Abstract
Specialized training for healthcare professionals (HCP) in order to reduce HIV/AIDS related stigma must be part of a public health model for HIV/AIDS. Tested interventions to reduce HIV/AIDS related stigma among HCP have been mostly absent from these efforts. A qualitative approach was used to assess stigma reduction within a traditional randomized controlled design in order to better understand how our current stigma intervention worked and was understood by 2nd year medical students. After conducting a quantitative follow up survey one-year post intervention we conducted 20 in-depth qualitative interviews with a subsample of our intervention group participants as part of the overall evaluation process. Once the interviews were finished, we transcribed them and used NVivo (v.8) to organized the qualitative data. In the process of analyzing the qualitative data we identified core intervention areas participants described as useful for their training and development: (1) acquiring more HIV/AIDS-related knowledge, (2) increased skills for management of high stigma situations, and (3) the ability to identify socio-structural factors that foster HIV infection among clients. The gathered information is important in order to have a deep understanding of how attitudinal change happens as part of our intervention strategies. Keywords: HIV/AIDS, Stigma, Randomized Controlled Trial, Qualitative Evaluation, Medical Students, Puerto Rico
HIV/AIDS stigma (HAS) has been documented as having negative consequences for people living with HIV/AIDS (PLWHA). Adverse effects include lack of access to treatment, problematic adherence to treatment, social isolation, and negative mental health consequences (Herek, 1999; Kuang, Li, Ma, & Liao, 2005; Phelan, Lucas, Ridgeway, & Taylor, 2014; Stangl, Lloyd, Brady, Holland & Baral, 2013). HAS remains one of the most challenging barriers to maintaining the overall health of PLWHA (Varas-Díaz et al., 2013). From a public health framework, HAS fosters and increase gaps in health disparities including negative outcomes (e.g., lack of social support, problems with medication adherence) for individuals who live with the virus (Hatzenbuehler & Link, 2014).
Theoretical perspectives on social stigma have been deeply influenced by Erving Goffman’s work on the subject during the 1980’s. He defined stigma as an attribute that is deeply discrediting to the individual and classified their sources as physical, character or tribal. Goffman’s contributions, although extremely valuable and influential, have been criticized for emphasizing the individual’s characteristics in conceptualizations of stigma (Ainlay, Becker, & Coleman, 1986). The emphasis of the micro-level one on one interaction has been criticized in the literature for its limitations regarding understanding how stigma is (also) created and manifested at a macro-level, particularly via social institutions (Hatzenbuehler & Link, 2014).
In addition to institutional influences, approaches to HAS reduction strategies have integrated socio-structural factors to gain a better understanding of stigma as a social phenomenon (Parker & Aggleton, 2002; Stangl, Lloyd, Brady, Holland, & Baral, 2013). Hatzenbuehler and Link (2014) define structural stigma as “societal-level conditions, cultural norms, and institutional policies that constrain the opportunities, resources, and wellbeing of the stigmatized.” (Hatzenbuehler & Link, 2014, p. 2).
This dimension of stigma includes structural discrimination, which result in unfair health policies that can create and increase health disparities among affected populations (Angermeyer, Matschinger, Link, & Schomerus, 2014; Link & Phelan, 2014). HAS has historically encompassed both dimensions. One the one hand it has hindered one on one social interactions, but more importantly it has also become a structural problem reflected in restrictive health policies and the worldwide response to the disease.
HIV/AIDS Stigma among Healthcare Providers
Global efforts are in effect to reduce HAS (Apinundecha, Laohasiriwong, Cameron, & Lim, 2007; Barroso et al., 2014; Li et al., 2010; Li et al., 2013; Neema et al., 2012; Stangl et al., 2013). Reducing HAS among health professionals is considered a priority in order to foster better services for PLWHA (U.S. Department of Health & Human Services, 2010; Varas-Díaz, Neilands, Malavé-Rivera, & Betancourt, 2010). HAS that emanates from health care professionals is a potential obstacle for the linkage to and retention in care among PLWHA (Li et al., 2007; Nyblade, Stangl, Weiss, & Ashburn, 2009; Varas-Díaz et al., 2013; Varas-Díaz et al., 2012). The current literature indicates there is a scarcity of HAS reduction interventions targeted to health professionals, and even less that focus on socio-structural approaches to stigma reduction (Parker & Aggleton, 2002; Stangl et al., 2013). Therefore, it is critical to identify interventions that effectively reduce HAS among health professionals while they are still in training and eager to learn new perspectives on health (Brown, Trujillo, & Mcintyre, 2008; Stangl et al, 2013).
