Abstract
Background
Acute kidney injury (AKI) occurs frequently and adversely affects patient and kidney outcomes, especially when its severity increases from stage 1 to stages 2 or 3. Early interventions may counteract such deterioration, but this requires early detection. Our aim was to evaluate whether the novel renal damage biomarker urinary chitinase 3-like protein 1 (UCHI3L1) can detect AKI stage ≥2 more early than serum creatinine and urine output, using the respective Kidney Disease | Improving Global Outcomes (KDIGO) criteria for definition and classification of AKI, and compare this to urinary neutrophil gelatinase-associated lipocalin (UNGAL).
Methods
This was a translational single-center, prospective cohort study at the 22-bed surgical and 14-bed medical intensive care units (ICU) of Ghent University Hospital. We enrolled 181 severely ill adult patients who did not yet have AKI stage ≥2 based on the KDIGO criteria at time of enrollment. The concentration of creatinine (serum, urine) and CHI3L1 (serum, urine) was measured at least daily, and urine output hourly, in the period from enrollment till ICU discharge with a maximum of 7 ICU-days. The concentration of UNGAL was measured at enrollment. The primary endpoint was the development of AKI stage ≥2 within 12 h after enrollment.
Results
After enrollment, 21 (12 %) patients developed AKI stage ≥2 within the next 7 days, with 6 (3 %) of them reaching this condition within the first 12 h. The enrollment concentration of UCHI3L1 predicted the occurrence of AKI stage ≥2 within the next 12 h with a good AUC-ROC of 0.792 (95 % CI: 0.726–0.849). This performance was similar to that of UNGAL (AUC-ROC of 0.748 (95 % CI: 0.678–0.810)). Also, the samples collected in the 24-h time frame preceding diagnosis of the 1st episode of AKI stage ≥2 had a 2.0 times higher (95 % CI: 1.3–3.1) estimated marginal mean of UCHI3L1 than controls. We further found that increasing UCHI3L1 concentrations were associated with increasing AKI severity.
Conclusions
In this pilot study we found that UCHI3L1 was a good biomarker for prediction of AKI stage ≥2 in adult ICU patients.
Electronic supplementary material
The online version of this article (doi:10.1186/s13054-016-1192-x) contains supplementary material, which is available to authorized users.
Keywords: Acute kidney injury, Biological markers, Chitinase, Intensive care, Lipocalins
Background
Acute kidney injury (AKI) occurs in approximately half of adult critically ill patients [1–9]. Besides its recognized adverse effect on individual patient outcomes, both in the short- and long-term [1, 2, 4–10], AKI causes an important socioeconomic burden ensuing from its relationship with the development of chronic kidney disease (CKD) [11], and end-stage renal disease requiring renal replacement therapy (RRT) [12].
Current diagnostic and staging criteria for AKI were defined by the Kidney Disease | Improving Global Outcomes (KDIGO) AKI work group (Additional file 1: Table S1) and require monitoring of two surrogate glomerular filtration rate (GFR) markers, i.e., serum creatinine (SCr) and urine output (UO), and of the intervention RRT [13]. As renal stress and damage to the kidneys precede the observed decline in GFR [14], diagnostic AKI biomarker research in the last decade has focused on detection of these early signals [15–17]. Studies have shown that urinary biomarkers like neutrophil gelatinase-associated lipocalin (NGAL) [18–22], and recently the panel tissue inhibitor of metalloproteinases 2 (TIMP-2) and insulin-like growth factor-binding protein 7 (IGFBP7) [21, 23, 24], can detect AKI in critically ill patients earlier than SCr or UO, even when using the most sensitive KDIGO criteria. In addition, these biomarkers may also allow detection of other outcomes such as progression of AKI, use of RRT, development of CKD, and long-term mortality [25, 26]. The complexity of the AKI syndrome and the interest in detecting other outcomes highly warrants evaluation of yet further candidate renal stress or damage biomarkers aiming to find either complementary or - less realistically - truly superior ones.
Recently, our group discovered chitinase 3-like protein 3 (CHI3L3) as a novel candidate biomarker for sepsis-induced AKI, by urinary proteomics [27–29]. Validation with western blot analysis confirmed the presence of CHI3L3 in urine of septic mice with AKI, and its absence in urine of septic mice without AKI. In view of translational research [30], two other members of the number-18 glycoside hydrolase-family [31], i.e., chitinase 3-like protein 1 (CHI3L1) and acidic mammalian chitinase (CHIA), showed similar results. Subsequently, we found that CHI3L1 measured in urine was more discriminative for the presence of AKI in human septic patients than CHIA [28].
The number-18 glycoside hydrolase-family is special in that it comprises catalytically inactive proteins such as chitinase-like proteins (CLP, e.g., CHI3L1) in addition to catalytically active proteins such as chitinases [31]. These CLPs function as lectins because they can bind, but not hydrolyze, the glycan chitin, and therefore, represent the chi-lectin subfamily [32, 33].
The objective of this study was first to evaluate the diagnostic performance of the urinary biomarker CHI3L1 for early detection of AKI stage ≥2 in adult critically ill patients, and then to compare this performance to that of NGAL, which was chosen as the reference urinary biomarker.
Methods
We followed recommendations for strengthening the reporting of observational studies in epidemiology (STROBE) (Additional file 1: Table S2) [34]. Details of the methods are provided in Additional file 1: Text S1 and Tables S3A-F. The methods for additional analyses not included in the manuscript are provided in Additional file 1: Text S2 and Tables S4A and B.
We will refer to AKI that was diagnosed and classified by KDIGO as AKISCr/UO, while AKISCr will imply that the KDIGO UO criteria were discarded.
Study population
We conducted a prospective cohort study at the 22-bed surgical and 14-bed medical intensive care units (ICU) of Ghent University Hospital from September 2012 till August 2014. The inclusion and exclusion criteria are shown in Table 1.
Table 1.
Inclusion and exclusion criteria of the study
| Inclusion criteria | Exclusion criteria |
|---|---|
| Age ≥18 y | AKISCr/UO stage ≥2 at time of enrollmenta |
| Presence of both arterial and urinary catheter | |
| Expected ICU stay ≥48 h | |
| Respiratory SOFA score ≥2 (PaO2/FiO2 < 300) or cardiovascular SOFA score ≥1 (MAP <70 mmHg or on vasopressor(s) for at least 1 h) | CKD KDOQI stage 5 (GFR <15 ml/min/1.73 m2 or RRT)b |
| Written informed consent |
aBased on the Kidney Disease | Improving Global Outcomes (KDIGO) serum creatinine (SCr) or urine output (UO) criteria for acute kidney injury (AKI). bKidney Disease Outcomes Quality Initiative (KDOQI) [62]. CKD chronic kidney disease, FiO 2 fraction of inspired oxygen, GFR glomerular filtration rate, ICU intensive care unit, MAP mean arterial pressure, PaO 2 partial pressure of oxygen in arterial blood, RRT renal replacement therapy, SOFA Sepsis-related Organ Failure Assessment
Ethics, consent and permissions
This study was approved by the Ethical Committee of the Ghent University Hospital (Belgian registration number of the study: B670201213147), and conducted in accordance with the declaration of Helsinki and in compliance with the Good Clinical Practice Guidelines. All patients or their legally authorized representatives provided written informed consent.
Sample collection, sample handling, and data collection
Blood and urine were collected at enrollment. The large majority of patients i.e., 89 % was enrolled on either the first (28 %) or second (61 %) ICU day, while the minority i.e., 11 % was enrolled on either the third (9 %) or fourth (2 %) ICU day. Each subject was sampled a second time on the day of enrollment (d1) at 6 pm if the first collection was before noon. The subsequent sampling times were at 6 am and 6 pm on d2–4, and at 6 am on d5–7 (Additional file 1: Table S3A). This is similar to the methodology used in the hallmark study by Kashani et. al. [21]. If the patient was discharged from the ICU before d7, the study stopped.
These paired blood and urine samples were collected by standard methods and centrifuged by standard protocols. Serum and urine supernatants were stored at −80 °C and thawed at room temperature immediately prior to analysis. Clinical data needed to complete the individual clinical research files were extracted from the hospital records by study coordinators. Clinical data and samples were anonymized. JDL had access to the anonymized SCr and serum C-reactive protein data in order to determine the appropriate sample dilution for CHI3L1 measurement by enzyme-linked immunosorbent assay (ELISA) (Additional file 1: Table S3B). All other technicians were blinded to clinical data.
Biomarker measurements
Creatinine and urinary NGAL (UNGAL) analyses were performed externally. Creatinine concentrations were measured with a kinetic rate-blanked Jaffé assay (commercial reagents, Roche Diagnostics, Basel, Switzerland) on a Cobas c502, while UNGAL concentrations were measured with a particle-enhanced turbidimetric immunoassay (ST001-3CA, BioPorto, Hellerup, Denmark) on a Modular P. The concentration of CHI3L1 was determined in-house with a sandwich ELISA (DC3L10, R&D Systems, Minneapolis, MN, USA).
