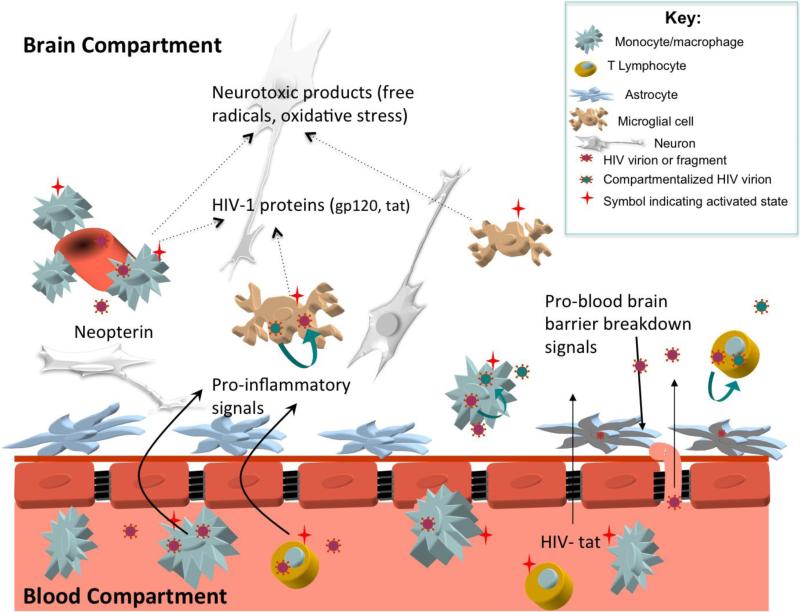
Figure 1.
Potential mechanisms of HIV related CNS injury prior to combination antiretroviral therapy. Systemic activation of immune cells stimulates increased transmigration of lymphocytes and monocytes across the blood brain barrier (BBB). Once in the central nervous system (CNS) compartment, immune cells release pro-inflammatory signals that stimulate further immune cell influx (cytokines such as monocyte chemoattractant protein-1 and interferon-inducible protein-10) and matrix metalloproteinases that disrupt the BBB. Some of the imported cells are infected with HIV, allowing for local production of virions that enter resident CNS cells including perivascular macrophages, brain microglial cells, and astrocytes. Macrophage, microglial, and T lymphocyte infection may support local CNS HIV replication, facilitating emergence of unique ‘compartmentalized’ CNS HIV that reflects production of HIV independent from the periphery. Activated microglia and perivascular macrophages release neurotoxic immune products that lead to neuronal dysfunction; this activation stimulates production of neopterin, a pteridine biomarker of immune activation readily measured in the cerebrospinal fluid. Potentially neurotoxic HIV proteins such as HIV-tat may freely cross the BBB or be released by resident HIV infected cells. Astrocytes harboring HIV virions or fragments may not facilitate viral replication, but may contribute to neuropathogenesis through multiple mechanisms including injury to the blood brain barrier and release of neurotoxic products.