Abstract
Background
Mal-distribution of health care workers is a global health challenge that exacerbates health disparities, especially in resource-limited settings. Interventions to mitigate the problem have targeted qualified personnel with little focus on medical students. However, studies have demonstrated that rural rotations positively influence students to practice in rural settings upon graduation. To evaluate the influence of peripheral rotations in a resource-limited setting, the Kilimanjaro Christian Medical University College introduced a 12-week clerkship rotation in peripheral hospitals for third-year medical (MD3) students in 2012. We administered an end-of-rotation survey to assess student perceptions, and attitudes toward rural practice after graduation.
Methods
Questionnaires were voluntarily and anonymously administered to MD3 students in April 2014. The questions assessed perceptions of the experience, and attitudes towards rural practice upon graduation. The perceptions were assessed using strength of consensus measures (sCns). The effect of the experience on likelihood for rural practice was assessed using Crude Odds Ratio (COR), and predictors using Adjusted Odds Ratio (AOR) with 95 % Confidence Intervals (CI) tested at a 5 % level of significance. Variation was assessed using Hosmer and Lemeshow test Chi-square.
Results
111 out of 148 MD3 students participated; 62 % were male; 62 % <25 years old; and 72 % matriculated directly from secondary school. Overall, 81 % of MD3 students were satisfied with rural rotations (sCns = 83 %). The likelihood of accepting rural practice deployment after graduation was predicted by satisfaction with the peripheral hospital rotation program (AOR, 4.32; 95 % CI, 1.44–12.96; p, 0.009) and being male (AOR, 2.73; 95 % CI, 1.09–6.84; p, 0.032). Students admitted in medical school after health-related practice trended toward a higher likelihood of accepting rural practice after graduation compared to those enrolled directly from secondary school, although the difference was not significant (AOR, 4.99; 95 % CI, 0.88–28.41; p, 0.070). The Hosmer and Lemeshow test p-value was 0.686, indicating a good fit of the model. No significant differences in satisfaction between these two groups were observed, and also no significant differences between students born in rural areas compared to those born in urban areas existed.
Conclusion
Results indicate that satisfaction with rural rotations is associated with increased likelihood of rural practice after graduation. We conclude that opportunities may exist to reduce mal-distribution of healthcare workers through interventions that target medical students.
Keywords: Peripheral hospital clerkship, Rural practice, Third year medical students
Background
Mal-distribution of health care workers is a global health challenge that exacerbates health disparities [1–3]. This mal-distribution is especially pronounced in resource-limited settings where inequalities in infrastructure between urban and rural areas exist [1, 3]. For example, a country like Tanzania faces high levels of imbalance in physician distribution between rural and urban areas. The numbers of physicians and specialists (consultants) per 10,000 population ratio are estimated at 0.260 and 0.079 respectively [4], which is far below the recommended ratio of 1:5,000 [5]. In 2013, of all registered physicians in Tanzania, 69 % were serving in the urban areas and only 31 % were serving rural populations, where 75 % of Tanzanians resided [6]. These healthcare inequities have significant impact on access and quality of healthcare in areas of great need [7].
Complex and overlapping factors have been related to these disparities in human resources for health. These factors are largely associated with health professional’s personal characteristics and preferences, health systems, and the social, political and economic environments [8]. Poor working conditions (including poor facilities such as equipment and infrastructure, and lack of drugs and supplies), limited future career prospects, and inadequate social amenities have been postulated as factors deterring health workers from choosing and remaining in rural practice [9].
Several interventions have attempted to reduce the urban-rural health workforce imbalances through recruitment and retention of health workers in rural and underserved areas. According to the World Health Organization, such interventions have included increasing the number of students enrolled in medical and allied sciences schools, regulatory policies such as compulsory rural service, monetary incentives or bonuses, access to continuing medical education opportunities, and provision of non-monetary incentives such as preferential selection of students for under- and post-graduate studies from rural areas [8]. However, the results of these interventions and their impact have been modest, including the challenges of sustainability [8]. For example, despite the implementation of most of the above-mentioned interventions, the proportion of practicing physicians in rural Tanzania has remained the same [6, 10–12]. These disparities also still exist despite an almost five-fold increase in the annual medical school enrolment in both public and private universities in Tanzania since 1997 [13]. Despite the increase in enrolment, there has been a dearth of interventions that target medical students to increase the recruitment and retention of these future health care workers into rural areas. Current resources for interventions have largely targeted qualified personnel [14]. Interventions that target medical students may have an effect on future choice of practice location and eventual retention in these areas. Wilson and colleagues found that interventions targeting medical schools could mitigate the rural health workforce shortages [15]. For example, there is evidence that training medical students with rural backgrounds (born and/or brought up in rural areas) and provision of medical training in schools located in rural areas could result in choice of rural medical practice after graduation. [16–21]. Also, another recent study in Australia found that rural background and/or training in a rural medical school predicted uptake of rural medical practice. As such, they found strong interaction between rural background and rural exposure during undergraduate training in predicting future rural medical practice [22]. Some studies have found that personal characteristics of medical students may influence acceptance of positions in rural hospitals. Age of a health professional may affect placement decisions [23]; for example, Leon and Kolstad found that age above 26 years increased the likelihood of accepting job offers in a rural hospital [24]. However, inconclusive findings have been reported on the influence of gender on acceptance of deployment to rural hospitals. For example, Wilkinson et al. [20] found a predominance of male general practitioner doctors in rural areas of Australia, implying increased likelihood of male acceptance of rural practice. Similarly, Kotha reported increased preference of male medical students for rural practice in Ghana [25]. Mehboob et al. did not find significant gender differences on preference for rural medical career in Saudi Arabia [26]. The argument for this difference could partly be explained by differences in family responsibilities between male and female, which differ among countries and among communities in the same country [7].