Both urinary CHI3L1 (UCHI3L1) and UNGAL concentrations were statistically analyzed as such and after correction for urine dilution by using the ratio to urinary creatinine (UCr). The relative change in SCr measured at enrollment was defined as the ratio of the enrollment SCr to reference SCr. The UO after enrollment, defined as the mean UO in the first valid 6-h period after enrollment, was determined as the mean of the 6 UO values that were calculated each h in the first valid 6-h period after enrollment.
Primary endpoint
The primary endpoint of the study was the development of AKISCr/UO stage ≥2 within 12 hours (h) after enrollment (Additional file 1: Table S1). Reference SCr was defined as the lowest SCr value within the last 3 months (mo) prior to enrollment. The details for calculation of UO are outlined in Additional file 1: Text S1.
Secondary endpoints
Secondary endpoints of the study were: AKISCr/UO stage ≥2 within 24 h and 7 days after enrollment; AKISCr stage ≥2 within 12 h, 24 h and 7 days after enrollment (Additional file 1: Table S1).
UCHI3L1 response to AKI
We compared samples that were collected in the 24 h preceding diagnosis of the first episode of AKISCr/UO stage ≥2 to those that were not followed by a first episode of AKISCr/UO stage ≥2 within the next 24 h. For this analysis, we excluded all samples collected in the period starting from diagnosis of the first episode of AKISCr/UO stage ≥2 till the end of the study.
For all 21 patients who developed AKISCr/UO stage ≥2 (reference time 0 h) within 7 days after enrollment, we documented the UCHI3L1 concentrations corresponding with the time points 24 h before, 12 h before, 12 h after, and 24 h after diagnosis of the first episode of AKISCr/UO stage ≥2. This allowed us to investigate the distribution of UCHI3L1 over time in patients with AKISCr/UO stage ≥2.
We also studied the distribution of UCHI3L1 in samples corresponding with different stages of severity of AKISCr/UO. If the total study period of 7 days was completed, 11 serum and 11 urine samples were available per ICU patient. All available UCHI3L1 concentrations were classified according to their AKISCr/UO stage at that moment. As such, UCHI3L1 concentrations were divided into four groups: no AKISCr/UO at the time of sampling, and AKISCr/UO stages 1, 2, or 3 at the time of sampling.
Statistical analysis
The primary analysis was based on comparison of the areas under the receiver-operating characteristics curves (AUC-ROC) of UCHI3L1 with those of UNGAL for predicting the defined endpoints, which was performed in MedCalc 15.2.1 (MedCalc Software, Oostende, Belgium). We also calculated Spearman’s coefficients of rank correlation with this program. In SPSS 22 (IBM, Armonk, NY, USA) we performed (1) mixed model analysis with log10(UCHI3L1) as the outcome variable; diagnosis of the first episode of AKISCr/UO stage ≥2 within 24 h after sampling, as the predictor variable; and patient as the random factor; (2) Fisher’s exact or the chi-square test - the 95 % confidence interval (CI) of a proportion was calculated with the Wilson procedure without correction for continuity [35, 36] - and the Mann–Whitney U test; (3) the Wilcoxon matched-pair signed-rank test; and (4) related-samples Friedman’s two-way analysis of variance by ranks. Box and whisker plots were generated in GraphPad Prism 5 (GraphPad Software, San Diego, CA, USA). For all analyses, two-sided P values <0.05 were considered statistically significant.
In Additional file 1: Text S1 and Tables S3C-F, we provide all details and also describe how the urinary biomarkers were introduced into the statistical programs.
Results
The results of additional analyses not included in the manuscript are provided in Additional file 1: Text S2 and Tables S4C-I, Additional file 2: Figure S1, Additional file 3: Figure S2, Additional file 4: Figure S3, and Additional file 5: Figure S4.
Patient characteristics and event rates
The patient flow diagram is presented in Fig. 1. Of the 190 enrolled patients in our study cohort, 9 already fulfilled the SCr criteria for AKI stage 2 at enrollment and were therefore excluded. In this analysis cohort (n = 181), 21 patients (12 %) developed AKISCr/UO stage ≥2 within 7 days after enrollment. Within 24 h AKISCr/UO stage ≥2 was met by 9 patients (5 %) and within 12 h by 6 patients (3 %). In Table 2 the demographic information for these patients, either meeting or missing the primary endpoint, is depicted. Baseline characteristics were similar between both groups with the exception of an older age and a higher proportion of elective surgery in patients who developed AKISCr/UO stage ≥2 within 12 h after enrollment. In Table 3 the distribution of patients over different SCr and UO AKI stages that were maximally reached within 12 h, 24 h and 7 days after enrollment is shown.
Fig. 1.
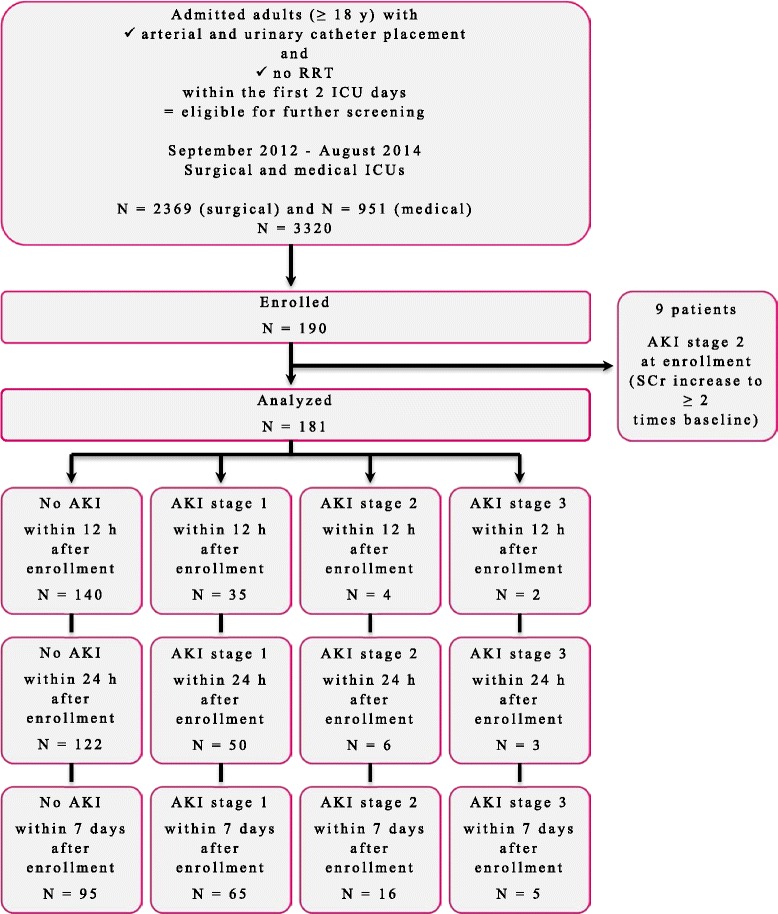
Flow diagram of the patient selection. Acute kidney injury (AKI) was defined and classified based on the Kidney Disease | Improving Global Outcomes serum creatinine (SCr) or urine output criteria. ICU intensive care unit, RRT renal replacement therapy, y year
Table 2.
