Abstract
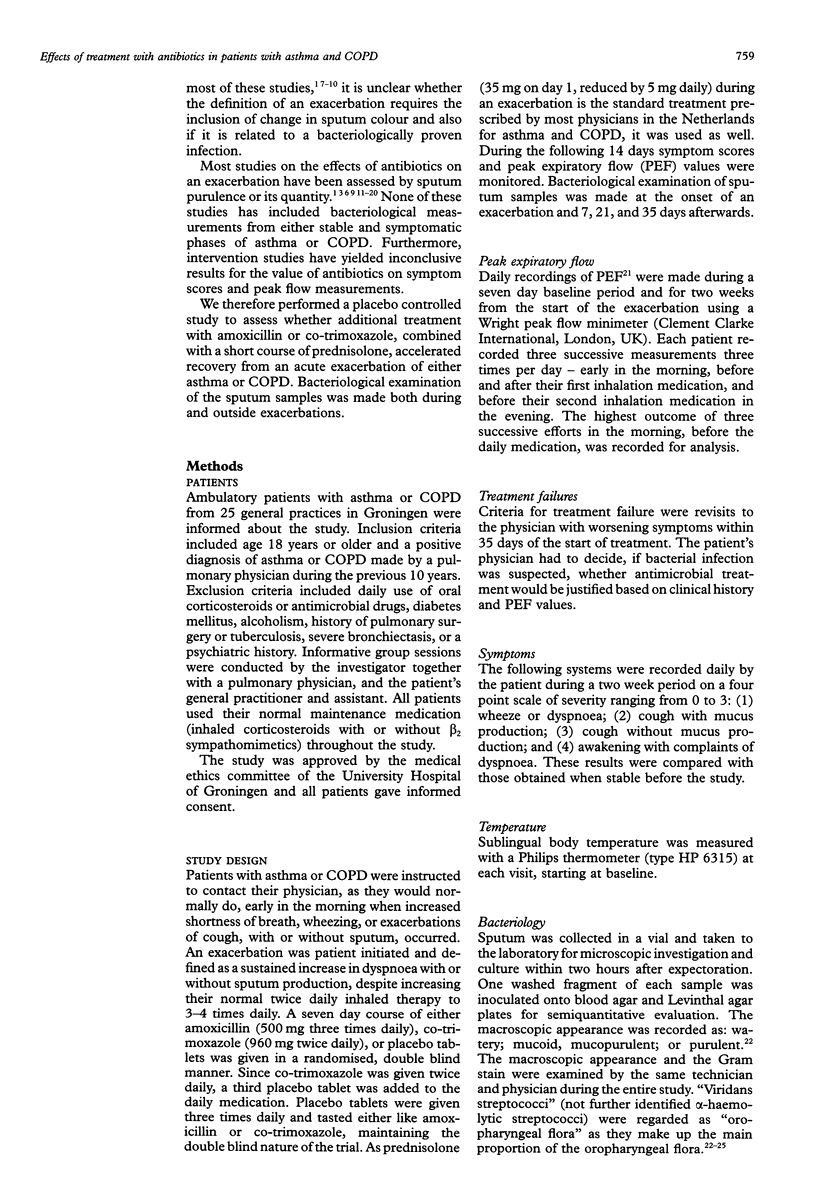
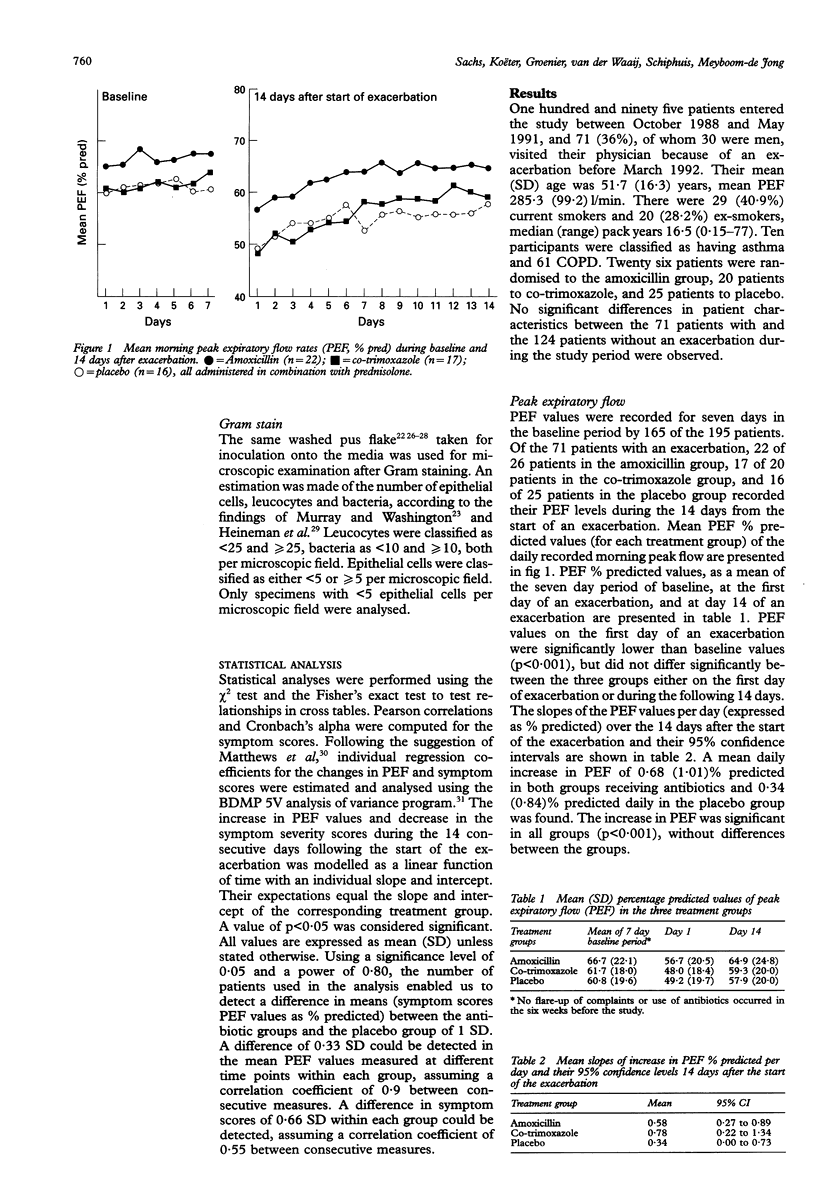
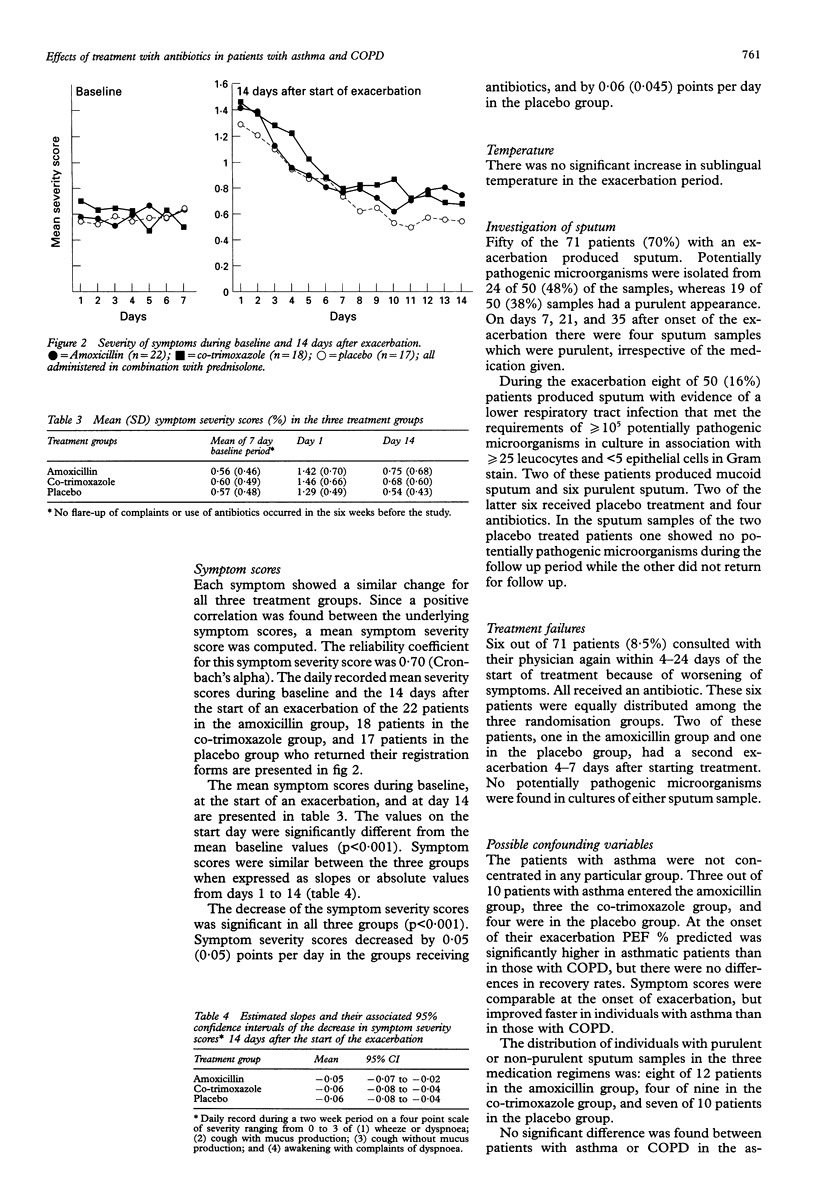
BACKGROUND--Bacterial infections of the lower airways during an exacerbation in patients with asthma or chronic obstructive pulmonary disease (COPD) may be the cause of an exacerbation or the consequence of a viral infection or an increase in airways limitation. To determine whether bacterial infection is an important component in the pathogenesis of an exacerbation, the effects of antimicrobial treatment must be studied. METHODS--Patients with asthma or COPD seen in general practice were studied in a double blind randomised manner to investigate whether the antimicrobial drugs amoxicillin (500 mg three times daily), cotrimoxazole (960 mg twice daily), or a placebo, each when added to a short course of oral corticosteroids, can accelerate recovery from