Abstract
Introduction
Pectopexy, a laparoscopic method for prolapse surgery, showed promising results in recent literature. Further improving this approach by reducing surgical time may decrease complication rates and patient morbidity. Since laparoscopic suturing is a time consuming task, we propose a single suture /mesh ileo-pectineal ligament fixation as opposed to the commonly used continues approach.
Methods
Evaluation was performed on human non-embalmed, fresh cadaver pelves. A total of 33 trials was performed. Eight female pelves with an average age of 75, were used. This resulted in 16 available ligaments. Recorded parameters were ultimate load, displacement at failure and stiffness.
Results
The ultimate load for the mesh + simplified single “interrupted” suture (MIS) group was 35 (± 12) N and 48 (± 7) N for the mesh + continuous suture (MCS) group. There was no significant difference in the ultimate load between both groups (p> 0.05). This was also true for displacement at failure measured at 37 (± 12) mm and 36 (±5) mm respectively. There was also no significant difference in stiffness and failure modes.
Conclusion
Given the data above we must conclude that a continuous suture is not necessary in laparoscopic mesh / ileo-pectineal ligament fixation during pectopexy. Ultimate load and displacement at failure results clearly indicate that a single suture is not inferior to a continuous approach. The use of two single sutures may improve ligamental fixation. However, overall stability should not benefit since the surgical mesh remains the limiting factor.
Introduction
In 2010 a new laparoscopic method for prolapse surgery, especially designed for obese women, called pectopexy, was presented by Noe et al. [1]. Literature suggests abdominal sacrocolpopexy to still be the gold standard [2–5]. However, laparoscopic sacrocolpopexy and robot-assisted sacrocolpopexy offer, although more cost and time consuming, effective alternatives [4,6]. In cases where it is difficult to reach the os sacrum however, a pectopexy has also been discussed as a useful and very effective option in recent literature [1,7–9]. The use of the ileo-pectineal ligament for a tension free mesh suspension is not a new concept and has been used by other groups [9,10]. Given the potential of this new method, we find that pectopexy is a surgical approach which may further be optimized. This is especially true since recent results from a prospective, randomized, clinical trial comparing laparoscopic sacrocolpopexy to laparoscopic pectopexy showed the latter to not reduce pelvic space, resulting in, a zero percentage of defecation disorders (compared to 19.5% in the sacrocolpopexy group) [8]. Literature describes the exact pectopexy fixation method of the transverse mesh as being performed with 2 separate stitches on the ileo-pectineal ligament with nonabsorbable sutures (No. 0 with attached needle) [7]. Noe et al. generally uses two single “interrupted” sutures or, in case of a colposuspension, a “continuous” type suture. While most of the surgical steps as described by Banerjee et al. [1] and Alkatout et al. [7] may not be eliminated, surgical time may only be optimized by omitting unnecessary procedures. Since laparoscopic continuous suturing is time-consuming we hypothesized that a single suture may also be sufficient. In order to evaluate this concept a randomized clinical trial should be initiated. Any deviation from gold standard should however be first supported with some sort of biomechanical data; this study therefore asks the following questions:
What load may be supported by standard (continuous) ileo-pectineal fixation methods?
May this load be supported by a single “interrupted” suture?
What are the biomechanical properties of the ileo-pectineal mesh /suture fixation?
What is the limiting factor of said fixation method (mesh, ligament, suture)?
Methods
Fixation method evaluation was performed on human non-embalmed, fresh cadaver pelves. Preparation of the ileo-pectineal ligament was performed by an experienced surgeon. Eight female pelves, average age 75, were used. This resulted in 16 available ligaments. All cadavers were procured from the Institute of Anatomy at the University of Aachen. Identifying data was available only to coauthor P.A. A total of 33 trials were performed. We were able to retest ligaments since all initial trials resulted in mesh failure at loads well within the elastic region of the load-displacement diagram. 4 types of trials were conducted. Group 1 (n = 9) used a single “interrupted” suture in combination with a mesh (MIS). One additional trial run resulted in data that could, unexpectedly, be included into this group. Group 2 (n = 8) evaluated the same mesh and a continuous suture (MCS). Group 3 (n = 8) evaluated a single “interrupted” suture (IS) and group 4 (n = 8) assessed continuous sutures (CS). An undyed, monofilament, partially absorbable mesh was used: SERA MESH® PA (15 x 5 mm—SERAG-WIESSNER GmbH & Co. KG, Naila, Germany). A synthetic, braided, non-absorbable Ethibond suture 0, FSLX needle, 75 cm green filament (Ethicon / Johnson & Johnson, Somerville, NJ, USA) was used in all 4 groups. Fig 1 shows all 4 fixation methods.
