Abstract
Team-based learning (TBL) helps instructors develop an active teaching approach for the classroom through group work. The TBL infrastructure engages students in the learning process through the Readiness Assessment Process, problem-solving through team discussions, and peer feedback to ensure accountability. This manuscript describes the benefits and barriers of TBL, and the tools necessary for developing, implementing, and critically evaluating the technique within coursework in a user-friendly method. Specifically, the manuscript describes the processes underpinning effective TBL development, preparation, implementation, assessment, and evaluation, as well as practical techniques and advice from authors’ classroom experiences. The paper also highlights published articles in the area of TBL in education, with a focus on pharmacy education.
Keywords: Team-based learning, pharmacy education, active learning, classroom education, learning, teaching
INTRODUCTION
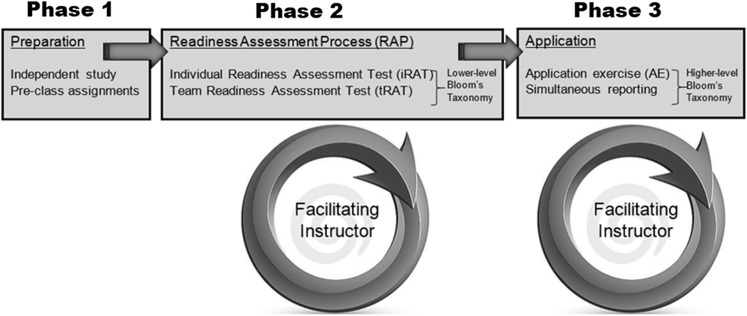
Team based learning is an instructional strategy designed to support the development of learning in teams1 and is characterized by a 3-phase approach (Figure 1). In the first phase (preparation), learners obtain new information prior to class and then are held accountable for learned information in class with a brief assessment based on assigned material reviewed prior to class called the Readiness Assessment Process (RAP) – the second phase of TBL. The RAP includes a brief assessment of individuals grasp on content followed by team engagement of the same assessment. This sequence seeks to leverage collaborative learning to assure the readiness of the student cohort to engage problem solving in the next phase (application exercises). During the third phase (application), students share information they acquired while in teams to solve real-world problems, apply learned information on an examination and, finally, provide peer feedback. Throughout this strategy, the instructor serves more as a facilitator than a content expert.
Figure 1.
Team-based learning process.
Teamwork permeates today’s health care institutions. The Accreditation Council for Pharmacy Education (ACPE), the American College of Clinical Pharmacy, the Institute of Medicine, and the World Health Organization promote interprofessional collaborations in practice and education.2-4 Team-based care encourages academicians to adopt educational styles that foster collaboration to solve problems. While enhancing student education, TBL benefits health outcomes and interprofessional collaborations, in addition to improving faculty satisfaction and reducing faculty workload.5
From a curricular perspective, the 2016 ACPE Accreditation Standards stress that curricula must include strategies that actively engage learners and emphasize that learners should be given opportunities to apply foundational knowledge in a patient-care context.2 While there are several ways to apply such knowledge in the patient care context, TBL provides a simple active-learning strategy that can be employed on a regular basis within a large classroom context with minimal faculty resources. The TBL model directly connects with the first, third, and fourth domains and competency areas in the CAPE Educational Outcomes.6
All 4 domains from the CAPE Outcomes have been adopted in full as the first 4 standards in the ACPE’s 2016 Standards. The first ACPE domain, Foundational Knowledge, is developed in phase 1 with overlap in phase 2 as readiness is assessed and feedback is given to students through a mini-lecture. Competency in foundational knowledge is significant to build on for ACPE domain 3, Approach to Practice and Patient Care. For ACPE domain 3, student problem-solving is developed in phases 2 and 3 of the TBL strategy. In phase 2, less complex applications may be used in the RAP, whereas, more complex problems are used in phase 3.
Through team efforts, students can enhance their abilities to think collaboratively, consider alternative viewpoints, educate others, communicate effectively to ensure their perspectives are considered, and advocate for patients as they solve problems relevant to patient care and pharmacy practice. There is also opportunity to connect TBL to the fourth domain, Professionalism, by assessing individual and team development of skills in the areas of self-awareness, leadership, innovative thinking, and professionalism. This may be accomplished through profile assessments and team assessments that can provide information useful in tracking student leadership development and development of cognitive and affective domains. Lastly, curricular content and experiences more loosely connect TBL to the second domain, Essentials for Practice and Care.
TBL is integrated into skill-set development in social and health sciences within undergraduate and graduate curricula, and across various topics. It has been extensively used in medical school education since 2001, and medical educators are an integral part of, and leaders within, the TBL community. The success of TBL in educating and training medical students is demonstrated in the literature.7,8 According to Michaelsen, a pioneer in this teaching strategy, TBL requires faculty members to do the following: make their reading and preclass preparation clear to students; use a mechanism to test students’ individual understanding of content within the assigned readings; use a mechanism to test students’ performance within a team that is consistent with, or similar to, that used to ascertain individual understanding; engage students in discussion after the individual-based and team-based assessments to identify areas where knowledge is strong and where it is weak.
When implemented well, this process can provide insight to help instructors better target mini-lectures to further student learning. Team-based learning can be implemented into any didactic course with a critical number of students (around 10 at minimum).9 To our knowledge, TBL has not been implemented in a purely experiential environment.
DEVELOPMENT, PREPARATION, AND IMPLEMENTATION OF TBL
Forming teams is an integral part of the TBL process. Ideally, teams should be composed of 5 to 7 students with diverse backgrounds to encourage varied perspectives.1 Team member diversification may include differing academic achievement, abilities, and cultural background. To limit homogenous team formation that may occur through group self-selection, instructors should strategically assign students to teams. Multiple methods exist for ensuring heterogeneity, including having students answer yes/no to questions about specific characteristics (eg, educational background, grade point average, ethnicity) or collecting relevant student information (such as learning style) before class, and devising groups accordingly. Once formed, teams should be permanent throughout a course or semester.
