Abstract
Hepatitis C virus (HCV) infection affects ≥ 180 million individuals worldwide especially those living in developing countries. Recent advances in direct-acting therapeutics promise effective treatments for chronic HCV carriers, but only if the affected individuals are identified. Good treatment coverage therefore requires accurate epidemiological data on HCV infection. In 2014, we determined the current prevalence of HCV in Thailand to assess whether over the past decade the significant number of chronic carriers had changed. In total, 5964 serum samples from Thai residents between 6 months and 71 years of age were obtained from 7 provinces representing all 4 geographical regions of Thailand and screened for the anti-HCV antibody. Positive samples were further analyzed using RT-PCR, sequencing, and phylogenetic analysis to identify the prevailing HCV genotypes. We found that 56 (0.94%) samples tested positive for anti-HCV antibody (mean age = 36.6±17.6 years), while HCV RNA of the core and NS5B subgenomic regions was detected in 23 (41%) and 19 (34%) of the samples, respectively. The seropositive rates appeared to increase with age and peaked in individuals 41–50 years old. These results suggested that approximately 759,000 individuals are currently anti-HCV-positive and that 357,000 individuals have viremic HCV infection. These numbers represent a significant decline in the prevalence of HCV infection. Interestingly, the frequency of genotype 6 variants increased from 8.9% to 34.8%, while the prevalence of genotype 1b declined from 27% to 13%. These most recent comprehensive estimates of HCV burden in Thailand are valuable towards evidence-based treatment coverage for specific population groups, appropriate allocation of resources, and improvement in the national public health policy.
Introduction
Hepatitis C virus (HCV) infection represents a major public health problem in many countries. Approximately 185 million people are chronically infected and 500,000 people die from HCV-related liver diseases annually [1–2]. As many as 75% of acute infection leads to chronic infection in some individuals, who are often unaware of their HCV status until the appearance of clinical symptoms years later. HCV infection results in liver fibrosis, cirrhosis, and hepatocellular carcinoma, which subsequently requires liver transplantation. Moreover, HCV carriers may unknowingly infect others via blood transfusion and from iatrogenic procedures or intravenous drug use [3].
The standard of care for chronic HCV has been pegylated interferon-alpha administered in combination with ribavirin (PEG-IFN plus ribavirin). However, the treatment does not lead to sustained virologic response (SVR) in all patients due to several factors including the viral genotype, patient age and genetic background, or poor adherence to therapy resulting from adverse events [4–6]. Fortunately, novel and effective direct-acting antivirals (DAA) available in several combination regimens have resulted in > 90% SVR rate in patients with HCV genotype 1, which is typically refractory to standard treatments [7]. Patients with HCV genotypes 2 and 3 who received sofosbuvir plus oral ribavirin treatment can also expect to achieve > 93–95% SVR. Although sofosbuvir treatment is considered cost-effective in developed countries, its use remains cost-prohibitive in developing countries [8–10].
In Thailand, the estimates of HCV prevalence differ considerably depending on the population size, target group, and period of study. The National Blood Center (NBC) has reported that the prevalence of new anti-HCV-positive blood donors declined from 1.6% to 0.5% between 1991 and 2009 [11]. Even though the frequency of HCV among blood donors appears relatively low, it may not reflect the true prevalence in the general population because preliminary screening of blood donors would exclude high-risk individuals such as sex workers, prisoners, intravenous drug users (IVDUs), and blood transfusion recipients [11]. Studies on the general population had reported a decrease in HCV infection from 1.95% in 1994 to 0.86% in 2002 [12–13], but a national survey suggested a higher prevalence of 2.15% in 2004 [14]. Since then, no new data regarding HCV infection in large population-based cohorts are available to indicate more recent national prevalence in the numbers of active and past HCV infection in Thailand. Therefore, the aims of this study are to evaluate the national population-based prevalence of HCV infection and HCV genotype distribution in 2014, and to compare these data to the previous national serosurvey performed in 2004 [14]. These results were then used to estimate the number of viremic carriers and past infection in different age groups.
Material and Methods
As part of the overall research consortium to assess the status of viral hepatitis in the country (“The impact of hepatitis B vaccine immunization program as part of EPI after 20 years implementation and seroprevalence of hepatitis A, B and C in Thailand”), we determined the prevalence of HCV in the Thai population between January and December 2014. This study was approved by the institutional review board (IRB 419/56) of the Faculty of Medicine, Chulalongkorn University, and in compliance with the principles of the Declaration of Helsinki. Written informed consents were obtained from all participants or their parents (if they were minors).
Sample collection
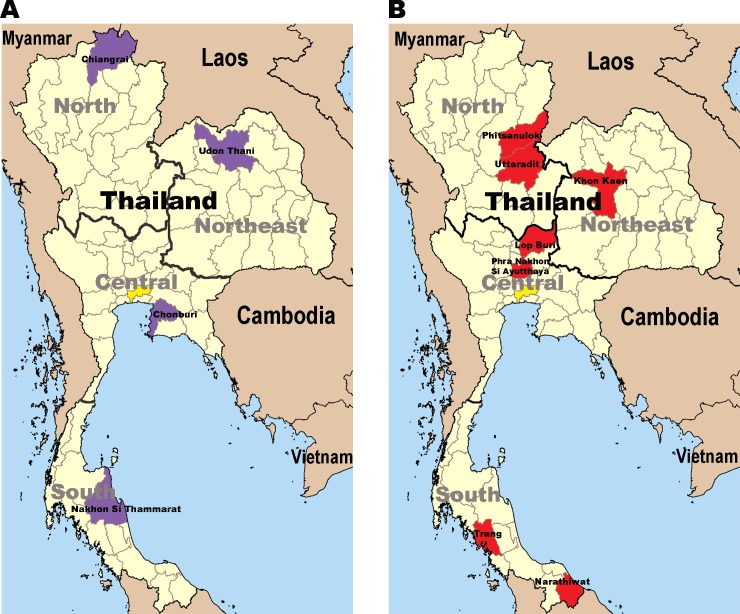
A total of 5964 serum samples were collected in 7 provinces (Pha Nakhon Si Ayutthaya, n = 757; Lop Buri, n = 778, Uttaradit, n = 903; Phitsanulok, n = 518; Khon Kaen, n = 1633; Trang, n = 730; and Narathiwat, n = 645) located in 4 different geographical regions of Thailand (north, northeast, central, and south) (Fig 1 and S1 Table). Blood samples were collected from individuals during scheduled pediatric health check-up or outpatient clinic at the hospital. The inclusion criteria were: age between 6 months and 71 years, no history of chronic diseases, no clinical signs or symptoms associated with either an immunodeficiency disorder or HIV infection, and no history of immunosuppressive therapy. The sera from clotted blood samples were collected within 24 hours and kept at -70°C until testing.
