Abstract
The World Health Organization's International Classification of Functioning, Disability and Health (ICF) provides an ideal framework within which to conceptualize grading and quantification of upper extremity function for children with spasticity. In this article the authors provide an overview of assessments and classification tools used to (1) understand upper extremity function associated with spasticity and the factors that contribute to dysfunction, (2) guide the selection of appropriate interventions, (3) identify specific muscles to target using surgical interventions and botulinum toxin-A injections, and (4) measure the outcomes of upper extremity interventions. Assessments of upper extremity function are briefly described and categorized as to whether they (1) measure children's best ability or actual performance in daily life, (2) are clinician administered or are a child/proxy report, (3) assist in planning intervention and/or measuring outcomes, and (4) evaluate unimanual or bimanual ability. In addition, measures of spasticity and hypertonicity, and classifications of static and dynamic upper extremity postures are summarized.
Keywords: spasticity, measurement, upper extremity, cerebral palsy, intervention
Pediatric rehabilitation has embraced the World Health Organization's International Classification of Functioning, Disability and Health (ICF)1 as a framework for understanding the complex lives of children with disabilities. The ICF defines children's function and disability as multidimensional concepts that are founded on three domains: children's body function and structure, ability to complete everyday tasks (activity), and engagement in broader life situations (participation). The ICF also posits that children's functional ability is interrelated with facilitators and barriers posed by their own personal characteristics, and the social and physical environments in which they live. Assessments and interventions can be broadly classified as pertaining to the three levels of the ICF. Upper extremity assessments tend to be either body function or activity-level measures. Likewise, interventions for the upper extremity tend to be classified as aiming to achieve either improvements in body function or activity-level outcomes. Examples of body function interventions for children presenting with upper extremity spasticity are botulinum toxin A (BoNT-A) injections, surgery, strengthening programs, orthoses, and casting. The therapeutic intent of these interventions is to alter body function characteristics such as muscle stiffness, length, balance, and strength. Frequently, these interventions are intended to impact on other outcomes such as pain and ease of caregiving. There is little evidence2 to suggest, however, that altering body function, such as spasticity, improves functioning at other levels of the ICF, for example, at the activity level. Exceptions exist when body function interventions are combined with an activity level intervention such as bimanual upper extremity occupational therapy or constraint-induced movement therapy.3 4
Activity-level assessments of upper extremity function focus on children's ability to grasp, release, and manipulate objects; and the ability to use the upper extremity for completing self-care and other daily living tasks. These assessments can be further categorized as measuring capacity or performance. Capacity refers to a child's best ability, generally measured in a clinic environment. Performance measures ascertain how children use their upper extremities in naturalistic, everyday activities.5 Additional subcategories of assessments are self- or proxy report versus therapist-observed measures, and measures that are considered individualized. Individualized assessments are those where a child and family identify particular goals for intervention and outcome is quantified by degree of attainment of these goals. Examples of individualized goals are tying shoelaces or catching a ball.
A family-focused approach to upper extremity intervention demands that desired outcomes of an intervention are collaboratively identified with children and their families. Surgery for a child presenting with profoundly significant spasticity may be to reduce pain, enable maintenance of hygiene in the upper extremity, and allow a program of casting or orthoses to be initiated to maintain range of motion (ROM). These are the three outcomes that should be measured before and after surgery. A child with hemiplegia and moderate spasticity of the elbow, wrist, and finger flexors may present for BoNT-A injections to enable him or her to push the more affected arm through a sleeve independently and to stabilize a page when handwriting at school. These are the activity-level outcomes that are measured to inform the degree of success of the injections. Measurements of ROM and spasticity, for instance, are useful to guide these interventions and to inform the overall outcome, but are not the outcomes of interest.
Understanding Spasticity as a Basis for Assessment
Spasticity is the result of upper motor neuron lesions and presents as a velocity-dependent increase in the muscle's response to passive stretch. Spasticity is one of the three subtypes of neurologically mediated hypertonia, along with dystonia and rigidity.2 6 Spasticity frequently coexists with dystonia. Other more difficult-to-quantify features such as muscle weakness, poor selective motor control, ataxia, and apraxia7 are also considered to significantly impact on function.
Spasticity is observed in several pediatric neurologic conditions, most commonly in cerebral palsy (CP), but also in acquired and traumatic brain injury, spinal cord injury, and different hereditary and progressive conditions. The majority of the forthcoming discussion relates to children with CP; most of the literature regarding grading and quantification of upper extremity function in children is in this area.
Measures Used to Grade and Quantify Upper Extremity Function of Children with Spasticity
For the purposes of this discussion, upper extremity function is defined as children's ability to reach, grasp, and manipulate objects and/or to use the upper extremity to complete daily activities either in a contrived clinical situation (capacity) or in everyday activity (usual performance).
The following is an approach to quantification of upper extremity function, which is illustrated in Fig. 1.
Fig. 1.