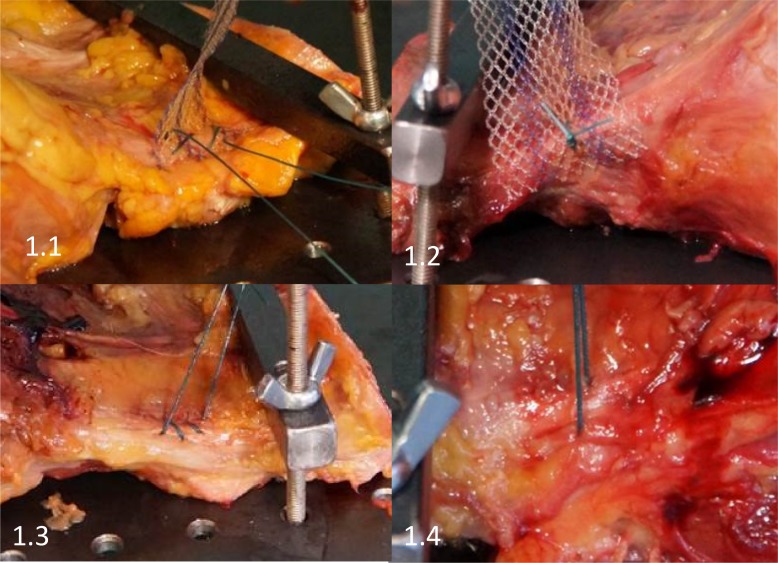
Fig 1. Shown are representative images of the 4 evaluated groups.
Fig 1.1 shows mesh + continuous suture (MCS). Fig 1.2 shows mesh + a single interrupted suture (MIS). Fig 1.3 shows a continuous suture (CS) and Fig 1.4 shows a single interrupted suture (IS).
Analysis was performed on an Instron 5565® test frame using the Bluehill 2 Software®. All tests were transient evaluations of the individual fixation methods at 5 N/s load increase. Recorded parameters were ultimate load (N) and displacement at failure (mm). These resulted in calculated parameters such as stiffness (N/mm) and load at 2 mm displacement. The latter being considered as fixation failure in biomechanical evaluations since stability may be lost as dehiscence exceeds 2 mm. [11–15]
Procedure
Cadaver pelves were prepared in a manner allowing the ileo-pectineal ligament to be placed in the Instron 5565® test frame appropriately, while still attached to the surrounding bone structure. Cadavers were only unfrozen once. Testing proceeded in a continuous /transient manner thereafter. As shown in Fig 1.1 the continuous suture + mesh group allowed for a fixation of the mesh on the ileo-pectineal ligament in a manner allowing for large areas of the mesh to be covered by suture material. Fig 1.2 shows a single “interrupted” suture attaching the mesh to the ligaments. Fig 1.3 shows above-mentioned continuous suture attaching to the ligament without a mesh and Fig 1.4 shows a single suture loop around the ileo-pectineal ligament. 3 mesh-loops were covered in the single “interrupted” suture, allowing adequate suture/mesh surface interaction. At least a 2-loop safety margin was maintained to the mesh edge. Suture length between ligament and the test frame was the same in all experiments. While suture distortion factored into all results, this effect was the same for all trials and may therefore be omitted.
Statistics
Statistical analysis was performed using the VassarStats® (Vassar College, Poughkeepsie, NY, USA) statistics program. ANOVA analysis and t-tests were used in order to evaluate significances when appropriate.