Fig 1. Provinces in Thailand for which HCV seroprevalence was determined.
(A) The provinces sampled in 2004 [14] (purple) and (B) in this study (red). The capital city Bangkok is shown in yellow.
Serological testing
All sera were tested for the HCV antibody using an automated chemiluminescent microparticle immunoassay with recombinant proteins HCr43 (core and NS3) and c100-3 (NS4a and NS4b) (ARCHITECT anti-HCV assay, Abbott Diagnostics, Wiesbaden, Germany) according to the manufacturer’s instructions. Samples identified as HCV antibody-positive by the automated assay were evaluated for their signal-to-cut-off (S/CO) ratio. True HCV antibody-positive result was defined by a high S/CO ratio ≥ 5.0 (Abbott, Architech anti-HCV), while sample with an S/CO ratio < 5.0 was further evaluated according to the U.S. Centers for Disease Control and Prevention (CDC) (http://www.cdc.gov/hepatitis/hcv/labtesting.htm). All HCV antibody-positive samples were subjected to further laboratory testing.
RT-PCR amplification and phylogenetic analysis
Viral RNA was extracted manually from HCV antibody-positive serum using the guanidinium thiocyanate extraction method. Reverse transcription was performed using random hexamers and ImProm-II Reverse Transcriptase (Promega, Madison, WI, USA). The HCV core and NS5B partial sequences were amplified by polymerase chain reaction (PCR) with the 2X Perfect Tag Plus Master Mix (5 PRIME, Gaithersburg, MD, USA) as previously described [15]. PCR amplicons were sequenced (First BASE Laboratories, Selangor, Malaysia) and analyzed using Chromas LITE (v2.01), BioEdit (v.5.0.9; Ibis Therapeutics, Carlsbad, CA, USA), SeqManPro (DNASTAR, Madison, WI, USA), and BLASTN search (http://www.ncbi.nlm.nih.gov).
The core and NS5B sequence alignments were done using ClustalX v.2.1. After trimming, the alignments (299 nucleotides for the core and 300 nucleotides for NS5B) were subjected to phylogenetic reconstruction using neighbor-joining method and Kimura’s two parameters model implemented in MEGA 6.0 [16]. Bootstrap testing relied on 1,000 replicates. The genotype of each sample was assigned according to where it clustered with the reference strain. The reference subtype sequences used in this study (and accession numbers) were: 1a (M62321, M67463), 1b (D90208, M58335), 1c (D14853), 2a (AB047639, D00944), 2b (D10988, AB030907), 2c (D50409), 3a (D17763, D28917), 3b (D49374), 4a (Y11604), 5a (Y13184, AF064490), 6a (Y12083, AY859526), 6b (D84262), 6c (EF424629), 6d (D84263), 6e (DQ314805), 6f (DQ835760), 6g (D63822), 6h (D84265), 6i (DQ835770), 6j (DQ835769), 6 (D84264), 6l (EF424628), 6m (DQ835767), 6n (DQ278894, DQ835768), 6o (EF424627), 6p (EF424626), 6q (EF424625), 6r (EU408328), 6s (EU408329), 6t (EF632071, EU246939), 6u (EU246940), 6v (EU158186, EU798760), 6w (DQ278892, EU643834), 6xa (EU408330, EU408332), 6xb (JX183552, KJ567645), 6xc (KJ567650, KJ567649), 6xd (KM252791, KM252789) and 6xe (JX183557, KM252792). All nucleotide sequences generated were submitted to the GenBank database under accession numbers KT921354-KT921395.
Comparison with the previous national survey
Data from this study were compared to those reported by a previously published national survey conducted in 2004 [14]. That study included the demographic data of healthy individuals and those with acute illness (age range = 6 months–60 years) who resided in 4 provinces (Chiang Rai, Udon Thani, Nakhon Si Thammarat, and Chon Buri) representing each geographical region (Fig 1A). In the previous survey, the anti-HCV antibody screening also utilized an automated ELISA assay (AxSYM; Abbott Laboratory, North Chicago, IL, USA). Viral RNA was also isolated and amplified using similar protocols as this study.
The Thai population data in 2004 and 2014 were derived from the Official Statistics Registration Systems (http://stat.dopa.go.th/stat/statnew/upstat_age.php). From these data, estimates of the numbers of both the anti-HCV-positive individuals and viremic carriers were extrapolated to yield the HCV-seropositive and viremic rate in this and the previous study [14]. The number of HCV carriers was calculated according to the population of each age group (0–10, 11–20, 21–30, 31–40, 41–50, and > 50 years), which in total provided the number of carriers in Thailand. The number of anti-HCV-positive individuals, viremic carriers, and genotypic distribution were compared over this 10-year period.
Data analysis
The Chi-square and Mann-Whitney U test were used to compare the categorical and continuous variables, respectively. In this study, p < 0.05 was considered statistically significant. All statistical analyzes were performed using SPSS for Windows (version 11.5; SPSS, Chicago, IL, USA).