Most of the medical schools in sub-Saharan Africa, including Tanzania, are located in urban centers and have concentrated their clinical clerkships in tertiary hospitals, where curative and highly specialized medical education is emphasized [27, 28]. Little emphasis has been put on community-based medical education, which has been shown to predict future intention for rural medical practice after graduation [29, 30]. Admission of medical students from rural areas has proved futile due to the fact that most secondary schools in rural areas are ill-equipped with laboratory spaces and lack science teachers to prepare them for admission in medical schools [31]. Furthermore, poor infrastructure in rural areas (lack of electricity, poor roads, poor communication services, and general poverty of rural populations) hampers the establishment of medical schools in rural settings, and as a consequence most medical schools are located in urban centers [32].
Rural clinical placements have been shown to have positive influence on medical student choices for rural practice after graduation. For example, Schoo et al. found that rural placement of Australian medical students during training was associated with starting practice in rural areas after graduation [33]. Also, a case–control study in South Africa demonstrated that rural exposure influenced the choice of practice. However, authors were skeptical about the influence of historical developments specific to South Africa such as apartheid which were not studied [29]. A qualitative study in South Africa [34] demonstrated that the decision of health care professionals for rural practice is enhanced by rural exposure during training, awareness of rural needs and influence of rural role models.
Studies have further reported that rural placements during training must provide a positive experience, which include good supervision and support in order to increase the likelihood of returning to rural areas [35]. Also, Rourke argued that the provision of positive rural learning experiences in medical schools could increase the number of graduating physicians with an interest in rural practice [17]. In a systematic literature review on the effectiveness of preceptors for medical students, the authors found that durations as short as 3 weeks influenced student career choices when preceptors were rated as quality teachers [21, 36]. Specifically, the authors emphasized the role of positive undergraduate experiences with preceptors during rural placements on the uptake of rural practice after medical school [21, 36]. Many of these studies addressing the influence of rural rotations on preferences for rural practice after graduation have been conducted in developed countries (Australia, Canada, and USA) and to some extent in South Africa (a medium-income country), but none have been conducted in a low-income sub-Saharan Africa country.
With the aim of exposing medical students to rural working environments, in 2012 the Kilimanjaro Christian Medical University College (KCMUCo) introduced 12-week peripheral hospital rotations into the junior clerkship curriculum to third-year medical (MD3) students. This was undertaken in part to address congestion during clinical training at the Kilimanjaro Christian Medical Centre (KCMC), and also to expose the students to the rural working environments. Eight hospitals had been carefully selected for this purpose (Table 1) after initial assessment of their appropriateness for training MD3 students during their junior clerkship. The selected hospitals had to demonstrate ability to accommodate students and adequate supervisors for students. Preceptors from these hospitals received adjunct appointments at KCMUCo and specialists from KCMC provided weekly clinics at the hospitals during the rotation period. This intervention was part of a larger project entitled the Medical Education Partnership Initiative (MEPI), which was conducted in collaboration with Duke University School of Medicine (DUSOM) and funded by the United States Government (USG). One of the main goals of the MEPI program was to develop interventions that would enhance retention of health care workers in areas of great need such rural locations. The survey, therefore, aimed to assess the likelihood and the factors that would influence acceptance of rural practice upon graduation among students who underwent short-term peripheral hospital clinical clerkship exposure during medical training.
Table 1.
Peripheral hospital characteristics
| S/N | Health facility name | Number of students | Doctors available | Total | Official bed capacity | Average daily bed occupancy | Average daily OPD attendance | Distance (km) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Specialists | ||||||||||||
| Obs tetrics & gynaecology | Paediatrics | Surgery | Internal medicine | General practitioners | ||||||||
| 1 | Mawenzi regional referral hospital | 15 | 0 | 0 | 0 | 0 | 0 | 0 | 300 | 164 | 97 | 5 |
| 2 | St. Joseph designated district hospital | 7 | 0 | 0 | 1 | 0 | 6 | 7 | 150 | 140 | 200 | 8 |
| 3 | Kibosho designated district hospital | 17 | 0 | 0 | 1 | 0 | 4 | 5 | 180 | 60 | 200 | 10 |
| 4 | St. Elizabeth hospital | 12 | 0 | 0 | 0 | 0 | 4 | 4 | 100 | 87 | 90 | 80 |
| 5 | Mt. Meru regional referral hospital | 27 | 3 | 3 | 3 | 0 | 12 | 18 | 500 | 200 | 180 | 80 |
| 6 | Tanganyika Planting Company (TPC) hospital | 15 | 0 | 0 | 0 | 0 | 1 | 1 | 90 | 65 | 200 | 18 |
| 7 | Same district hospital | 10 | 0 | 0 | 0 | 0 | 4 | 4 | 136 | 70 | 80 | 105 |
| 8 | Gonja hospital | 8 | 0 | 0 | 0 | 0 | 3 | 3 | 67 | 50 | 50 | 165 |
Methods
Study design
Non-experimental.