Demographic information for patients of the analysis cohort
| All patients | AKISCr/UO stage ≥ 2a | No AKISCr/UO stage ≥ 2a | P value | |
|---|---|---|---|---|
| All patients | 181 (100 %) | 6 (3.3 %) | 175 (96.7 %) | NA |
| (1.5–7.0 %) | (93.0–98.5 %) | |||
| Baseline characteristics | ||||
| Sex, male | 114 (63.0 %) | 4 (66.7 %) | 110 (62.9 %) | 1.000 |
| (55.7–69.7 %) | (30.0–90.3 %) | (55.5–69.7 %) | ||
| Ageb, y | 60.0 (51.0–70.0) | 70.5 (65.8–78.0) | 59.0 (50.0–70.0) | 0.040 |
| Race, white | 181 (100 %) | 6 (100 %) | 175 (100 %) | NA |
| (97.9–100 %) | (61.0–100 %) | (97.9–100 %) | ||
| Body mass index | 24 (22–28) | 25 (23–28) | 24 (22–28) | 0.594 |
| Reference renal function | ||||
| SCr (mg/dl) | 0.66 (0.52–0.79) | 0.64 (0.55–0.69) | 0.66 (0.51–0.79) | 0.660 |
| eGFRMDRD (ml/min/1.73 m2) | 119 (89–150) | 120 (105–134) | 119 (89–153) | 0.975 |
| eGFRCKD-EPI (ml/min/1.73 m2) | 102 (89–118) | 98 (92–102) | 103 (89–118) | 0.392 |
| Diabetes mellitus | 0.787 | |||
| Type I | 2 (1.1 %) | 0 (0.0 %) | 2 (1.1 %) | |
| (0.3–3.9 %) | (0.0–39.0 %) | (0.3–4.1 %) | ||
| Type II | 11 (6.1 %) | 0 (0.0 %) | 11 (6.3 %) | |
| (3.4–10.6 %) | (0.0–39.0 %) | (3.5–10.9 %) | ||
| Heart failure | 1.000 | |||
| NYHA class I | 179 (98.9 %) | 6 (100 %) | 173 (98.9 %) | |
| (96.1–99.7 %) | (61.0–100 %) | (95.9–99.7 %) | ||
| NYHA class II | 2 (1.1 %) | 0 (0.0 %) | 2 (1.1 %) | |
| (0.3–3.9 %) | (0.0–39.0 %) | (0.3–4.1 %) | ||
| NYHA class III | 0 (0.0 %) | 0 (0.0 %) | 0 (0.0 %) | |
| (0.0–2.1 %) | (0.0–39.0 %) | (0.0–2.1 %) | ||
| NYHA class IV | 0 (0.0 %) | 0 (0.0 %) | 0 (0.0 %) | |
| (0.0–2.1 %) | (0.0–39.0 %) | (0.0–2.1 %) | ||
| Myocardial infarction or cardiac arrestc | 17 (9.4 %) | 0 (0.0 %) | 17 (9.7 %) | 1.000 |
| (5.9–14.5 %) | (0.0–39.0 %) | (6.2–15.0 %) | ||
| Malignancyc | 17 (9.4 %) | 1 (16.7 %) | 16 (9.1 %) | 0.451 |
| (5.9–14.5 %) | (3.0–56.4 %) | (5.7–14.3 %) | ||
| ICU admission | ||||
| Referred from | 0.063 | |||
| Other hospital | 42 (23.2 %) | 0 (0.0 %) | 42 (24.0 %) | |
| (17.7–29.9 %) | (0.0–39.0 %) | (18.3–30.8 %) | ||
| Emergency room | 75 (41.4 %) | 1 (16.7 %) | 74 (42.3 %) | |
| (34.5–48.7 %) | (3.0–56.4 %) | (35.2–49.7 %) | ||
| Operating room | 21 (11.6 %) | 1 (16.7 %) | 20 (11.4 %) | |
| (7.7–17.1 %) | (3.0–56.4 %) | (35.8–50.3 %) | ||
| Floor | 43 (23.8 %) | 4 (66.7 %) | 39 (22.3 %) | |
| (18.1–30.5 %) | (30.0–90.3 %) | (16.8–29.0 %) | ||
| Reason | 0.038 | |||
| Medical | 108 (59.7 %) | 3 (50.0 %) | 105 (60.0 %) | |
| (52.4–66.5 %) | (18.8–81.2 %) | (52.6–67.0 %) | ||
| Elective surgery | 13 (7.2 %) | 2 (33.3 %) | 11 (6.3 %) | |
| (4.2–11.9 %) | (9.7–70.0 %) | (3.5–10.9 %) | ||
| Urgent surgery | 60 (33.1 %) | 1 (16.7 %) | 59 (33.7 %) | |
| (26.7–40.3 %) | (3.0–56.4 %) | (27.1–41.0 %) | ||
| First day of study | ||||
| SOFA score (points) | 9 (7–11) | 11 (8–16) | 9 (7–11) | 0.189 |
| Mechanical ventilation | 122 (67.4 %) | 5 (83.3 %) | 117 (66.9 %) | 0.665 |
| (60.3–73.8 %) | (43.6–97.0 %) | (59.6–73.4 %) | ||
| Vasopressors | 117 (64.6 %) | 4 (66.7 %) | 113 (64.6 %) | 1.000 |
| (57.4–71.2 %) | (30.0–90.3 %) | (57.2–71.3 %) | ||
| Infection | 153 (84.5 %) | 6 (100 %) | 147 (84.0 %) | 0.592 |
| (78.6–89.1 %) | (61.0–100 %) | (77.8–88.7 %) | ||
| Infection ++d | 122 (67.4 %) | 6 (100 %) | 116 (66.3 %) | 0.179 |
| (60.3–73.8 %) | (61.0–100 %) | (59.0–72.9 %) | ||
| Nephrotoxic drugs (before or at the first study day) | ||||
| ACE inhibitors | 25 (13.8 %) | 1 (16.7 %) | 24 (13.7 %) | 0.596 |
| (9.5–19.6 %) | (3.0–56.4 %) | (9.4–19.6 %) | ||
| ARBs | 5 (2.8 %) | 0 (0.0 %) | 5 (2.9 %) | 1.000 |
| (1.2–6.3 %) | (0.0–39.0 %) | (1.2–6.5 %) | ||
| Iodinated contrast media | 81 (44.8 %) | 2 (33.3 %) | 79 (45.1 %) | 0.693 |
| (37.7–52.0 %) | (9.7–70.0 %) | (38.0–52.5 %) | ||
| Aminoglycosides | 6 (3.3 %) | 0 (0.0 %) | 6 (3.4 %) | 1.000 |
| (1.5–7.0 %) | (0.0–39.0 %) | (1.6–7.3 %) | ||
| Vancomycine | 15 (8.3 %) | 0 (0.0 %) | 15 (8.6 %) | 1.000 |
| (5.1–13.2 %) | (0.0–39.0 %) | (5.3–13.7 %) | ||
| Diuretics | 45 (24.9 %) | 3 (50.0 %) | 42 (24.0 %) | 0.164 |
| (19.1–31.6 %) | (18.8–81.2 %) | (18.3–30.8 %) | ||
| Tacrolimus | 2 (1.1 %) | 1 (16.7 %) | 1 (0.6 %) | 0.065 |
| (0.3–3.9 %) | (3.0–56.4 %) | (0.1–3.2 %) | ||
| Cyclosporine | 1 (0.6 %) | 0 (0.0 %) | 1 (0.6 %) | 1.000 |
| (0.1–3.1 %) | (0.0–39.0 %) | (0.1–3.2 %) | ||
| NSAIDs (chronic) | 10 (5.5 %) | 1 (16.7 %) | 9 (5.1 %) | 0.292 |
| (3.0–9.9 %) | (3.0–56.4 %) | (2.7–9.5 %) | ||
| Corticosteroids (chronic) | 24 (13.3 %) | 1 (16.7 %) | 23 (13.1 %) | 0.580 |
| (9.1–19.0 %) | (3.0–56.4 %) | (8.9–18.9 %) | ||
aWithin 12 h after enrollment (primary endpoint); based on the Kidney Disease | Improving Global Outcomes (KDIGO) serum creatinine (SCr) or urine output (UO) criteria for acute kidney injury (AKI). bDetermined at the first day of the study. cAt time of hospital or ICU admission. dSuspected bacterial infection, either leading to arterial hypotension or organ dysfunction, or leading to shock (Additional file 1: Table S4A). Data represent number (%) (95 % CI) and median (IQR) for categorical and continuous variables, respectively. ACE angiotensin converting enzyme, ARB angiotensin-II receptor blocker, CI confidence interval, CKD-EPI Chronic Kidney Disease Epidemiology Collaboration, eGFR estimated glomerular filtration rate, ICU intensive care unit, IQR interquartile range, MDRD Modification of Diet in Renal Disease, NSAID nonsteroidal anti-inflammatory drug, NYHA New York Heart Association, SOFA Sepsis-related Organ Failure Assessment
Table 3.
Distribution of patients over different KDIGO serum creatinine and urine output acute kidney injury stages maximally reached within indicated observation periods
| Time window | Maximum AKI stage Number (%) | UO 0a | UO 1a | UO 2a | UO 3a | Total in row |
|---|---|---|---|---|---|---|
| 12 h | SCr 0a | 140 (77) | ░ 11 (6) | ▒ 2 (1) | ▓ 0 (0) | 153 (85) |
| 24 h | 122 (67) | ░ 19 (10) | ▒ 4 (2) | ▓ 0 (0) | 145 (80) | |
| 7 days | 95 (52) | ░ 23 (13) | ▒ 2 (1) | ▓ 0 (0) | 120 (66) | |
| 12 h | SCr 1a | ░ 21 (12) | ░ 3 (2) | ▒ 0 (0) | ▓ 0 (0) | 24 (13) |
| 24 h | ░ 27 (15) | ░ 4 (2) | ▒ 0 (0) | ▓ 0 (0) | 31 (17) | |
| 7 days | ░ 35 (19) | ░ 7 (4) | ▒ 3 (2) | ▓ 0 (0) | 45 (25) | |
| 12 h | SCr 2a | ▒ 1 (1) | ▒ 1 (1) | ▒ 0 (0) | ▓ 0 (0) | 2 (1) |
| 24 h | ▒ 0 (0) | ▒ 2 (1) | ▒ 0 (0) | ▓ 0 (0) | 2 (1) | |
| 7 days | ▒ 4 (2) | ▒ 4 (2) | ▒ 3 (2) | ▓ 0 (0) | 11 (6) | |
| 12 h | SCr 3a | ▓ 1 (1) | ▓ 1 (1) | ▓ 0 (0) | ▓ 0 (0) | 2 (1) |
| 24 h | ▓ 2 (1) | ▓ 1 (1) | ▓ 0 (0) | ▓ 0 (0) | 3 (2) | |
| 7 days | ▓ 4 (2) | ▓ 1 (1) | ▓ 0 (0) | ▓ 0 (0) | 5 (3) | |
| 12 h | Total in column | 163 (90) | 16 (9) | 2 (1) | 0 (0) | 181 (100) |
| 24 h | 151 (83) | 26 (14) | 4 (2) | 0 (0) | 181 (100) | |
| 7 days | 138 (76) | 35 (19) | 8 (4) | 0 (0) | 181 (100) |
Patients with different stages of severity of acute kidney injury (AKI) diagnosed and classified by the Kidney Disease | Improving Global Outcomes (KDIGO) serum creatinine (SCr) or urine output (UO) criteria (AKI SCr/UO) are marked with a different shaded rectangle: the darker this shade, the worse the kidney injury. a SCr 0 represents no AKI based on the KDIGOSCr criteria. Likewise, UO 0 represents no AKI based on the KDIGOUO criteria. SCr 1/2/3 represents AKI stage 1/2/3 based on the KDIGOSCr criteria. Likewise, UO 1/2/3 represents AKI stage 1/2/3 based on the KDIGOUO criteria
Biomarkers’ diagnostic performances
The biomarkers UCHI3L1 and UNGAL, both measured at enrollment, were good predictors of the development of AKISCr/UO stage ≥2 within the next 12 h, with an AUC-ROC of 0.792 (95 % CI: 0.726–0.849) for UCHI3L1 and 0.748 (0.678–0.810) for UNGAL (P = 0.587; Fig. 2). When UO criteria were discarded, these AUC-ROCs improved to 0.877 (0.820–0.921) for UCHI3L1 and 0.865 (0.807–0.911) for UNGAL (P = 0.661). Extending our prediction window to 24 h slightly decreased the AUC-ROC for both biomarkers for predicting AKISCr/UO stage ≥2, while the AUC-ROC for predicting AKISCr stage ≥2 remained similar (Fig. 2). In the 7-d prediction window both biomarkers became poor predictors of AKI stage ≥2, irrespective of the definition used. To obtain 2 explicit clinical phenotypes, the AUC-ROC analyses were repeated excluding AKI stage 1 (comparing AKI stage ≥2 with no AKI). These showed essentially unchanged results for UCHI3L1 and UNGAL, both measured at enrollment (Additional file 1: Table S5).