Learning objectives and phases of TBL
Writing learning objectives for a TBL session follow the same general principles as any other classroom teaching methodology. Instructors develop general learning objectives for the entire course and specific objectives for major units or course blocks. A unit, or block, is approximately 6-10 hours of coursework.9 A popular strategy for writing learning objectives for TBL is with the “backwards” course design, which uses terminal behavior objectives (ie, what the student should be able to do at the completion of the course) as the cornerstone for course development. If constructed optimally, the need for rote memorization of irrelevant details is eliminated.
Learning objectives also assist students in focusing on assigned readings during the preparation phase. While not unique to TBL, preclass assigned activities are foundational to student success in all phases of TBL. The purpose is to provide essential background information, as opposed to a comprehensive in-depth review of the subject. Reading assignments may include book chapters, instructor-prepared handouts, prerecorded lectures, PowerPoint slides, or specific website reviews.10 Some authors suggest a 30-page maximum for each block or unit of reading.11,12
The RAP holds students accountable for completing the prereading assignment. At the beginning of each module, students complete a brief individual quiz (usually multiple-choice) called an individual readiness assurance test (iRAT). In general, iRAT questions are written at the knowledge and comprehension level of Bloom’s Taxonomy to test students’ overall understanding of key concepts rather than factual knowledge. After completing the iRAT, the instructor collects all answer sheets and distributes an identical quiz to be completed in teams—the tRAT. Teams discuss each question and arrive at an agreed upon answer. If an incorrect answer is initially selected, discussion continues until the correct response is identified. Awarded points decrease in value until the correct answer is finally chosen. This process is dynamic and, if the test is sufficiently challenging, generates much discussion within the team. Instructors may need to clarify why correct answers are right and why incorrect answers are wrong. Michaelsen contends that a short lecture may be used in this final step of the RAP; however, this lecture should be focused on what the students do not know, instead of reiterating the knowledge they already gained during the preparation phase. Afterward, students have the option to appeal missed questions. This usually occurs if a team or individual believes that an item was ambiguous. The appeal should be written and supported with sufficient evidence. Only the team or individual drafting the appeal, if granted, receives credit for the challenged question. The RAP should be used judiciously in the classroom to motivate students to arrive prepared. Frequent use may promote a “reward” system that favors memorizing details to acquire points and not necessarily the application of content. A general rule is to use approximately 6-9 RATs within a typical 15-week semester.
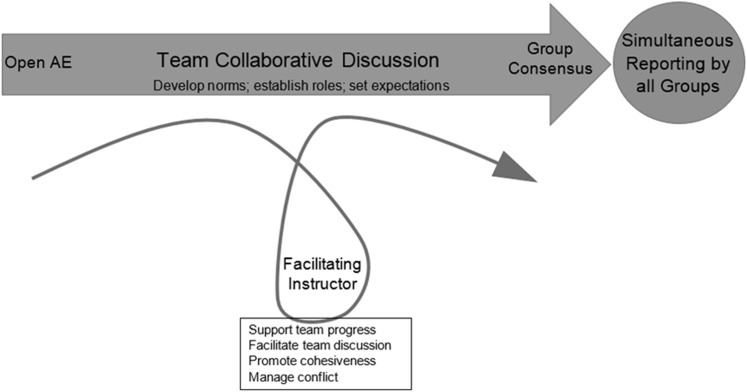
The next phase is the application phase. During this phase, students work in small groups to use information learned in the preparation phase to solve complex therapeutic problems called application exercises (AEs) (Figure 2). Generally, AEs progress in difficulty and achieve higher levels of Bloom’s Taxonomy as students gain mastery of the topic. The exercises are carefully crafted to help students gain an in-depth comprehension of the material and also allow opportunities for team discussion. To optimize learning, Michaelsen recommends the exercise process provide individual accountability, team togetherness, interteam and intrateam discussion, immediate instructor feedback, and a reward for performance. Additionally, each AE should be relevant and applicable and ultimately lead to choosing a specific answer. Each team works on the same problem and report answers simultaneously. Programs may use large answer-choice cards revealed by a designated team member to answer an AE question.13 Dissention within teams provides a starting point for discussion and opportunities for input from multiple students.
Figure 2.
Application exercise process.
Discussion serves to expand the students’ critical thinking, as all facets of the solution are delineated and differing opinions offer alternative ways of thinking about the same problem. Discussion within teams allows students to build support for their answers with evidence and also challenges their own thought process through peer-to-peer debate. The instructor circulates in the classroom to facilitate discussion and provide clarification during the AE. This not only gives students a sense that an expert opinion is close by, but it also helps students stay on task. At the end of the discussion facilitation period, the instructor attempts to determine the class’s level of understanding. During this time, the instructor can reinforce basic concepts and tenets that emerged during the RAP and application phase. This also allows the instructor to fill in gaps in student learning and highlight concepts that did not emerge during the application phase. Application exercises are not typically graded but used for formative feedback. However, Michaelsen asserts that some reward system should be in place to provide an incentive for group performance. This could be in the form of a small percentage of individual students’ overall grade.12,14
Equipment Needed for TBL
Identifying what resources are needed entails considering activities that will occur before, during, and after class. It is best done after completing the “backwards design” process.9 Keeping TBL sessions organized and on task while maintaining security of course material is essential. Learning management systems (LMS), such as Sakai (Apereo Foundation, Ann Arbor, MI) or Blackboard (Blackboard, Inc, Washington, DC), provide a secure and traceable portal for student access and allow instructors to control distribution. Alternatively, nondigital methods may be employed, the most economic method being paper folders. Consider the direct cost of the system in addition to the faculty workload involved with each method. Regardless of the method selected, it is important to safeguard confidential documents and educate students about which materials may be used outside of class.