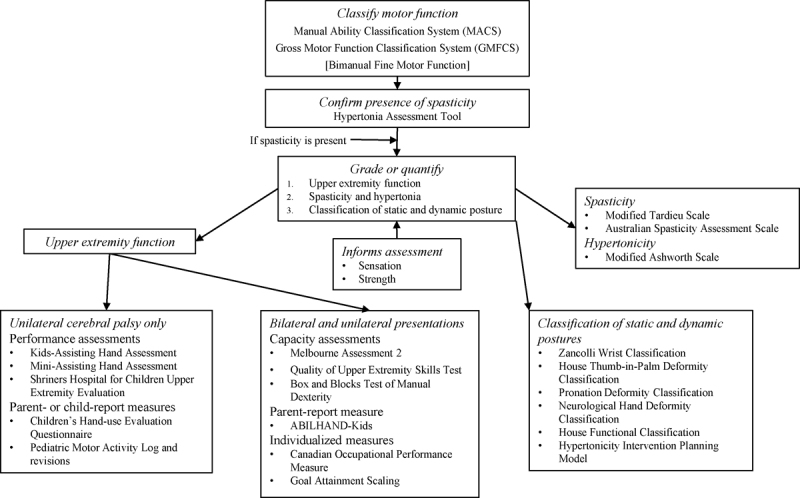
Measures for grading and quantifying upper extremity function in children with spasticity.
Classification of Gross Motor and Manual Ability
Classification systems provide a snapshot of a child's functional levels of motor ability and a common language across families, clinicians, and researchers, and they are a useful preliminary step in understanding function.
The Manual Ability Classification System (MACS),8 Bimanual Fine Motor Function (BFMF),9 10 and Gross Motor Functional Classification System (GMFCS)11 form part of a suite of tools to classify motor function in children with CP. The other main classification tool is the Communication Function Classification System (CFCS).12 The MACS, BFMF, CFCS, and GMFCS classify function on a 5-level scale, where level I is well functioning and level V equates to significant disability. The MACS8 was developed to classify the usual ability of children with CP aged 4 to 18 years to use their hands to handle objects in everyday life. The Mini-MACS for children 1 to 4 years is under development. The MACS is readily available at http://www.macs.nu/. The BFMF is not as universally used as the MACS, and has undergone less investigation of its psychometric properties.
Confirming the Presence of Spasticity
Following classification of motor ability, the next step, if not already completed, is to differentiate between the three neurologically mediated subtypes of hypertonia: spasticity, dystonia, and rigidity. The Hypertonia Assessment Tool13 (http://research.hollandbloorview.ca/Outcomemeasures/HAT) is a 7-item tool developed for children and adolescents with CP between the ages of 4 to 19 years. It can discriminate spasticity, dystonia, rigidity, or mixed presentations in both the upper and lower extremities. This is necessary to guide selection of appropriate grading and quantification measures and interventions. Implementation of some types of interventions is contraindicated with children with spasticity and coexisting dyskinesias such as dystonia.
Selection of Appropriate Grading and Quantification Tools
Fig. 1 is a schematic diagram of the various measures used to grade and quantify upper extremity function in children with spasticity. The choice of measures is influenced by one or more of the following factors:
The child's characteristics: Specific characteristics associated with the child such as age, type of diagnosis (e.g., traumatic brain injury or CP), severity of motor function, and intellectual and functional impairments will guide whether it is appropriate for a child to complete particular assessments.
Requirements of the measurement tool: Some tools have been developed and validated for particular ages and diagnoses, whereas others are more universal. ABILHAND-Kids,14 for instance, has been validated for children aged 6 to 15 years with unilateral or bilateral CP of all levels of severity. The Mini-Assisting Hand Assessment15 is suitable only for 8- to 18-month-old infants with unilateral (hemiplegic) CP.
Intervention considerations: Some assessments may be used to guide intervention. The Shriners Hospital for Children Upper Extremity Evaluation,16 for example, guides decision-making regarding the selection and focus of interventions. The House Thumb-in-Palm Deformity Classification17 assists in identifying muscles to target with BoNT-A and surgical interventions. Other assessments are selected for their suitability to measure the outcome of a proposed intervention. The Melbourne Assessment 230 can measure the effects of an intervention intended to improve quality of upper extremity movement, but is not generally useful for guiding intervention. The Kids-Assisting Hand Assessment18 is a valuable tool for both planning and measuring the outcome of intervention. However, classification tools for static and active postures, such as the Zancolli Wrist Classification,19 would not be appropriate to measure the outcomes of an activity-based intervention such as intensive bimanual occupational therapy.
The goals for intervention: Goals are developed in collaboration with children and their families, and often include domains or activities that are not included in a standard assessment. The Canadian Occupational Performance Measure20 or Goal Attainment Scaling21 22 are used to measure the effects of an intervention on an individually negotiated specific outcome. For instance, the quantification of progress toward the ability to catch a ball or to use cutlery is best achieved with one of these measures.
