Abstract
Background: African Americans' beliefs about end-of-life care may differ from those of whites, but racial differences in advance care planning (ACP) outcomes are unknown.
Objective: The aim of this study was to compare the efficacy of an ACP intervention on preparation for end-of-life decision making and post-bereavement outcomes for African Americans and whites on dialysis.
Method: A secondary analysis of data from a randomized trial comparing an ACP intervention (Sharing Patient's Illness Representations to Increase Trust [SPIRIT]) with usual care was conducted. There were 420 participants, 210 patient-surrogate dyads (67.4% African Americans), recruited from 20 dialysis centers in North Carolina. The outcomes of preparation for end-of-life decision making included dyad congruence on goals of care, surrogate decision-making confidence, a composite of the two, and patient decisional conflict assessed at 2, 6, and 12 months post-intervention. Surrogate bereavement outcomes included anxiety, depression, and post-traumatic distress symptoms assessed at 2 weeks, and at 3 and 6 months after the patient's death.
Results: SPIRIT was superior to usual care in improving dyad congruence (odds ration [OR] = 2.31, p = 0.018), surrogate decision-making confidence (β = 0.18, p = 0.021), and the composite (OR = 2.19, p = 0.028) 2 months post-intervention, but only for African Americans. SPIRIT reduced patient decisional conflict at 6 months for whites and at 12 months for African Americans. Finally, SPIRIT was superior to usual care in reducing surrogates' bereavement depressive symptoms for African Americans but not for whites (β = −3.49, p = 0.003).
Conclusion: SPIRIT was effective in improving preparation for end-of-life decision-making and post-bereavement outcomes in African Americans.
Introduction
End-stage renal disease (ESRD) currently affects 640,000 people in the United States.1 Despite the advances in dialysis, adjusted all-cause mortality rates are 6 to 8 times greater for dialysis patients than for individuals in the general age-matched Medicare population.1 The importance of advance care planning (ACP) in dialysis care is well recognized by stakeholders, including patients, families, and dialysis care providers.2–6 However, few studies have demonstrated the beneficial impact of an ACP intervention in dialysis patients.7
African Americans, comprising approximately 31% of the ESRD population, are thought to prefer more aggressive treatment at the end of life,8 to be less likely to have a do not resuscitate (DNR) order,9 and to be less amenable to using advance directives (ADs) compared with whites.10,11 Such differences might be associated with health and illness experiences that differ between African Americans and whites as these experiences are influenced by socioeconomic status, marriage, family experiences, and other cumulative life situations.12 African Americans are more likely than other racial/ethnic groups in the United States to be religiously affiliated and to adhere to ideologies that may influence decision making about issues such as discontinuation of life-sustaining treatments.13 However, despite knowledge that such beliefs are important in end-of-life decision making, little has been done to develop and test an ACP intervention for African Americans that takes such beliefs into consideration.14–16
To address these gaps, we tested the long-term effects of an ACP intervention entitled SPIRIT (Sharing Patient's Illness Representations to Increase Trust) on preparation for end-of-life decision making for dialysis patients and surrogates and on bereavement outcomes for surrogates. SPIRIT was based on the Representational Approach to Patient Education17,18 and designed to help patients and surrogates understand the patient's illness and implications for end-of-life decision making. An intervention that uses the Representational Approach first establishes an understanding of the cognitive, emotional, and spiritual or religious aspects of the patient's representation (beliefs or understandings) of his or her illness. These understandings serve as a foundation for the interventionist to provide individualized health care information.19 Results of the intention-to-treat analysis, reported elsewhere, revealed SPIRIT was superior to usual care in improving preparation for end-of-life decision making and bereavement outcomes.20 Here, as a planned analysis, we examined whether the effects of SPIRIT differ between African Americans and whites on preparation for end-of-life decision making for patients and surrogates and on bereavement outcomes for surrogates.
Methods
Study design
The original study was a two-group randomized controlled trial with measures of patient and surrogate preparedness at baseline and 2, 6, and 12 months later, and measures of surrogate bereavement outcomes at baseline, 2 weeks, and 3 and 6 months after the patient's death. Dyads were randomized to SPIRIT or usual care with stratification by race (African American versus white), dialysis center type (university-affiliated versus non-affiliated), and dialysis modality (hemodialysis versus peritoneal). The University of North Carolina at Chapel Hill Institutional Review Board (IRB) approved the study. The clinicaltrials.gov Identifier is NCT01259011 (A Representational Intervention to Promote Preparation for End-of-Life Decision Making).