The iRAT portion of the RAP can be completed using pen and paper, a machine-readable form (eg, Scantron [Scantron Corp., Eagan, MN]); electronically, using an audience response system (eg, “clickers”); or an online system (eg, team-based testing system). Paper testing requires the least resources but is the most time consuming method for grading. Machine-readable forms and audience response systems can expedite the grading process but come with an additional cost for the forms and reader or devices and software.
The tRAT is more complex, as it requires immediate feedback and multiple responses until a correct answer is identified. This may be accomplished using Immediate Feedback Assessment Technique (IF-AT) Forms (Epstein Educational Enterprises, Cincinnati, OH). These scratch-off answer forms have an opaque coating similar to a lottery ticket, which allows teams to immediately determine if their selected answer choice is correct. Students can subsequently scratch off other boxes in search of the correct answer. The IF-AT forms provide opportunities for partial credit on the tRAT depending on the number of unsuccessful scratches. Students only receive full credit if they find the correct answer on the first attempt. These forms are available in lengths of 10, 25, and 50 questions, with either 4 or 5 question/answer choice options. Each form has a tear-away number at the bottom that corresponds to a specific key. The manufacturer of these forms – Epstein Educational Enterprises (Cincinnati, OH) – also developed a free test bank program called “IF-AT Testmaker,” which keys items to the specific test form.
An electronic alternative to the IF-AT Form is an open source program called Team Based Testing (TBT).15,16 Students individually sign on to individual Internet-ready computers using this system to complete the tRAT. Each group must choose a team leader, who then submits the tRAT answers. The system provides immediate feedback on whether their choice was correct and dithers, or grays out, incorrectly selected answers for subsequent attempts. The instructor may download results in a spreadsheet format and upload the information into an LMS system for confidential student sharing.
Many of the same resources can be used for both the RAP and application exercises. To simultaneously demonstrate a specific choice, groups can respond by holding up a colored card for classmates to see. Similarly, for short answer or graphic responses, flip charts or white boards may be an option; however, if not built into the classroom, logistical issues may arise. Using nondigital methods may unfortunately hinder groups’ decision making if teams observe each other during the process. Using an electronic method (eg, ARS) where responses are blinded may help avoid this issue. The technological learning curve involved in assembling and executing ARS sessions can be an initial hindrance. Lastly, depending on the system, it can be challenging to link teams with their selected answers when students are not forthcoming. There are shared spaces in an LMS that can be used in this setting, including discussion boards, file exchange pages, blogs, and Wikis.
Traditionally, student peer evaluations are either hand-written or typed and submitted electronically. In large classrooms, collating, reviewing, and grading can be a daunting task. To date, most LMS’s do not have tools to expedite this process. “iPeer” is an open-source program (Centre for Teaching, Learning and Technology, University of British Columbia, Vancouver, BC, Canada) designed for the TBL peer evaluation process. The program, which is written in PHP (Hypertext Preprocessor), must be installed on a local server and maintained by each institution’s information technology staff. Therefore, start-up may be difficult because of the potentially unfamiliar software language and need for onsite installation. Despite initial barriers, once the program is functional, it streamlines the peer-review process and may be worth the effort.
Faculty training and workload requirement
Team-based learning may increase faculty workload compared to delivering the same course material via traditional lectures. Faculty members must identify or prepare preclassroom readings for students, with matching learning objectives,17 which are a roadmap to faculty-identified key material. This may include careful construction of supplemental materials such as notes, PowerPoint presentations, or other resources (eg, video clips) to foster effective student learning. Once the reading and supplemental materials are devised, appropriate RAT questions and AEs should be developed, which may take several class sessions. Ensuring tRAT answers are coded correctly takes time. If using nonelectronic means, preparation of materials including photocopying, placing RATs and AEs into individual team folders, and administering the iRATs and tRATs can be time consuming. Therefore, developing a new unit can be time consuming.
Faculty training should be specific to an institution’s needs, aligned to TBL, and provide desired outcomes. New faculty members should become acquainted with TBL through reading material and experiencing the TBL process before teaching. One method is to devise a nonthreatening TBL unit using a recent journal article for faculty training. Faculty members can submit unit objectives, RAT items, and AEs prior to the training session. The facilitator may then discuss which objectives, items, and AEs are appropriate. During the TBL training session, faculty members can complete the iRAT, tRAT, and AEs.
Team-based learning encompasses individual and group work so student participation and classroom time management can be challenging. Some instructors suggest “time flags,” or other devices to alert the instructor when group discussion has ended. Instructors can then more easily gauge when most groups are ready to move on to simultaneous reporting. Being flexible and managing time may allow planning for extra time to review topic concepts and overflow of AE-stimulated class discussion, which can promote student learning.
FACILITATION TECHNIQUES
The primary role of the instructor in TBL is to guide and encourage student learning by moving away from lecturing and promoting student-led discussions. Through this method, instructors encourage critical thinking, foster self-directed learning, monitor group processes and progress, promote teamwork, encourage debate and uncertainty, and create an environment conducive to learning.18 Facilitators in TBL are often content experts who provide suggestions for resources, advice on how to learn, and encouragement and feedback on content and process.
In TBL, facilitators must avoid providing too much direction, which may negatively affect group dynamics and interfere with the development of skills related to judgment, innovation, perspective, questioning, reflection, and feedback.19 However, if facilitators provide too little direction, teams may drift away from content or process. The practice of facilitation requires instructors to know when to intervene and when to allow groups to come to their own conclusions.
Advocates of TBL argue that most experienced educators already have many of the skills and competencies required to effectively implement TBL.20 The major difference is that instead of focusing on how and what to teach, instructors focus on how to enhance student learning. Essential facilitator skills include: creating a climate for student-centered learning; responding to individual student needs; and guiding learners through their own discovery by asking open-ended questions as they engage in reflective dialogue and critical thinking.20
Facilitators create an effective learning climate by maintaining an open mind and promoting inclusiveness. Clear and specific expectations for participation and behavior are necessary for maintaining trust, cooperation, support, respect, and accountability. Instructors who dominate the discussion or lecture instead of encouraging dialogue can stifle group development and student learning.21 In guiding learners and encouraging dialogue and debate, facilitators can ask questions, summarize what has been said, or make observations in order to promote reflection.