Fig. 2.
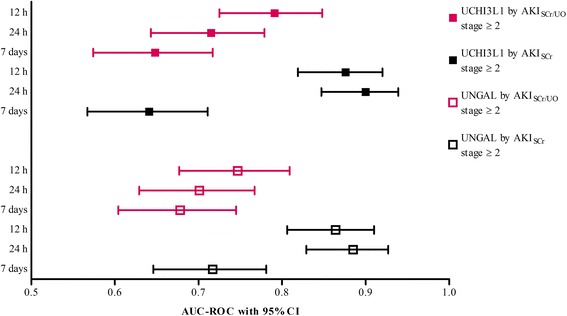
Area under the receiver-operating characteristics curve (AUC-ROC) with 95 % confidence interval (CI) for urinary chitinase 3-like protein 1 (UCHI3L1) and urinary neutrophil gelatinase-associated lipocalin (UNGAL) at enrollment for prediction of the six different endpoints. The P value for the difference in AUC-ROC between both biomarkers for predicting acute kidney injury (AKI) stage ≥2 based on the Kidney Disease | Improving Global Outcomes (KDIGO) serum creatinine (SCr) or urine output (UO) criteria (AKI SCr/UO) within 12 h after enrollment was 0.587. In the 24-h prediction window the P value was 0.823, and in the 7-d prediction window it was 0.522. Likewise, the P value for the difference in AUC-ROC between both biomarkers for predicting AKISCr stage ≥2 within 12 h after enrollment was 0.661. In the 24-h prediction window the P value was 0.495, and in the 7-d prediction window it was 0.099
Correction of the urinary biomarker concentrations for urine dilution by calculating the ratio to UCr, decreased the AUC-ROC for both biomarkers when diagnosing AKI stage ≥2 based on SCr or UO, while there was no difference observed when diagnosing AKI stage ≥2 based on SCr alone (Table 4).
Table 4.
Comparison of areas under the receiver-operating characteristics curves
| Biomarker measurement | Time window | AKISCr/UO stage ≥ 2a | AKISCr stage ≥ 2b | ||||
|---|---|---|---|---|---|---|---|
| AUC-ROC | 95 % CI | P valuec | AUC-ROC | 95 % CI | P valuec | ||
| Number = 181 | |||||||
| ▓ Enrollment UCHI3L1 | 12-h | ▓ 0.792 | ▓ 0.726–0.849 | ▓ 0.877 | ▓ 0.820–0.921 | ||
| 24-h | ▓ 0.716 | ▓ 0.644–0.780 | ▓ 0.901 | ▓ 0.848–0.940 | |||
|
|
Comparison with | ||||||
| Enrollment UCr-corrected UCHI3L1 | 12-h | 0.674 | 0.601–0.742 | 0.038 | 0.832 | 0.769–0.883 | 0.359 |
| 24-h | 0.587 | 0.511–0.659 | 0.005 | 0.861 | 0.802–0.908 | 0.308 | |
| Enrollment SCHI3L1 | 12-h | 0.645 | 0.570–0.714 | 0.071 | 0.784 | 0.717–0.842 | 0.300 |
| 24-h | 0.548 | 0.472–0.622 | 0.022 | 0.830 | 0.767–0.881 | 0.324 | |
| Enrollment SCr | 12-h | 0.624 | 0.549–0.695 | 0.113 | 0.732 | 0.662–0.795 | 0.363 |
| 24-h | 0.639 | 0.565–0.709 | 0.406 | 0.766 | 0.697–0.826 | 0.278 | |
| Enrollment SCr to reference SCr ratio | 12-h | 0.690 | 0.618–0.757 | 0.274 | 0.806 | 0.741–0.861 | 0.614 |
| 24-h | 0.695 | 0.622–0.761 | 0.784 | 0.847 | 0.786–0.896 | 0.622 | |
| ▓ Enrollment UNGAL | 12-h | ▓ 0.748 | ▓ 0.678–0.810 | ▓ 0.865 | ▓ 0.807–0.911 | ||
| 24-h | ▓ 0.702 | ▓ 0.630–0.768 | ▓ 0.886 | ▓ 0.830–0.928 | |||
|
|
Comparison with | ||||||
| Enrollment UCr-corrected UNGAL | 12-h | 0.622 | 0.547–0.693 | 0.007 | 0.795 | 0.729–0.851 | 0.123 |
| 24-h | 0.570 | 0.495–0.644 | 0.001 | 0.826 | 0.763–0.878 | 0.109 | |
| Number = 180d | |||||||
| ▓ Enrollment UCHI3L1 | 12-h | ▓ 0.791 | ▓ 0.724–0.848 | ▓ 0.876 | ▓ 0.819–0.921 | ||
| 24-h | ▓ 0.715 | ▓ 0.643–0.779 | ▓ 0.901 | ▓ 0.847–0.940 | |||
|
|
Comparison with | ||||||
| UO after enrollmente | 12-h | 0.833 | 0.771–0.885 | 0.728 | 0.759 | 0.690–0.820 | 0.034 |
| 24-h | 0.808 | 0.743–0.863 | 0.438 | 0.795 | 0.728–0.851 | 0.022 | |
aBased on the Kidney Disease | Improving Global Outcomes (KDIGO) serum creatinine (SCr) or urine output (UO) criteria for acute kidney injury (AKI). bBased on the KDIGO SCr criteria for AKI. cThe P value is shown for the difference in the area under the receiver-operating characteristics curve (AUC-ROC). We always compared with the AUC-ROC of the urinary biomarker (UCHI3L1 or UNGAL; marked with a shaded rectangle). dUO after enrollment could not be calculated in one patient. eDefined as the mean UO in the first valid 6-h period after enrollment (in ml/kg/h). CI confidence interval, SCHI3L1 serum chitinase 3-like protein 1, UCHI3L1 urinary chitinase 3-like protein 1, UCr urinary creatinine, UNGAL urinary neutrophil gelatinase-associated lipocalin
In contrast to UCHI3L1, serum CHI3L1 (SCHI3L1) measured at enrollment was a poor predictor of AKISCr/UO stage ≥2 within the next 12 h, with an AUC-ROC of 0.645 (0.570–0.714). In the 24-h prediction window SCHI3L1 did not predict AKISCr/UO stage ≥2. Again, when diagnosing based on SCr alone, the AUC-ROC for SCHI3L1 improved, i.e., 0.784 (0.717–0.842) in the 12-h and 0.830 (0.767–0.881) in the 24-h prediction window (Table 4).
We additionally studied the discriminatory ability of the individual KDIGO parameters, i.e., (relative change in) SCr measured at enrollment and UO after enrollment (Table 4). The AUC-ROC was similar for UCHI3L1, SCr and UO. However, UCHI3L1 performed better than UO when diagnosing AKI stage ≥2 based on SCr alone (P = 0.034 in the 12-h and 0.022 in the 24-h prediction window). In addition, compared to SCr, there was a clear trend towards a better AUC-ROC for UCHI3L1, especially when diagnosing AKI stage ≥2 based on SCr or UO within 12 h after enrollment.
Combining both urinary biomarkers as the two-biomarker panel [UCHI3L1]•[UNGAL] did not improve the diagnostic performance of each of these single biomarkers for predicting either the 12-h or 24-h endpoints (Table 5). A positive relationship between these markers was observed, with a Spearman’s coefficient of rank correlation of 0.615 (0.515–0.698) (Additional file 1: Table S6).