Setting and participants
Patients recruited from 20 free-standing outpatient dialysis centers in eight counties in North Carolina were age 18 years or older; self-identified African American or white, had been on dialysis for at least 6 months prior to enrollment, had a Charlson Comorbidity Index (CCI)21,22 score ≥6 or CCI = 5 and were hospitalized in the last 6 months, were English-speaking, had no hearing impairment, had <3 errors on the Short Portable Mental Status Questionnaire,23 and had an English-speaking surrogate over age 18 who could participate. We randomized 210 dyads:141 African American dyads and 69 white dyads.
Interventions
Usual care
As required by the Centers for Medicare and Medicaid Services (CMS),24 written information on ADs was provided to every patient on the first day of dialysis, and a social worker encouraged patients to complete an AD and addressed questions about life-sustaining treatments. A nephrologist (or physician assistant or nurse practitioner) reviewed resuscitation statements with the patient to determine whether the patient wanted a DNR order at the dialysis center. If completed, the AD and DNR were placed in the medical record. If there was no DNR order in the record, a full code was presumed.
Intervention
Dyads randomized to intervention received usual care plus SPIRIT. SPIRIT was conducted by one of three nurse interventionists using an intervention guide. The interventionists had at least 2 years of clinical experience and had completed a competency-based training program.
SPIRIT included two sessions. During the first session at the dialysis center, the interventionist assessed cognitive, emotional, and spiritual/religious aspects of the dyad's representations of (beliefs and understanding about) the patient's illness, prognosis, and end-of-life care. This assessment allowed the interventionist to then provide individualized information about topics such as the effectiveness of life-sustaining treatment for people with ESRD, and to assist the patient in examining his/her values about life-sustaining treatment at the end of life. The interventionist actively involved the surrogate in the discussion and helped the surrogate prepare for being a decision-maker and for the emotional burden of end-of-life decision making.
A goals-of-care document was completed at the end of the session to indicate the patient's preferences. A brief second session was delivered 2 weeks later at the patient's home (to reduce the burden of travel to the center). During the session, the patient's goals-of-care document and resuscitation preferences were reviewed again. The interventionist explored potential family conflicts and encouraged the dyad to talk with other family members and to complete a health care power of attorney. The interventionist then created a written summary of information about the patient's end-of-life preferences, communicated those preferences to dialysis staff, and placed the summary in the medical record.
Of the dyads randomized to SPIRIT, 36 white dyads (97.3%) and 71 African American dyads (98.6%) received Session I; of those, 33 (91.7%) whites and 67 (94.4%) African Americans received Session II. Session I averaged 85 minutes for whites and 81 minutes for African Americans. Session II averaged 21 minutes for whites and 20 minutes for African Americans.
Measurement
Preparedness outcomes
Dyad congruence, patient decisional conflict, and surrogate decision-making confidence were measured. Dyad congruence was assessed using the goals-of-care document,15 which included two scenarios describing medical conditions that commonly occur in ESRD patients. In the first, the patient developed a severe complication and could not speak for himself/herself; the medical team believed recovery unlikely and continuing life-sustaining treatment, including dialysis, would no longer be beneficial. In the second scenario, the patient developed advanced dementia. Each scenario had three response options: “The goals of care should focus on delaying my death, and thus I want to continue life-sustaining treatment,” “The goals of care should focus on my comfort and peace, and thus I do not want life-sustaining treatment, including dialysis,” and “I am not sure.” Patient and surrogate responses to these scenarios were compared to determine dyad congruence—either congruent in both scenarios or incongruent. If both members of the dyad endorsed “I am not sure,” they were considered incongruent.