Ethics Committee Approval
This study was conducted in accordance with institutional review board standard operating procedures. An ethics committee vote was initiated, but deemed unnecessary by the “Ethikkommission der Aerztekammer Nordrhein”. A written statement to this extent is available.
Results
A total of 33 trials was conducted, resulting in four subgroups. A summary of all results is given in Table 1. Due to the complexity of intergroup ANOVA analyses, p values are listed in Figs 2 and 3.
Table 1. This table show overall results for all four evaluated groups.
| Evaluated Entity | Number Tested | Ultimate Load | Displacement at Failure | Stiffness | Calculated Load at 2 mm | Failure Mode |
|---|---|---|---|---|---|---|
| Total Trials = 33 | n | N | mm | N /mm | N | |
| Mesh + Interrupted Suture | 9 | 35 (± 12) | 37 (± 12) | 1,76 (± 0.32) | 3.5 (± 0.6) | Individual loop failure (9/9) |
| Mesh + Continuous Suture | 8 | 48 (± 7) | 36 (± 5) | 2,51 (± 0.53) | 5.0 (± 1.1) | Global mesh failure (8/8) |
| Only Interrupted Suture | 8 | 85 (± 27) | 21 (± 4) | 4,65 (± 1.06) | 9,3 (± 2.1) | Ligament failure (5/8) Suture failure (3/8) |
| Only Continuous Suture | 8 | 74 (± 24) | 28 (± 8) | 2,83 (± 0.46) | 5.6 (± 0.9) | Ligament failure (3/8) Suture failure (5/8) |
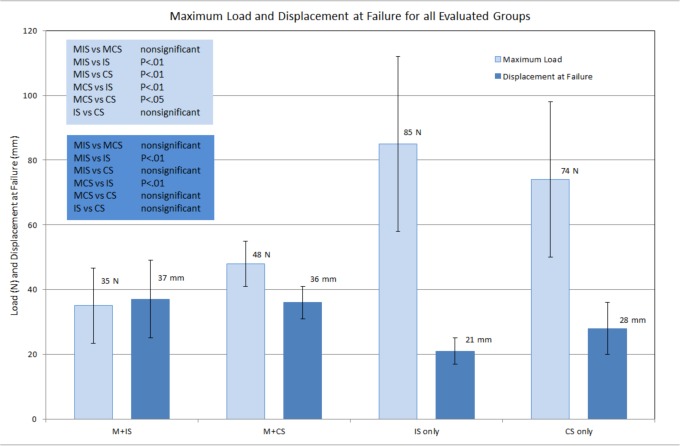
Fig 2. Shown are maximum loads and displacement at failure for all four subgroups.
ANOVA analysis results are shown as well. Error bars represent standard deviations. M+IS = mesh + interrupted (single) suture, M + CS = mesh + continuous suture, IS = interrupted (single) suture, CS = continuous suture.
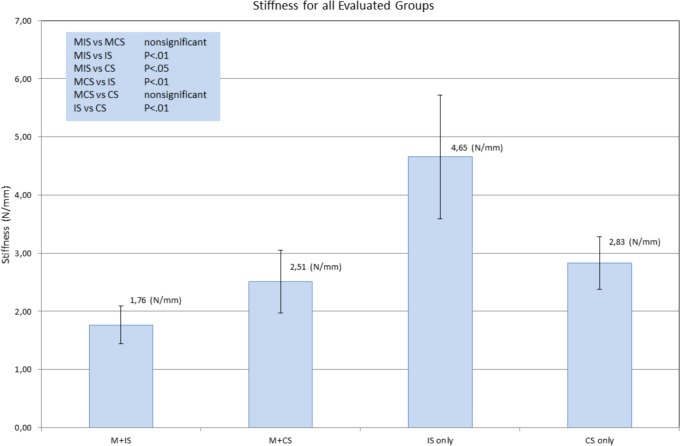
Fig 3. Shown is fixation method stiffness for all four subgroups.