Results
HCV seroprevalence
The demographic data of all 5,964 individuals included in this study are shown in Table 1. The mean age was 24.55 ± 18.52 years and there were more females than males (male = 2,530 samples, female = 3,434 samples). A total of 56 samples tested positive for anti-HCV antibody (mean age = 36.46 ± 17.16 years). HCV seropositivity was higher in men than women and was highest in the northeastern region (20 positive samples, or 1.22%) and lowest in the southern region (8 positive samples, or 0.58%). There were no significant differences between genders and HCV antibody-positive status regionally (p = 0.340 and 0.081, respectively). However, there were statistically significant differences in the mean ages of seropositive individuals in these 4 regions (p = 0.044) because the participants in the northeastern region were the oldest (41.30 ± 11.67 years) and those in the southern region were the youngest (20.75 ± 17.17 years).
Table 1. Demographic data of individuals in this study.
| Region | Central | North | Northeast | South | Total | p |
|---|---|---|---|---|---|---|
| No. of samples | 1535 | 1421 | 1633 | 1375 | 5964 | NAa |
| Age (SD) | 24.12 18.45) | 25.14 (18.63) | 23.16 (18.13) | 26.08 (18.81) | 24.55 (18.52) | NAa |
| Sex (M/F) | 701/834 | 580/841 | 782/851 | 467/908 | 2530/3434 | NAa |
| Anti-HCV (%) | 15 (0.98) | 13 (0.91) | 20 (1.22) | 8 (0.58) | 56 (0.94) | 0.340 |
| Age (SD) | 40.20 (17.02) | 34.38 (19.97) | 41.30 (11.67) | 20.75 (17.17) | 36.46 (17.16) | 0.044 |
| Sex (M/F) | 7/8 | 8/5 | 15/5 | 5/3 | 35/21 | 0.081 |
| HCV RNA +ve(%) | 4 (26.67) | 3 (23.08) | 14 (70.00) | 2 (25.00) | 23 (41.07) | NAa |
| Genotype | NAa | |||||
| 1a | - | - | 1 | - | 1 (4.35) | |
| 1b | - | 2 | 1 | - | 3 (13.04) | |
| 3a | 1 | 1 | 6 | 2 | 10 (43.48) | |
| 3b | 1 | - | - | - | 1 (4.35) | |
| 6c | - | - | 1 | - | 1 (4.35) | |
| 6f | - | - | 3 | - | 3 (13.04) | |
| 6i | - | - | 2 | - | 2 (8.70) | |
| 6j | 1 | - | - | - | 1 (4.35) | |
| 6n | 1 | - | - | - | 1 (4.35) | |
aThis parameter was not analyzed.
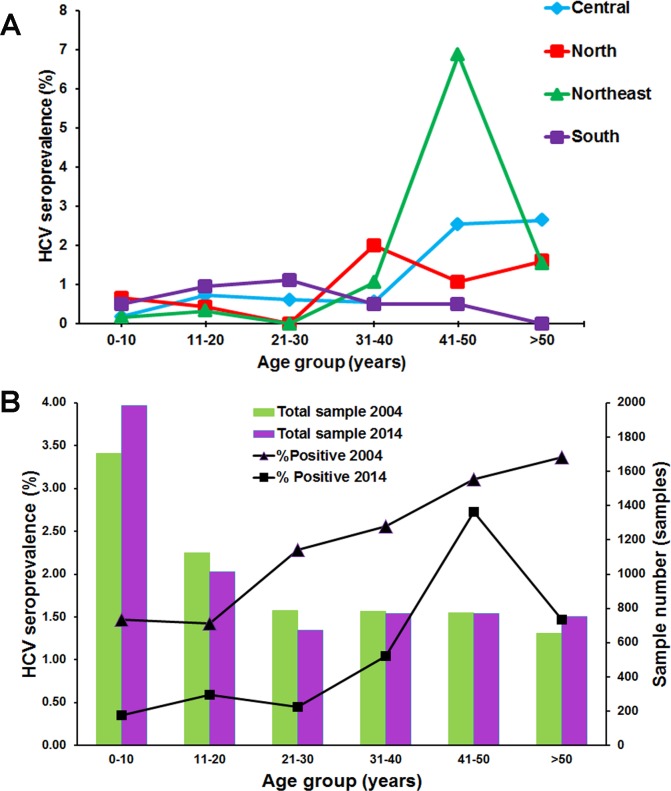
The anti-HCV prevalence was relatively low among individuals < 30 years of age regardless of the region in which they reside (Fig 2A, S1 Table). Regionally, the highest anti-HCV prevalence among individuals 31–40 years was in the north (2.00%), while among the age group 41–50 years was in the northeast (6.88%). Among individuals > 50 years of age, the highest prevalence was in the central region (2.65%). In the south, prevalence of anti-HCV antibody appeared to increase up to the age of 30, then declined among individuals > 30 years.
Fig 2. Distribution of HCV seropositive rates in 2014 compared to 2004.
(A) The prevalence of anti-HCV antibody was stratified by age group and geographical region. (B) The number of samples examined in 2004 (green) and 2014 (purple) for each age group. The seroprevalence in 2004 (triangle) [14] and 2014 (square) for each age group.
Given comparable number of samples surveyed in 2004 and 2014, it was noted that the overall seroprevalence in 2004 correlated with increasing age (Fig 2B). In 2014, however, the prevalence of anti-HCV antibody markedly decreased. The seroprevalence was highest among individuals 41–50 years of age (2.72%) and appeared to decline among those > 50 years of age (1.46%).