Clinical utility: The selection of a measure may be dictated by its availability, education required to be certified in its use, cost of the assessment, and time taken to complete, score, and interpret results. The Mini-Assisting Hand Assessment (Mini-AHA),15 for instance, requires education and certification, and a minimum of 40 minutes to administer, score, and interpret. A parent-report measure may be more efficient when time and financial constraints preclude the use of a more intensive observational assessment.
Psychometric properties: Preferred measures are those that have been rigorously developed for the purpose for which they are used, and have adequate reliability and validity. These properties enable accurate classification and therefore confident decisions regarding intervention selection. Tools measuring the outcomes of intervention should also possess sensitivity to change to ensure accurate quantification of response to intervention. An additional consideration in interpreting change following intervention is whether the magnitude of the change represents a clinically important difference from preintervention. Psychometric details of the tools reported on here are not discussed, but can be obtained elsewhere.5 23
Measures of Upper Extremity Function
The following descriptions of upper extremity function measures are expanded on in Table 1. The majority of these assessments will also provide a clinician with the opportunity to observe the presence, nature, and timing of children's voluntary motor control and active ROM during voluntary movement.
Table 1. Measures of upper extremity function.
| Assessment | Age | Reasons for use | Measures | ICF domain | Diagnostic group | Mode of administration | Unilateral or bimanual |
|---|---|---|---|---|---|---|---|
| Kids-Assisting Hand Assessment18 | Small Kids AHA: 18 mo–5 y School-Kids AHA: 6–12 y |
Planning intervention Measuring outcome |
Performance | Activity | Unilateral cerebral palsy Obstetric brachial plexus palsy |
Clinician administered Scored from video of 15-min semistructured play session Clinician accreditation required |
Bimanual |
| Mini-Assisting Hand Assessment15 | 8–18 mo | Planning intervention Measuring outcome |
Performance | Activity | Clinical signs of unilateral cerebral palsy | Clinician administered Scored from video of 15-min semistructured play session Clinician accreditation required |
Bimanual |
| Shriners Hospital for Children Upper Extremity Evaluation16 | 3–18 y | Planning intervention Measuring outcome |
Performance | Activity and body function and structure | Unilateral cerebral palsy | Clinician administered Scored from video Training package available |
Unilateral |
| Children's Hand-use Evaluation Questionnaire25 | 6–18 y | Describing upper extremity ability May measure outcome after further research of psychometric properties |
Performance | Activity | Unilateral cerebral palsy | Parent or child report if over 12 y | Bimanual activities to understand the function of the more affected hand |
| Pediatric Motor Activity Log (and revisions)26 27 28 | 7 mo–8 y depending on version | Measuring unilateral upper extremity outcome | Performance | Body function and structure | Unilateral cerebral palsy | Parent-report Self or clinician administered depending on version used Training package available |
Unilateral |
| Melbourne Assessment 230 | 2 y 6 mo–5 y | Measuring outcome | Capacity | Activity ± body function | All neurologic conditions | Clinician administered Training package available |
Unilateral, both extremities can be evaluated separately |
| Quality of Upper Extremity Skills Test31 | 18 m–8 y but used with older children | Measuring outcome | Capacity | Activity ± body function | Spastic cerebral palsy | Clinician administered Test manual available |
Unilateral function, both arms can be tested Measures quality not function |
| Box and Blocks Test of Manual Dexterity33 | 6–19 y | Measuring outcome | Capacity | Activity ± body function | Any diagnosis | Clinician administered | Unilateral |
| ABILHAND-Kids14 | 6–15 y | Measuring outcome | Performance | Activity | All topographies of cerebral palsy | Parent-report Available on website |
Mostly bilateral |
| Canadian Occupational Performance Measure20 | Any age | Planning intervention Measuring outcome |
Performance | Activity | Any diagnosis | Parent-report or chid self-report if aged over 8 y Training package available |
Individualized |
| Goal Attainment Scaling21 | Any age | Planning intervention Measuring outcome |
Performance | Activity | Any diagnosis | Clinician and child/family collaboratively | Individualized |
Abbreviations: ICF, World Health Organization's International Classification of Functioning, Disability and Health.
Assessment of Performance (Usual Ability) of Children with Unilateral Spastic Cerebral Palsy
Kids-Assisting Hand Assessment and Mini-Assisting Hand Assessment
The Kids-Assisting Hand Assessment (Kids-AHA) measures and describes the effectiveness with which a child who has unilateral CP or obstetric brachial plexus palsy makes use of his or her affected hand (assisting hand) during bimanual activities.18 The Kids-AHA is a Rasch-modeled, standardized, criterion-referenced test that is valid and reliable. In addition to being particularly useful for targeting activity-level interventions, it is sensitive to change and therefore an effective outcome measure. There are two versions: a Small Kids AHA for children aged 18 months to 5 years, and the School Kids AHA for children aged 6 years to 12 years.