exacerbations. Patients were instructed to contact their own physician early in the morning when complaints of increased shortness of breath, wheezing, or exacerbations of cough with or without sputum production occurred. Treatment effects were evaluated over the next 14 days by studying symptom scores (wheeze, dyspnoea, cough with and without mucus production, and awakening with dyspnoea), peak expiratory flow values (PEF, expressed as % predicted), and sublingual temperature. Bacteriological study of the sputum was made at the onset of an exacerbation and 7, 21 and 35 days afterwards. RESULTS--Of 195 patients enrolled 71 (36%) contacted their physician for symptoms of an exacerbation. Symptoms improved in all three groups, improvements ranging from 0.54 to 0.75 points per day on a four point scale. PEF% predicted showed improvements in the three groups after the exacerbation, ranging from 0.34% to 0.78% predicted per day, finally returning to baseline values. Sublingual temperature did not change. Six of 71 patients consulted their physician because of a relapse between four and 24 days after the start of treatment. In only two of the 50 sputum samples, collected during an exacerbation, and which contained > or = 10(5) bacteria in culture sensitive to the chosen antibiotic given, did any benefit from antimicrobial treatment occur. During the recovery period sputum purulence improved irrespective of antibiotic treatment. CONCLUSIONS--Antibiotics given with a short course of oral prednisolone during an exacerbation do not accelerate recovery as measured by changes in peak flow and symptom scores in ambulatory patients with mild to moderate asthma or COPD when treated by their general practitioners. Moreover, antibiotics do not reduce the number of relapses after treating an exacerbation.