HCV viremia
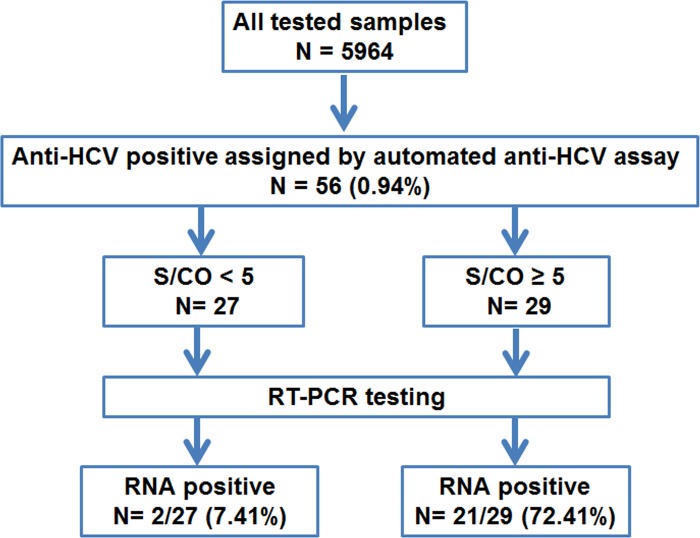
To determine the prevalence of viremia among the 56 seropositive samples, HCV RNA was assessed using RT-PCR analysis of the subgenomic core region. According to the U.S. CDC guidelines of (http://www.cdc.gov/hepatitis/hcv/labtesting.htm), the S/CO ratio for optical density (OD) predictive of the true HCV positivity in > 95% of samples is ≥ 5.0. Therefore, the 56 anti-HCV-positive samples were divided into the low and high S/CO-ratio groups (Fig 3 and S2 Table). For the low S/CO-ratio group (OD < 5), there were 27 samples with a mean OD of 2.34 ± 0.95. Only 2 samples tested positive for viral RNA, giving a viremic rate of 7.41%. Meanwhile, the high S/CO-ratio group (OD ≥ 5.0) comprised 29 samples with a mean OD of 12.39 ± 2.20. However, only 21 samples tested positive for viral RNA and thus yielded a viremic rate of 72.41%. In all, 23 out of 56 seropositive samples (41.07%) tested positive for the HCV core region. We also determined the HCV RNA of the NS5B region, but only 19 samples tested positive (S2 Table). Among the 4 NS5B-negative samples, 2 had low S/CO ratios and 2 others had high S/CO ratios.
Fig 3. Schematic diagram of the study protocol.
S/CO denotes the signal-to-cutoff ratio.
HCV genotypes in Thailand
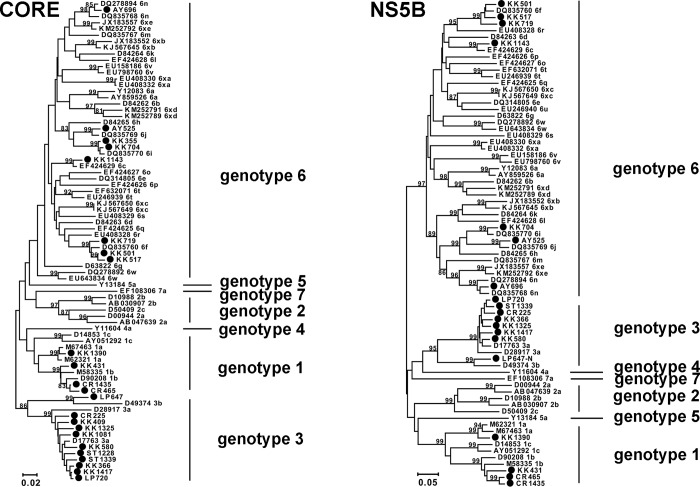
Phylogenetic analysis of the core and the NS5B regions were consistent in identifying HCV genotypes among the positive samples (Fig 4). The most common HCV belonged to genotype 3a (43.48%), followed by 1b (13.04%), 6f (13.04%), 6i (8.70%), 1a (4.35%), 3b (4.35%), 6c (4.35%), 6j (4.35%), and 6n (4.35%) (Table 1).
Fig 4. Phylogenetic tree based on the core (left) and NS5B (right) sequences of the HCV-positive samples.
The positive samples in this study are indicated (black circles). The accession numbers with the respective genotypes and > 80% bootstrap values are shown.
HCV prevalence over time
To assess the current trend in HCV infection, we calculated the approximate HCV seroprevalence and viremia in the general population based on the data from this and a previous study (Fig 2B and Table 2) [14]. Comparison of the HCV antibody-positive and RNA-positive rates between 2004 and 2014 showed that the HCV prevalence gradually declined in Thailand. In 2004, approximately 1.4 million people were HCV antibody-positive, and 715,930 people were presumed viremic with appreciable HCV RNA. In 2014, however, there were 758,940 HCV antibody-positive individuals, 356,670 of whom were viremic for HCV. Overall, both HCV seroprevalence and the viremic rate decreased from 2.15% to 0.94% and from 1% to 0.39%, respectively. This trend was in agreement with the seroprevalence screening donated blood screened by the Thailand National Blood Bank (Fig 5). Therefore, the estimated number of HCV carriers decreased by half from 715,930 people in 2004 to 356,670 people in 2014 (Table 2).
Table 2. Estimated HCV carriers in the Thai population.
| Year 2004 | Year 2014 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age range | Anti-HCV +ve rate | RNA +ve rate | Thai population | Anti-HCV carrier | HCV carrier | Anti-HCV +ve rate | RNA +ve rate | Thai Population | Anti-HCV carrier | HCV carrier |
| 0–10 | 1.47 | 0.41 | 9,553,008 | 140429 | 39,244 | 0.35 | 0.05 | 8,485,974 | 29701 | 4,273 |
| 11–20 | 1.42 | 0.53 | 9,419,566 | 133758 | 50,238 | 0.59 | 0.10 | 8,829,060 | 52091 | 8,699 |
| 21–30 | 2.28 | 1.02 | 10,570,790 | 241014 | 107,318 | 0.45 | 0.00 | 9,330,783 | 41989 | 0 |
| 31–40 | 2.56 | 1.92 | 10,972,787 | 280903 | 210,745 | 1.04 | 0.13 | 10,346,437 | 107603 | 13,472 |
| 41–50 | 3.10 | 1.55 | 8,859,873 | 274656 | 137,540 | 2.72 | 1.69 | 10,465,811 | 285061 | 176,466 |
| >50 | 3.36 | 1.53 | 11,173,300 | 375423 | 170,846 | 1.46 | 0.93 | 16,496,285 | 242495 | 153,760 |
| Total | 2.15 | 1.00 | 60,549,324 | 1,446,183 | 715,930 | 0.94 | 0.39 | 63,954,350 | 758,940 | 356,670 |
Fig 5. HCV seropositivity rate derived from blood screening by the National Blood Center (NBC) between 1995–2014.