The Mini-AHA is similar to the Kids-AHA, but was developed specifically for infants aged 8 months to 18 months with clinical signs of unilateral CP.15 Two additional assessments that are currently under development but will contribute to assessment of upper extremity function of infants at risk of unilateral CP are the Hand Assessment for Infants and the Grasping and Reaching Assessment of Brisbane.24
Shriners Hospital for Children Upper Extremity Evaluation
The Shriners Hospital for Children Upper Extremity Evaluation (SHUEE)16 was developed to assist in targeting and measuring the outcome of spasticity and surgical management. Children are video recorded completing several tasks. The domains assessed include spontaneous functional upper extremity use during simple tasks, and analysis of the alignment of upper extremity anatomical segments and of grasp and release.
Parent- or Child-Report Measures of Upper Extremity Use in Everyday Activity (Performance) for Children with Unilateral Cerebral Palsy
Children's Hand-use Experience Questionnaire
The Children's Hand-use Experience Questionnaire (CHEQ)25 is a questionnaire developed for children aged between 6 and 17 years with unilateral functional limitations, for example, unilateral CP. This parent- or child-report questionnaire evaluates and describes the experience of children using their more affected hand during bilateral activities. Respondents specify whether they are independent in 29 activities typically requiring the use of two hands, such as putting on socks, buttoning trousers, and cutting out a picture using scissors. If an activity is independently completed, four further questions are asked: (1) whether one or two hands are used; and ratings on a 4-point scale regarding (2) effectiveness of grasp, (3) time required in comparison to peers, and (4) the experience of feeling bothered while doing the activity. The questionnaire and information about the CHEQ can be accessed online at http://www.cheq.se/.
Pediatric Motor Activity Log
The Pediatric Motor Activity Log (PMAL) has an original version26 and two different and independent revisions.27 28 Everyday, mainly unilateral tasks are rated by parents on two scales exploring the amount and the quality of upper extremity use. Careful attention is required before using and reporting PMAL, as each version differs in terms of administration, number and nature of items, rating scale, and psychometrics.5 29
Upper Extremity Capacity (Best Ability) for Children with Unilateral or Bilateral Presentations
Each of these measures evaluates the function of one extremity only (unimanual ability), but both upper extremities can be tested independently.
Melbourne Assessment 2
The Melbourne Assessment 2 (MA2)30 is a criterion-referenced measure to evaluate change in quality of unilateral upper extremity function for children with neurologic impairment. Children are video recorded completing 14 unilateral tasks that are later scored on 30 items. The items cover four separate domains: ROM; accuracy of reach and pointing; dexterity of reach, grasp, and manipulation; and fluency of movement.
Quality of Upper Extremity Skills Test
The Quality of Upper Extremity Skills Test (QUEST)31 is a standardized, criterion-referenced assessment that evaluates the quality of upper extremity function in the domains of dissociated movement, grasp, protective extension, and weight bearing. It is used with children with spasticity aged 18 months to 12 years. The assessment focuses on patterns of movement that form the basis of developmental upper extremity performance.
Box and Blocks Test of Manual Dexterity
The Box and Blocks Test of Manual Dexterity (BBT) is a measure of unilateral gross manual dexterity for use with children of any diagnosis. Children are asked to move as many 1-inch blocks as they can from one side of a box over the top of a barrier to the other side of the box in 1 minute.32 33
Parent-Report Measure of Bimanual Ability for Children with Unilateral or Bilateral Cerebral Palsy
ABILHAND-Kids
ABILHAND-Kids14 is a Rasch-developed measure of manual ability during completion of daily activities requiring the use of the upper extremities. Parents rate 21 items according to the difficulty they perceive their child to experience in performing each activity. Items include buttoning trousers and a shirt/sweater, opening the cap of a toothpaste tube, sharpening a pencil, and unwrapping a chocolate bar. ABILHAND-Kids is accessible at http://www.rehab-scales.org/abilhand-kids.html; the site includes the capacity to enter scores and generate Rasch-derived logits for analysis.
Individualized Outcome Measures for Any Child Presenting with Upper Extremity Spasticity
The following two measures are among the most commonly used to identify and measure progress on individualized goals and are intended to foster collaborative goal setting with families.
Canadian Occupational Performance Measure
The Canadian Occupational Performance Measure (COPM)20 is an individualized measure used to identify problems experienced by children in self-care (e.g., dressing, eating), school/preschool, and leisure activities. A semistructured interview is used with families or children, if older than 8 years, to elicit and then prioritize the problem areas. Up to five of these areas are then rated by families on a scale to identify their perception of the child's current level of performance and the family's satisfaction with that performance. Outcome is measured by re-rating these scales after intervention.
Goal Attainment Scaling
To complete Goal Attainment Scaling, children and families identify up to five goals for intervention. These are then scaled, most commonly using a 5-point (−2 to +2) scale. The baseline, current level of performance is allocated −2 and the desired performance on the goal is given a zero. An intermediary goal is ascribed −1, and two better-than-expected goals are given +1 and +2, respectively. Progress toward attainment of the desired goal can then be monitored and evaluated quantitatively.