Processes for iRAT/tRAT
Facilitation does not generally occur during the iRAT; there is no discussion or facilitation while the iRAT is being completed. Students discuss content during the tRAT; however, the instructor does not facilitate discussion at this point. Content-based questions may arise after the iRAT and tRAT are completed. Facilitation during this part of the TBL process will set the tone for the instructor’s ability to command the class.
If the validity of the question is challenged, the facilitator decides whether or not the challenge is legitimate. Rather than defending an answer, facilitators can acknowledge the student’s concern and reminds the student of the appeal process.22 This minimizes class disruption, maintains the schedule, and allows for a more thorough review of the concern. At the end of the testing and appeal phase, facilitators may open the floor to student questions about the content or respond to items identified in the individual test as challenging. A brief discussion or mini-lecture may be employed to clarify major issues, or offer evidence of personal expertise or credibility.20
The timing of the RAT is determined prior to the first class. Some facilitators may require all students to complete the iRAT before the tRAT is started, which is what Michaelsen recommends.23 Other instructors may give a 5-minute warning when half of the class has completed the iRAT to help keep TBL activities on schedule. This strategy only works if iRAT completion can be effectively monitored. Teams that complete the tRAT should be quiet and remain in the classroom until the entire class is finished. However, after a reasonable period of time, if all teams have not completed the tRAT, discussion can occur among all teams.
All processes should be communicated upfront to students to ensure understanding of expectations, which may include that resources may not be used during the iRAT and tRAT and that answer choices on an IF-AT (if used), may not be altered; doing so will result in the question being marked as incorrect. This includes situations where students report accidentally scratching off an incorrect answer choice or report being pressured into selecting an incorrect answer. If the policies are well established up front, the facilitator may only need to remind students of the policy.
Processes for team application exercises
The facilitator is responsible for monitoring group progress and intervening when obstacles interfere with a team’s technical, informational, or motivational needs24 (Figure 2). Instructors can monitor team progress by walking around the classroom and observing students’ participation and interactions.20 If students ask questions about the application, the facilitator should respond by asking open-ended questions that engage students in critical thinking. A facilitator might respond to a question by asking, “How would anyone else answer that?” or “Where did you look to try to find the answer?” or counting to 10 before addressing students’ questions.20 If a question posed by an individual team needs to be answered to move the AE forward, the facilitator may decide to address the entire class. However, a specific question arising from a team’s discussion may be addressed only with that team.
As team members collaborate and develop norms, roles, expectations, and a sense of accountability may emerge. Preferably, team members will engage a nonparticipatory student rather than relying on the instructor to prompt that individual to contribute. Group ground rules set by teams are beneficial.25 Such rules could include no texting, surfing the Internet, studying for another class, or loafing while AEs are being completed. However, if individual teams do not devise such rules, the instructor may need to intervene. Although not preferred, another strategy to engage a disinterested student is for the instructor to ask that individual for an answer to the AE. This may have consequences, however, such as forcing the student to become more withdrawn and even resentful toward the instructor.
Another tactic that may raise team accountability is to allow the nonparticipatory student to select a team member to share the spotlight. Team members may realize that this peer is responsible for the instructor’s additional attention and require better engagement in the future. Anonymous peer evaluations within each team are also useful for maintaining individual accountability. The instructor should provide instruction at the start of the semester about giving helpful, constructive feedback, in an effort to avoid students giving unsupportive, negative comments.
Other strategies for enhancing student participation within teams include: arranging seating, if possible, in a circle or semi-circle so team members are facing each other; using eye contact and other nonverbal communication (nodding or smiling) to open a communication channel and select a student for a turn to speak; moving toward the speaker to indicate interest in the presentation and that others should be listening as well; emphasizing the value of student contributions or responses by paraphrasing or making connections between their contributions and the discussion at large; using a token system (team members receive a certain number of tokens, which are turned in each time the student contributes—the goal is to turn in all tokens by the end of the session); limiting facilitator involvement in the discussion and encouraging students to develop their own ideas, questions, and responses; drawing quiet students into the discussion with nonthreatening questions that do not require a detailed or correct response and encouraging other teams to expand on those ideas; and calling on different students in the group to increase attentiveness, participation, and accountability.26
At times, teams may struggle reaching an agreement. However, techniques may be employed to facilitate team consensus, such as providing a summary of team progress 24 or asking students to contemplate another solution or rethink their position. Another strategy involves having the team identify criteria they will use to make a decision and then evaluate ideas against the criteria.27 This “go around” technique requires each team member to explain their assessment approach, which allows similar and conflicting perspectives to be revealed.28 Using a majority vote is not representative of consensus and should be avoided, if possible. Teams should make every effort to achieve consensus through discussion. Facilitator neutrality is essential when it comes to students achieving consensus and making critical decisions. Effective team process may be sabotaged when members perceive that the facilitator agrees or disagrees with a particular response.
One responsibility of the facilitator is to maintain a safe environment for dialogue and exploration. Conflict among team members may be beneficial to a lively and in-depth discussion about the AE. However, unresolved conflict may produce a negative atmosphere and limit effective teamwork. Ideally, team members are able to negotiate the conflict without instructor intervention, which ultimately helps to build team cohesiveness and provides the students with valuable lessons in conflict resolution. Facilitators should allow students to engage in conflict resolution on their own without disrupting others’ learning. When facilitator intervention is required, facilitators should discourage criticism and personal attacks, and instead refocus the discussion toward concepts. This may involve carefully phrasing responses to unconstructive comments and establishing ground rules that promote and honor diversity.