ANOVA analysis results are shown as well. Error bars represent standard deviations. M+IS = mesh + interrupted (single) suture, M + CS = mesh + continuous suture, IS = interrupted (single) suture, CS = continuous suture.
Group 1 represents the hypothesis group with mesh + single “interrupted” suture and group 2 represents the gold standard mesh + continuous suture. Both groups showed the mesh to be the limiting factor. The number of times the sutured was threaded through the surgical mesh was irrelevant. Neither the suture nor the ileo-pectineal ligament failed in all 17 trials (groups 1 and 2). The ultimate load for the MIS group was 35 ± 12 N and 48 ± 7 N for the MCS group. There was no significant difference in the ultimate load between both groups (p> 0.05). The same holds true for displacement at failure which was 37 ± 12 mm (MIS) and 36 ±5 mm (MCS). There is also no significant difference in stiffness between the single suture group and continuous suture group. The only difference wasthe method of failure. The single suture + mesh group resulted in a failure where suture material would cut through an individual loop of the applied mesh. This was not the case for the continuous suture group. The latter showed global mesh deterioration. This, although different, did not result in a significant difference in maximum load, displacement at failure and fixation method stiffness.
Test groups 3 and 4 evaluated the suture techniques on their own. This, representing a control group, resulted in either ligament failure or suture tearing. Having eliminated the limiting factor “mesh”, failure loads were significantly higher 85 ± 27 N for the single “interrupted” suture group and 74 ± 24 N for the continuous suture group. Failure loads without the mesh did not differ significantly between suture methods (see Fig 2), neither did displacement at failure. Interestingly, a significant difference could be shown for fixation method stiffness where the individual suture showed to be significantly stiffer than all tests groups at 4.65 ± 1.06 N/mm (p > 0.01 –for all groups). The failure mode within groups 3 and 4 was either ligament failure or suture failure. Distribution of suture and ligament failure did not differ between single suture and continue suture groups.
Discussion
To our knowledge there has thus far not been any biomechanical analysis performed in this specific area, although some data regarding pelvic ligament strength is available [16]. Overall, our results support the primary hypothesis that a single suture is sufficient in a pectopexy scenario. As shown in Table 1, ultimate load, fixation stiffness and displacement at failure do not differ significantly when comparing the continuous suture application to a single “interrupted” suture. This indicates that a continuous suture method is not superior to a single “interrupted” suture scenario. Alternatively, the use of two single sutures may be considered, but since the limiting factor seems to be the applied surgical mesh an additional single loop may not be beneficial. This is also supported by the failure modes listed in Table 1. We found that single “interrupted” sutures supported loads of up to 85 N. Since, the SERA MESH® PA failed well before this load was achieved we may either opt for a more sturdy mesh or accept the fact that the number and manner of sutures is not important for overall fixation method stability. Additionally, literature has not reported mesh failure in a pectopexy scenario and personal experience shows this not to be a problem in everyday clinical practice. We therefore argue that a single “interrupted” type suture is an adequate option for mesh fixation.
Ultimate load
While it is important to understand that the limiting factor is the applied mesh, other factors regarding ultimate load analysis should also be addressed. A load of 35 N as reported in the MIS situation is considerable. Zimkowski et al. recently reported surgical polyester mesh (PETKM14001, Textile Development Associates) failure at 16.65 ± 3.30N [17] in a semi-physiological setting. Our results maintain the same order of magnitude, thus limited comparability is given. A direct comparison remains difficult since different materials were used. Results are nonetheless similar to those reported in literature and allow us to postulated study comparability to a physiological setting. Furthermore, issues such as immediate postoperative mesh-deformation, known from hernia repair [18], may certainly be prevented by a fixation method allowing for a load of at least 35 N. Since, literature has not reported biomechanical data for this specific method, larger trials may have to be initiated in order to clearly define the biomechanical spectrum for pectopexy.
Displacement at failure
This parameter has been previously investigated in an in vitro situation, in an attempt to reduce surgical time [17,19]. When comparing our data to Zimkowski et al. (control mesh failure at approx. 21.92 ± 3.76 mm) our findings (36–37 mm) agree with literature. From a clinical point of view, a maximum of 37 mm of displacement seems adequate.