A cross-sectional survey was administered to students who participated in the peripheral hospital rotation.
Study population and sampling
Study population included all third year medical students at KCMUCo. Since the peripheral hospital junior clerkship rotation is a compulsory curriculum activity, all third year students were eligible to participate in the study. A census was thus employed for students who were willing and available to participate in the survey.
Data collection methods
A self-administered questionnaire was used to collect data from students soon after their return from the peripheral hospital rotation in April 2014. The questions assessed students’ perceptions of the experience, attitudes towards the peripheral hospital rotation and willingness to accept rural practice upon graduation. The perceptions and attitude were assessed using 5-point Likert scale (strongly agree”5” to strongly disagree “1”).
Reliability
Since no standardized and validated questionnaires were available, the team developed a questionnaire that was piloted to 10 fourth year medical students (MD4) who had done the peripheral hospital junior clinical clerkship rotation the previous year and showed high reliability with Cronbach’s Alpha of 0.949.
Ethical issues
Since this survey was part of the monitoring and evaluation activities of the MEPI project, and hence educational, ethical approval was exempted by the Kilimanjaro Christian Medical University College Research Ethics Committee and consent was sought from students before completing the questionnaires after explanation of the purpose and benefits of the survey. Permission for withdrawal from participation in the survey without any penalties was explained to the students. No names appeared on the questionnaires; instead code numbers were used. Thus, the survey was voluntary and anonymous.
Data processing and analysis
Data entry was completed using IBM Statistical Package for Social Sciences (SPSS) version 20.0 computer program. Strength of consensus measure (sCns) was used to measure the strength of agreement/disagreement to statements since it objectively assesses the level of group/team agreement to a construct. A strength of consensus ≥80 % was considered significantly strong. The effect of the peripheral hospital clerkship experience on likelihood for acceptance of rural practice after graduation was assessed using Crude Odds Ratio (COR) with 95 % Confidence Intervals (CI), and tested with a 5 % level of significance. Binary logistic regression analysis was used to determine predictors of accepting rural practice after graduation with Adjusted Odds Ratio (AOR) with 95 % CI, and the Hosmer and Lemeshow Test was used to test goodness-of-fit of the model.
Results
Of 148 MD3 students, 111 (75 %) responded to the survey; 62 % were male, 62 % younger than 25 years and 28 % enrolled after health-related practice in a junior cadre. Figure 1 shows the overall satisfaction of MD3 students with the peripheral hospital rotations. More than 80% of MD3 were either satisfied (61.1 %) or very satisfied (19.4 %) with the peripheral hospital placement. Only 5.5 % of the students were either dissatisfied (4.6 %) or very dissatisfied (0.9 %) with their peripheral hospital placements. The majority of the dissatisfied students had been born or brought up in urban areas, were male, and joined medical school directly from secondary school. All of them were government-sponsored students. About three quarters (74 %) of students enrolled after health-related practice (in-service) had been born or brought up in rural areas as compared to 43 % students enrolled direct after completing secondary education (pre-service) (Fig. 2). In-service students were about 4 times significantly more likely to have been born or brought up in rural areas than pre-service (OR, 3.9; 95 % CI, 1.6–9.7; p, 0.003).
Fig. 1.

Overall satisfaction with peripheral hospital placement program
Fig. 2.
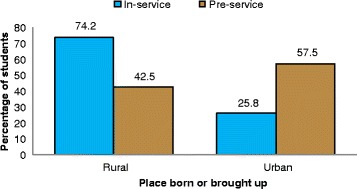
Students’ status at enrolment according to place born or brought up
Further analysis was done using the Strength of Consensus (sCns) measure to assess the aspects for which students were satisfied (Table 2). Overall, 81 % of MD3 students were satisfied with rural rotations (mean sCns = 83 %). Most students had favorable perceptions with significant sCns measures ranging from 83.5 to 86.5 %. A weak strength of consensus measure (74.4 %) was noted only for the statement ‘Easy to practice clinical skills in the peripheral hospital’.
Table 2.