Table 5.
Comparison of AUC-ROC between the two-biomarker panel [urinary chitinase 3-like protein 1]•[urinary neutrophil gelatinase-associated lipocalin] and each of these single biomarkers
| Two-biomarker panel | Time window | AKISCr/UO stage ≥2a | AKISCr stage ≥2b | ||||
|---|---|---|---|---|---|---|---|
| AUC-ROC | 95 % CI | P value | AUC-ROC | 95 % CI | P value | ||
| Enrollment [UCHI3L1]•[UNGAL] | 12 h | 0.784 | 0.717–0.841 | 0.764c | 0.874 | 0.817–0.919 | 0.879c |
| 0.522d | 0.544d | ||||||
| 24 h | 0.721 | 0.650–0.785 | 0.856c | 0.899 | 0.845–0.939 | 0.877c | |
| 0.622d | 0.311d | ||||||
aBased on the Kidney Disease | Improving Global Outcomes (KDIGO) serum creatinine (SCr) or urine output (UO) criteria for acute kidney injury (AKI). bBased on the KDIGO SCr criteria for AKI. cDifference in the area under the receiver-operating characteristics curve (AUC-ROC) between the two-biomarker panel and urinary chitinase 3-like protein 1 (UCHI3L1), both measured at enrollment. dDifference in AUC-ROC between the two-biomarker panel and urinary neutrophil gelatinase-associated lipocalin (UNGAL), both measured at enrollment
With the Youden index a cutoff for UNGAL of 139 ng/ml was identified corresponding to the reference cutoff for this variable (>150 ng/ml [22]) (Additional file 1: Table S7).
UCHI3L1 response to AKI
Samples collected in the 24 h preceding diagnosis of the first episode of AKISCr/UO stage ≥2 had a 2.0 times higher (95 % CI: 1.3–3.1) estimated marginal mean of UCHI3L1 than those not followed by a first episode of AKISCr/UO stage ≥2 within the next 24 h. The general time–concentration profile of UCHI3L1 showed a trend for increasing concentrations from 24 h before, towards diagnosis of the first episode of AKISCr/UO stage ≥2 (reference time 0 h; Fig. 3). After reference time 0 h, median UCHI3L1 concentrations showed a decreasing trend.
Fig. 3.
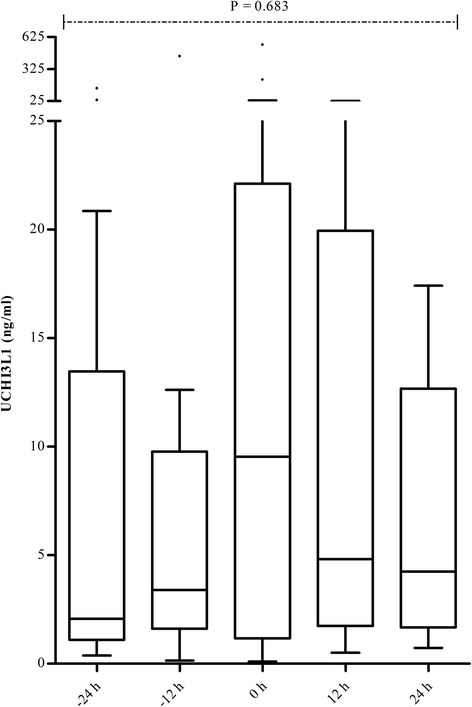
Distribution of urinary chitinase 3-like protein 1 (UCHI3L1) over time in patients who developed acute kidney injury (AKI) stage ≥2 based on the Kidney Disease | Improving Global Outcomes (KDIGO) serum creatinine (SCr) or urine output (UO) criteria (AKISCr/UO) within 7 days after enrollment. The reference time 0 h represents time of diagnosis of the first episode of AKISCr/UO stage ≥2. At time −24 h, a UCHI3L1 concentration was available for 14 of these 21 patients. Likewise, 13 values were available at time −12 h, 19 at reference time 0 h, 14 at time 12 h, and 12 at time 24 h
Samples corresponding with AKISCr/UO stage 1 at time of collection had higher UCHI3L1 concentrations than those corresponding with no AKISCr/UO at the time of collection (P <0.001) (Fig. 4). Stage 1 and stage 2 samples had similar UCHI3L1 concentrations (P = 0.514). Stage 3 samples again had higher UCHI3L1 concentrations than stage 2 samples (P <0.001).
Fig. 4.
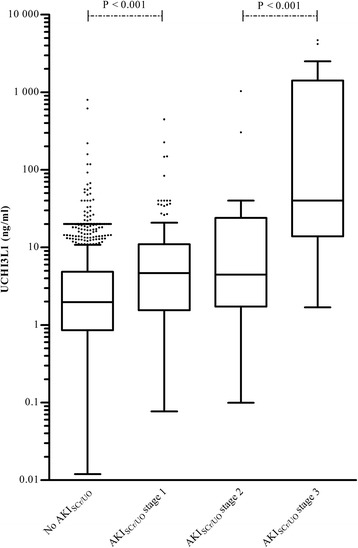
Distribution of urinary chitinase 3-like protein 1 (UCHI3L1) in samples corresponding with different stages of severity of acute kidney injury (AKI) based on the Kidney Disease | Improving Global Outcomes serum creatinine (SCr) or urine output (UO) criteria (AKI SCr/UO)
Discussion
We found that UCHI3L1 was a good biomarker for early detection of AKI stage ≥2 in adult critically ill patients admitted to an ICU, with a performance similar to that of UNGAL.
These findings may have important clinical and socioeconomic impact. Increasing severity of AKI is associated with increased risk of worse patient and kidney outcomes [1, 2, 4–10]. Importantly, observational and also intervention studies showed that early AKI management can counteract AKI deterioration, and is associated with lower mortality and less RRT dependence at discharge [37–44]. Consequently, even earlier identification of AKI using a biomarker may have a much stronger effect on these outcomes.
Both UCHI3L1 and UNGAL better predicted AKI stage ≥2 that was defined based on SCr alone versus based on SCr or UO. These two urinary proteins are biomarkers of renal stress or damage [45, 46], while SCr and UO are GFR surrogates. However, UO is much more sensitive to decline in GFR, and therefore is probably associated with less renal stress or damage than SCr, which is supported by studies reporting that UO-based AKI classes are associated with a lower ICU/hospital mortality than SCr-based ones [9, 47, 48]. This may explain the better AUC-ROCs when considering SCr alone for diagnosis. The findings by Macedo et al. [49], who reported similar ICU mortality for exclusively UO+ AKI patients (8.8 %) and (non)oliguric SCr+ AKI patients (10.4 %), appear contradictory to previous findings [9, 47, 48]. However, severity of AKI was greater in exclusively UO+ patients: >60 % of these patients were stage 2, while >70 % of the (non)oliguric SCr+ patients were stage 1 [49]. We also observed a partial overlap in UCHI3L1 between AKISCr/UO stage 1 and stage 2 samples, indicating heterogeneity of AKI severity within KDIGO classes, which can be partly explained by the different impact of meeting the defined criteria for either UO alone, or SCr alone, or both SCr and UO [9]. This could also clarify the decreased performance of UCHI3L1 and UNGAL at enrollment for prediction of AKISCr/UO stage ≥2 within the next 24 h. The majority of the extra AKISCr/UO stage ≥2 patients in the 24 h observation period fulfilled UO criteria only. These patients, therefore, probably had less renal stress or damage, and consequently a low biomarker signal. Another explanation could be that the hit leading to AKI is following the biomarker measurement. This may more likely occur when the observation period is longer [21].
The observation that the AUC-ROC for the individual KDIGO parameters, i.e., SCr and UO, were similar to those of UCHI3L1 for detection of AKI stage ≥2, warrants discussion. First, when comparing the AUC-ROC for UO and UCHI3L1, we must take into account that although the measurement of UO started at enrollment, it was only completed 6 h later than the time at which UCHI3L1 was measured. Second, renal stress or damage may not always be reflected by decline in GFR; vice versa, a decline in GFR may not always reflect renal stress or damage. This may lead to underestimation of the diagnostic performance of UCHI3L1 in our study.
We found a trend for increased UCHI3L1 concentrations in the 24 h preceding AKI, and for decreased concentrations afterwards. However, it should be emphasized that after meeting AKISCr/UO stage ≥2, the individual time–concentration profiles of AKISCr/UO differed widely between patients: some remained in the same severity stage, some deteriorated and others ameliorated (data not shown). The number of patients observed in this pilot study also precludes firm conclusions.
This is the first translational study demonstrating that UCHI3L1 predicts the occurrence of AKI stage ≥2 in adult critically ill patients [28]. Schmidt et al. independently showed that UCHI3L1 predicts the occurrence of delayed graft function in adult patients who receive deceased-donor kidney transplants [46]. In their preclinical study, these authors reported that the transcription of the CHI3L1 gene is significantly upregulated in the mouse kidney after ischemia/reperfusion (I/R) injury with increased excretion of its protein in urine. These mRNA and protein levels correlated with the degree of kidney injury and were at earliest measured on the first day after I/R, when SCr values had already peaked. Recently, the same group also studied a cohort of hospitalized patients who had AKI, and found that UCHI3L1 was associated with the composite outcome of AKI progression and in-hospital death [50].