Processes for class discussion
The most important skills of facilitators emerge during discussion and sequential reporting of AE answers. Because this aspect allows teams to compare answers, it is essential for facilitators to focus classroom conversation through thoughtful questions, help students appropriately summarize their key points, support critical reflection, and provide positive feedback for participation.20 When students are reluctant to share individual or team ideas, one can ask what others can add to the idea. If a team does not engage in discussion, the facilitator may physically move closer, shifting focus to that team.29 Students can also stand when they are speaking or asking a question. To prompt discussion, facilitators can inquire about acceptable, alternative options, or the rationale used to eliminate incorrect answers.29 Facilitators may inquire about differing opinions within teams, which gives students who did not necessarily agree with their team’s answer the opportunity to express their views. Alternatively, one can ask teams to identify changes in the AE that would alter an answer from incorrect to correct.29 This may lead to differing group answers during simultaneous reporting, which can generate class discussion.
Throughout the discussion while teams are sharing, the facilitator should avoid verbal or nonverbal cues that indicate agreement or disagreement as value judgments may interfere with discussion. The facilitator should exercise caution and resist offering expert opinion before all teams have had a chance to share and sufficient discussion has taken place. After a given question has been thoroughly discussed, the facilitator should provide an explanation of the correct answer or answers. This is the facilitator’s opportunity to critique the different options and explain content that students may not have fully understood.
ASSESSMENT AND EVALUATION OF TBL
Assessment of programs relies heavily on the goals of the individual topic, courses, and curriculum. Because the extent to which TBL is integrated into a curriculum can vary greatly, schools must determine where this type of learning may best meet the needs of students and faculty members. Students may be introduced to this method of learning early in a program so that TBL can be utilized throughout all courses. Alternatively, specific topics or classes may be identified for a TBL experience. It is important to consider the workload requirements of other courses in order to assess the feasibility of students completing the out-of-class learning.
Smaller elective courses may be more realistic for some schools and can still provide students with the opportunity to gain self-learning and teamwork skills commonly acquired through TBL. Alternatively, using TBL for larger class sizes or for core courses provides more opportunity for students to work with a variety of students and concepts. Regardless, TBL can be successfully accomplished in a variety of course sizes as long as there is adequate preparation and planning.
Preparation and Assessment of Faculty Members
Faculty development must be incorporated into the initial planning long before TBL is implemented17 to lay the groundwork and foster open discussion of concerns and solutions. Invitation of TBL experts to faculty workshops may increase the comfort level and confidence of faculty members and reduce their resistance to change. These efforts require a significant investment of resources and support by the college, dean, and other key administrators. The dean and department chair in particular should be prepared to support faculty members in areas such as travel or resource purchases, workload reallocation, mentoring, recognition of innovations in teaching, and budget support for scholarship of teaching TBL. Less obvious is the need for their support during declines in student and/or peer evaluations of teaching performance. Any pedagogy that induces discomfort in students may result in a decrease in satisfaction among some students. Evaluators must be able to differentiate student feedback on the pedagogy from feedback specific to a faculty member. Faculty members may require several years to improve, respond to peer feedback, and adapt teaching materials to TBL.
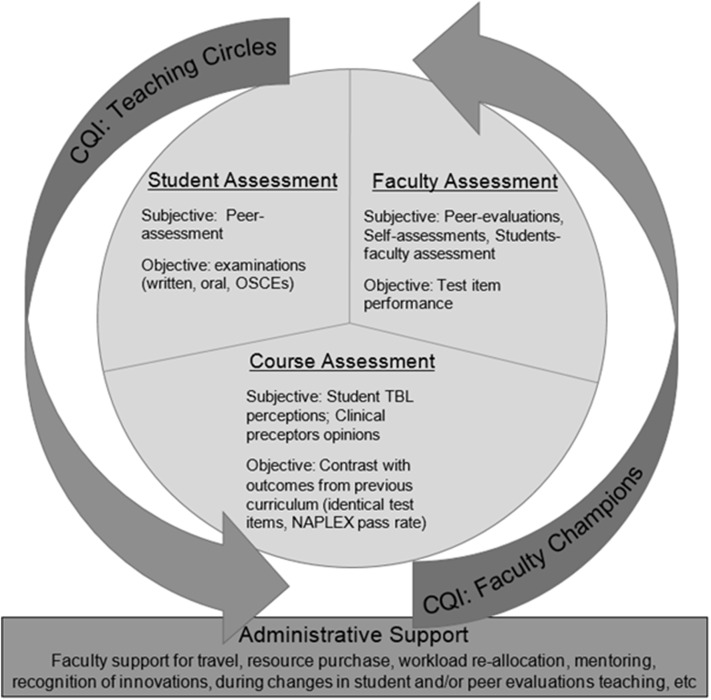
Continuous quality improvement is another essential aspect in the faculty planning process (Figure 3). Consider developing faculty “teaching circles” that meet periodically throughout each semester. These circles can share their experiences, successes, strategies for improvement, and new resources to maintain consistency of course modules. The circles agree upon and provide peer-review for the overall course syllabus, module structure, teaching objectives, grading schemes, RAT, AEs, and examination questions. Lastly, the teaching circle faculty members, in addition to the department chair, provide formative feedback to the instructors facilitating TBL.
Figure 3.
Team-based learning continued quality improvement and assessment.
If TBL is team-taught, administrative encouragement for faculty members to support the process can maintain consistency. The faculty members most resistant to adopting a TBL model may be those who believe they have successfully mastered more traditional approaches. “Faculty champions” who are enthusiastic and willing to invest in development may assist with bringing more resistant faculty members on board. Overall, encouraging faculty members to promote a student-centered learning philosophy will assist in the acceptance of TBL and reinforce benefits to student learning.9Assessing TBL faculty members and instructors can be challenging. The majority of faculty efforts are spent in the planning process rather than in face-to-face time with students. This requires a special means of assessing the effectiveness of faculty members and places of emphasis on nonstudent evaluations. Students’ individual perceptions of TBL may affect their ability to objectively assess a specific component of the course. Additionally, much of the impact of TBL, such as developing problem-solving skills, may be best assessed in later stages of the curriculum. This should not prevent solicitation and utilization of student feedback. However, student input should be measured in the context of other forms of faculty assessment. Student evaluation of faculty members should include the faculty member’s preparation, appropriateness, and confidence as well as usefulness, clarity, and effectiveness of objectives, RAT, and AEs.