Patient decisional conflict was measured using the 13-item Decisional Conflict Scale (DCS)25; higher scores indicate greater difficulty in decision making (score range 1–5). Surrogate decision-making confidence was measured using the 5-item Decision Making Confidence (DMC) scale15,26 in which higher scores reflect greater comfort in performing as a surrogate (score range 0–4). A composite outcome was created to differentiate surrogates who understand the patient's wishes and feel confident in their role from those who do not (i.e., understand the wishes but lack confidence, misunderstand the wishes but feel confident, or neither understand the patient's wishes nor feel confident);15,26 dyads were grouped as congruent in both scenarios and surrogate DMC score ≥3 (“Confident” to “Very Confident”), or not.
Bereavement outcomes
Surrogates' symptoms of anxiety and depression were measured using the Hospital Anxiety and Depression Scale27; subscale scores range from 0 to 21 with higher scores indicating greater symptom severity. The intensity of post-traumatic distress symptoms was assessed using the Post-Traumatic Symptoms Scale-10 (PTSS-10).28 Higher scores indicate more intense symptoms (range 10–70).
Patients completed the 12-item Functional Assessment of Chronic Illness Therapy (FACIT-Sp),29 a reliable and validated scale that measures the extent to which individuals have experienced spiritual well-being in the past week on a 5-point scale from 0 (Not at All) to 4 (Very Much).30 FACIT-Sp has three subscales (4 items each): meaning (e.g., “I feel a sense of purpose in life”), peace (“I feel peaceful”), and faith (“My illness has strengthened my faith or spiritual beliefs”). A higher score indicates greater spiritual well-being.
Statistical analysis
Descriptive statistics were used to summarize participants' characteristics. χ2 tests and t tests or analysis of variance were performed as appropriate to compare group difference within race and to compare African Americans with whites in baseline characteristics.
Most missing data on preparedness outcomes were due to deaths of patients (n = 30). Because the study was not powered for formal testing of the interaction between SPIRIT and race, we examined intervention effects within each race using generalized estimating equation (GEE) methods.31 For preparation for end-of-life decision-making outcomes, a group indicator, time, the baseline value, and the interaction between SPIRIT and time were included in GEE models for each racial group. For bereavement outcomes, SPIRIT-time interaction was not included in the models due to the small sample size (n = 45).
To identify potential covariates associated with the study outcomes within each race, the baseline characteristics (e.g., age) were examined using GEE models adjusting for intervention, time, and the baseline value of each outcome. Then, we entered the covariates that were significantly associated with any of the study outcomes into a GEE model to examine the effect of the covariate on the outcome within race after adjusting for intervention, time, the interaction between SPIRIT and time, and the baseline value of the outcome. All analyses were conducted using SAS software version 9.3 (SAS Institute Inc., Cary, NC).
Results
Sample description
African Americans comprised 67.1% (n = 141) of the sample. Compared with whites, African American patients were more likely to be women (66.7% versus 37.7%, χ2 = 15.9, p < 0.001), younger (mean [M] = 60.6 versus 65.2, t = 2.9, p = 0.005), on dialysis for a longer time (M = 4.9 versus 3.1, t = 3.6, p = 0.003), have less education (M = 12.5 versus 13.4, t = 2.1, p = 0.04), have lower incomes (M = 3.1 versus 4.1, t = 4.5, p < 0.001), rate the importance of spirituality more highly (M = 3.4 versus 2.9, t = 5.1, p < 0.001), and have a higher total spiritual well-being (FACIT-Sp) score (M = 39.0 versus 33.3, t = 5.1, p < 0.001) and subscale scores (all ps < 0.01), and be less likely to have an advance directive (11.3% versus 33.3%, χ2 = 14.8, p < 0.001).
African American and white surrogates were similar in baseline characteristics except that African American surrogates were more likely to rate the importance of spirituality in life higher compared with whites (M = 3.5 versus 3.1, t = 3.2, p = 0.002). The SPIRIT and control groups within race were similar in baseline characteristics. Table 1 presents baseline characteristics of participants by racial group.
Table 1.