The SPACES Project
In recent years, HAS interventions have been tested in different populations of healthcare providers included doctors and nurses with positive results on stigma reduction (Varas-Díaz et al., 2013; Li et al., 2013). From these interventions we have learned that understanding how structural factors influence HAS is a vital part of impacting populations of interest (Stangl et al., 2013). In this context, the SPACES project was a randomized controlled trial (RCT) conducted to test a HAS reduction intervention in a sample of medical students in Puerto Rico. The intervention is a nine-hour workshop divided into three sessions (three hours each). SPACES addresses the sources and functions of HAS via multiple theoretical approaches (from micro to macro levels) in order to have participants understand how stigma may be manifested in health care scenarios via one on one interactions and also through hospital policies. Therefore SPACES directly and simultaneously addressed the manifestation of stigma on both micro and macro levels within the health care setting. The aim of our main study was to assess the efficacy of the SPACES intervention in reducing HAS attitudes among medical students in Puerto Rico (micro level). Furthermore, we aimed to have the tested intervention included as part of the training curriculum for future physicians, therefore changing the traditional educational strategies on HIV/AIDS in local medical schools (macro level). The intervention was efficacious for stigma reduction among medical students with continued effects at 12-months after completing the intervention (Varas-Díaz et al., 2013).
Although traditional intervention testing strategies might end with the implementation of a randomized clinical trial, our team also aimed to richly detail how participants described their experience and further conceptualized HAS after completing the intervention. Therefore, we implemented a qualitative research strategy to better understand these phenomena.
Qualitative Techniques to Compliment RCTs to Reduce HIV/AIDS Stigma
Qualitative approaches within traditional randomized controlled designs can foster and improve knowledge of how HAS interventions work. RCTs are considered the gold standard to establish causal relationships in health sciences research (Lewin, Glenton, & Oxman, 2009) and is particularly important for testing the efficacy of behavioral and attitudinal interventions. Still, the inclusion of mixed methods in RCTs is increasing, specifically with the integration of qualitative techniques. Using different approaches to evaluate an intervention is a good tool to use when trying to understand and change social phenomena (Hawe, Shiell, Riley, & Gold, 2004). It is also not uncommon to see the use of mixed methods as part of an evaluation of intervention research (Catallo, Jack, Ciliska, & MacMillan, 2013; Nelson et al., 2013; Sokunbi, Cross, Watt, & Moore, 2010; Young, Gomersall, & Bowen, 2012).
The use of mixed methods stems from the need to understand how an RCT’s efficacy is embedded within a context that can facilitate or hinder its implementation (e.g., qualitative process evaluations). Although challenges abound when combining research techniques in a single study, the benefits can be considerable (Catallo et al., 2013). Mixed method approaches can contribute to a better understanding of implementation and evaluation components, while also strengthening our interpretation of the intervention’s results and our ability to make recommendations for future implementation. Mixed methods approaches have been used to explain reasons for lack of significant effects when testing interventions (Hawe et al., 2004). In this paper we aim to document the use of qualitative techniques to assess HAS reduction within a traditional randomized controlled design in order to better understand how the SPACES intervention was interpreted by participants (Varas-Díaz et al., 2013).
Method
Design
The SPACES intervention was tested via an RCT with a sample of 507 medical students in Puerto Rico. After the intervention group participants completed their 12-month quantitative follow-up assessment they were eligible to participate in a qualitative phase consisting of in-depth interviews. Our study consisted of implementing a sequential explanatory design in which our qualitative component followed our quantitative RCT to explore the experience of the participants who had participated in the SPACES intervention (Creswell, Plano Clark, Gutman, & Hanson, 2003). We conducted 20 semi-structured interviews with eligible participants. Our data analysis process was guided by Social Stigma Theory and Discourse Analysis approaches (Blumer, 1986; Chandler, 2002; Goffman, 1963; Starks & Brown-Trinidad, 2007).
Sample
The sample of this study was composed of 20 participants selected from the SPACES project intervention group (Varas-Díaz et al., 2013). The statistician in our team identified participants who scored the highest and lowest levels of change in HAS attitudes at 12 months post intervention. These scores emanated from the measure used to assess the impact of our intervention. The Stigma and HIV/AIDS Scale is a 44-item scale that addresses the social meanings ascribed to PLWHA via a 5-point Likert scale with values ranging from strongly agree (score of 5) to strongly disagree (score of 1). The scale has been documented as reliable when used with health professionals at α=.91 (Varas-Diaz & Neilands, 2009).