Satisfaction with aspects of peripheral hospital placement
| Satisfaction with clinical practice in a peripheral hospital | n | SA | A | N | Dis | SD | Mean (SDev) | sCns (%) |
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| Easy to practice clinical skills in the peripheral hospital | 110 | 19 (17.3) | 58 (52.7) | 24 (21.8) | 6 (5.5) | 3 (2.7) | 3.8 (0.9) | 74.4 |
| Learnt a lot on clinical clerkship skills in a peripheral hospital | 110 | 40 (36.4) | 57 (51.8) | 9 (8.2) | 2 (1.8) | 2 (1.8) | 4.2 (0.8) | 83.6 |
| Would want to return to practice clinical skills at a peripheral hospital | 110 | 46 (41.8) | 46 (41.8) | 13 (11.8) | 3 (2.7) | 2 (1.8) | 4.2 (0.9) | 83.4 |
| Glad that I had the opportunity to utilize my clinical skills at a peripheral hospital | 110 | 47 (42.7) | 54 (49.1) | 6 (5.5) | 1 (0.9) | 2 (1.8) | 4.3 (0.8) | 85.8 |
| Enjoyed practicing at a peripheral hospital | 110 | 40 (36.4) | 54 (49.1) | 13 (11.8) | 2 (1.8) | 1 (0.9) | 4.2 (0.8) | 83.5 |
| I can now see the importance of basic sciences in my clinical practice | 110 | 50 (45.5) | 50 (45.5) | 7 (6.4) | 2 (1.8) | 1 (0.9) | 4.3 (0.8) | 86.5 |
| Worthwhile teaching clinical practice in a peripheral hospital | 110 | 41 (37.3) | 55 (50.0) | 9 (8.2) | 4 (3.6) | 1 (0.9) | 4.2 (0.8) | 83.6 |
| Mean | 4.2 | 83.0 | ||||||
n number of students, SA Strongly Agree, A Agree, N Neutral/Undecided, Dis Disagree, SD Strongly Disagree, SDev Standard Deviation, sCns Strength of consensus measure
Furthermore, students were asked to indicate their attitudes towards future peripheral hospital placements. Overall, 84 % of students exhibited positive attitudes toward peripheral hospital placements (mean sCns = 80.4 %) (Table 3). Specific attitudes on peripheral hospital placements had sCns ranging from 81.8 to 83 %, with the exception of the statement ‘I am very likely to accept deployment to the rural hospitals after completion of my studies’, which exhibited a weak strength of consensus measure (sCns = 73 %).
Table 3.
Attitudes toward peripheral hospital placement
| Attitude towards peripheral hospital placement | n | SA | A | N | Dis | SD | Mean (SDev) | sCns (%) |
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| I like the idea of peripheral hospital placement | 108 | 29 (26.9) | 67 (62.0) | 8 (7.4) | 2 (1.9) | 2 (1.9) | 4.1 (0.8) | 81.9 |
| I have general favourable attitude towards peripheral hospital placement | 107 | 30 (28.0) | 62 (57.9) | 13 (12.1) | 0 (0.0) | 2 (1.9) | 4.1 (0.8) | 81.9 |
| I believe that it is a good idea to place students in the peripheral hospital in clinical care | 108 | 35 (32.4) | 61 (56.5) | 7 (6.5) | 2 (1.9) | 3 (2.8) | 4.1 (0.8) | 82.4 |
| Peripheral hospital placement is a great idea | 108 | 35 (32.4) | 60 (55.6) | 10 (9.3) | 1 (0.9) | 2 (1.9) | 4.2 (0.8) | 83.0 |
| I am very likely to accept deployment to the rural hospitals after completion of my studies | 108 | 19 (17.6) | 53 (49.1) | 27 (25.0) | 4 (3.7) | 5 (4.6) | 3.7 (1.0) | 73.0 |
| Mean | 4.0 | 80.4 | ||||||
n number of students, SA Strongly Agree, A Agree, N Neutral/Undecided, Dis Disagree, SD Strongly Disagree, SDev Standard Deviation, sCns Strength of consensus measure
Bivariate and multivariate logistic regression analyses of the determinants of acceptance of rural hospital placements after graduation are shown in Table 4. Bivariate analysis of student characteristics and acceptance of deployment to a rural hospital after graduation demonstrated a significantly higher likelihood if the respondent’s gender was male (COR, 3; 95 % CI, 1.3–7.0; p = 0.008), age 25 years or above (COR, 2.8; 95 % CI,1.1–7.0; p,0.024), enrolment after health-related practice (in-service) (COR, 6.2, 95 % CI,1.7–22.3; p, 0.002), born in a rural area (COR, 2.5, 95 % CI,1.1–5.7; p,0.029), and being satisfied with peripheral hospital placement (OR,4.5; 95 % CI,1.7–12.3; p, 0.002).
Table 4.
Students’ characteristics and willingness to accept a job in a rural hospital
| Variable | Total | Acceptance of deployment to a rural hospital | COR (95 % CI) | AOR (95 % CI) | p-value | |
|---|---|---|---|---|---|---|
| Will accept | Will not accept | |||||
| No. (%) | No. (%) | |||||
| Sex: | ||||||
| Male | 67 | 51 (76.1) | 16 (23.9) | 3.0 (1.3–7.0) | 2.7 (1.1–6.8) | 0.032 |
| Female | 41 | 21 (51.2) | 20 (48.8) | 1.0 | 1.0 | |
| Age (years): | ||||||
| 25 or older | 40 | 32 (80.0) | 8 (20.0) | 2.8 (1.1–7.0) | 0.9 (0.2–3.5) | 0.898 |
| Younger than 25 | 68 | 40 (58.8) | 28 (41.2) | 1.0 | 1.0 | |
| Enrolment status: | ||||||
| In-service | 29 | 26 (89.7) | 3 (10.3) | 6.2 (1.7–22.3) | 5.0 (0.9–28.4) | 0.070 |
| Pre-service | 79 | 46 (58.2) | 33 (41.8) | 1.0 | 1.0 | |
| Place of birth and/or upbringing: | ||||||
| Rural | 55 | 42 (76.4) | 13 (23.6) | 2.5 (1.1–5.7) | 1.8 (0.7–4.7) | 0.214 |
| Urban | 53 | 30 (56.6) | 23 (43.4) | 1.0 | 1.0 | |
| Satisfaction with rural placement: | ||||||
| Satisfied | 87 | 64 (73.6) | 23 (26.4) | 4.5 (1.7–12.3) | 4.3 (1.4–13.0) | 0.009 |
| Not satisfied | 21 | 8 (38.1) | 13 (61.9) | 1.0 | 1.0 | |
Multivariate logistic regression revealed that the likelihood of accepting deployment in rural practice after graduation was predicted by being satisfied with the peripheral hospital rotation program (AOR, 4.32; 95 % CI, 1.44–12.96; p, 0.009) and being male (AOR, 2.73; 95 % CI, 1.09–6.84; p, 0.032). Also, enrolment after health-related practice increased the likelihood of accepting rural practice after graduation by 300 % compared to enrolment direct from secondary school, although the difference was not significant (AOR, 4.99; 95 % CI, 0.88–28.41; p, 0.070). The Hosmer and Lemeshow test Chi-square was 3.9 with p-value 0.686, indicating a good fit of the model, that is, our model predicts values not significantly different from what we observed.