Self-assessment paired with peer assessments may be the most appropriate way to measure a faculty member’s performance in TBL. These should focus on major TBL components, such as RAT items (linked to lower-order Bloom’s Taxonomy levels) and examination items (linked to higher-order Bloom’s Taxonomy levels), both of which should be paired to module objectives. Peer review of the AE should focus on accuracy and realism in addition to effectiveness of an embedded trigger to drive students to consider specific concepts. Having both content experts and those with less topic familiarity assess all components of the module provides a more full evaluation. Combining student, peer, and self-evaluations allows for a critical assessment of the relevance and clarity from the point of view of the expert as well as the student.
Student Peer Assessment
Team-based learning involves extensive group work for completion of the tRAT and AEs. Thus, this active-learning method relies heavily on student interactions in team settings. Unfortunately, “social loafing” may develop when individuals are graded equally based on the group’s completed work. This phenomenon of unequal participation by individual group members inhibits effective learning in the team environment.30,31 As described by Michaelsen, one of the 4 essential principles of TBL is that students are accountable for personal preparation and contributing to team work.13
In traditional classes, students who attend class unprepared put their own learning in jeopardy. In TBL, they also fail to positively contribute to their team’s performance, potentially affecting group dynamics and other students’ success. The need for accountability on the part of each student is a strength of TBL as a student-centered pedagogy. The challenge created for faculty members is to address the potential impact of social loafing on individual and team learning.
Team-based learning requires a system of evaluating student performance to assess the dynamics of individual interactions within teams. Team members working together during a course are in the position to provide feedback on the contributions and performance of their peers. While a number of systems have been used for student peer evaluations,9,31 scores should comprise a significant portion of an individual student’s grade.9 The peer-evaluation score can be a stand-alone component of the final course grade or used as a multiplier to “weight” team grades for each student.31 For example, a student receiving a peer-evaluation of 80% would receive 80% of the total points awarded for the team’s graded work.
Providing feedback to peers can be a difficult task for students. To improve the success of the process, one can first educate students about the purpose and significance of peer evaluations. Health care professionals increasingly work in teams in various practice settings, so it is appropriate that pharmacy students learn in team environments. The feedback received from students regarding their team interactions can be valuable in their growth as professionals. The more the peer-evaluation system is accepted, the more effectively students can incorporate the feedback they receive into changing their behaviors. Use of peer-evaluation tools, in which students remain anonymous and/or faculty advisors summarize feedback prior to communicating results to students, may improve both the quantity and quality of feedback.32Adequate training must be provided to students so they can understand the mechanics of the peer-evaluation tool to ensure accurate, effective, and efficient feedback.
When constructing the peer-evaluation instrument, it is important to allow students to provide quantitative and qualitative feedback.33 Quantitative portions of peer evaluations may be problematic because they allow students to assign similar grades to all of their teammates. For example, students may be asked to rate fellow students on a scale from 1 to 10 on a variety of characteristics valued by the program (eg, preparation, responsibility, promptness, interpersonal skills, respect for others). Students may be reluctant to assign low scores or provide negative comments to peers, despite the confidentiality of the process. Some may have concerns for the potential of breech of confidentiality and subsequent retaliation from their student colleagues if authorship of negative, despite constructive, feedback is discovered. These concerns can lead to provision of only positive comments and allocation of high scores. To preserve the integrity and effectiveness of the peer-evaluation process in these situations, the quantitative section of the instrument can include a forced ranking system. Total points can be determined for each item (eg, 42 points for a 5-member team), with students being asked to divide the points among all team members.
Alternatively, students may be asked to assign top-to-bottom scores for each item so students rank their 4 team members by assigning one student 6 points, one 4 points, one 2 points, and one 0 points. Students can provide comments to justify the rankings to develop a deeper understanding of how peers might improve their contributions to the team. Requiring quantitative ranking for peer evaluations with justification challenges students to approach the process using greater critical-thinking and assessment techniques and may help prevent grade inflation. Regardless of the approach taken to assess individual performance in the team setting, peer evaluation is a critical component of TBL because it increases student accountability, supports higher-level and more effective educational activities, and ultimately leads to improved learning (Figure 3).
Improving Student Perceptions of TBL
A school transitioning to TBL from other teaching formats must be prepared for a significant culture shift.9 Although pharmacy education is adopting more active-teaching modalities, many students expect to attend class and listen passively to the instructor. Faculty members should anticipate resistance from students, given the active engagement and accountability required in TBL. To ease this transition, it may help to prepare students and faculty members by facilitating discussion through student class representatives, liaisons to curriculum committees, and focus groups.
Clarifying the expectations and rationale for TBL is essential in allaying students’ fears of this learning approach. Course coordinators, deans, and department chairs should discuss the new teaching format with student advisory groups prior to implementation. These informational meetings ideally should be accomplished prior to initiating a TBL course. Long-term benefits gained by using TBL in a professional curriculum can be explained and examples of successful TBL programs in other health-related fields can be shared. To improve buy-in, one can consider incorporating practice opportunities for students to engage in TBL efforts using nonpharmacy content (eg, RATs based on the school’s student handbook). Low-stakes practice activities can generate enthusiasm for and understanding of TBL as an effective learning technique.