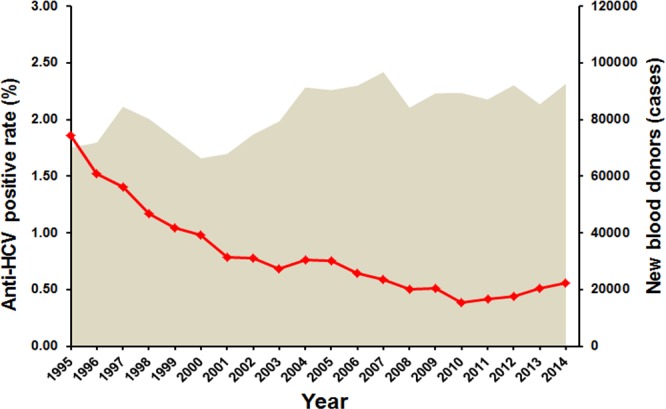
The shaded area represents the number of annual screenings of new blood donors performed by NBC. The seroprevalence trend is denoted by the line.
Discussion
HCV genotype 1a, 1b, 3a, 3b, and 6 variants were identified in this study, which suggested that genotypic distribution remained relatively unchanged over the past decade. HCV genotype 3a continued to be the most common genotype in Thailand (51.5% in the previous study vs 43.5% in the current study). Interestingly, genotype 6 variants significantly increased from 8.9% to 33.8% between 2004 and 2014, while genotype 1b declined by half (from 26.7% to 13.1%). An increase in the distribution of the genotype 6 variants was also observed in the blood donors in some regions of Thailand and IVDUs in China [17–18]. These changes may be associated with behaviors that are transmission route-specific as it has been suggested that the transmission patterns of genotype 1b and 6 were linked to blood transfusion and sharing of contaminated needles or IVDUs, respectively [18–20].
To exclude false-positive anti-HCV results and minimize the number of samples required for additional tests, we used the U.S. CDC guideline to classify HCV antibody-positive samples into 2 groups based on their OD values. As expected, the high S/CO-ratio group in this study demonstrated 72% HCV-RNA positivity upon confirmatory RT-PCR testing, which was in agreement with a previous study examining the anti-HCV-positive antibodies among blood donors (71%) [21]. The higher OD value from the S/CO ratio also correlated with the likelihood of an active HCV infection. In contrast, a lower S/CO ratio was predictive of HCV RNA negativity [22] as HCV RNA was only detected in 2 samples in the low S/CO-ratio group (7%). The latter may be due to several reasons including spontaneous clearance of previous HCV exposure, low viral load, or occult infection [23–24]. HCV viremic individuals with detectable viral RNA ideally would require long-term follow-up to confirm infection in this population. In addition, a more sensitive test may be needed to detect extremely low viral RNA load in some HCV viremic individuals.
Epidemiological trends of HCV infection in Thailand have been difficult to evaluate for several reasons. Sampling differed in locations and consequently showed different rates of infection. For example, a study by a northern regional blood center reported an HCV-positivity rate of 2.16–2.91%, while another blood center in the northeast reported a higher prevalence at 5.62% [25–27]. In addition, the time period of the study also led to different rates of HCV positivity. In 1994, a survey in Bangkok found an anti-HCV-positive incidence of 1.95% in the general population, which was consistent with the 1.86% positivity rate found in blood donors by the National Blood Center (NBC) in Bangkok the very same year [11–12]. However, the rate appeared to decrease to 0.86% according to a study conducted in 2000–2002, which surveyed only individuals residing in the central region of Thailand including Bangkok [13]. The selection of study cohort also influenced HCV prevalence. HCV infection tends to be more frequent among high-risk groups such as IVDUs, hemodialysis patients, and in populations residing in remote areas compared to the general population [28–29]. In particular, HCV is highly prevalent among drug injectors (up to 86%) compared to the general population (approximately 2%) [14,30–31].
Accurately derived HCV seropositive rate ideally requires data analysis with comparable parameters. A similar population-based survey in 2004 by our group suggested that HCV seroprevalence was approximately 2.15%. This was 3 times higher than the 0.76% positivity rate reported by NBC [11,14]. Therefore, this study attempted to include different geographical locations in order to represent the overall population and produce the current HCV rate. Using a comparative sample size, nearly 6,000 individuals were sampled and screened using similar methods as in 2004. Consequently, we found that the HCV prevalence (0.94%) decreased by half compared to a decade ago. The rate was low among younger Thais and slightly higher in older individuals. The increasing HCV prevalence with age in Thailand was also similarly observed in U.S. and Spain [32–33]. The relatively high HCV positive rate in the northeastern region (7.0% in individuals between 41–50 years of age) was concordant with a previous study conducted in 1995 on blood donors in the same region. At that time, a very high prevalence (6.5%) was found in individuals between 21–30 years of age [27]. It is unclear why HCV infection remained relatively unchanged in the northeast, therefore further studies are likely needed to identify HCV transmission and disease burden in this population.