Discussion
Interventions aimed at retaining healthcare providers in settings of high need have been focused on qualified individuals, and despite these efforts, there has been minimal effect. There is a dearth of interventions that focus on medical students or those in in-service training. Studies looking at factors that influence acceptance of rural practice post training of medical students have illuminated the need to conduct interventions that will expose students to rural placements. This survey found that, for the MD3 students who responded to our survey, the majority were satisfied with the peripheral hospital rotation with a strong strength of consensus measure. Also, majority of students had positive attitudes toward peripheral hospital placements as indicated by a significant strength of consensus measure. However, weak strength of consensus measures were noted for ease to practice clinical skills at the peripheral hospital, and attitudes towards undertaking rural practice after graduation.
Our study found strong consensus (sCns > 83 %) in gaining clinical clerkship skills after getting an opportunity to utilize these skills at the peripheral hospital. This finding corroborates the observations of Kibore et al. in Kenyan students who reported satisfaction after a 7-week peripheral hospital rotation. Specifically, they felt they had taken an active role in patient care, had improved their clinical skills, and had learned to tackle socio‑cultural challenges in patient care [37]. Other authors elsewhere in the developed world also observe high satisfaction after a rural rotation, due to factors such as seeing a wide variety of patients [38, 39], and thus perceiving their rural experiences as an important component of medical education [40].
A majority of students indicated their willingness to accept deployment in a peripheral (rural) hospital after graduation. Other studies have also shown that peripheral rotations, when well organized and with good clinical and personal support to students, can positively influence students’ attitudes toward rural practice [8, 24, 37]. Though, Couper [41] acknowledges that the influence of stand-alone short-term rural placements on practice choices can be strengthened if integrated by other interventions, evidence suggests that placements as short as 4–6 weeks during training can positively influence rural medical practice choice [42].
Bivariate analysis of the factors influencing student willingness to accept deployment to a rural hospital after graduation demonstrated that age above 25 years, being male, being born or brought up in a rural area, and having worked before joining medical school (in-service) were significant factors that increased the likelihood of accepting deployment to a rural hospital after graduation.
Our survey showed that male medical students were about three times more likely to accept deployment in a rural area than female. There have been mixed results on gender influence for uptake of rural practice. Thus, for example, while in Ghana it was reported that male gender influenced rural practice choice [25], in Saudi Arabia no difference in preference was observed [26]. In the Tanzanian context, the influence of gender on place of practice choice could much depend on family considerations such as place of employment of the husband (if married) or location of parents whereby rural residence of parents increases the probability of choosing to practice in areas nearer the location of parents [27]. Available literature, however, indicates that the determining factor for women’s job mobility is family considerations, while for men it is economic considerations [7].
Leon and Kolstad [24], in their study in Tanzania among fifth year medical students in three medical schools, found that age above 26 years influenced acceptance of employment in rural settings. In our case, this could be explained by the fact that, most of these students are in-service and therefore have experience with rural settings (most of them being middle cadre clinicians who were deployed in lower level health facilities found in rural areas). This observation was further strengthened after binary logistic regression of rural birth and in-service enrolment on acceptance of a job in a rural hospital, whereby in-service enrolment status remained to be a significant predictor. McDonald et al. [43] found that Australian medical graduates with rural origins were about four times likely to undertake rural practice compared to those with an urban place of birth and/or upbringing. Similar evidence has been documented in several studies [23, 27, 29, 44–46]. Comparable results have been reported in Tanzania whereby it was shown that final year medical students in three medical schools who had not spent their childhood in Dar es Salaam (the biggest city in Tanzania) were more likely to accept a job in a district hospital (mostly found in remote/rural areas), although the study could not establish this difference for students with rural birth perse [21]. The inclination of medical students with rural backgrounds to practice in rural areas after graduation could be explained by their familiarity with rural life and cultural norms [46].