Grading Upper Extremity Spasticity and Classifying Static and Dynamic Wrist/Hand Postures
Spasticity and Hypertonicity Scales
Intervention offered to children with upper extremity spasticity will vary depending on the severity of spasticity, its impact on upper extremity function, and the available active and passive ROM. Joint ROM is often restricted in children with spasticity by hypertonia and muscle and/or bony contracture, and can impact on function. The most common clinical measures of spasticity and hypertonicity follow.
Modified Tardieu Scales
The Modified Tardieu Scale (MTS)34 35 quantifies severity of muscle spasticity and guides decision-making about the potential effectiveness of spasticity management. Two measures are taken. The first is maximum passive ROM of the target muscle group, referred to as R2. The second measure, R1, is elicited by moving the target muscle group from its shortest to longest position using a rapid velocity stretch. R1, is the angle at which muscle resistance or “catch” is felt in response to the stretch. Both these angles are measured with a goniometer. A catch early in the available range indicates more significant spasticity than a catch toward the end of the ROM. The relationship between R1 and R2, calculated as R2 minus R1, is important and indicates the dynamic component of spasticity. A large R2 - R1 difference implies potential for effective spasticity management.
Australian Spasticity Assessment Scale
The Australian Spasticity Assessment Scale (ASAS),36 a clinical measure of spasticity for people with CP, was developed to provide unambiguous, mutually exclusive criteria for grading spasticity. Like the MTS, a muscle group is subjected to a rapid passive stretch. A 5-point scale grades the absence of a catch, or if a catch is present whether the catch occurs in the first or second half of the available ROM, and any resistance felt throughout the remaining ROM. Details of reliability and validity of the ASAS in children have yet to be published.
Modified Ashworth Scale
The Modified Ashworth Scale (MAS)37 measures hypertonicity: the resistance of the muscle to passive movement. The target muscle group is moved through its ROM over a period of 1 second. Muscle response is graded on a 6-point scale that describes muscle resistance, the presence or absence of a catch, and the ease with which the joint is able to be moved through the available ROM. Reliability of the MAS for the upper extremity is adequate.38 39
Classification of Static and Dynamic Posture
Active movement of the wrist and hand presents a complex interaction of intrinsic and extrinsic musculature. An imbalance of muscle activity dictates the pattern of active and static thumb, wrist, hand, and forearm deformity.40 Scales that classify the consistent patterns of deformity of the hand observed in clinical practice and that result from spasticity have been developed. Most of these scales facilitate analysis of the anatomical and biomechanical components of neurologically based wrist and hand deformity to assist in identifying the primary muscles that are contributing to deformity and causing the dynamic presentation of the deformity during approach, grasp, and release of an object. Consequently, the scales guide surgery, interventions such as orthoses and casting, and assist in targeting muscles for BoNT-A injections.
Zancolli Wrist Classification
The Zancolli Wrist Classification19 categorizes the most commonly observed wrist and hand deformities of children with spastic CP and the relative contributions of intrinsic and extrinsic muscles to hand deformity and function.
House Thumb-in-Palm Deformity Classification
The House Thumb-in-Palm Deformity Classification17 is a tool that classifies the static and dynamic components of four commonly observed thumb deformities and the contributing balance of intrinsic and extrinsic muscle spasticity.
Pronation Deformity Classification
Four groups of pronation deformities are described, based on relative availability of active and passive supination.41 Each group is linked to recommendations for surgery to alter active supination.
The Neurological Hand Deformity Classification
Building on existing classification scales, the Neurological Hand Deformity Classification (NHDC) classifies hand deformity in children and adults with neurologically based upper extremity impairment.42 The NHDC allows classification of hands with no active movement as well as wrist flexion and extension deformity with differing degrees of active movement. Muscles implicated in the postures are identified, therefore guiding individualized interventions.
House Functional Classification System
The House Functional Classification System17 was developed to evaluate the ability of children with unilateral CP to use their more affected hand to carry out activities following thumb surgery. It is a 9-point scale where hand function is classified from does not use, through use as a passive assist, an active assist, to spontaneous use of the more affected hand during tasks.
Hypertonicity Intervention Planning Model for Upper Limb Neurorehabilitation
The Hypertonicity Intervention Planning Model (HIPM)43 is a framework to identify the presence and severity of impairment and the type and amount of controlled movement in children and adults with hypertonicity. It provides guidance for selecting upper extremity interventions taking into account personal and environmental factors and individual goals.
Complementary Assessments
Assessment of sensation and strength add to a comprehensive understanding of the factors contributing to upper extremity function and will inform decisions regarding potentially effective interventions.