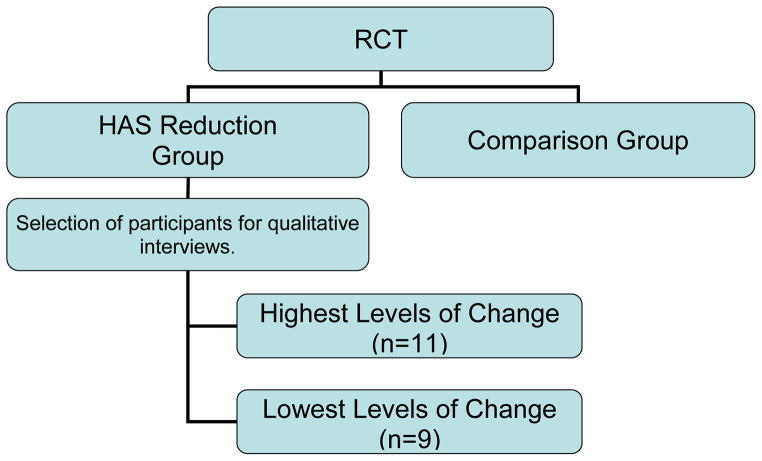
The characteristics of each participant (low vs. high changers) were not informed to the rest of the team who was blinded in order to avoid bias while interacting with interviewees. Participants were then contacted via phone calls or emails and invited to engage in our interview (See Figure 1). These contacts yielded 11 participants from the group with the highest levels of change and 9 from the group with the lowest levels of change. Demographic data for this subsample are presented in Table 1. The participants had a mean age of 26 (range 22–31 years old). More than half of the sample was composed of females [55%; n=11]. All interviews were conducted in Spanish and were then translated to English reporting the analysis.
Figure 1.
Participant Selection Process
Table 1.
Sample Characteristics
| Variable | n | % |
|---|---|---|
| Female gender | 11 | 55.0 |
| Heterosexual orientation | 19 | 95.0 |
| National origin | ||
| Puerto Rican | 15 | 75.0 |
| Other | 5 | 25.0 |
| Ever tested for HIV | 12 | 60.0 |
| HIV negative test result (among those who tested) | 11 | 55.0 |
| Knew someone with HIV | 7 | 35.0 |
| Taken a class where HIV was discussed | 18 | 90.0 |
| Believe other medical students discriminate | 20 | 100.0 |
| Religion importance | ||
| Somewhat important | 3 | 15.0 |
| Important | 8 | 40.0 |
| Very Important | 9 | 45.0 |
| Annual income | ||
| < $10,000 | 5 | 25.0 |
| $10,001–$20,000 | 5 | 25.0 |
| $20,001–$30,000 | 1 | 5.0 |
| $30,001–$40,000 | 3 | 15.0 |
| $40,001–$50,000 | 3 | 15.0 |
| > $60,000 | 3 | 15.0 |
| Perception of risk of HIV infection | ||
| Not at all | 4 | 20.0 |
| A little | 8 | 40.0 |
| A regular amount | 6 | 30.0 |
| A lot | 1 | 5.0 |
| Medical students attitudes towards PLWHA | ||
| Totally positive | 1 | 5.0 |
| Partially positive | 6 | 30.0 |
| Neutral | 7 | 35.0 |
| Partially negative | 6 | 30.0 |
| Prepared to provided services to PLWHA | ||
| Totally agree | 4 | 20.0 |
| Partially agree | 16 | 80.0 |
Notes: For sexual orientation, the comparison category is homosexual/lesbian/bisexual. For HIV testing, the comparison group was "Don't know" (no respondents reported an HIV-positive test result).
Procedure
Once our team completed the implementation of SPACES, we selected the 20 participants to engage in qualitative interviews taking into consideration gender balance in the sample (See Figure 1). Once participants accepted our invitation to engage in the interviews, we set a date of their convenience. The interviews were carried out during the period of June, 2009 to February, 2010. The interviews were semi-structured and conducted face to face or via phone, depending on the participant’s availability. After a brief explanation of the purpose of the interview, participants read and completed a consent form. We audio-recorded each interview for the purpose of analysis. All study procedures were approved by the Institutional Review Board at the University of Puerto Rico.