Expectations regarding assessments of individual knowledge (eg, RATs, exams, peer assessments) should be explained during the initial information session. Involving students in deciding the relative weighting for each grade component is “…the most effective way to alleviate student concerns about grades.”9 On the first day of class, instructors should present all components of the grading scheme and provide a range limit on each component. After some discussion, student teams or team representatives should reach a “…mutually acceptable set of weights for each of the grade components.”9 These standards then are applied for all teams within a given course for the entire semester.
A period of adaptation and learning is expected for students and faculty members, which should be communicated to students. Regular feedback structures to enhance course development should be established. This can be achieved through various methods, such as using student focus groups or liaising with student advisory groups. Midpoint student evaluations of the course and/or of instructors can be incorporated to assure students their concerns are noted. Regardless of the methods, all feedback approaches should facilitate dialogue between students and faculty members. Establishing structures for feedback ahead of the course may help avoid emotional reactions from students.
Assessment of the Process, Course, and Program
The impact of TBL should be assessed at multiple levels and include analysis of student knowledge and problem-solving skills. Schools implementing a new TBL component may compare and contrast student performance with the prior curricular model. Basic knowledge acquisition and higher order pharmacotherapy skills can be compared through examination-item analyses of similar content and question types. Further, by mapping a curriculum or component back to curricular objectives, administrators are able to determine the success or failure of the new program to meet these objectives.
Schools that use a standardized approach to student evaluations (eg, tools for student ratings available through the IDEA center34 can compare changes in student responses to achieving relevant objectives, assessing the performance of the faculty members, and assessing overall course quality over time. Qualitative feedback from clinical preceptors can be particularly useful. Preceptors often are better able to assess a student’s knowledge deficits and problem-solving skills based on their level of interactions. They also may offer valuable insight on the general skills of a group of students participating in the TBL program compared with those educated with the previous curriculum. This anecdotal evidence can be quantified through a structured survey or end-of-program evaluation. Finally, though not always the ultimate goal, student success on standardized licensure examinations [eg, the North American Pharmacist Licensure Examination (NAPLEX)] can provide data regarding knowledge acquisition.
The transferability of TBL to other programs requires an assessment of the program's resources and, depending on the level of integration, the acceptability of this approach for faculty members and students, as well as any staff engagement necessary to support TBL activities. Using Bolman and Deal’s 4 leadership frames (structural, political, human resources, and symbolic frames), institutions can systematically approach an assessment of the feasibility of TBL.35
From a structural perspective, the current curricular model may either help or hinder application of TBL. Moreover, it might be more easily integrated into curricula that offer extended hours of teaching in one course (usually 3 or more hours per teaching session), to more easily incorporate all TBL activities in one session and have adequate time for meaningful discussion between students and faculty members. From a political perspective, it might be useful for administrators seeking to convert their curriculum to TBL to engage faculty members and identify champions of the idea and where resistance to TBL exists through open conversations about the pros and cons of TBL.
Discussions about whether to start TBL in specific courses or have a complete curricular revision using TBL approaches should be done strategically and should be inclusive and open to faculty concerns. Strategic and intentional faculty development and student support sessions would also be needed to help faculty members and students transition through this curricular change.36 One method could be a presentation about TBL’s benefits and challenges, as well as a defined statement from the program about how TBL will shape the roles and identities of faculty members and students within the program so faculty can readily be seen as facilitators of learning, and students are prepared to engage collaboratively in their own development. Consistent use of readiness assessments can demonstrate the value the program places on proactive student-centered learning. The omission of lecture-heavy sessions in TBL also communicates how much the program values meaningful dialogue between students and faculty members. Program administrators and faculty members wishing to adopt this must consider their available resources, the philosophy and feelings of other faculty members and students, and the implications TBL might have on expectations of students and faculty members.
CONCLUSION
Team-based learning is an effective teaching strategy for faculty members wishing to increase student engagement, active learning, and discussion in the classroom. It has been evaluated in various curricular models in pharmacy education and other disciplines. Through RAP, students better understand instructors’ expectations, arrive to class prepared for discussion, and become active participants in their learning within the framework of a team. Using TBL allows students to apply foundational knowledge to practice-based scenarios per the 2016 ACPE Accreditation Standards2 and directly integrates CAPE Educational Outcomes into the curriculum, as well.6 Investment is required in the areas of faculty development efforts about how to effectively use TBL, manage student expectations with a new teaching strategy, and provide methods for facilitating team dynamics to ensure proper implementation. Team-based learning activities should be regularly and effectively assessed to document progression and verify that desired end points are achieved. To meaningfully measure effectiveness of any curricular change, faculty members, student, and course assessment metrics must be considered in shaping future iterations of TBL.
ACKNOWLEDGMENTS
The authors wish to thank the following colleagues for their collaborations: Linda Farho, Brenda Gleason, Micheline A. Goldwire, Sarah E. Grady, June F. Johnson, Katie McClendon, Marianne McCollum, and Suzanne Rabi.
REFERENCES
- 1.Michaelsen LK, Knight AB, Fink LD. Team-Based Learning: A Transformative Use of Small Groups in College Teaching. Sterling, VA: Stylus Publishing; 2004. [Google Scholar]
- 2.Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Standards 2016. Released February 2, 2015. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf. Accessed March 17, 2015.
- 3.Page RL, Hume AL, Trujillo JM, et al. Interprofessional education: principles and application. A framework for clinical pharmacy. Pharmacotherapy. 2009;29(3):145e–164e. [Google Scholar]
- 4.World Health Organization. Geneva: Switzerland. Department of Human Resources for Health; 2010. Framework for action on interprofessional education and collaborative practice.http://www.who.int/hrh/resources/framework_action/en/ [Google Scholar]
- 5.Considine J, Currey J, Payne R, Williamson S. Participant evaluation of team-based learning using one-off teams in a hospital setting. Australas Emerg Nurs J. 2014;17(2):68–76. doi: 10.1016/j.aenj.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Center for Advancement of Pharmacy Education. Educational outcomes 2013. http://www.aacp.org/documents/CAPEoutcomes071213.pdf. Accessed March 19 2015.