The estimated 345,670 HCV carriers derived from this study was significantly lower than the previously estimated HCV viremic carriers in Thailand [34]. The decreasing prevalence of HCV over the past decade may have resulted from several factors. The discovery of HIV greatly increased the public health awareness of bloodborne pathogens. After the first case of HIV was reported in Thailand [35], there was a significant improvement in the healthcare system and clinical practice. Emphasis on sterilized medical equipment, use of disposable needles, increased screening of donated blood, and the practice of universal precautions all contributed to the reduction of bloodborne agents including HCV, which shares the similar routes of transmission as HIV. In addition, Thailand had placed increased emphasis on the safety of the blood supply since HCV was discovered in 1989. From 1991, mandated screening of donated blood included the use of molecular biology to detect viral nucleic acid beginning in 2006 [11,36–37]. As a result, the number of HCV antibody-positive blood donors had slowly declined from 2% in the early years of implementation to 0.5% in 2014 (Fig 5). Furthermore, declining HCV infection may be related to increased methamphetamine use as it has replaced intravenous heroin injection during the last 10 years. Finally, increased awareness through health education may have also contributed to the reductions in HCV infection in Thailand.
Information on HCV infection in other Southeast Asian countries is either limited or demonstrates varying prevalence rates [38–39]. Generally high HCV prevalence has been reported in Myanmar (11.6%) and Cambodia (5.8%) [40–41], although they are lower among Myanmarian (1.69%) and Cambodian (2.3%) migrants living in Thailand [42]. Intermediate levels of HCV infection have been reported in Vietnam (1.0–3.3%), Indonesia (2.1%), and the Philippines (2.2%) [38–39,43–44]. HCV prevalence among Laotian migrants living in Australia was approximately 3.2% [45]. The present Thailand HCV prevalence of 0.94% resembles that of more developed countries such as Singapore (0.37%) and Malaysia (0.14%) [46–47].
Effective HCV treatments have begun to reduce the overall incidence of HCV in carriers. Recent changes in the Thai healthcare policy have made universal HCV treatment available to all HCV patients, but access to treatment remains a challenge. In other developing countries, highly effective DAA therapy regimens are often not available due to financial barrier, and the cost-effectiveness of using these promising new drugs remains debatable [8,48].
Supporting Information
(DOCX)
The HCV genotype based on the core and NS5B sequences are indicated.
(DOCX)
(DOCX)
Acknowledgments
We would like to thank all the personnel and staff of the Center of Excellence in Clinical Virology, Faculty of Medicine, Chulalongkorn University, Uttaradit Hospital, Lablae Hospital, Naresuan University Hospital, Chumphae Hospital, Phra Nakhon Si Ayutthaya Hospital, King Narai Hospital, Narathiwat Ratchanakarin Hospital and Trang Hospital for their technical and administrative assistance, which made this study possible.
Data Availability
All sequence files are available from the GenBank database (accession numbers KT921354-KT921395).
Funding Statement
This work was supported by The National Research University Project, Office of Higher Education Commission (WCU-58-006-HR), The National Research Council of Thailand (NRCT), The Research Chair Grant from the National Science and Technology Development Agency, Chulalongkorn University Centenary Academic Development Project (CU56-HR01), Ratchadaphiseksomphot Endowment Fund of Chulalongkorn University (RES560530093), The Outstanding Professor of Thailand Research Fund (DPG5480002), and The Center of Excellence in Clinical Virology of Chulalongkorn University (GCE 58-014-30-004), King Chulalongkorn Memorial Hospital, and the Rachadapisek Sompote Fund of Chulalongkorn University for postdoctoral fellowship to Rujipat Wasitthankasem. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology 2013; 57: 1333–1342. 10.1002/hep.26141 [DOI] [PubMed] [Google Scholar]
- 2.WHO (2014) Hepatitis C. Available: http://www.who.int/mediacentre/factsheets/fs164/en/.
- 3.Hajarizadeh B, Grebely J, Dore GJ. Epidemiology and natural history of HCV infection. Nat Rev Gastroenterol Hepatol 2013; 10: 553–562. 10.1038/nrgastro.2013.107 [DOI] [PubMed] [Google Scholar]
- 4.Tanaka Y, Nishida N, Sugiyama M, Kurosaki M, Matsuura K, Sakamoto N, et al. Genome-wide association of IL28B with response to pegylated interferon-alpha and ribavirin therapy for chronic hepatitis C. Nat Genet 2009; 41: 1105–1109. 10.1038/ng.449 [DOI] [PubMed] [Google Scholar]
- 5.Suppiah V, Moldovan M, Ahlenstiel G, Berg T, Weltman M, Abate ML, et al. IL28B is associated with response to chronic hepatitis C interferon-alpha and ribavirin therapy. Nat Genet 2009; 41: 1100–1104. 10.1038/ng.447 [DOI] [PubMed] [Google Scholar]
- 6.Fellay J, Thompson AJ, Ge D, Gumbs CE, Urban TJ, Shianna KV, et al. ITPA gene variants protect against anaemia in patients treated for chronic hepatitis C. Nature 2010; 464: 405–408. 10.1038/nature08825 [DOI] [PubMed] [Google Scholar]