Full text
PDF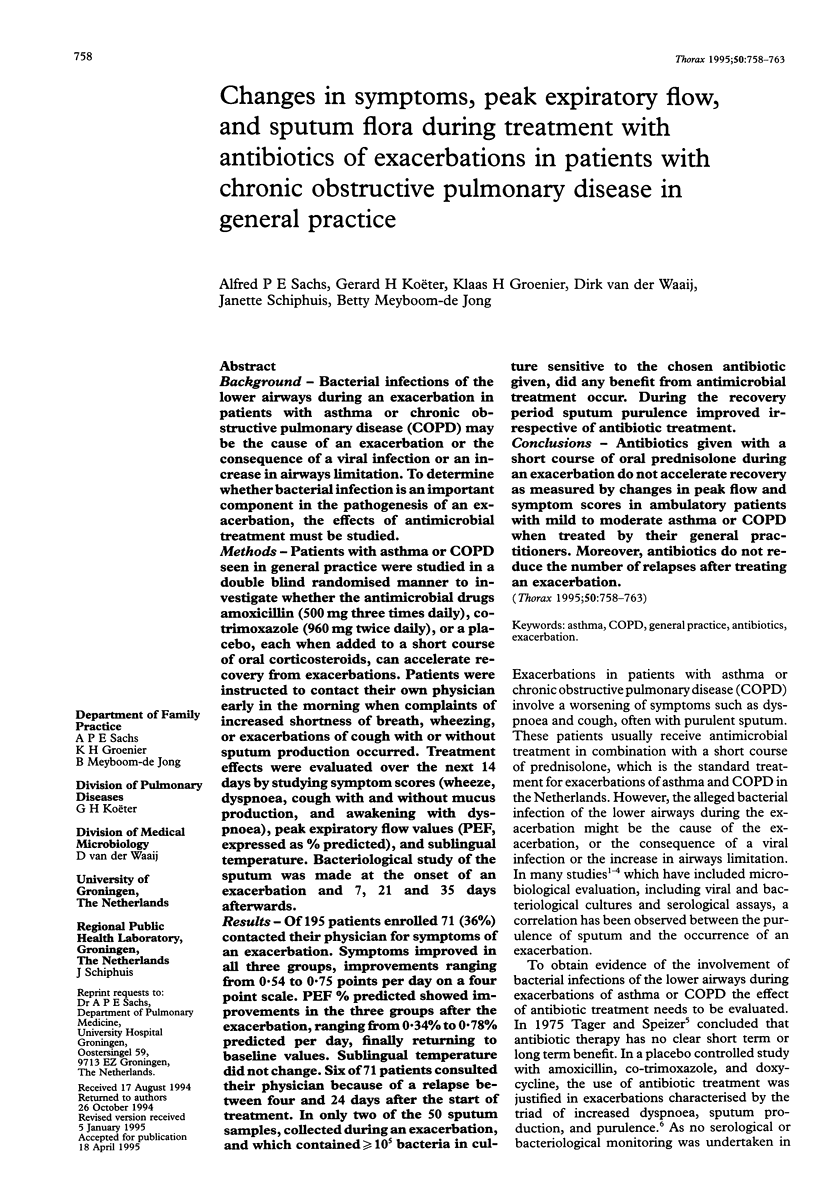

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson G., Jariwalla A. G., Saour J. A comparison of ampicillin and amoxycillin in acute on chronic bronchitis. Thorax. 1979 Dec;34(6):814–816. doi: 10.1136/thx.34.6.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anthonisen N. R., Manfreda J., Warren C. P., Hershfield E. S., Harding G. K., Nelson N. A. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987 Feb;106(2):196–204. doi: 10.7326/0003-4819-106-2-196. [DOI] [PubMed] [Google Scholar]
- BERRY D. G., FRY J., HINDLEY C. P., HODSON J. M., HORDER E. J., HORDER J. P., MARIEN E. A., REA J. N., RYLE A., CURWEN M. P. Exacerbations of chronic bronchitis treatment with oxytetracycline. Lancet. 1960 Jan 16;1(7116):137–139. doi: 10.1016/s0140-6736(60)90056-8. [DOI] [PubMed] [Google Scholar]
- Bartlett J. G., Finegold S. M. Bacteriology of expectorated sputum with quantitative culture and wash technique compared to transtracheal aspirates. Am Rev Respir Dis. 1978 Jun;117(6):1019–1027. doi: 10.1164/arrd.1978.117.6.1019. [DOI] [PubMed] [Google Scholar]
- Basran G. S., Joseph J., Abbas A. M., Hughes C., Tillotson G. S. Treatment of acute exacerbations of chronic obstructive airways disease--a comparison of amoxycillin and ciprofloxacin. J Antimicrob Chemother. 1990 Dec;26 (Suppl F):19–24. doi: 10.1093/jac/26.suppl_f.19. [DOI] [PubMed] [Google Scholar]
- Billas A. Lower respiratory tract infections. Prim Care. 1990 Dec;17(4):811–824. [PubMed] [Google Scholar]
- Chodosh S. Acute bacterial exacerbations in bronchitis and asthma. Am J Med. 1987 Apr 27;82(4A):154–163. [PubMed] [Google Scholar]
- Chodosh S., Eichel B., Ellis C., Medici T. C. Comparison of trimethoprim-sulfamethoxazole with ampicillin in acute infectious exacerbations of chronic bronchitis: a double-blind crossover study. Rev Infect Dis. 1982 Mar-Apr;4(2):517–527. doi: 10.1093/clinids/4.2.517. [DOI] [PubMed] [Google Scholar]
- ELMES P. C., KNOX K., FLETCHER C. M. Sputum in chronic bronchitis; effects of antibiotics. Lancet. 1953 Oct 31;265(6792):903–906. doi: 10.1016/s0140-6736(53)90565-0. [DOI] [PubMed] [Google Scholar]