Baseline Characteristics of Participants by Group within Race
| Participants, no. (%) | ||||
|---|---|---|---|---|
| Whites (n = 69) | African Americans (n = 141) | |||
| Characteristics | SPIRIT (n = 37) | Control (n = 32) | SPIRIT (n = 72) | Control (n = 69) |
| Patient, sociodemographic | ||||
| Age, mean (SD), years | 63.8 (12.5) | 66.8 (11.0) | 59.6 (10.6) | 61.5 (10.8) |
| Women | 14 (37.8) | 12 (37.5) | 51 (70.8) | 43 (62.3) |
| Marital status | ||||
| Married/living with partner | 22 (59.5) | 16 (50.0) | 34 (47.2) | 27 (39.1) |
| Divorced/separated/widowed | 12 (32.4) | 15 (46.9) | 28 (38.9) | 34 (49.3) |
| Never married | 3 (8.1) | 1 (3.1) | 10 (13.9) | 8 (11.6) |
| Formal education completed, mean (SD), years | 13.7 (3.4) | 13.0 (3.2) | 12.8 (2.7) | 12.2 (2.6) |
| Extent of following religious customs | ||||
| Never/sometimes | 14 (37.8) | 15 (46.9) | 17 (23.6) | 25 (36.2) |
| Frequently/always | 23 (63.1) | 17 (53.1) | 55 (76.4) | 44 (63.8) |
| Importance of spirituality in life | ||||
| Not at all/somewhat important | 13 (35.1) | 10 (31.3) | 5 (6.9) | 4 (5.8) |
| Very/extremely important | 24 (73.0) | 22 (68.8) | 67 (93.1) | 65 (94.2) |
| Annual income | ||||
| <$20,000 | 13 (35.1) | 12 (37.5) | 40 (55.6) | 41 (59.4) |
| $20,000–$50,000 | 18 (48.6) | 12 (37.5) | 22 (30.6) | 21 (30.4) |
| >$50,000 | 6 (16.2) | 7 (21.9) | 8 (11.1) | 6 (8.7) |
| Refused to answer | 0 | 1 (3.1) | 2 (2.8) | 2 (2.9) |
| Previously lost a close family member or a friend | 37 (100) | 31 (98.9) | 71 (98.6) | 67 (97.1) |
| Involved in tough medical decisions for the lost family member or friend | 14 (37.8) | 7 (21.9) | 22 (30.6) | 18 (26.1) |
| FACIT-Sp spiritual well-being total, mean (SD)a | 32.8 (8.1) | 33.9 (8.1) | 39.1 (7.2) | 39.0 (7.6) |
| FACIT-meaning subscale | 11.7 (3.2) | 11.8 (2.7) | 13.0 (2.7) | 13.2 (2.9) |
| FACIT-peace | 10.0 (3.5) | 10.5 (3.0) | 11.9 (3.1) | 11.9 (3.5) |
| FACIT-faith | 11.2 (3.8) | 11.6 (4.2) | 14.1 (2.5) | 14.1 (2.5) |
| Patient, clinical | ||||
| Hemodialysis | 33 (89.2) | 28 (87.5) | 72 (100) | 68 (98.6) |
| Years on dialysis | ||||
| Median (IQR) | 2.3 (1.1 – 4.5) | 2.0 (1.1–4.3) | 4.6 (2.3–6.9) | 2.6 (1.4–5.3) |
| Mean (SD) | 3.2 (3.0) | 2.9 (2.3) | 5.1 (3.5) | 4.7 (5.6) |
| CCI illness severity, mean (SD) | 8.4 (1.9) | 8.3 (2.2) | 8.1 (1.8) | 8.1 (1.6) |
| Has an advance directive | 13 (35.1) | 10 (31.3) | 8 (11.1) | 8 (11.6) |
| Do not resuscitate order at the center | 4 (10.8) | 1 (3.1) | 2 (2.8) | 1 (1.4) |
| Surrogate, sociodemographic | ||||
| Relationship to patient | ||||
| Spouse/partner | 19 (51.4) | 14 (43.8) | 25 (34.7) | 23 (33.3) |
| Parent | 7 (18.9) | 14 (43.8) | 20 (27.8) | 24 (34.8) |
| Sibling | 3 (8.1) | 1 (3.1) | 13 (18.1) | 10 (14.5) |
| Child | 3 (8.1) | 1 (3.1) | 5 (6.9) | 3 (4.3) |
| Friend | 5 (13.5) | 1 (3.1) | 1 (1.4) | 3 (4.3) |
| Other(e.g., other relatives, in-laws) | 0 | 1 (3.1) | 8 (11.1) | 6 (8.7) |
| Age, mean (SD), years | 56.2 (13.5) | 56.6 (14.6) | 53.1 (12.9) | 52.9 (14.0) |
| Women | 27 (73.0) | 28 (87.5) | 48 (66.7) | 49 (71.0) |
| Marital status | ||||
| Married/living with partner | 29 (78.4) | 25 (78.2) | 44 (61.1) | 38 (55.1) |