Measures
Our qualitative interview guide included open-ended questions addressing the following subjects: (1) their evaluation of the overall experience in the SPACES project; (2) HIV-related knowledge gained as part of the intervention; (3) perceived self-efficacy for interacting with PLWHA in health care facilities and (4) understanding of socio-structural factors that can foster HIV infection and HAS. These subjects were integrated to the interview guide as they are an essential part of understanding participant’s evaluation of the intervention and because they have been identified as key components of stigma change (i.e., knowledge, self-efficacy, understanding of the social context; Varas & Neilands, 2009). The interview duration was approximately 25 minutes.
Analysis
In order to ensure the quality of our analysis, we started with a supervised transcription process to ensure fidelity. Transcriptionists were trained on the appropriate way to transcribe an audio interview (Poland, 2002). We developed a guide with steps and instructions on how to transcribe in order to ensure quality of the final product. Afterwards, the team read the transcriptions while listening to the audiotapes in order to identify inconsistencies between them. This team was composed by doctoral students and the principal and co-investigators. The team met and corrected all errors in the transcriptions. Once this process was completed for each audiotape, the data analysis procedures began. We carried out a discourse analysis procedure based on Potter and Wetherell’s framework (2004) in order to document how participants verbally constructed the subjects of interest of our study and simultaneously allow for emerging thematic patters to be manifested without constraints of pre-planned categories of analysis. The research team met on a weekly basis for three months to identify themes or patterns in our transcriptions (Catallo et al., 2013). The themes emerged as part of the discussion between team members in a collective manner and only after a team member provided evidence based on the transcribed interviews. Team members developed a list of these themes to keep as a master list for the analysis. These themes continued to be modified throughout the reading of all the transcriptions. Once those general themes were identified for all the interviews, the team searched for texts that evidenced them in the transcriptions. Members of the team continued to discuss all the selected texts for each theme in weekly meetings. This step was carried out in order to ensure that the analysts agreed on the final interpretation of the coded passages. Once an agreement was reached with a passage, it was coded in our interviews via Nvivo software (NVivo V.8; Bazeley, 2007). This consensus-based dispute resolution procedure will generated an inter-rater reliability of 100% for the analysis (Miller, 2001).
Throughout the process several steps were taken in order to ensure the trustworthiness of the data:
supervising the overall transcription process of the audio taped interviews,
meeting with members of the research team to discuss the quality of these transcriptions, and
establishing group discussions throughout the data collection and analysis process so that team members could discuss concerns and findings throughout the data analysis process.
Results
As described in our methods section half of the sample (n=11) was selected from the group with the highest levels of change and half (n=9) were selected from the group with the lowest levels of change. We carried out this division in order to explore potential differences between those individuals we interviewed. Our findings indicated there were no thematic differences between participants’ responses in both groups. Therefore, we present the results from our data analysis for the complete sample.
Emerged Themes
Participants made verbalizations about their experiences in the SPACES workshops. Their answers were organized via our qualitative data analysis into three main thematic patterns. These were
HIV/AIDS related knowledge,
skills for management of stigma situations, and
ability to identify socio-structural factors that foster HIV infection among clients.
In Table 1 we include a description of these three main categories. Below we present each category individually.
HIV/AIDS-related Knowledge
Participant shared their knowledge on HIV/AIDS and their definition of HAS a year after their participated in the SPACES intervention. The SPACES intervention fostered a greater knowledge and exploration of HIV biology and sources of HIV infection. As part of this increased awareness and contextualization of HIV/AIDS, participants were able to define and describe HAS examples based on personal experiences they had encountered after the intervention. They were also able to critically examine how the HIV/AIDS epidemic had been portrayed in Puerto Rico through the media. For example, the following verbalizations reflect how participants developed a more nuanced understanding of sources of infection that have driven the epidemic in their context.
“The high risk groups in Puerto Rico...I know that I always thought that homosexuals were the first risk group, and they are not… ahh it’s intravenous drug users.”
[Female]
“Well… I liked the discussion of high-risk activities at the workshops. It was difficult... We did it in a group dynamic where we had to place HIV risky behaviors or impacted groups in order of prevalence… they included multiple sexual partners, drug users, needle use, health care staff… For me that was the best part.”
[Male]
Participants were also able to define HAS, its impact on health care delivery and on social interaction with PLWHA. This is particularly important as it evidences reflection on what HAS is and its consequences.
“More or less… stigma is … that we can provide less services, less quality services. The use of double gloves when interacting with PLWHA. People who use double gloves when it is unnecessary… right?”