- Elmes P. C., King T. K., Langlands J. H., Mackay J. A., Wallace W. F., Wade O. L., Wilson T. S. Value of ampicillin in the hospital treatment of exacerbations of chronic bronchitis. Br Med J. 1965 Oct 16;2(5467):904–908. doi: 10.1136/bmj.2.5467.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heineman H. S., Chawla J. K., Lopton W. M. Misinformation from sputum cultures without microscopic examination. J Clin Microbiol. 1977 Nov;6(5):518–527. doi: 10.1128/jcm.6.5.518-527.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway Y., Boersma W. G., Kuttschrütter H., Snijder J. A. Impact of washing sputum on Streptococcus pneumoniae and other microorganisms. J Infect Dis. 1992 Feb;165(2):397–398. doi: 10.1093/infdis/165.2.397. [DOI] [PubMed] [Google Scholar]
- Hudgel D. W., Langston L., Jr, Selner J. C., McIntosh K. Viral and bacterial infections in adults with chronic asthma. Am Rev Respir Dis. 1979 Aug;120(2):393–397. doi: 10.1164/arrd.1979.120.2.393. [DOI] [PubMed] [Google Scholar]
- Hudgel D. W., Langston L., Jr, Selner J. C., McIntosh K. Viral and bacterial infections in adults with chronic asthma. Am Rev Respir Dis. 1979 Aug;120(2):393–397. doi: 10.1164/arrd.1979.120.2.393. [DOI] [PubMed] [Google Scholar]
- Johanson W. G., Jr, Pierce A. K., Sanford J. P., Thomas G. D. Nosocomial respiratory infections with gram-negative bacilli. The significance of colonization of the respiratory tract. Ann Intern Med. 1972 Nov;77(5):701–706. doi: 10.7326/0003-4819-77-5-701. [DOI] [PubMed] [Google Scholar]
- Jordan G. W., Wong G. A., Hoeprich P. D. Bacteriology of the lower respiratory tract as determined by fiber-optic bronchoscopy and transtracheal aspiration. J Infect Dis. 1976 Nov;134(5):428–435. doi: 10.1093/infdis/134.5.428. [DOI] [PubMed] [Google Scholar]
- MULDER J. Bacteriology of bronchitis. Proc R Soc Med. 1956 Oct;49(10):773–776. [PubMed] [Google Scholar]
- Matthews J. N., Altman D. G., Campbell M. J., Royston P. Analysis of serial measurements in medical research. BMJ. 1990 Jan 27;300(6719):230–235. doi: 10.1136/bmj.300.6719.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy T. F., Sethi S. Bacterial infection in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1992 Oct;146(4):1067–1083. doi: 10.1164/ajrccm/146.4.1067. [DOI] [PubMed] [Google Scholar]
- Murray P. R., Washington J. A. Microscopic and baceriologic analysis of expectorated sputum. Mayo Clin Proc. 1975 Jun;50(6):339–344. [PubMed] [Google Scholar]