Stiffness
The topic of fixation method stiffness is important. This parameter describes the elongation due to force of a given entity. Stiffness, being highly dependent on the trial setup, may not be compared to literature since this reported data is the first of its kind. We found stiffness to be lowest in the mesh groups. Suture methods did not impact this parameter significantly (within the mesh groups). However, a trend favoring the continuous suture may be observed here. The relevance of this fact is not yet known, especially since the “suture only” groups (no mesh) show the opposite to be true.
Calculated Load at 2 mm Displacement
This parameter is directly proportional to the stiffness and serves only as a point of comparison to biomechanical analyses performed in recent literature. A 2 mm displacement is considered initial failure in orthopedics. While soft tissue surgery may allow for more error, the authors felt this value to be worth listing in order to improve inter-publication comparability.
The biomechanical analysis of a single suture versus a continuous suture with and without mesh used in a pectopexy scenario yielded the following results.
What load may be supported by standard (continuous) ileo-pectineal fixation methods? Loads of up to 48 N may be supported by the standard fixation method.
May this load be supported by a single “interrupted” suture? There is no statistically significant difference between continuous and single “interrupted” suture fixation methods. 2 single sutures may improve ligamental fixation, but overall stability does not benefit.
What are the biomechanical properties of the ileo-pectineal mesh /suture fixation? This is the first reported data in this area. Table 1 shows a wide array of biomechanical data on this subject.
What is the limiting factor of said fixation method (mesh, ligament, suture)? All tests lead to the conclusion that the limiting factor is the utilized surgical mesh.
Further Investigation
Despite the obvious need for long term in-vivo testing and the ever present benefit of increased sample size, we feel the need to mention that variability in ligament quality may also play a role in everyday clinical practice and must not be ignored [16].
Conclusion
Given the data above we must conclude that a continuous suture is not necessary in laparoscopic mesh / ileo-pectineal ligament fixation during pectopexy. Ultimate load and displacement at failure results clearly indicate that a single “interrupted” suture is not inferior to a continuous approach. The use of 2 single sutures may improve ligamental fixation. Theoretically, overall stability should not benefit since the surgical mesh remains the limiting factor.
Supporting Information
(XLSX)
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1.Banerjee C, Noe KG (2011) Laparoscopic pectopexy: a new technique of prolapse surgery for obese patients. Arch Gynecol Obstet 284: 631–635. 10.1007/s00404-010-1687-7 [DOI] [PubMed] [Google Scholar]
- 2.Maher C, Baessler K, Glazener CM, Adams EJ, Hagen S (2004) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev: CD004014 [DOI] [PubMed] [Google Scholar]
- 3.Siddiqui NY, Grimes CL, Casiano ER, Abed HT, Jeppson PC, Olivera CK, et al. (2015) Mesh Sacrocolpopexy Compared With Native Tissue Vaginal Repair: A Systematic Review and Meta-analysis. Obstet Gynecol 125: 44–55. 10.1097/AOG.0000000000000570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee RK, Mottrie A, Payne CK, Waltregny D (2014) A review of the current status of laparoscopic and robot-assisted sacrocolpopexy for pelvic organ prolapse. Eur Urol 65: 1128–1137. 10.1016/j.eururo.2013.12.064 [DOI] [PubMed] [Google Scholar]
- 5.Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, et al. (2004) Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol 104: 805–823. [DOI] [PubMed] [Google Scholar]