[Female]
“I understand that (stigma) is the stratification that we create that relies in our considerations of who has the disease. Also, what we consider as physical evidence in PLWHA… someone who is homeless, or a person with wounds… we are going to think that the person is HIV positive. A skinny homeless person… We tend to consider that they are HIV positive and it is not necessary the case. There could be other reasons why he or she is sick.”
[Male]
“Well, social stigma in this case for the HIV patients is when people try to put HIV patients in a box and look them as if they were… and it is not correct.”
[Female]
Skills for Identifying HAS and Interacting with PLWHA
Another major theme that emanated from our qualitative interviews was the acquisition of skills for identifying HAS in health care scenarios and interacting with PLWHA in stigma-free ways. Participants provided examples of stigma identification after engaging in the SPACES intervention. Some examples included:
“Well… the workshops changed those ideas about HIV/AIDS. Statistics, epidemiology and the fact that you don’t need to use double gloves with patients. You just need to use the same quality control you use with other patients.”
[Female]
“… so much discrimination with these patients… sometimes due to the health care providers’ lack of information and education.”
[Female]
One participant also described changes in social interaction outside of the clinical setting. He specifically described his interaction with a PLWHA in which handshaking was involved. Although he felt he could engage in such interactions, doubts still lingered over fear of infection. This evidences the complexity entailed in reducing HIV/AIDS stigma as some attitudes may change, but others can still linger.
“…I remember, a few weeks after completed the workshops a homeless came up to me… he wanted to shake my hand and said: “I’m a HIV positive.” Instantly, I thought “why does he want to shake my hand? Maybe, he has something to hide.” But immediately I also thought “I was recently in an HIV workshop…” and then I was super relaxed. I shook hands with him. But you know… then you think: “Do I have to wash my hands or not?” [Male]
[Male]
Understanding of Socio Structural Factors that Foster HAS
Finally, the last thematic pattern found in our analysis was the role of socio-structural factors that drive the HIV/AIDS epidemic, specially, how these factors interact to make people more vulnerable for infection. Participants mentioned the following:
“I also think it is because of lack of education. People don't know what happened. It’s more like prejudice. People judge without having knowledge of the situation, they are not informed. A lot of times, people with this disease have so many social problems, education, homelessness […] it is not only the disease, it is more the consequences and many times we don't know and it is easier to be prejudiced. Stigmatize these people and then throw them to the side. I think it is for lack of education.”
[Female]
“You need to explore your community, see what the risky groups in your community are. For example, intravenous drug users. Identify risky groups and give them information. Here (in Puerto Rico) it is intravenous drug use, why don’t we have a needle exchange program?” [Male]
[Male]
“Sometimes we do not talk about sex with adolescents and young people because of religion… it is awkward for them… but is a great opportunity if we can educate in (schools).”
[Female]
“We need to go to schools, colleges, universities and educate people about stigma using media campaigns…” [Male]
[Male]
“Fear is not an effective teaching technique. That aspect of STD prevention campaigns … it doesn’t work.”
[Female]
Discussion
HAS stigma reduction interventions have increased in the past years and have begun to systematically inform the published scientific literature on the subject. This is an important step in the development, testing and dissemination of effective strategies to address HAS and its multiple manifestations in the lives of PLWHA. Many of the now published interventions have incorporated RCT designs as a tried and tested strategy to assess their efficacy, which provide valuable data on whether these interventions are working in controlled scenarios and reducing HAS. Still, several challenges have been identified and are still of concern when developing and testing these interventions. Some of these include:
scarce evidence of sustained intervention impact beyond three months after completion of the intervention (Brown et al., 2003), and
the need for more rigorous research designs that can better explain how HIV/AIDS stigma is reduced (Stangl et al., 2013).
The integration of qualitative interviews into our overall research design for intervention development and testing served to address these gaps. It allowed us to:
qualitatively explore from the perspective of participants the manner in which HAS reduction was still present after our 12-month quantitative stigma measurement, and
have an in-depth understanding of issues that would still need to be addressed in future versions of the SPACES intervention.
For example, sustained HAS reduction was evident as participants were able to provide detailed descriptions of HAS and identify stigma in their workplace scenarios. Furthermore, participants were able to describe social factors (i.e., lack of education, religion, media) that fostered HIV infection and HAS. This is of vital importance as a deep understanding of the context in which individuals are affected by HIV/AIDS can help medical students avoid blaming patients for their acquisition of the virus, which is a common practice in HAS. Although these subjects were addressed in our intervention workshops, our qualitative evidence allowed us to understand how participants interpreted HAS, its consequences and social determinants beyond the numerical evidence of our RCT quantitative data analysis. Although these statistical tests are of vital importance to document the HAS reduction, they do not yield in-depth descriptions of how HAS reduction is interpreted by participants.