We must speculate on the source of CHI3L1. Upon renal stress or damage, this protein is secreted by macrophages within the kidney [46], while NGAL is secreted by specific cells of the distal nephron [45]. Another source for the urine component of NGAL is the circulating plasma pool [51]. We speculate that the same is true for CHI3L1 as this protein has an apparent molecular weight of ±39–40 kDa [52, 53], and as within the group of patients with no AKI (in the 7-d prediction window) a concomitant very high level of SCHI3L1 was observed more in those with an increased than with a normal UCHI3L1 at enrollment (Additional file 1: Table S8). Additionally, we speculate that CHI3L1 binds to the megalin receptor for tubular reabsorption. This implies that NGAL and CHI3L1 can each indirectly affect the urinary concentration of the other, as they are then competitors [51].
Similar to NGAL, CHI3L1 is also stored in the secondary granules of circulating neutrophils [54–56]. This could implicate that in the urine of patients with a urinary tract infection (UTI), CHI3L1 is increased too [57]. Although data on UCHI3L1 in UTI patients are missing, proteome profiling of human neutrophils suggests that this issue is less relevant for UCHI3L1 [56], which agrees with the reported 12 pg NGAL and 0.16 pg CHI3L1 per leukocyte [57, 58].
Surprisingly, only in 2013 He et al. investigated the possibility that the CLP CHI3L1 mediates its biological effects through receptor binding, and identified interleukin-13 receptor α2 as the binding partner [59]. These biological effects include inhibition of apoptosis in renal epithelial cells [46, 59], and inhibition of pyroptosis and interleukin-1β production in macrophages [59, 60]. These innate immune cells play an important role in both kidney injury and repair [61].
Our study has important limitations. First, this is a single-center study conducted in surgical and medical ICUs. Although the baseline characteristics of patients, the observed outcomes, and the NGAL cutoff based on the Youden index suggest that the patients included are representative of ICUs in developed Western countries, these data remain to be confirmed in other centers and in different types of ICU. Second, only a limited number of patients reached the primary endpoint, which can be partly explained by selection bias, i.e., not asking (legally authorized representatives of) the most critically ill patients for consent. Yet, this is a typical and hence, rather unavoidable feature of prospective studies like this [21]. The restricted period for observation of AKI stage ≥2 certainly contributes to the low event rate as well. Therefore, we included all 21 patients (12 %) who developed AKISCr/UO stage ≥2 within 7 days after enrollment in the mixed model analysis. Third, following the KDIGO guidelines [13], reference SCr was defined as the lowest SCr value within the last 3 mo prior to enrollment. This method is prone to bias, as blood draws for SCr measurement tend to be performed more often when patients are in hospital or sick, thereby not reflecting true baseline kidney function. Fourth, we did not measure urinary [TIMP-2]•[IGFBP7], a two-biomarker panel found to be superior to UNGAL [21, 23, 24], because it was not available at the start of our study.
Conclusions
In summary, we demonstrated that UCHI3L1 measured in critically ill patients admitted to an ICU, predicted the occurrence of AKI stage ≥2 within a 12-h or 24-h observation period. The results of this pilot study need confirmation in different settings and in larger patient cohorts.
Key messages
The urinary proteome contains very relevant information: following an acute renal attack, CHI3L1 will appear in urine, indicating damage to the kidneys.
In this pilot cohort of critically ill patients admitted to an ICU, the UCHI3L1 response predicted development of AKI stage ≥2 within a 12-h or 24-h period.
The higher the concentration of UCHI3L1, the greater the severity of AKI.
Acknowledgements
This work was supported by the Research Foundation-Flanders (FWO, pre-doctoral grant to J. De Loor and postdoctoral grant to E. Hoste) and the Industrial Research Fund from Ghent University (IOF, advanced project ref. F2012/IOF-Advanced/001 with promoters E. Meyer and E. Hoste). We are grateful to L. De Crop, C. Clauwaert, S. Bracke, and D. Vermeiren, study coordinators of the Ghent University Hospital Division of Intensive Care, for their excellent work including screening of patients, collection, processing and freezing of samples, and completing the individual clinical research files. Likewise, we are grateful to all staff members of the Surgical and Medical Divisions of Intensive Care for asking eligible patients or their legally authorized representatives for consent for this study. We want to thank Prof. Dr. J. Delanghe for giving us the opportunity to measure UNGAL concentrations on an automated clinical platform in his laboratory and K. Van Nuffel for his dedicated help with the determination of UCHI3L1 concentrations by ELISA. This translational research was facilitated by Prof. Dr. S. Bekaert, coordinator of Bimetra-Clinical Research Center Ghent. Patent application was facilitated by Dr. P. De Vos and Dr. P. Jacobs of the IP and Licensing Technology Transfer Office of Ghent University Tech Transfer. An abstract reporting the main results of this study was published in Intensive Care Medicine Experimental 2015, 3(Suppl 1):A840 (doi:10.1186/2197-425X-3-S1-A840).
Abbreviations
- AKI
acute kidney injury
- AKISCr
AKI that was diagnosed and classified by the Kidney Disease | Improving Global Outcomes serum creatinine criteria
- AKISCr/UO
AKI that was diagnosed and classified by the Kidney Disease | Improving Global Outcomes serum creatinine or urine output criteria
- AUC-ROC
area under the receiver-operating characteristics curve
- CHI3L1
chitinase 3-like protein 1
- CHI3L3
chitinase 3-like protein 3
- CHIA
acidic mammalian chitinase
- CI
confidence interval
- CKD
chronic kidney disease
- CLP
chitinase-like protein
- d1
day of enrollment
- ELISA
enzyme-linked immunosorbent assay
- GFR
glomerular filtration rate
- h
hour
- I/R
ischemia/reperfusion
- ICU
intensive care unit
- IGFBP7
insulin-like growth factor-binding protein 7
- KDIGO
Kidney Disease | Improving Global Outcomes
- mo
month
- NGAL
neutrophil gelatinase-associated lipocalin
- RRT
renal replacement therapy
- SCHI3L1
serum chitinase 3-like protein 1
- SCr
serum creatinine
- STROBE
strengthening the reporting of observational studies in epidemiology
- TIMP-2
tissue inhibitor of metalloproteinases 2
- UCHI3L1
urinary chitinase 3-like protein 1
- UCr
urinary creatinine
- UNGAL
urinary neutrophil gelatinase-associated lipocalin
- UO
urine output
- UTI
urinary tract infection
Additional files
Supplemental data. This file provides all details on the study methods (Supplemental Text S1 and Tables S3A-F) and on additional analyses not included in the manuscript (Supplemental Text S2, Tables S4A-I and Figure Legends S1-S4). It also contains the Supplemental Tables S1, S2, S5-S8, to which we refer in the manuscript. (PDF 628 kb)
Area under the receiver-operating characteristics curve (AUC-ROC) with 95 % confidence interval (CI) of urinary chitinase 3-like protein 1 (UCHI3L1) (a) and urinary neutrophil gelatinase-associated lipocalin (UNGAL) (b) at enrollment for predicting acute kidney injury (AKI) stage ≥2 based on the Kidney Disease | Improving Global Outcomes (KDIGO) serum creatinine (SCr) or urine output (UO) criteria (AKI SCr/UO) within 12 h in different subgroups of patients. (TIF 434 kb)
Area under the receiver-operating characteristics curve (AUC-ROC) with 95 % confidence interval (CI) of urinary chitinase 3-like protein 1 (UCHI3L1) (a) and urinary neutrophil gelatinase-associated lipocalin (UNGAL) (b) at enrollment for predicting acute kidney injury (AKI) stage ≥2 based on the Kidney Disease | Improving Global Outcomes (KDIGO) serum creatinine (SCr) criteria (AKI SCr) within 24 h in different subgroups of patients. (TIF 436 kb)
Distribution of urinary chitinase 3-like protein 1 (UCHI3L1) (a) and urinary neutrophil gelatinase-associated lipocalin (UNGAL) (b) at enrollment in the eight selected subgroups of patients who did not develop acute kidney injury (AKI) based on the Kidney Disease | Improving Global Outcomes serum creatinine (SCr) or urine output (UO) criteria (No AKI SCr/UO) within 7 days after enrollment, compared to the distribution in all patients with no AKISCr/UO within 12 h after enrollment, and in all those maximally reaching AKISCr/UO stages 1, 2, or 3 within 12 h after enrollment. (TIF 715 kb)
Distribution of urinary chitinase 3-like protein 1 (UCHI3L1) (a) and urinary neutrophil gelatinase-associated lipocalin (UNGAL) (b) at enrollment in the eight selected subgroups of patients who did not develop acute kidney injury (AKI) based on the Kidney Disease | Improving Global Outcomes serum creatinine (SCr) criteria (No AKI SCr) within 7 days after enrollment, compared to the distribution in all patients with no AKISCr within 24 h after enrollment, and in all those maximally reaching AKISCr stages 1, 2, or 3 within 24 h after enrollment. (TIF 716 kb)
Footnotes
Eric AJ Hoste and Evelyne Meyer act as equivalent co-senior authors.