- 7.Kohli A, Shaffer A, Sherman A, Kottilil S. Treatment of hepatitis C: a systematic review. JAMA 2014; 312: 631–640. 10.1001/jama.2014.7085 [DOI] [PubMed] [Google Scholar]
- 8.Chhatwal J, Kanwal F, Roberts MS, Dunn MA. Cost-effectiveness and budget impact of hepatitis C virus treatment with sofosbuvir and ledipasvir in the United States. Ann Intern Med 2015; 162: 397–406. 10.7326/M14-1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pfeil AM, Reich O, Guerra IM, Cure S, Negro F, Müllhaupt B, et al. Cost-effectiveness analysis of sofosbuvir compared to current standard treatment in Swiss patients with chronic hepatitis C. PLOS One 2015; 10: e0126984 10.1371/journal.pone.0126984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cure S, Guerra I, Camma C, Craxi A, Carosi G. Cost-effectiveness of sofosbuvir plus ribavirin with or without pegylated interferon for the treatment of chronic hepatitis C in Italy. J Med Econ 2015; 18: 678–690. 10.3111/13696998.2015.1040024 [DOI] [PubMed] [Google Scholar]
- 11.Chimparlee N, Oota S, Phikulsod S, Tangkijvanich P, Poovorawan Y. Hepatitis B and hepatitis C virus in Thai blood donors. Southeast Asian J Trop Med Public Health 2011; 42: 609–615. [PubMed] [Google Scholar]
- 12.Suwanagool S, Tieangrim S, Ratanasuwan W, Mekanantagosol S, Luengrojanakul P, Kunasol P. Seroprevalence of anti-HCV among HIV-infected persons and general population. J Med Assoc Thai 1995; 78: 611–617. [PubMed] [Google Scholar]
- 13.Ratanasuwan W, Sonji A, Tiengrim S, Techasathit W, Suwanagool S. Serological survey of viral hepatitis A, B, and C at Thai Central Region and Bangkok: a population base study. Southeast Asian J Trop Med Public Health 2004; 35: 416–420. [PubMed] [Google Scholar]
- 14.Sunanchaikarn S, Theamboonlers A, Chongsrisawat V, Yoocharoen P, Tharmaphornpilas P, Warin- athien P, et al. Seroepidemiology and genotypes of hepatitis C virus in Thailand. Asian Pac J Allergy Immunol 2007; 25: 175–182. . [PubMed] [Google Scholar]
- 15.Akkarathamrongsin S, Hacharoen P, Tangkijvanich P, Theamboonlers A, Tanaka Y, Mizokami M, et al. Molecular epidemiology and genetic history of hepatitis C virus subtype 3a infection in Thailand. Intervirology 2013; 56: 284–294. 10.1159/000351621 [DOI] [PubMed] [Google Scholar]
- 16.Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Mol Biol Evol 2013; 30: 2725–2729. 10.1093/molbev/mst197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sistayanarain A, Kunthalert D, Vipsoongnern Y. A shift in the hepatitis C virus genotype dominance in blood donor samples from Thailand. Mol Biol Rep 2011; 38: 4287–4290. 10.1007/s11033-010-0552-x [DOI] [PubMed] [Google Scholar]
- 18.Zhang Z, Yao Y, Wu W, Feng R, Wu Z, Cun W, et al. Hepatitis C virus genotype diversity among intra- venous drug users in Yunnan Province, Southwestern China. PLOS One 2013; 8: e82598 10.1371/journal.pone.0082598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fu Y, Qin W, Cao H, Xu R, Tan Y, Lu T, et al. HCV 6a prevalence in Guangdong province had the origin from Vietnam and recent dissemination to other regions of China: phylogeographic analyses. PLOS One 2012; 7: e28006 10.1371/journal.pone.0028006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ng KT, Lee YM, Al-Darraji HA, Xia X, Takebe Y, Chan KG, et al. Genome sequence of the hepatitis C virus subtype 6n isolated from Malaysia. Genome Announc 2013; 1: e00168–12. 10.1128/genomeA.00168-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanistanon D, Neelamek M, Dharakul T, Songsivilai S. Genotypic distribution of hepatitis C virus in different regions of Thailand. J Clin Microbiol 1997; 35: 1772–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kao HH, Chen KS, Lin CL, Chang JJ, Lee CH. Utilization of Signal-to-Cutoff Ratio of Hepatitis C Virus Antibody Assay in Predicting HCV Viremia among Hemodialysis Patients. Nephron 2015; 130: 127–133. 10.1159/000430988 [DOI] [PubMed] [Google Scholar]
- 23.Vidimliski PD, Nikolov I, Geshkovska NM, Dimovski A, Rostaing L, Sikole A. Review: Occult hepatitis C virus infection: still remains a controversy. J Med Virol 2014; 86: 1491–1498. 10.1002/jmv.23979 [DOI] [PubMed] [Google Scholar]
- 24.Baid-Agrawal S, Schindler R, Reinke P, Staedtler A, Rimpler S, Malik B, et al. Prevalence of occult hepatitis C infection in chronic hemodialysis and kidney transplant patients. J Hepatol 2014; 60: 928–933. 10.1016/j.jhep.2014.01.012 [DOI] [PubMed] [Google Scholar]
- 25.Sawanpanyalert P, Boonmar S, Maeda T, Matsuura Y, Miyamura T. Risk factors for hepatitis C virus infection among blood donors in an HIV-epidemic area in Thailand. J Epidemiol Community Health 1996; 50: 174–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luksamijarulkul P, Thammata N, Tiloklurs M. Seroprevalence of hepatitis B, hepatitis C and human immunodeficiency virus among blood donors, Phitsanulok Regional Blood Center, Thailand. Southeast Asian J Trop Med Public Health 2002; 33: 272–279. [PubMed] [Google Scholar]
- 27.Songsivilai S, Jinathongthai S, Wongsena W, Tiangpitayakorn C, Dharakul T. High prevalence of hepatitis C infection among blood donors in northeastern Thailand. Am J Trop Med Hyg 1997; 57: 66–69. [DOI] [PubMed] [Google Scholar]