Limitations and Future Directions
One main limitation of our study was that we concentrated our discussion on participants’ experiences and their perception of exercises and subjects discussed through the workshops. Since our qualitative approach was implemented 12 months after completion of the initial study, participants had completed a great deal of quantitative measures in the process. Therefore we concentrated our line of inquiry on issues of importance for intervention development in order to reduce potential burden.
Still, the gathered qualitative evidence also pointed towards areas that need further attention in future implementations of the SPACES intervention. For example, some participants still used language that PLWHA can consider as manifestations of HAS. This was evident in their use of the “high risk group” concept, instead of focusing on individuals’ high-risk behaviors. We were also able to document how even when HAS was reduced, some lingering concerns over fear of infection were present in everyday interactions (i.e., washing hands). In this sense, qualitative evidence allowed us to have a better understanding of areas that our intervention needs to better address in the future when working with our population of interest.
We understand that the overall evaluation of the SPACES intervention was strengthened by the inclusion of qualitative techniques into our quantitative RCT design. This process allowed for a better understanding of how the intervention worked in HAS reduction via examples provided by participants 12-months after participating in our study. Future efforts to test HAS reduction would benefit from this mixed methods approach and would help to better inform the scientific literature on how HAS can be reduced.
Biographies
Melissa Marzán-Rodríguez is a Doctor in Public Health with a major in Epidemiology from the Ponce Health Sciences University (PHSU). Her research work is based at the Public Health Program at PHSU and the Puerto Rico Department of Health. Is an assistant professor at the Public Health Program at PHSU. It’s Certified Public Health from the National Board of Public Health Examiners. Have been published in journals such as AIDS Care, Journal of International Association of Physicians in AIDS Care, and Forum: Qualitative Social Research. Her areas of interest include HIV epidemiology, social epidemiology, drug abuse, qualitative methods, men sex with men, social stigma, and health professional’s trainings. Correspondence regarding this article can be addressed directly to: Melissa Marzán-Rodríguez at melissa.marzan.rdz@gmail.com.
Dr. Nelson Varas-Díaz is interested in the social, political and individual level implications of stigmatization. His academic career addresses the role of social and structural factors in the development of stigmatized individual and collective identities. His research has focused on the social stigmatization of disease (i.e., HIV/AIDS, addiction), marginalized groups (i.e., transgender individuals) and cultural practices (i.e., metal music, religion). These interests are manifested through research, policy work, teaching at the graduate level, independent consulting, and community involvement. Other subjects of interest include: (1) qualitative research, (2) mixed methodology, (3) issues related to community participation, and (4) social justice through research. Correspondence regarding this article can also be addressed directly to: Nelson Varas-Diaz at, nvaras@mac.com.
Torsten B. Neilands is a Professor at the UCSF Center for AIDS Prevention Studies (CAPS) in the Department of Medicine and Center’s Methods Core. Originally trained as a social psychologist, he spent eight years as a statistical consultant at the University of Texas academic computing center before coming to CAPS in 2001. Since arriving at CAPS, Dr. Neilands has participated as statistical co-investigator or consultant on over 50 NIH, CDC, and state projects in the areas of HIV prevention, reproductive health, and tobacco prevention. His methodological areas of interest are multivariate statistical models with a special interest in latent variable models for survey scale development and validation, and mixed effects (i.e., multilevel; HLM) models for clustered and longitudinal data. His substantive interests include training the next generation of HIV-prevention prevention researchers working in U.S. minority communities. Dr. Neilands is currently PI of two NIH-sponsored R25 research education grants to foster grant-writing and related research capacity-building for early-career faculty working in U.S. minority communities to prevent the spread of HIV/AIDS and STIs and to improve the lives of those living with HIV/AIDS. He also actively collaborates as a senior statistician and quantitative methods co-investigator on multiple HIV prevention and tobacco prevention research projects. Correspondence regarding this article can also be addressed directly to: Torsten Neilands at, torsten.neilands@ucsf.edu
Contributor Information
Melissa Marzán-Rodríguez, University of Puerto Rico – Río Piedras, San Juan, Puerto Rico.
Dr. Nelson Varas-Díaz, University of Puerto Rico – Río Piedras, San Juan, Puerto Rico
Torsten Neilands, University of California - San Francisco, San Francisco, California, USA.