| Divorced/separated/widowed | 5 (13.5) | 6 (18.7) | 14 (19.4) | 16 (23.2) |
| Never married 1 | 3 (8.1) | 1 (3.1) | 14 (19.4) | 15 (21.7) |
| Formal education completed, mean (SD), years | 13.6 (2.9) | 13.8 (1.7) | 13.5 (2.4) | 13.1 (2.1) |
| Extent of following religious customs | ||||
| Never/sometimes | 8 (21.6) | 7 (21.9) | 19 (26.4) | 13 (18.8) |
| Frequently/always | 29 (78.3) | 25 (78.1) | 53 (73.6) | 56 (81.2) |
| Importance of spirituality in life | ||||
| Not at all/somewhat important | 4 (10.8) | 10 (31.3) | 4 (5.6) | 4 (5.8) |
| Very/extremely important | 33 (89.2) | 22 (68.8) | 68 (94.5) | 65 (94.2) |
| Annual income | ||||
| < $20,000 | 8 (21.6) | 7 (21.9) | 20 (27.8) | 21 (30.4) |
| $20,000–$50,000 | 19 (51.4) | 12 (37.5) | 32 (44.4) | 31 (44.9) |
| >$50,000 | 9 (24.3) | 12 (37.5) | 17 (23.6) | 13 (18.8) |
| Refused to answer | 1 (2.7) | 1 (3.1) | 3 (4.2) | 4 (5.8) |
| Previously lost a close family member or a friend | 34 (91.9) | 31 (96.9) | 69 (95.8) | 67 (97.1) |
| Involved in tough medical decisions for the lost family member or friend | 16 (43.2) | 9 (28.1) | 23 (31.9) | 26 (37.7) |
Peterman et al.29 FACIT-Sp total scores range from 0 to 48, with a higher score indicating greater spiritual well-being.
Due to rounding up, percentages may not add up to 100.
CCI, Charlson Comorbidity Index; FACIT, Functional Assessment of Chronic Illness Therapy; IRQ, interquartile range; SD, standard deviation; SPIRIT, Sharing Patient's Illness Representations to Increase Trust.
The mean age of the 45 patients who died during the study was 64.6 (standard deviation [SD] = 12.6). Mean (SD) survival months after randomization for the 21 deceased whites was 11.5 (9.2), and for the 24 African Americans was 13.6 (10.8). Within race, survival months between the SPIRIT and control groups were similar. Patients who died and their surrogate's sociodemographic characteristics were similar between SPIRIT and control groups within race. Five whites and five African American patients died suddenly requiring no surrogate decision making; 16 white surrogates and 19 African American surrogates were involved in end-of-life decision making.
Intervention effects on outcomes by race
Preparedness
The effect of SPIRIT on dyad congruence was not significant for whites at any time point (Table 2), whereas for African Americans, the number of dyads congruent in goals of care was significantly higher in SPIRIT than in control at 2 months (OR = 2.31 [95% confidence interval (CI), 1.16 to 4.60]; p = 0.018). SPIRIT significantly reduced patient decisional conflict at 6 months for whites (β = −0.24 [95% CI, −0.44 to −0.04]; p = 0.018) and at 12 months for African Americans (β = −0.18 [95% CI, −0.33 to −0.03]; p = 0.021). SPIRIT did not improve surrogate decision-making confidence for whites but did so at 2 months for African Americans (β = 0.18 [95% CI, 0.03 to 0.33]; p = 0.021). There was no difference between SPIRIT and controls in the composite outcome for whites; but African Americans in SPIRIT fared better at 2 months (OR = 2.19 [95% CI, 1.09 to 4.38]; p = 0.028) than did controls.
Table 2.