Competing interests
A patent application was filed on 4 April 2011 by Ghent University with E. Meyer and B. Maddens as inventors. The international patent application has been published as WO2012/136548. E. Hoste received a speaker’s fee from Astute Medical. For the remaining authors no competing interests were declared.
Authors’ contributions
Design and conduct of the study: EH designed the study in conjunction with EM, JDL and LN. EH was the Principal Investigator. Data collection: EH, JD and the other staff members of the Surgical and Medical Divisions of Intensive Care enrolled subjects. JDL and KD performed the laboratory analyses and analytically interpreted the results in conjunction with EM. EH and JDL clinically interpreted the data. Management: clinical data were managed by the study coordinators of the Ghent University Hospital Division of Intensive Care, under supervision of EH. Statistical analysis: JDL and EH performed the statistical analysis for the study. Interpretation of the data: all authors reviewed the data and participated in discussions related to interpretation. Preparation, review or approval of the manuscript: JDL wrote the paper. All authors reviewed and edited the paper and have seen and approved the final draft.
Contributor Information
Jorien De Loor, Email: Jorien.DeLoor@UGent.be.
Johan Decruyenaere, Email: Johan.Decruyenaere@UGent.be.
Kristel Demeyere, Email: Kristel.Demeyere@UGent.be.
Lieve Nuytinck, Email: Lieve.Nuytinck@UGent.be.
Eric AJ Hoste, Email: Eric.Hoste@UGent.be.
Evelyne Meyer, Email: Evelyne.Meyer@UGent.be.
References
- 1.Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care. 2006;10:R73. doi: 10.1186/cc4915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ostermann M, Chang RWS. Acute kidney injury in the intensive care unit according to RIFLE. Crit Care Med. 2007;35:1837–43. doi: 10.1097/01.CCM.0000277041.13090.0A. [DOI] [PubMed] [Google Scholar]
- 3.Bagshaw SM, George C, Bellomo R, Committe ADM. A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients. Nephrol Dial Transplant. 2008;23:1569–74. doi: 10.1093/ndt/gfn009. [DOI] [PubMed] [Google Scholar]
- 4.Hoste EA, Schurgers M. Epidemiology of acute kidney injury: how big is the problem? Crit Care Med. 2008;36:S146–51. doi: 10.1097/CCM.0b013e318168c590. [DOI] [PubMed] [Google Scholar]
- 5.Thakar CV, Christianson A, Freyberg R, Almenoff P, Render ML. Incidence and outcomes of acute kidney injury in intensive care units: A Veterans Administration study. Crit Care Med. 2009;37:2552–8. doi: 10.1097/CCM.0b013e3181a5906f. [DOI] [PubMed] [Google Scholar]
- 6.Mandelbaum T, Scott DJ, Lee J, Mark RG, Malhotra A, Waikar SS, et al. Outcome of critically ill patients with acute kidney injury using the Acute Kidney Injury Network criteria. Crit Care Med. 2011;39:2659–64. doi: 10.1097/CCM.0b013e3182281f1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nisula S, Kaukonen KM, Vaara ST, Korhonen AM, Poukkanen M, Karlsson S, et al. Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study. Intensive Care Med. 2013;39:420–8. doi: 10.1007/s00134-012-2796-5. [DOI] [PubMed] [Google Scholar]
- 8.Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41:1411–23. doi: 10.1007/s00134-015-3934-7. [DOI] [PubMed] [Google Scholar]
- 9.Kellum JA, Sileanu FE, Murugan R, Lucko N, Shaw AD, Clermont G. Classifying AKI by urine output versus serum creatinine level. J Am Soc Nephrol. 2015;26:2231–8. doi: 10.1681/ASN.2014070724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bagshaw SM, George C, Dinu I, Bellomo R. A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol Dial Transplant. 2008;23:1203–10. doi: 10.1093/ndt/gfm744. [DOI] [PubMed] [Google Scholar]
- 11.Chawla LS, Eggers PW, Star RA, Kimmel PL. Acute kidney injury and chronic kidney disease as interconnected syndromes. N Engl J Med. 2014;371:58–66. doi: 10.1056/NEJMra1214243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vanholder R, Davenport A, Hannedouche T, Kooman J, Kribben A, Lameire N, et al. Reimbursement of dialysis: a comparison of seven countries. J Am Soc Nephrol. 2012;23:1291–8. doi: 10.1681/ASN.2011111094. [DOI] [PubMed] [Google Scholar]
- 13.Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138.
- 14.Gomez H, Ince C, De Backer D, Pickkers P, Payen D, Hotchkiss J, et al. A unified theory of sepsis-induced acute kidney injury: inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaptation to injury. Shock. 2014;41:3–11. doi: 10.1097/SHK.0000000000000052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellomo R, Kellum JA, Ronco C. Acute kidney injury. Lancet. 2012;380:756–66. doi: 10.1016/S0140-6736(11)61454-2. [DOI] [PubMed] [Google Scholar]
- 16.De Loor J, Gevaert K, Hoste E, Meyer E. How has urinary proteomics contributed to the discovery of early biomarkers of acute kidney injury? Expert Rev Proteomics. 2014;11:415–24. doi: 10.1586/14789450.2014.932252. [DOI] [PubMed] [Google Scholar]
- 17.Murray PT, Mehta RL, Shaw A, Ronco C, Endre Z, Kellum JA, et al. Potential use of biomarkers in acute kidney injury: report and summary of recommendations from the 10th Acute Dialysis Quality Initiative consensus conference. Kidney Int. 2014;85:513–21. doi: 10.1038/ki.2013.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365:1231–8. doi: 10.1016/S0140-6736(05)74811-X. [DOI] [PubMed] [Google Scholar]
- 19.Martensson J, Bell M, Oldner A, Xu SY, Venge P, Martling CR. Neutrophil gelatinase-associated lipocalin in adult septic patients with and without acute kidney injury. Intensive Care Med. 2010;36:1333–40. doi: 10.1007/s00134-010-1887-4. [DOI] [PubMed] [Google Scholar]
- 20.de Geus HRH, Bakker J, Lesaffre EMEH, le Noble JLML. Neutrophil gelatinase-associated lipocalin at ICU admission predicts for acute kidney injury in adult patients. Am J Respir Crit Care Med. 2011;183:907–14. doi: 10.1164/rccm.200908-1214OC. [DOI] [PubMed] [Google Scholar]
- 21.Kashani K, Al-Khafaji A, Ardiles T, Artigas A, Bagshaw SM, Bell M, et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care. 2013;17:R25. doi: 10.1186/cc12503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haase-Fielitz A, Haase M, Devarajan P. Neutrophil gelatinase-associated lipocalin as a biomarker of acute kidney injury: a critical evaluation of current status. Ann Clin Biochem. 2014;51:335–51. doi: 10.1177/0004563214521795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bihorac A, Chawla LS, Shaw AD, Al-Khafaji A, Davison DL, DeMuth GE, et al. Validation of cell-cycle arrest biomarkers for acute kidney injury using clinical adjudication. Am J Respir Crit Care Med. 2014;189:932–9. doi: 10.1164/rccm.201401-0077OC. [DOI] [PubMed] [Google Scholar]
- 24.Hoste EAJ, McCullough PA, Kashani K, Chawla LS, Joannidis M, Shaw AD, et al. Derivation and validation of cutoffs for clinical use of cell cycle arrest biomarkers. Nephrol Dial Transplant. 2014;29:2054–61. doi: 10.1093/ndt/gfu292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koyner JL, Garg AX, Coca SG, Sint K, Thiessen-Philbrook H, Patel UD, et al. Biomarkers predict progression of acute kidney injury after cardiac surgery. J Am Soc Nephrol. 2012;23:905–14. doi: 10.1681/ASN.2011090907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koyner JL, Shaw AD, Chawla LS, Hoste EA, Bihorac A, Kashani K, et al. Tissue inhibitor metalloproteinase-2 (TIMP-2)IGF-binding protein-7 (IGFBP7) levels are associated with adverse long-term outcomes in patients with AKI. J Am Soc Nephrol. 2015;26:1747–54. doi: 10.1681/ASN.2014060556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doi K. How to replicate the complexity of human sepsis: development of a new animal model of sepsis. Crit Care Med. 2012;40:2722–3. doi: 10.1097/CCM.0b013e31825bc83f. [DOI] [PubMed] [Google Scholar]
- 28.Maddens B, Ghesquiere B, Vanholder R, Demon D, Vanmassenhove J, Gevaert K, et al. Chitinase-like proteins are candidate biomarkers for sepsis-induced acute kidney injury. Mol Cell Proteomics. 2012;11:M111 013094. [DOI] [PMC free article] [PubMed]
- 29.Maddens B, Vandendriessche B, Demon D, Vanholder R, Chiers K, Cauwels A, et al. Severity of sepsis-induced acute kidney injury in a novel mouse model is age dependent. Crit Care Med. 2012;40:2638–46. doi: 10.1097/CCM.0b013e3182591ebe. [DOI] [PubMed] [Google Scholar]