Multivariate logistic regression isolated satisfaction with peripheral hospital rotation and male gender as two independent predictors for willingness to accept a job in rural health facilities. In their study in Kenya, Kibore et al. [37] showed that clinical rotations in peripheral, non-tertiary hospitals motivated medical students to accept employment in those hospitals. The same result was reported in a study in Uganda whereby it was shown that the choice to work in rural and underserved areas was greatly influenced by exposure to community-based training experiences [47]. Somers and Spencer [48] demonstrated that upon graduation, students who had exposure to rural rotations had a significantly higher probability of choosing rural practice compared to those who were not and hence a higher probability of choosing rural practice. Wandiraa and Maniple [9] argued that preference for working in rural areas commences and grows during training, and exposure to rural environments during clinical rotations should cement this preference. However, Leon and Kolstad [24] in their study in Tanzania, found that students who underwent community health rotations during medical training were less likely to accept deployment in a rural hospital after graduation. They attributed this to either general dislike of the rural areas due to poor working environment (poor infrastructure, lack/shortage of medical equipment and supplies etc.) or poor organization and/or content of the community rural rotations. Gum argued that poorly organized rural placement can negatively impact students on their willingness to uptake a job in rural areas [49]. Thus, it is important that good educational environment such as comfortable accommodations [50, 51] adequate allowances and internet access [52] is created to influence students to accept a job in a rural setting.
The higher likelihood of in-service students to accept rural practice could be explained by the fact that most of these were admitted at the medical school after practicing at lower cadre for some time (mostly in rurally-located health facilities), although the difference was only a trend and not significant. Their familiarity with working in rural environments could influence their preferences to continue practice in similar environments. The low number of in-service students in our study could explain the insignificant difference.
Strengths and limitations of the study
Strengths
This study attempted to find out if stand-alone short-term placements during medical training could influence future acceptance of rural practice in a resource-limited setting (RLS). Most of the studies on the role of rural exposure during undergraduate medical training in increasing rural medical practice after graduation have been done in high-income countries and very few, if any, in resource-limited settings. Since health workers' mal-distribution is prevalent in RLS, the results of this study are of great importance.
Limitations
Our study relied on self-reported data from students with high reliance on preferences rather than actual practice, which could weaken the strength of our conclusions. While the majority of MD3 students completed the survey, not all students participated, and it is possible that the non-participants might have more negative perceptions of peripheral rotations. Also, the lack of a comparison group could make it difficult to understand how the predictors are influencing preferences. Furthermore, the lack of feedback information from the peripheral hospitals to complement students’ self-reported data coupled with other individual and group effects of the surveyed students also limit the strength of our conclusions. A stronger study designs that incorporates a comparison group could lead to better understanding of our results.
Conclusions
Satisfaction with the rural rotation program was associated with increased likelihood of rural practice after graduation. Opportunities exist in reducing mal-distribution of health care workers through interventions that target health care workers in-training. Institutions of higher learning and other stakeholders involved in human resource for health (HRH) should consider introducing well organized, rural clinical rotations in their medical curricula to increase the likelihood of future rural location placement. Also, recruitment of more in-service students, especially those who have worked in rural areas for at least two years should be considered due to their high propensity to return back to rural areas after graduation.
Way forward
This was a cross-sectional study with its pertinent shortcomings. Follow-up studies that will utilize national and KCMUCo alumni databases will provide a better analysis of the translation of intent to actual practice and retention in rural and/or underserved areas.
Acknowledgements
We thank the third year medical students of Kilimanjaro Christian Medical University College for participating in this survey. We also thank the preceptors/mentors and staff at the peripheral hospitals together with supervisors from Kilimanjaro Christian Medical Centre and Kilimanjaro Christian Medical University College for facilitating the peripheral hospital placement program.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
GK conceived, designed and carried out the statistical analysis of data. The manuscript was also drafted by GK. CM participated in the conception and design of the study and also critically reviewed the draft manuscript. ATK participated in the conception and design of the study. CNT was involved in the design, data collection and coordination of the study. EL was involved conception and design and the proofing and reviewing the draft manuscript. LM participated in the design and coordination of the study. KM participated in the conception, planning and implementation of the study. JAB participated in the conception, design and reviewing the draft manuscript. All authors read and approved the final draft manuscript.
Contributor Information
Gibson Erick Kapanda, Email: nsokolo2005@yahoo.co.uk.
Charles Muiruri, Email: charles.muiruri@duke.edu.
Ahaz T. Kulanga, Email: ahaz47@gmail.com
Chrispina N. Tarimo, Email: cintya086@yahoo.com
Esther Lisasi, Email: estherlisasi@yahoo.co.uk.
Lucy Mimano, Email: lucymimano@gmail.com.
Kien Mteta, Email: akamteta@hotmail.com.
John A. Bartlett, Email: john.bartlett@dm.duke.edu
References
- 1.Does the positive influence of an undergraduate rural placement persist into postgraduate years? Rural and Remote Health. 2012. Available at: http://www.rrh.org.au: Accessed on 03/11/2015. [PubMed]
- 2.WHO. Global health workforce crisis: Key messages - 2013. Available at: http://www.who.int/workforcealliance/media/KeyMessages_3GF.pdf: Accessed on 04/11/2015.
- 3.Smith T. Recruitment/Retention to Improve Rural Service, Desk Review. Arlington: USAID | AIDSTAR-One Project, Task Order 1; 2010. [Google Scholar]
- 4.United Republic of Tanzania (URT) Human resource for health information system and training institution information system and National Population Census. Da.res Salaam: National Bureau of Statistics; 2012. [Google Scholar]
- 5.Makasa E. The Human Resource crisis in the Zambian Health Sector – a discussion paper. Med J Zambia. 2009 [Google Scholar]
- 6.URT . Human resource for health country profile 2012/2013. Dar es Salaam: Ministry of Health and Social Welfare; 2013. [Google Scholar]
- 7.Araújo E. and Maeda A. How to recruit and retain health workers in rural and remote areas in developing countries: A guidance note. Health, Nutrition and Population Family (HNP) 2013; Discussion Paper No. 78506.