References
- Ainlay SC, Becker G, Coleman LM. The dilemma of difference. A multidisciplinary view of stigma. New York, NY: Plenum Press; 1986. [Google Scholar]
- Angermeyer MC, Matschinger H, Link BG, Schomerus G. Public attitudes regarding individual and structural discrimination: Two sides of the same coin? Social Science & Medicine. 2014;103:60–66. doi: 10.1016/j.socscimed.2013.11.014. [DOI] [PubMed] [Google Scholar]
- Apinundecha C, Laohasiriwong W, Cameron MP, Lim S. A community participation intervention to reduce HIV/AIDS stigma, Nakhon Ratchasima province, northeast Thailand. AIDS Care. 2007;19(9):1157–65. doi: 10.1080/09540120701335204. [DOI] [PubMed] [Google Scholar]
- Barroso J, Relf MV, Williams MS, Arscott J, Moore ED, Caiola C, Silva SG. A randomized controlled trial of the efficacy of a stigma reduction intervention for HIV-infected women in the Deep South. AIDS Patient Care STDS. 2014;28(9):489–98. doi: 10.1089/apc.2014.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazeley P. Qualitative data analysis with NVivo. London, UK: Sage; 2007. [Google Scholar]
- Blumer H. Symbolic interactionism. Berkeley, CA: University of California Press; 1986. [Google Scholar]
- Brown L, Mcintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Education Prevention. 2003;15:49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- Catallo C, Jack SM, Ciliska D, MacMillan HL. Mixing a grounded theory approach with a randomized controlled trial related to intimate partner violence: What challenges arise for mixed methods research? Nursing Research and Practice. 2013;2013:1–12. doi: 10.1155/2013/798213. Retrieved from http://dx.doi.org/10.1155/2013/798213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler D. Semiotics: The basics. London, UK: Routledge; 2002. [Google Scholar]
- Creswell JW, Plano Clark VL, Gutman ML, Hanson WE. Advanced mixed methods research designs. In: Tashakkori A, Teddlie C, editors. Handbook of mixed methods in social and behavioral research. Thousand Oaks, CA: Sage; 2003. pp. 209–240. [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. New York, NY: Simon & Schuster, Inc; 1963. [Google Scholar]
- Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Social Science & Medicine. 2014;103:1–6. doi: 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- Hawe P, Shiell A, Riley T, Gold L. Methods for exploring implementation variation and local context within a cluster randomized community intervention trial. Journal of Epidemiology Community Health. 2004;58:788–793. doi: 10.1136/jech.2003.014415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM. AIDS and stigma. American Behavioral Scientists. 1999;42:1106–1116. [Google Scholar]
- Herek GM, Capitanio JP. Symbolic prejudice or fear of infection? A functional analysis of AIDS-related stigma among heterosexual adults. Basic and Applied Social Psychology. 1998;20(3):230–241. [Google Scholar]
- Kuang W, Li J, Ma Y, Liao J. Survey on psychologic status and quality of life for HIV infected people or AIDS patients. Journal of Sichuan University. 2005;36(1):97–100. [PubMed] [Google Scholar]
- Li L, Wu Z, Liang LJ, Lin C, Guan J, Jia M, … Zhiahua Y. Reducing HIV-related stigma in health care settings: A randomized controlled trial in China. American Journal of Public Health. 2013;103(2):286–92. doi: 10.2105/AJPH.2012.300854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Li-Jung L, Chunqing L, Zunyou W, Rotheram-Borus M. HIV prevention intervention to reduce HIH-related stigma: Evidence from China. AIDS. 2010;24:115–22. doi: 10.1097/QAD.0b013e3283313e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Lin C, Wu Z, Rotheram-Borus MJ, Detels R, Jia M. Stigmatization and shame: Consequences of caring for HIV/AIDS patients in China. AIDS Care. 2007;19(2):258–263. doi: 10.1080/09540120600828473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan J. Stigma power. Social Science & Medicine. 2014;103:24–32. doi: 10.1016/j.socscimed.2013.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin S, Glenton C, Oxman A. Use of qualitative methods alongside randomised controlled trials of complex healthcare interventions: Methodological study. BMJ. 2009;339(101):b3496. doi: 10.1136/bmj.b3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller RL. Innovation in HIV prevention: Organizational and intervention characteristics affecting program adoption. American Journal of Community Psychology. 2001;29:621–647. doi: 10.1023/A:1010426218639. [DOI] [PubMed] [Google Scholar]