Sensation
Sensation refers to the ability to identify and interpret the nature, location, and intensity of sensory stimuli. Intact sensation is necessary for modulating grip forces, in-hand manipulation, and effective tool use. Sensation is compromised in children with CP.44 Although poor sensation is not a contraindication for surgery or other interventions, greater functional outcomes are proposed to result when sensation is intact.45
Strength
Spasticity frequently masks underlying muscle weakness,7 which is a secondary consequence of neurologic impairment and impacts on a child's motor ability and participation in activities of daily living. Children with CP often do not move as much as their typically developing peers and consequently their muscles atrophy as well as fail to develop normally.46 Understanding any weakness of spastic muscles and their antagonists will assist in predicting the outcome of intervention and in planning for rehabilitation following surgery or BoNT-A. Handheld dynamometry and manual muscle testing are typically used for measuring isometric muscle strength, but weakness may be difficult to assess objectively in young children, those with an intellectual impairment, or those with significant contractures.7
Conclusion
Choosing appropriate measures to grade and quantify upper extremity function of children with spasticity to select, plan, and measure the outcomes of intervention depends on a range of factors. Fig. 1 presents some of the available assessments and tools. An understanding of the child within their environment, the activities they need and want to be able to do, and the function that is required to achieve these activities is part of the measurement process. Accurate assessment of severity of impairment, volitional movement, the muscles contributing to active and static deformity, and factors impacting on function, such as spasticity, sensation, strength, and ROM, will add to the perspective. Regardless of the results of assessments and classification tools, other considerations are critical to consider in selecting interventions. The child's age, growth trajectory, intellectual ability, and motivation are necessary to consider. Intensive rehabilitation efforts are usually required after some types of surgery, for example, and the capacity of children to engage in these may influence a decision about whether to proceed. Availability of family time to commit to intervention, motivation, and financial resources will also be considerations in the selection of an intervention. Finally, the availability of skilled occupational therapy or other rehabilitation services may influence intervention options. For instance, intensive occupational therapy is recommended after upper extremity BoNT-A injections aimed at achieving functional goals. Such therapy will maximize the impact of injections and target motor activity toward goal achievement.
Acknowledgments
We thank Dr. Mary-Clare Waugh and Jane Berry for their thoughtful comments on the final draft of this article.
References
- 1.World Health Organization. International Classification of Functioning, Disability and Health, 2001 Available at: http://www.who.int/classifications/icf/en. Accessed July 27, 2015
- 2.James M A, Bagley A, Vogler J B IV, Davids J R, Van Heest A E. Correlation between standard upper extremity impairment measures and activity-based function testing in upper extremity cerebral palsy. J Pediatr Orthop. 2015 doi: 10.1097/BPO.0000000000000591. [DOI] [PubMed] [Google Scholar]
- 3.Hoare B, Imms C, Villanueva E, Rawicki H B, Matyas T, Carey L. Intensive therapy following upper limb botulinum toxin A injection in young children with unilateral cerebral palsy: a randomized trial. Dev Med Child Neurol. 2013;55(3):238–247. doi: 10.1111/dmcn.12054. [DOI] [PubMed] [Google Scholar]
- 4.Wallen M, Ziviani J, Naylor O, Evans R, Novak I, Herbert R D. Modified constraint-induced therapy for children with hemiplegic cerebral palsy: a randomized trial. Dev Med Child Neurol. 2011;53(12):1091–1099. doi: 10.1111/j.1469-8749.2011.04086.x. [DOI] [PubMed] [Google Scholar]
- 5.Wallen M, Stewart K. Upper limb function in everyday life of children with cerebral palsy: description and review of parent report measures. Disabil Rehabil. 2015;37(15):1353–1361. doi: 10.3109/09638288.2014.963704. [DOI] [PubMed] [Google Scholar]
- 6.Sanger T D Delgado M R Gaebler-Spira D Hallett M Mink J W; Task Force on Childhood Motor Disorders. Classification and definition of disorders causing hypertonia in childhood Pediatrics 20031111e89–e97. [DOI] [PubMed] [Google Scholar]