- Nicotra M. B., Rivera M., Awe R. J. Antibiotic therapy of acute exacerbations of chronic bronchitis. A controlled study using tetracycline. Ann Intern Med. 1982 Jul;97(1):18–21. doi: 10.7326/0003-4819-97-1-18. [DOI] [PubMed] [Google Scholar]
- Nunn A. J., Gregg I. New regression equations for predicting peak expiratory flow in adults. BMJ. 1989 Apr 22;298(6680):1068–1070. doi: 10.1136/bmj.298.6680.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortqvist A., Hammers-Berggren S., Kalin M. Respiratory tract colonization and incidence of secondary infection during hospital treatment of community-acquired pneumonia. Eur J Clin Microbiol Infect Dis. 1990 Oct;9(10):725–731. doi: 10.1007/BF02184684. [DOI] [PubMed] [Google Scholar]
- Pines A., Raafat H., Greenfield J. S., Linsell W. D., Solari M. E. Antibiotic regimens in moderately ill patients with purulent exacerbations of chronic bronchitis. Br J Dis Chest. 1972 Apr;66(2):107–115. [PubMed] [Google Scholar]
- Pines A., Raafat H., Plucinski K., Greenfield J. S., Solari M. Antibiotic regimens in severe and acute purulent exacerbations of chronic bronchitis. Br Med J. 1968 Jun 22;2(5607):735–738. doi: 10.1136/bmj.2.5607.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pines A. Trimethoprim-sulfamethoxazole in the treatment and prevention of purulent exacerbations of chronic bronchitis. J Infect Dis. 1973 Nov;128(Suppl):706–p. doi: 10.1093/infdis/128.supplement_3.s706. [DOI] [PubMed] [Google Scholar]
- Sachs A. P., van der Waaij D., Groenier K. H., Koëter G. H., Schiphuis J. Oropharyngeal flora in asthma and in chronic obstructive pulmonary disease. Indigenous oropharyngeal microorganisms in outpatients with asthma or chronic obstructive pulmonary disease. Am Rev Respir Dis. 1993 Nov;148(5):1302–1307. doi: 10.1164/ajrccm/148.5.1302. [DOI] [PubMed] [Google Scholar]
- Tager I., Speizer F. E. Role of infection in chronic bronchitis. N Engl J Med. 1975 Mar 13;292(11):563–571. doi: 10.1056/NEJM197503132921105. [DOI] [PubMed] [Google Scholar]
- Tillotson J. R., Finland M. Bacterial colonization and clinical superinfection of the respiratory tract complicating antibiotic treatment of pneumonia. J Infect Dis. 1969 Jun;119(6):597–624. doi: 10.1093/infdis/119.6.597. [DOI] [PubMed] [Google Scholar]
- Tomson C. R., Veale D., Gould K. Antibiotic policy and infective exacerbation of obstructive airways disease. Lancet. 1987 Jul 4;2(8549):45–45. doi: 10.1016/s0140-6736(87)93081-9. [DOI] [PubMed] [Google Scholar]