- 8.WHO. “Increasing Access to Health Workers in Remote and Rural Areas through Improved Retention: Global Recommendations” 2010. Geneva. [PubMed]
- 9.Wandiraa G, Maniple E. Do Ugandan medical students intend to work in rural health facilities after training? Health Policy Dev. 2009;7(3):203–214. [Google Scholar]
- 10.SADC . Human development report 2000. Harare: SAPES; 2001. [Google Scholar]
- 11.World Bank. World Bank Development Indicators 2002. Washington.
- 12.Khan MM, Hotchkiss DR, Berutti AA, Hutchinson PL. Geographical aspects of poverty and health in Tanzania: Does living in a poor area matter? Partners for health reform plus 2003. Tulane University.
- 13.O’Shea A, Rawls A, Golden E, Cecil R, Slota E, Biezychudek K. Action Now on the Tanzanian Health Workforce Crisis: Expanding Health Worker training-The Twiga initiative 2009. Touch Foundation.
- 14.World Bank. 2011. Reducing geographical imbalances of health workers in sub-Saharan Africa: A labour market perspective on what works, what does not, and why. World Bank 2011. Working Paper No. 209.
- 15.Wilson NW, Bouhuijs PAJ, Conradie HH, Reuter H, Van Heerden BB, Marais B. Perceived educational value and enjoyment of a rural clinical rotation for medical students. Rural Remote Health. 2008;8:999. [PubMed] [Google Scholar]
- 16.Strasser R. Rural health around the world: Challenges and solutions. Fam Pract. 2003;20:457–463. doi: 10.1093/fampra/cmg422. [DOI] [PubMed] [Google Scholar]
- 17.Rourke J. How can medical schools contribute to the education, recruitment and retention of rural physicians in their region? Bull World Health Organ. 2010;88:395–396. doi: 10.2471/BLT.09.073072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skochelak S. A decade of reports calling for change in Medical Education: what do they say? Acad Med. 2010;85(suppl 9):S26–S33. doi: 10.1097/ACM.0b013e3181f1323f. [DOI] [PubMed] [Google Scholar]
- 19.Wilkinson D, Laven G, Pratt N, Beilby J. Impact of undergraduate and postgraduate rural training and medical entry criteria on rural practice among Australian general practitioners: national study of 2414 doctors. Med Educ. 2003;37:809–814. doi: 10.1046/j.1365-2923.2003.01596.x. [DOI] [PubMed] [Google Scholar]
- 20.Wilkinson D. Evidence based rural workforce policy: an enduring challenge. Rural Remote Health. 2003;3:224. [PubMed] [Google Scholar]
- 21.Hsueh W, Wilkinson T, Bills J. What evidence based undergraduate interventions promote rural health. New Zealand Med J. 2004;117(suppl 1204):U1117. [PubMed] [Google Scholar]
- 22.Kondalsamy-Chennakesavan S, Eley DS, Ranmuthugala G, Chater AB, Toombs MR, Darshan D, Nicholson GC. Determinants of rural practice: positive interaction between rural background and rural undergraduate training. MJA. 2015;202(1):41–46. doi: 10.5694/mja14.00236. [DOI] [PubMed] [Google Scholar]
- 23.Lehmann U, Dieleman M, Martineau T. “Staffing Remote Rural Areas in Middle- and Low-Income Countries: A Literature Review of Attraction and Retention.”. BMC Health Serv Res. 2008;8:19. doi: 10.1186/1472-6963-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leon BK, Riise KJ. Wrong schools or wrong students? The potential role of medical education in regional imbalances of the health workforce in the United Republic of Tanzania. Hum Resour Health. 2010;8:3. doi: 10.1186/1478-4491-8-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kotha SR. Lifecourse factors and likelihood of rural practice and emigration: A survey of Ghanaian medical students. Rural Remote Health. 1898;2012(12):1–13. [PubMed] [Google Scholar]
- 26.Mehmood SI, Khan MA, Walsh KM, Borleffs JC. Personality types and specialist choices in medical students. Med Teach. 2013;35(suppl 1):63–68. doi: 10.3109/0142159X.2012.731104. [DOI] [PubMed] [Google Scholar]
- 27.Dussault G, Franceschini MC. “Not Enough There, Too Many Here: Understanding Geographical Imbalances in the Distribution of the Health Workforce.”. Hum Resour Health. 2010;4(suppl 12):1–19. doi: 10.1186/1478-4491-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vanneste A. Recruitment strategies for medical students in primary health care in sub-Saharan Africa. Thesis submitted in fulfillment of a Master Degree in Management of Health Care, 2012.
- 29.Reid SJ, Couper ID, Volmink J. Educational factors that influence the urban-rural distribution of health professionals in South Africa: A case-control study. S Afr Med J. 2011;101(suppl 1):29–33. doi: 10.7196/samj.4342. [DOI] [PubMed] [Google Scholar]
- 30.Rabinowitz HK, Diamond JJ, Markham FW, Rabinowitz C. Long-term retention of graduates from a program to increase the supply of rural family physicians. Acad Med. 2005;80:728–732. doi: 10.1097/00001888-200508000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Komba CK, Hizza EL, Jonathan WTY. Factors influencing academic performance of ward secondary schools: A case of selected schools in Moshi municipality and Moshi district. MUCCoBS, 2013 Working Paper Series No. 1/2013.