- 7.Sanger T D Chen D Delgado M R Gaebler-Spira D Hallett M Mink J W; Taskforce on Childhood Motor Disorders. Definition and classification of negative motor signs in childhood Pediatrics 200611852159–2167. [DOI] [PubMed] [Google Scholar]
- 8.Eliasson A C, Krumlinde-Sundholm L, Rösblad B. et al. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. 2006;48(7):549–554. doi: 10.1017/S0012162206001162. [DOI] [PubMed] [Google Scholar]
- 9.Beckung E, Hagberg G. Neuroimpairments, activity limitations, and participation restrictions in children with cerebral palsy. Dev Med Child Neurol. 2002;44(5):309–316. doi: 10.1017/s0012162201002134. [DOI] [PubMed] [Google Scholar]
- 10.Randall M, Harvey A, Imms C, Reid S, Lee K J, Reddihough D. Reliable classification of functional profiles and movement disorders of children with cerebral palsy. Phys Occup Ther Pediatr. 2013;33(3):342–352. doi: 10.3109/01942638.2012.747584. [DOI] [PubMed] [Google Scholar]
- 11.Palisano R J, Rosenbaum P, Bartlett D, Livingston M H. Content validity of the expanded and revised Gross Motor Function Classification System. Dev Med Child Neurol. 2008;50(10):744–750. doi: 10.1111/j.1469-8749.2008.03089.x. [DOI] [PubMed] [Google Scholar]
- 12.Hidecker M J, Paneth N, Rosenbaum P L. et al. Developing and validating the Communication Function Classification System for individuals with cerebral palsy. Dev Med Child Neurol. 2011;53(8):704–710. doi: 10.1111/j.1469-8749.2011.03996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jethwa A, Mink J, Macarthur C, Knights S, Fehlings T, Fehlings D. Development of the Hypertonia Assessment Tool (HAT): a discriminative tool for hypertonia in children. Dev Med Child Neurol. 2010;52(5):e83–e87. doi: 10.1111/j.1469-8749.2009.03483.x. [DOI] [PubMed] [Google Scholar]
- 14.Arnould C, Penta M, Renders A, Thonnard J L. ABILHAND-Kids: a measure of manual ability in children with cerebral palsy. Neurology. 2004;63(6):1045–1052. doi: 10.1212/01.wnl.0000138423.77640.37. [DOI] [PubMed] [Google Scholar]
- 15.Greaves S, Imms C, Dodd K, Krumlinde-Sundholm L. Development of the Mini-Assisting Hand Assessment: evidence for content and internal scale validity. Dev Med Child Neurol. 2013;55(11):1030–1037. doi: 10.1111/dmcn.12212. [DOI] [PubMed] [Google Scholar]
- 16.Davids J R, Peace L C, Wagner L V, Gidewall M A, Blackhurst D W, Roberson W M. Validation of the Shriners Hospital for Children Upper Extremity Evaluation (SHUEE) for children with hemiplegic cerebral palsy. J Bone Joint Surg Am. 2006;88(2):326–333. doi: 10.2106/JBJS.E.00298. [DOI] [PubMed] [Google Scholar]
- 17.House J H, Gwathmey F W, Fidler M O. A dynamic approach to the thumb-in palm deformity in cerebral palsy. J Bone Joint Surg Am. 1981;63(2):216–225. [PubMed] [Google Scholar]
- 18.Krumlinde-Sundholm L, Holmefur M, Kottorp A, Eliasson A C. The Assisting Hand Assessment: current evidence of validity, reliability, and responsiveness to change. Dev Med Child Neurol. 2007;49(4):259–264. doi: 10.1111/j.1469-8749.2007.00259.x. [DOI] [PubMed] [Google Scholar]
- 19.Zancolli E A Zancolli E Surgical rehabilitation of the spastic upper limb in cerebral palsy In: Lamb D W, ed. . The Paralysed Hand. Edinburgh, Scotland: Churchill Livingstone; 1987153–168. [Google Scholar]
- 20.Law M, Baptiste S, Carswell A, McColl M A, Polatajko H J, Pollock N, Ottawa, ON, Canada: CAOT Publications ACE; 2005. Canadian Occupational Performance Measure. 4th ed. [Google Scholar]
- 21.Kiresuk T J, Smith A, Cardillo J E. Mahwah, NJ: Erlbaum; 1994. Goal Attainment Scaling: applications, theory, and measurement. [Google Scholar]
- 22.Wallen M, Stewart K. London, England: Jessica Kingsley Publishers; 2015. The GAS approach: scaling tailored goals. [Google Scholar]
- 23.Gilmore R, Sakzewski L, Boyd R. Upper limb activity measures for 5- to 16-year-old children with congenital hemiplegia: a systematic review. Dev Med Child Neurol. 2010;52(1):14–21. doi: 10.1111/j.1469-8749.2009.03369.x. [DOI] [PubMed] [Google Scholar]
- 24.Krumlinde-Sundholm L, Ek L, Eliasson A C. What assessments evaluate use of hands in infants? A literature review. Dev Med Child Neurol. 2015;57 02:37–41. doi: 10.1111/dmcn.12684. [DOI] [PubMed] [Google Scholar]
- 25.Sköld A, Hermansson L N, Krumlinde-Sundholm L, Eliasson A C. Development and evidence of validity for the Children's Hand-use Experience Questionnaire (CHEQ) Dev Med Child Neurol. 2011;53(5):436–442. doi: 10.1111/j.1469-8749.2010.03896.x. [DOI] [PubMed] [Google Scholar]
- 26.Taub E, Ramey S L, DeLuca S, Echols K. Efficacy of constraint-induced movement therapy for children with cerebral palsy with asymmetric motor impairment. Pediatrics. 2004;113(2):305–312. doi: 10.1542/peds.113.2.305. [DOI] [PubMed] [Google Scholar]
