care is Safer Care”; pp. 1–25. [Google Scholar]
- 28.United States: Centers for Disease Control and Prevention; 2002. [Last accessed on 2014 Sep 03]. Guideline for Hand Hygiene in Health-Care Settings. Available from: http://www.cdc.gov/mmwr/PDF/rr/rr5116.pdf . [Google Scholar]
- 29.Geneva: World Health Organization; 2009. [Last accessed on 2014 Sep 03]. World Health Organization. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Care; p. 270. Available from: http://www.whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf . [PubMed] [Google Scholar]
- 30.Allegranzi B, Sax H, Bengaly L, Richet H, Minta DK, Chraiti MN, et al. Successful implementation of the World Health Organization hand hygiene improvement strategy in a referral hospital in Mali, Africa. Infect Control Hosp Epidemiol. 2010;31:133–41. doi: 10.1086/649796. [DOI] [PubMed] [Google Scholar]
- 31.Ataei B, Zahraei SM, Pezeshki Z, Babak A, Nokhodian Z, Mobasherizadeh S, et al. Baseline evaluation of hand hygiene compliance in three major hospitals, Isfahan, Iran. J Hosp Infect. 2013;85:69–72. doi: 10.1016/j.jhin.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 32.Askarian M, Hajiabadi MJ, Kashkooli YA, Yousofi M, Fathi H, Kouchack F, et al. Improving infection prevention methods in hemodialysis units: A multicenter survey. Am J Infect Control. 2014;42:193–4. doi: 10.1016/j.ajic.2013.09.024. [DOI] [PubMed] [Google Scholar]
- 33.Malekmakan L, Haghpanah S, Askarian M, Jowkari M, Moalaee M. Hand hygiene in Iranian health care workers. Am J Infect Control. 2008;36:602–3. doi: 10.1016/j.ajic.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 34.Geneva: World Health Organization; 2009. [Last accessed on 2014 Sep 03]. World Health Organization. Guide to Implementation of the WHO Multimodal Hand Hygiene Improvement Strategy. Available from: http://www.whqlibdoc.who.int/hq/2009/WHO_IER_PSP_200902_eng.pdf . [Google Scholar]
- 35.Randmaa M, Mårtensson G, Leo Swenne C, Engström M. SBAR improves communication and safety climate and decreases incident reports due to communication errors in an anaesthetic clinic: A prospective intervention study. BMJ Open. 2014;4:e004268. doi: 10.1136/bmjopen-2013-004268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kesten KS. Role-play using SBAR technique to improve observed communication skills in senior nursing students. J Nurs Educ. 2011;50:79–87. doi: 10.3928/01484834-20101230-02. [DOI] [PubMed] [Google Scholar]
- 37.Safe Surgery Checklist. The Joint Commission. [Last accessed on 2014 Dec 01]. Available from: http://www.jointcommission.org/safe_surgery_checklist/
- 38.WHO. Surgical Safety Checklist. World Health Organization . [Last accessed on 2014 Dec 01]. Available from: http://www.who.int/patientsafety/safesurgery/checklist/en/
- 39.Patient Safety Tool: SURPASS Checklist. Becker's Infection and Quality Control. [Last accessed on 2014 Dec 09]. Available from: http://www.beckersasc.com/asc-quality-infection-control/patient-safety-tool-surpass-checklist-for-safe-surgery.html .
- 40.Banschbach SK. Revisiting the universal protocol. AORN J. 2009;89:257–9. doi: 10.1016/j.aorn.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 41.Corso R, Vacirca F, Patelli C, Leni D. Use of “Time-Out” checklist in interventional radiology procedures as a tool to enhance patient safety. Radiol Med. 2014;119:828–34. doi: 10.1007/s11547-014-0397-9. [DOI] [PubMed] [Google Scholar]
- 42.Vivekanantham S, Ravindran RP, Shanmugarajah K, Maruthappu M, Shalhoub J. Surgical safety checklists in developing countries. Int J Surg. 2014;12:2–6. doi: 10.1016/j.ijsu.2013.10.016. [DOI] [PubMed] [Google Scholar]
- 43.Kuo CC, Robb WJ., rd Critical roles of orthopaedic surgeon leadership in healthcare systems to improve orthopaedic surgical patient safety. Clin Orthop Relat Res. 2013;471:1792–800. doi: 10.1007/s11999-012-2719-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Geneva: World Health Organization; 2009. [Last accessed on 2014 Sep 03]. World Health Organization. WHO Guidelines for Hand Hygiene in Health Care. Available from: http://www.who.int/gpsc/5may/tools/who_guidelines-handhygiene_summary.pdf . [Google Scholar]
- 45.Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: Performance, beliefs, and perceptions. Ann Intern Med. 2004;141:1–8. doi: 10.7326/0003-4819-141-1-200407060-00008. [DOI] [PubMed] [Google Scholar]
- 46.Rebaudet S, De Pina JJ, Rapp C, Kraemer P, Savini H, Demortiere E, et al. Risk of nosocomial infection in Intertropical Africa. Part 4: Prevention. Med Trop (Mars) 2008;68:73–82. [PubMed] [Google Scholar]
- 47.Borghi J, Guinness L, Ouedraogo J, Curtis V. Is hygiene promotion cost-effective. A case study in Burkina Faso? Trop Med Int Health. 2002;7:960–9. doi: 10.1046/j.1365-3156.2002.00954.x. [DOI] [PubMed] [Google Scholar]
- 48.Hugonnet S, Perneger TV, Pittet D. Alcohol-based handrub improves compliance with hand hygiene in intensive care units. Arch Intern Med. 2002;162:1037–43. doi: 10.1001/archinte.162.9.1037. [DOI] [PubMed] [Google Scholar]
- 49.Wharton EM, Platt AJ. Can we improve doctors’ hand hygiene on ward rounds? J Hosp Infect. 2006;64:400–1. doi: 10.1016/j.jhin.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 50.Owusu-Ofori A, Jennings R, Burgess J, Prasad PA, Acheampong F, Coffin SE. Assessing hand hygiene resources and practices at a large African teaching hospital. Infect Control Hosp Epidemiol. 2010;31:802–8. doi: 10.1086/654005. [DOI] [PubMed] [Google Scholar]
- 51.Allegranzi B, Conway L, Larson E, Pittet D. Status of the implementation of the World Health Organization multimodal hand hygiene strategy in United States of America health care facilities. Am J Infect Control. 2014;42:224–30. doi: 10.1016/j.ajic.2013.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yawson AE, Hesse AA. Hand hygiene practices and resources in a teaching hospital in Ghana. J Infect Dev Ctries. 2013;7:338–47. doi: 10.3855/jidc.2422. [DOI] [PubMed] [Google Scholar]