- 32.Chen C, Buch E, Wassermann T, Frehywot S, Mullan F, Omaswa F, et al. A survey of sub-Saharan African medical schools. Hum Resour Health. 2012;10:4. doi: 10.1186/1478-4491-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schoo AM, McNamara KP, Stagnitti KE. Clinical placement and rurality of career commencement: a pilot study. Rural Remote Health Res. 2008;8:964. [PubMed] [Google Scholar]
- 34.Couper ID, Hugo JF, Conradie H, Mfenyana K. Influences on the choice of health professionals to practice in rural areas. S Afr Med J. 2007;97:1083–1086. [PubMed] [Google Scholar]
- 35.Katzenellenbogen J, Dury A, Haigh M, Woods J, editors. Critical success factors for recruiting and retaining health professionals to primary health care in rural and remote locations: Contemporary review of the literature. 2013. [Google Scholar]
- 36.Stagg P, Greenhill JA, Worley PS. A new model to understand the career choice and practice location decisions of medical graduates. Rural Remote Health. 2009;9:1245. [PubMed] [Google Scholar]
- 37.Kibore MW, Daniels JA, Child MJ, Nduati R, Njiri FJ, Kinuathia RM, et al. Kenyan medical student and consultant experiences in a pilot decentralized training program at the University of Nairobi. Educ Health. 2014;27(suppl 2):170–176. doi: 10.4103/1357-6283.143778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stearns JA, Stearns MA, Glasser M, Londo RA. Illinois RMED: a comprehensive program to improve the supply of rural family physicians. Fam Med. 2000;32:17–21. [PubMed] [Google Scholar]
- 39.Londo RA, Glasser M. Perspectives on longer community-based preceptorships. Fam Med. 1999;31:13–14. [PubMed] [Google Scholar]
- 40.Mateen FJ. Future practice location and satisfaction with rural medical education. Can Fam Phys. 2006;52:1106–1107. [PMC free article] [PubMed] [Google Scholar]
- 41.Couper I. Short-term rural placements for medical students. WONCA Rural Medical Education Guidebook. Accessed at: www.globalfamilydoctor.com/GetFile.aspx?oid=65652362-27B7.
- 42.Wilson NW, Couper ID, De Vries E, Reid S, Fish T, Marais BJ. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health. 2009;9(2):1060. [PubMed] [Google Scholar]
- 43.McDonald J, Bibby L, Caroll S. Recruiting and retaining general practitioners in rural areas: improving outcomes through evidence based research and community capacity building. Centre for health research and practice. University of Ballarat. 2002.
- 44.Somers GT, Strasser R, Jolly B. What does it take? The influence of rural upbringing and sense of rural background on medical students’ intention to work in a rural environment. Rural Remote Health. 2007;7:706. [PubMed] [Google Scholar]
- 45.Kondalsamy-Chennakesavan S, Eley DS, Ranmuthugala G, Chater AB, Toombs MR, Darshan D, Nicholson GC. Determinants of rural practice: positive interaction between rural background and rural undergraduate training. Med J Aust. 2015;202(suppl 1):41–45. doi: 10.5694/mja14.00236. [DOI] [PubMed] [Google Scholar]
- 46.Deressa W, Azazh A. Attitudes of undergraduate medical students of Addis Ababa University towards medical practice and migration, Ethiopia. BMC Med Educ. 2012;12:68. doi: 10.1186/1472-6920-12-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kaye DK, Mwanika A, Sewankambo N. Influence of the training experience of Makerere University medical and nursing graduates on willingness and competence to work in rural health facilities. 2010. [PubMed] [Google Scholar]
- 48.Somers GT, Spencer RJ. Nature or nurture: The effect of undergraduate rural clinical rotations on pre-existent rural career choice likelihood as measured by the SOMERS Index. Aust J Rural Health. 2012;20:80–87. doi: 10.1111/j.1440-1584.2012.01258.x. [DOI] [PubMed] [Google Scholar]
- 49.Gum LF. Studying nursing in a rural setting: Are students adequately supported and prepared for rural practice? A pilot study. Rural Remote Health. 2007;7(suppl1):628. [PubMed] [Google Scholar]
- 50.Page S, Birden H. Twelve tips on rural medical placements: What has worked to make them successful. Med Teach. 2008;30(suppl 6):592–6. doi: 10.1080/01421590801965129. [DOI] [PubMed] [Google Scholar]
- 51.Gupta TK, Murray RB, Beaton NS, Farlow DJ, Jukka CB, Coventry NL. A tale of three hospitals: Solving learning and workforce needs together. Med J Aust. 2009;191(suppl 2):105–109. doi: 10.5694/j.1326-5377.2009.tb02705.x. [DOI] [PubMed] [Google Scholar]
- 52.Deaville JA, Wynn-Jones J, Hays RB, Coventry PJ, McKinley RK, Randall-Smith J. Perceptions of UK medical students on rural clinical placements. Rural Remote Health. 2009;9(suppl 2):1165. [PubMed] [Google Scholar]