- 6.Huber SA, Northington GM, Karp DR (2014) Bowel and bladder dysfunction following surgery within the presacral space: an overview of neuroanatomy, function, and dysfunction. Int Urogynecol J. [DOI] [PubMed] [Google Scholar]
- 7.Alkatout I, Mettler L, Peters G, Noe G, Holthaus B, Jonat W, et al. (2014) Laparoscopic hysterectomy and prolapse: a multiprocedural concept. JSLS 18: 89–101. 10.4293/108680813X13693422520846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Noe KG, Schiermeier S, Alkatout I, Anapolski M (2014) Laparoscopic Pectopexy: A Prospective, Randomized, Comparative Clinical Trial of Standard Laparoscopic Sacral Colpocervicopexy with the New Laparoscopic Pectopexy-Postoperative Results and Intermediate-Term Follow-Up in a Pilot Study. J Endourol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noe KG, Spuntrup C, Anapolski M (2013) Laparoscopic pectopexy: a randomised comparative clinical trial of standard laparoscopic sacral colpo-cervicopexy to the new laparoscopic pectopexy. Short-term postoperative results. Arch Gynecol Obstet 287: 275–280. 10.1007/s00404-012-2536-7 [DOI] [PubMed] [Google Scholar]
- 10.Burch JC (1961) Urethrovaginal fixation to Cooper's ligament for correction of stress incontinence, cystocele, and prolapse. Am J Obstet Gynecol 81: 281–290. [DOI] [PubMed] [Google Scholar]
- 11.Thelen S, Betsch M, Schneppendahl J, Grassmann J, Hakimi M, Eichler C, et al. (2013) Fixation of multifragmentary patella fractures using a bilateral fixed-angle plate. Orthopedics 36: e1437–1443. 10.3928/01477447-20131021-29 [DOI] [PubMed] [Google Scholar]
- 12.Thelen S, Schneppendahl J, Baumgartner R, Eichler C, Koebke J, Betsch M, et al. (2013) Cyclic long-term loading of a bilateral fixed-angle plate in comparison with tension band wiring with K-wires or cannulated screws in transverse patella fractures. Knee Surg Sports Traumatol Arthrosc 21: 311–317. 10.1007/s00167-012-1999-1 [DOI] [PubMed] [Google Scholar]
- 13.Thelen S, Schneppendahl J, Jopen E, Eichler C, Koebke J, Schonau E, et al. (2012) Biomechanical cadaver testing of a fixed-angle plate in comparison to tension wiring and screw fixation in transverse patella fractures. Injury 43: 1290–1295. 10.1016/j.injury.2012.04.020 [DOI] [PubMed] [Google Scholar]
- 14.Wild M, Eichler C, Thelen S, Jungbluth P, Windolf J, Hakimi M (2010) Fixed-angle plate osteosynthesis of the patella—an alternative to tension wiring? Clin Biomech (Bristol, Avon) 25: 341–347. [DOI] [PubMed] [Google Scholar]
- 15.Wild M, Thelen S, Jungbluth P, Betsch M, Miersch D, Windolf J, et al. (2011) Fixed-angle plates in patella fractures—a pilot cadaver study. Eur J Med Res 16: 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cosson M, Boukerrou M, Lacaze S, Lambaudie E, Fasel J, Mesdagh H, et al. (2003) A study of pelvic ligament strength. Eur J Obstet Gynecol Reprod Biol 109: 80–87. [DOI] [PubMed] [Google Scholar]
- 17.Zimkowski MM, Rentschler ME, Schoen J, Rech BA, Mandava N, Shandas R (2013) Integrating a novel shape memory polymer into surgical meshes decreases placement time in laparoscopic surgery: an in vitro and acute in vivo study. J Biomed Mater Res A 101: 2613–2620. 10.1002/jbm.a.34556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Endo M, Feola A, Sindhwani N, Manodoro S, Vlacil J, Engels AC, et al. (2014) Mesh contraction: in vivo documentation of changes in apparent surface area utilizing meshes visible on magnetic resonance imaging in the rabbit abdominal wall model. Int Urogynecol J 25: 737–743. 10.1007/s00192-013-2293-6 [DOI] [PubMed] [Google Scholar]
- 19.Zimkowski MM, Rentschler ME, Schoen JA, Mandava N, Shandas R (2014) Biocompatibility and tissue integration of a novel shape memory surgical mesh for ventral hernia: in vivo animal studies. J Biomed Mater Res B Appl Biomater 102: 1093–1100. 10.1002/jbm.b.33091 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.