- 27.Uswatte G, Taub E, Griffin A, Vogtle L, Rowe J, Barman J. The Pediatric Motor Activity Log-Revised: assessing real-world arm use in children with cerebral palsy. Rehabil Psychol. 2012;57(2):149–158. doi: 10.1037/a0028516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wallen M, Bundy A, Pont K, Ziviani J. Psychometric properties of the Pediatric Motor Activity Log used for children with cerebral palsy. Dev Med Child Neurol. 2009;51(3):200–208. doi: 10.1111/j.1469-8749.2008.03157.x. [DOI] [PubMed] [Google Scholar]
- 29.Wallen M, Ziviani J. Caution regarding the Pediatric Motor Activity Log to measure upper limb intervention outcomes for children with unilateral cerebral palsy. Dev Med Child Neurol. 2013;55(6):497–498. doi: 10.1111/dmcn.12057. [DOI] [PubMed] [Google Scholar]
- 30.Randall M, Imms C, Carey L M, Pallant J F. Rasch analysis of the Melbourne Assessment of Unilateral Upper Limb Function. Dev Med Child Neurol. 2014;56(7):665–672. doi: 10.1111/dmcn.12391. [DOI] [PubMed] [Google Scholar]
- 31.DeMatteo C Law M Russell D et al. The reliability and validity of Quality of Upper Extremity Skills Test Phys Occup Ther Pediatr 199313(2):1–18. [Google Scholar]
- 32.Jongbloed-Pereboom M, Nijhuis-van der Sanden M W, Steenbergen B. Norm scores of the Box and Blocks Test for children ages 3-10 years. Am J Occup Ther. 2013;67(3):312–318. doi: 10.5014/ajot.2013.006643. [DOI] [PubMed] [Google Scholar]
- 33.Mathiowetz V Federman S Wiemer D Box and Blocks Test of Manual Dexterity: norms for 6–19 year olds Can J Occup Ther 198552(5):241–245. [Google Scholar]
- 34.Gracies J M, Marosszeky J E, Renton R, Sandanam J, Gandevia S C, Burke D. Short-term effects of dynamic Lycra splints on upper limb in hemiplegic patients. Arch Phys Med Rehabil. 2000;81(12):1547–1555. doi: 10.1053/apmr.2000.16346. [DOI] [PubMed] [Google Scholar]
- 35.Boyd R N Barwood S A Balieu C et al. Validity of a clinical measure of spasticity in children with cerebral palsy in a double blinded randomised controlled clinical trial Dev Med Child Neurol 199840(S78):7 [Google Scholar]
- 36.Williams S Love S C Gibson N et al. Reliability of the Australian Spasticity Assessment Scale Dev Med Child Neurol 200850(S113):4. [DOI] [PubMed] [Google Scholar]
- 37.Bohannon R W, Smith M B. Interrater reliability of a Modified Ashworth Scale of Muscle Spasticity. Phys Ther. 1987;67(2):206–207. doi: 10.1093/ptj/67.2.206. [DOI] [PubMed] [Google Scholar]
- 38.Clopton N, Dutton J, Featherston T, Grigsby A, Mobley J, Melvin J. Interrater and intrarater reliability of the Modified Ashworth Scale in children with hypertonia. Pediatr Phys Ther. 2005;17(4):268–274. doi: 10.1097/01.pep.0000186509.41238.1a. [DOI] [PubMed] [Google Scholar]
- 39.Klingels K, De Cock P, Molenaers G. et al. Upper limb motor and sensory impairments in children with hemiplegic cerebral palsy. Can they be measured reliably? Disabil Rehabil. 2010;32(5):409–416. doi: 10.3109/09638280903171469. [DOI] [PubMed] [Google Scholar]
- 40.Wilton J. Casting, splinting, and physical and occupational therapy of hand deformity and dysfunction in cerebral palsy. Hand Clin. 2003;19(4):573–584. doi: 10.1016/s0749-0712(03)00044-1. [DOI] [PubMed] [Google Scholar]
- 41.Gschwind C, Tonkin M. Surgery for cerebral palsy: Part 1. Classification and operative procedures for pronation deformity. J Hand Surg [Br] 1992;17(4):391–395. doi: 10.1016/s0266-7681(05)80260-8. [DOI] [PubMed] [Google Scholar]
- 42.Georgiades M, Elliott C, Wilton J, Blair E, Blackmore M, Garbellini S. The Neurological Hand Deformity Classification for children with cerebral palsy. Aust Occup Ther J. 2014;61(6):394–402. doi: 10.1111/1440-1630.12150. [DOI] [PubMed] [Google Scholar]
- 43.Copley J, Kuipers K. West Sussex, UK: Wiley Blackwell; 2014. Neurorehabilitation of the upper limb across the lifespan: managing hypertonicity for optimal function. [Google Scholar]
- 44.Auld M L, Boyd R, Moseley G L, Ware R, Johnston L M. Tactile function in children with unilateral cerebral palsy compared to typically developing children. Disabil Rehabil. 2012;34(17):1488–1494. doi: 10.3109/09638288.2011.650314. [DOI] [PubMed] [Google Scholar]
- 45.Zancolli E A, Goldner L J, Swanson A B. Surgery of the spastic hand in cerebral palsy: report of the Committee on Spastic Hand Evaluation (International Federation of Societies for Surgery of the Hand) J Hand Surg Am. 1983;8(5 Pt 2):766–772. doi: 10.1016/s0363-5023(83)80267-6. [DOI] [PubMed] [Google Scholar]
- 46.Damiano D L Strengthening in children with motor disabilities: Just do it! Dev Med Child Neurol 200850(S113):3 [Google Scholar]