- 28.Thaikruea L, Thongsawat S, Maneekarn N, Netski D, Thomas DL, Nelson KE. Risk factors for hepatitis C virus infection among blood donors in northern Thailand. Transfusion 2004; 44: 1433–1440. [DOI] [PubMed] [Google Scholar]
- 29.Ishida T, Takao S, Settheetham-Ishida W, Tiwawech D. Prevalence of hepatitis B and C virus infection in rural ethnic populations of Northern Thailand. J Clin Virol 2002; 24: 31–35. [DOI] [PubMed] [Google Scholar]
- 30.Verachai V, Phutiprawan T, Theamboonlers A, Chinchai T, Tanprasert S, Haagmans BL, et al. Preva- lence and genotypes of hepatitis C virus infection among drug addicts and blood donors in Thailand. Southeast Asian J Trop Med Public Health 2002; 33: 849–851. [PubMed] [Google Scholar]
- 31.Jittiwutikarn J, Thongsawat S, Suriyanon V, Maneekarn N, Celentano D, Razak MH, et al. Hepatitis C infection among drug users in northern Thailand. Am J Trop Med Hyg 2006; 74: 1111–1116. [PubMed] [Google Scholar]
- 32.Garcia Comas L, Ordobas Gavin M, Sanz Moreno JC, Ramos Blazquez B, Gutierrez Rodriguez A, Astray Mochales J, et al. Prevalence of hepatitis C antibodies in the population aged 16–80 years in the Community of Madrid 2008–2009. J Med Virol 2015; 87: 1697–1701. 10.1002/jmv.24219 [DOI] [PubMed] [Google Scholar]
- 33.Hart-Malloy R, Carrascal A, Dirienzo AG, Flanigan C, McClamroch K, Smith L. Estimating HCV prevalence at the state level: a call to increase and strengthen current surveillance systems. Am J Public Health 2013; 103: 1402–1405. 10.2105/AJPH.2013.301231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribu- tion of the hepatitis C virus infection. J Hepatol 2014; 61: S45–S57. 10.1016/j.jhep.2014.07.027 [DOI] [PubMed] [Google Scholar]
- 35.Phanuphak P, Locharernkul C, Panmuong W, Wilde H. A report of three cases of AIDS in Thailand. Asian Pac J Allergy Immunol 1985; 3: 195–199. [PubMed] [Google Scholar]
- 36.Choo QL, Kuo G, Weiner AJ, Overby LR, Bradley DW, Houghton M. Isolation of a cDNA clone derived from a blood-borne non-A, non-B viral hepatitis genome. Science 1989; 244: 359–362. [DOI] [PubMed] [Google Scholar]
- 37.Houghton M. Discovery of the hepatitis C virus. Liver Int 2009; 29: 82–88. 10.1111/j.1478-3231.2008.01925.x [DOI] [PubMed] [Google Scholar]
- 38.Nguyen VT, McLaws ML, Dore GJ (2007) Prevalence and risk factors for hepatitis C infection in rural north Vietnam. Hepatol Int 1: 387–393. 10.1007/s12072-007-9008-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Do SH, Yamada H, Fujimoto M, Ohisa M, Matsuo J, Akita T, et al. High prevalences of hepatitis B and C virus infections among adults living in Binh Thuan province, Vietnam. Hepatol Res 2014. 10.1111/hepr.12350 [DOI] [PubMed] [Google Scholar]
- 40.Lwin AA, Shinji T, Khin M, Win N, Obika M, Okada S, et al. Hepatitis C virus genotype distribution in Myanmar: Predominance of genotype 6 and existence of new genotype 6 subtype. Hepatol Res 2007; 37: 337–345. [DOI] [PubMed] [Google Scholar]
- 41.Yamada H, Fujimoto M, Svay S, Lim O, Hok S, Goto N, et al. Seroprevalence, genotypic distribution and potential risk factors of hepatitis B and C virus infections among adults in Siem Reap, Cambodia. Hepatol Res 2014. 10.1111/hepr.12367 [DOI] [PubMed] [Google Scholar]
- 42.Akkarathamrongsin S, Praianantathavorn K, Hacharoen N, Theamboonlers A, Tangkijvanich P, Poovorawan Y. Seroprevalence and Genotype of Hepatitis C Virus among Immigrant Workers from Cam- bodia and Myanmar in Thailand. Intervirology 2011; 54: 10–16. 10.1159/000318884 [DOI] [PubMed] [Google Scholar]
- 43.Arguillas MO, Domingo EO, Tsuda F, Mayumi M, Suzuki H. Seroepidemiology of hepatitis C virus infection in the Philippines: a preliminary study and comparison with hepatitis B virus infection among blood donors, medical personnel, and patient groups in Davao, Philippines. Gastroenterol Jpn 1991; 26: 170–175. [DOI] [PubMed] [Google Scholar]
- 44.Inoue Y, Sulaiman HA, Matsubayashi K, Julitasari, Iinuma K, Ansari A, et al. Genotypic analysis of hep- atitis C virus in blood donors in Indonesia. Am J Trop Med Hyg 2000; 62: 92–98. [DOI] [PubMed] [Google Scholar]
- 45.Caruana SR, Kelly HA, De Silva SL, Chea L, Nuon S, Saykao P, et al. Knowledge about hepatitis and previous exposure to hepatitis viruses in immigrants and refugees from the Mekong Region. Aust N Z J Public Health 2005; 29: 64–68. [DOI] [PubMed] [Google Scholar]
- 46.Wang JE. A study on the epidemiology of hepatitis C infection among blood donors in Singapore. J Public Health Med 1995; 17: 387–391. [PubMed] [Google Scholar]
- 47.Haslina MN, Khairiah Y, Zainy DZ, Shafini MY, Rosnah B, Marini R. Seroprevalence of hepatitis C virus infection among blood donors in a teaching hospital in northeastern Malaysia. Southeast Asian J Trop Med Public Health 2012; 43: 668–673. [PubMed] [Google Scholar]
- 48.Gane EJ, Hyland RH, An D, Svarovskaia E, Pang PS, Brainard D, et al. Efficacy of Ledipasvir and Sofosbuvir, With or Without Ribavirin, for 12 Weeks in Patients With HCV Genotype 3 or 6 Infection. Gastroenterology 2015; 149:1454–1461.e1. 10.1053/j.gastro.2015.07.063 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
The HCV genotype based on the core and NS5B sequences are indicated.
(DOCX)
(DOCX)
Data Availability Statement
All sequence files are available from the GenBank database (accession numbers KT921354-KT921395).