- 7.Koles PG, Stolfi A, Borges NJ, Nelson S, Parmelee DX. The impact of team-based learning on medical students’ academic performance. Acad Med. 2010;85(11):1739–1745. doi: 10.1097/ACM.0b013e3181f52bed. [DOI] [PubMed] [Google Scholar]
- 8.Parmelee D, Michaelsen LK. Team-based learning: it’s here and it works! Acad Med. 2010;85(11):1658–1659. doi: 10.1097/ACM.0b013e3181f55a35. [DOI] [PubMed] [Google Scholar]
- 9.Michealsen LK, Parmalee DX, McMahon KK, Levine RE.Team-based learning for health professions education: A guide to using small groups for improving learning. Sterling, VA: Stylus Publishing; 2008. [Google Scholar]
- 10.Michaelsen LK, Sweet M, Parmelee DX. Team-based learning: Small group learning’s next big step. San Francisco, CA: Jossey-Bass, 2008 No. 116. Print.
- 11.Grady SE. Team-based learning in pharmacotherapeutics. Am J Pharm Educ. 2011;75(7) doi: 10.5688/ajpe757136. Article 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Letassy NA, Fugate SE, Medina MS, Stroup JS, Britton ML. Using team-based learning in an endocrine module taught across two campuses. Am J Pharm Educ. 2008;72(5) doi: 10.5688/aj7205103. Article 103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michaelsen LK, Sweet M. Team-based learning. New Directions for Teaching and Learning. 2011;128:41–51. doi: 10.1002/tl.467. [DOI] [Google Scholar]
- 14.Conway SE, Johnson JL, Ripley TL. Integration of team-based learning strategies into a cardiovascular module. Am J Pharm Educ. 2010;74(2) doi: 10.5688/aj740235. Article 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robinson DH, Schraw G. Recent Innovations in Educational Technology that Facilitate Student Learning. Greenwich, CT: Information Age Publishing; 2008. [Google Scholar]
- 16.Robinson D, Walker J. Technological alternatives to paper-based components of team-based learning. New Directions for Teaching and Learning. 2008;116:79–85. [Google Scholar]
- 17.Sibley J, Parmelee DX. Knowledge is no longer enough: enhancing professional education with team-based learning. New Directions for Teaching and Learning. 2008;116:41–53. [Google Scholar]
- 18.Wilkerson L. Tutors and small groups in problem-based learning: lessons from the literature. New Directions for Teaching and Learning. 1996;68:23–32. [Google Scholar]
- 19.Raelin JA. The role of facilitation in praxis. Organizational Dynamics. 2008;35(1):83–95. [Google Scholar]
- 20.Lane DR. Teaching skills for facilitating team-based learning. New Directions for Teaching and Learning. 2008;116:55–68. [Google Scholar]
- 21.Jaques D. ABC of learning and teaching in medicine: teaching small groups. BMJ. 2003;326:492–494. doi: 10.1136/bmj.326.7387.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michaelsen L, Sweet M. Team-based learning. Thriving in Academe. 2008;25(6):5–8. [Google Scholar]
- 23.Michaelsen LK, Sweet M. The essential elements of team-based learning. New Directions for Teaching and Learning. 2008;116:7–27. [Google Scholar]
- 24. Bailey ML, Luetkehans L. Ten great tips for facilitating virtual learning teams. In: Distance Learning ’98. Proceedings of the Annual Conference on Distance Teaching and Learning (14th, Madison, WI, August 5-7, 1998).
- 25.Druskat VW, Wollf SB. Building the emotional intelligence of groups. Harv Bus Rev. 2001;79(3):80–90. 164. [PubMed] [Google Scholar]
- 26.Centre for Teaching Excellence. Facilitating effective discussions. https://uwaterloo.ca/centre-for-teaching-excellence/teaching-resources/teaching-tips/alternatives-lecturing/discussions/facilitating-effective-discussions . Accessed: January 31, 2012.
- 27.Results Through Training. Tips for team facilitators. http://www.rttworks.com/%7Erttworks/www.rttworks.com/images/downloads/TipsFacil.HTML . Accessed January 31, 2012.
- 28.Weiss J, Hughes J. Want collaboration? Accept – and actively manage – conflict. Harv Bus Rev. 2005;83(3):92–101. 149. [PubMed] [Google Scholar]
- 29.Pelley JW, McMahon KK. Chapter 8: Facilitator Skills. In: Michaelsen LK, Parmelee DX, McMahon KK, Levine RE, editors. Team-Based Learning for Health Professions Education. Sterling, VA: Stylus Publishing; 2008. pp. 99–102. [Google Scholar]
- 30.Karau SJ, Williams KD. Social loafing: A meta-analytic review and theoretical integration. J Person and Social Psych. 1993;65(4):681–706. [Google Scholar]
- 31.Michaelsen LK, Knight AB, Fink LD. Team-Based Learning: A Transformative Use of Small Groups. Westport, CT: Praeger Publishers; 2002. [Google Scholar]
- 32.Basheti IA, Ryan G, Woulfe J, Bartimote-Aufflick K. Anonymous peer assessment of medication management reviews. Am J Pharm Educ. 2010;74(5) doi: 10.5688/aj740577. Article 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O’Brien CE, Franks AM, Stowe CD. Multiple rubric-based assessments of student case presentations. Am J Pharm Educ. 2008;72(3) doi: 10.5688/aj720358. Article 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The IDEA Center. http://www.theideacenter.org/ . Accessed February 8, 2012.
- 35.Bolman LG, Deal TE. Reframing Organizations: Artistry, Choice and Leadership. 3rd ed. Hoboken, NJ: John Wiley & Sons; 2007. [Google Scholar]
- 36.Kotter JP.Leading change: why transformation efforts fail Harvard Bus RevHarvard Business School1995 [Google Scholar]