- 30.Lee CG, Da Silva CA, Dela Cruz CS, Ahangari F, Ma B, Kang MJ, et al. Role of chitin and chitinase/chitinase-like proteins in inflammation, tissue remodeling, and injury. Annu Rev Physiol. 2011;73:479–501. doi: 10.1146/annurev-physiol-012110-142250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lombard V, Golaconda Ramulu H, Drula E, Coutinho PM, Henrissat B. The carbohydrate-active enzymes database (CAZy) in 2013. Nucleic Acids Res. 2014;42:D490–5. doi: 10.1093/nar/gkt1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bussink AP, Speijer D, Aerts JM, Boot RG. Evolution of mammalian chitinase(−like) members of family 18 glycosyl hydrolases. Genetics. 2007;177:959–70. doi: 10.1534/genetics.107.075846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huang QS, Xie XL, Liang G, Gong F, Wang Y, Wei XQ, et al. The GH18 family of chitinases: their domain architectures, functions and evolutions. Glycobiology. 2012;22:23–34. doi: 10.1093/glycob/cwr092. [DOI] [PubMed] [Google Scholar]
- 34.Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4:1628–54. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc. 1927;22:209–12. doi: 10.1080/01621459.1927.10502953. [DOI] [Google Scholar]
- 36.Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17:857–72. doi: 10.1002/(SICI)1097-0258(19980430)17:8<857::AID-SIM777>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 37.Chertow GM, Lee J, Kuperman GJ, Burdick E, Horsky J, Seger DL, et al. Guided medication dosing for inpatients with renal insufficiency. JAMA. 2001;286:2839–44. doi: 10.1001/jama.286.22.2839. [DOI] [PubMed] [Google Scholar]
- 38.Balasubramanian G, Al-Aly Z, Moiz A, Rauchman M, Zhang ZW, Gopalakrishnan R, et al. Early nephrologist involvement in hospital-acquired acute kidney injury: a pilot study. Am J Kidney Dis. 2011;57:228–34. doi: 10.1053/j.ajkd.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 39.Ponce D, Zorzenon CDF, dos Santos NY, Balbi AL. Early nephrology consultation can have an impact on outcome of acute kidney injury patients. Nephrol Dial Transplant. 2011;26:3202–6. doi: 10.1093/ndt/gfr359. [DOI] [PubMed] [Google Scholar]
- 40.Cho A, Lee JE, Yoon JY, Jang HR, Huh W, Kim YG, et al. Effect of an electronic alert on risk of contrast-induced acute kidney injury in hospitalized patients undergoing computed tomography. Am J Kidney Dis. 2012;60:74–81. doi: 10.1053/j.ajkd.2012.02.331. [DOI] [PubMed] [Google Scholar]
- 41.Colpaert K, Hoste EA, Steurbaut K, Benoit D, Van Hoecke S, De Turck F, et al. Impact of real-time electronic alerting of acute kidney injury on therapeutic intervention and progression of RIFLE class. Crit Care Med. 2012;40:1164–70. doi: 10.1097/CCM.0b013e3182387a6b. [DOI] [PubMed] [Google Scholar]
- 42.Costa e Silva VT, Liaño F, Muriel A, Díez R, de Castro I, Yu L. Nephrology referral and outcomes in critically ill acute kidney injury patients. PLoS One. 2013;8:e70482. doi: 10.1371/journal.pone.0070482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goldstein SL, Kirkendall E, Nguyen H, Schaffzin JK, Bucuvalas J, Bracke T, et al. Electronic health record identification of nephrotoxin exposure and associated acute kidney injury. Pediatrics. 2013;132:E756–67. doi: 10.1542/peds.2013-0794. [DOI] [PubMed] [Google Scholar]
- 44.Kolhe NV, Staples D, Reilly T, Merrison D, McIntyre CW, Fluck RJ, et al. Impact of compliance with a care bundle on acute kidney injury outcomes: a prospective observational study. PLoS One. 2015;10:e0132279. doi: 10.1371/journal.pone.0132279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paragas N, Qiu A, Zhang Q, Samstein B, Deng SX, Schmidt-Ott KM, et al. The Ngal reporter mouse detects the response of the kidney to injury in real time. Nat Med. 2011;17:216–22. doi: 10.1038/nm.2290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schmidt IM, Hall IE, Kale S, Lee S, He CH, Lee Y, et al. Chitinase-like protein Brp-39/YKL-40 modulates the renal response to ischemic injury and predicts delayed allograft function. J Am Soc Nephrol. 2013;24:309–19. doi: 10.1681/ASN.2012060579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cruz DN, Bolgan I, Perazella MA, Bonello M, de Cal M, Corradi V, et al. North East Italian Prospective Hospital Renal Outcome Survey on Acute Kidney Injury (NEiPHROS-AKI): targeting the problem with the RIFLE criteria. Clin J Am Soc Nephrol. 2007;2:418–25. doi: 10.2215/CJN.03361006. [DOI] [PubMed] [Google Scholar]
- 48.Haase M, Bellomo R, Matalanis G, Calzavacca P, Dragun D, Haase-Fielitz A. A comparison of the RIFLE and Acute Kidney Injury Network classifications for cardiac surgery-associated acute kidney injury: A prospective cohort study. J Thorac Cardiovasc Surg. 2009;138:1370–6. doi: 10.1016/j.jtcvs.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 49.Macedo E, Malhotra R, Bouchard J, Wynn SK, Mehta RL. Oliguria is an early predictor of higher mortality in critically ill patients. Kidney Int. 2011;80:760–7. doi: 10.1038/ki.2011.150. [DOI] [PubMed] [Google Scholar]
- 50.Hall IE, Stern EP, Cantley LG, Elias JA, Parikh CR. Urine YKL-40 is associated with progressive acute kidney injury or death in hospitalized patients. BMC Nephrol. 2014;15:133. doi: 10.1186/1471-2369-15-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hvidberg V, Jacobsen C, Strong RK, Cowland JB, Moestrup SK, Borregaard N. The endocytic receptor megalin binds the iron transporting neutrophil-gelatinase-associated lipocalin with high affinity and mediates its cellular uptake. FEBS Lett. 2005;579:773–7. doi: 10.1016/j.febslet.2004.12.031. [DOI] [PubMed] [Google Scholar]
- 52.Nyirkos P, Golds EE. Human synovial-cells secrete a 39-kDa protein similar to a bovine mammary protein expressed during the nonlactating period. Biochem J. 1990;269:265–8. doi: 10.1042/bj2690265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johansen JS, Williamson MK, Rice JS, Price PA. Identification of proteins secreted by human osteoblastic cells in culture. J Bone Miner Res. 1992;7:501–12. doi: 10.1002/jbmr.5650070506. [DOI] [PubMed] [Google Scholar]
- 54.Kjeldsen L, Bainton DF, Sengelov H, Borregaard N. Identification of neutrophil gelatinase-associated lipocalin as a novel matrix protein of specific granules in human neutrophils. Blood. 1994;83:799–807. [PubMed] [Google Scholar]
- 55.Volck B, Price PA, Johansen JS, Sorensen O, Benfield TL, Nielsen HJ, et al. YKL-40, a mammalian member of the chitinase family, is a matrix protein of specific granules in human neutrophils. Proc Assoc Am Physicians. 1998;110:351–60. [PubMed] [Google Scholar]
- 56.Rorvig S, Ostergaard O, Heegaard NHH, Borregaard N. Proteome profiling of human neutrophil granule subsets, secretory vesicles, and cell membrane: correlation with transcriptome profiling of neutrophil precursors. J Leukoc Biol. 2013;94:711–21. doi: 10.1189/jlb.1212619. [DOI] [PubMed] [Google Scholar]
- 57.Decavele ASC, Dhondt L, De Buyzere ML, Delanghe JR. Increased urinary neutrophil gelatinase associated lipocalin in urinary tract infections and leukocyturia. Clin Chem Lab Med. 2011;49:999–1003. doi: 10.1515/CCLM.2011.156. [DOI] [PubMed] [Google Scholar]
- 58.Nordenbaek C, Johansen JS, Junker P, Borregaard N, Sorensen O, Price PA. YKL-40, a matrix protein of specific granules in neutrophils, is elevated in serum of patients with community-acquired pneumonia requiring hospitalization. J Infect Dis. 1999;180:1722–6. doi: 10.1086/315050. [DOI] [PubMed] [Google Scholar]
- 59.He CH, Lee CG, Dela Cruz CS, Lee CM, Zhou Y, Ahangari F, et al. Chitinase 3-like 1 regulates cellular and tissue responses via IL-13 receptor alpha 2. Cell Rep. 2013;4:830–41. doi: 10.1016/j.celrep.2013.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dela Cruz CS, Liu W, He CH, Jacoby A, Gornitzky A, Ma B, et al. Chitinase 3-like-1 promotes Streptococcus pneumoniae killing and augments host tolerance to lung antibacterial responses. Cell Host Microbe. 2012;12:34–46. doi: 10.1016/j.chom.2012.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee S, Huen S, Nishio H, Nishio S, Lee HK, Choi BS, et al. Distinct macrophage phenotypes contribute to kidney injury and repair. J Am Soc Nephrol. 2011;22:317–26. doi: 10.1681/ASN.2009060615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Eknoyan G, Levin NW. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification - foreword. Am J Kidney Dis. 2002;39:S14–266. doi: 10.1053/ajkd.2002.32720. [DOI] [PubMed] [Google Scholar]