- Neema S, Atuyambe LM, Otolok-Tanga E, Twijukye C, Kambugu A, Thayer L, McAdam K. Using a clinic based creativity initiative to reduce HIV related stigma at the Infectious Diseases Institute, Mulago National Referral Hospital, Uganda. African Health Science. 2012;12(2):231–239. doi: 10.4314/ahs.v12i2.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson P, Cox H, Furze G, Lewin RJP, Morton V, Norris H, … Carty R. Participants’ experiences of care during a randomized controlled trial comparing a lay-facilitated angina management programme with usual care: A qualitative study using focus groups. Journal of Advanced Nursing. 2013;69(4):840–850. doi: 10.1111/j.1365-2648.2012.06069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyblade L, Stangl A, Weiss E, Ashburn K. Combating HIV stigma in health care settings: What works? Journal of International AIDS Sociology. 2009;12(1):15. doi: 10.1186/1758-2652-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker R, Aggleton P. HIV/AIDS-related stigma and discrimination: A conceptual framework and agenda for action. New York, NY: The Population Council; 2002. [Google Scholar]
- Phelan JC, Lucas JW, Ridgeway CL, Taylor CJ. Stigma, status, and population health. Social Science & Medicine. 2014;103:15–23. doi: 10.1016/j.socscimed.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poland B. Transcription quality. In: Gubrium JF, Holstein JA, editors. Handbook of interview research: Context and method. Thousand Oaks, CA: Sage; 2002. pp. 629–649. [Google Scholar]
- Potter J. Discourse analysis. In: Hardy M, Bryman A, editors. Handbook of data analysis. Thousand Oaks, CA: Sage; 2004. pp. 607–624. [Google Scholar]
- Sokunbi O, Cross V, Watt P, Moore A. Experiences of individuals with chronic low back pain during and after their participation in a spinal stabilisation exercise programme - A pilot qualitative study. Manual Therapy. 2010;15(2):179–84. doi: 10.1016/j.math.2009.10.006. [DOI] [PubMed] [Google Scholar]
- Stangl AL, Lloyd JF, Brady LM, Holland CE, Baral SB. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? Journal of the International AIDS Society. 2013;16(2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks H, Brown-Trinidad S. Choose your method: A comparison of phenomenology, discourse analysis, and grounded theory. Qualitative Health Research. 2007;17:1372. doi: 10.1177/1049732307307031. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services. National HIV/AIDS Strategy (NHAS) 2010 Retrieved from https://www.aids.gov/federal-resources/national-hiv-aids-strategy/overview/
- Varas-Díaz N, Neilands TB. Development and validation of a culturally appropriate HIV stigma scale for Puerto Rican health professionals in training. AIDS Care. 2009;21(10):1259–1270. doi: 10.1080/09540120902804297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varas-Díaz N, Neilands TB, Cintrón-Bou F, Marzán-Rodríguez M, Santos-Figueroa A, Santiago-Negrón S, … Rodríguez-Madrea S. Testing the efficacy of an HIV stigma reduction intervention with medical students in Puerto Rico: The SPACES project. Journal of the International AIDS Society. 2013;16(2):18670. doi: 10.7448/IAS.16.3.18670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varas-Díaz N, Neilands TB, Cintrón-Bou F, Santos-Figueroa A, Marzán-Rodríguez M, Marqués D. Religion and HIV stigma in Puerto Rico: A cultural challenge for training future physicians. Journal of International Association of Physiological AIDS Care. 2014 Retrieved from http://jia.sagepub.com/content/early/2013/02/20/2325957412472935. [PubMed]
- Varas-Díaz N, Neilands TB, Cintrón-Bou F, Santos-Figueroa A, Rodríguez-Madera S, Santiago-Negrón S. The role of gender on HIV stigma among medical students in Puerto Rico: Implications for training and service delivery. Puerto Rico Health Science Journal. 2012;31:220–222. [PMC free article] [PubMed] [Google Scholar]
- Varas-Díaz N, Neilands TB, Malavé-Rivera S, Betancourt E. Religion and HIV stigma: Implications for health professionals in Puerto Rico. Global Public Health. 2010;19:109–118. doi: 10.1080/17441690903436581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young A, Gomersall T, Bowen A. Trial participants’ experiences of early enhanced speech and language therapy after stroke compared with employed visitor support: A qualitative study nested within a randomized controlled trial. Clinical Rehabilitation. 2012;27(2):174–182. doi: 10.1177/0269215512450042. [DOI] [PMC free article] [PubMed] [Google Scholar]