Intervention Effects on the Preparedness Outcomes by Racea
| Outcomes | SPIRIT | Control | Odds ratio or regression coefficient(95% CI) | P value |
|---|---|---|---|---|
| Dyad congruence, no. (%) | ||||
| Whites | (n = 37) | (n = 32) | ||
| Baseline | 21 (56.8) | 18 (56.3) | - | |
| 2-month follow-up | 24 (68.6) | 20 (64.5) | 1.14 (0.40 to 3.21) | 0.81 |
| 6-month follow-up | 26 (78.8) | 23 (79.3) | 0.76 (0.20 to 2.87) | 0.69 |
| 12-month follow-up | 17 (65.4) | 19 (82.6) | 0.32 (0.08 to 1.24) | 0.10 |
| African Americans | (n = 72) | (n = 69) | ||
| Baseline | 26 (36.1) | 25 (36.3) | - | |
| 2-month follow-up | 40 (60.6) | 28 (40.6) | 2.31 (1.16 to 4.60) | 0.018 |
| 6-month follow-up | 40 (64.5) | 36 (53.7) | 1.45 (0.69 to 3.05) | 0.32 |
| 12-month follow-up | 34 (57.6) | 33 (52.4) | 1.16 (0.57 to 2.39) | 0.68 |
| Patient DCS, mean (SD) | ||||
| Whites | ||||
| Baseline | 1.7 (0.5) | 1.7 (0.4) | - | |
| 2-month follow-up | 1.6 (0.4) | 1.7 (0.4) | −0.15 (−0.32 to 0.01) | 0.069 |
| 6-month follow-up | 1.5 (0.5) | 1.8 (0.4) | −0.24 (−0.44 to −0.04) | 0.018 |
| 12-month follow-up | 1.5 (0.4) | 1.7 (0.4) | −0.21 (−0.43 to 0.006) | 0.056 |
| African Americans | ||||
| Baseline | 1.6 (0.5) | 1.7 (0.6) | - | |
| 2-month follow-up | 1.8 (0.5) | 1.7 (0.4) | 0.06 (−0.08 to 0.21) | 0.41 |
| 6-month follow-up | 1.7 (0.4) | 1.8 (0.4) | −0.05 (−0.19 to 0.08) | 0.45 |
| 12-month follow-up | 1.7 (0.4) | 1.9 (0.5) | −0.18 (−0.33 to −0.03) | 0.021 |
| Surrogate DMC, mean (SD) | ||||
| Whites | ||||
| Baseline | 3.4 (0.5) | 3.7 (0.4) | - | |
| 2-month follow-up | 3.7 (0.3) | 3.7 (0.3) | 0.006 (−0.13 to 0.14) | 0.93 |
| 6-month follow-up | 3.7 (0.3) | 3.7 (0.3) | 0.008 (−0.15 to 0.17) | 0.93 |
| 12-month follow-up | 3.8 (0.3) | 3.7 (0.4) | 0.04 (−0.15 to 0.22) | 0.69 |
| African Americans | ||||
| Baseline | 3.6 (0.6) | 3.6 (0.5) | - | |
| 2-month follow-up | 3.7 (0.4) | 3.6 (0.5) | 0.18 (0.03 to 0.33) | 0.021 |
| 6-month follow-up | 3.7 (0.5) | 3.6 (0.5) | 0.15 (−0.009 to 0.31) | 0.064 |
| 12-month follow-up | 3.7 (0.4) | 3.7 (0.5) | 0.05 (−0.11 to 0.21) | 0.52 |
| Composite outcome, no. (%) | ||||
| Whites | ||||
| Baseline | 21 (56.8) | 18 (56.3) | - | |
| 2-month follow-up | 24 (68.6) | 20 (64.5) | 1.13 (0.40 to 3.22) | 0.82 |
| 6-month follow-up | 25 (75.8) | 23 (79.3) | 0.62 (0.17 to 2.28) | 0.47 |
| 12-month follow-up | 17 (65.4) | 18 (78.3) | 0.43 (0.12 to 1.53) | 0.19 |
| African Americans | ||||
| Baseline | 25 (34.7) | 25 (36.3) | - | |
| 2-month follow-up | 38 (57.6) | 27 (39.1) | 2.19 (1.09 to 4.38) | 0.028 |
| 6-month follow-up | 39 (62.9) | 32 (47.8) | 1.78 (0.86 to 3.69) | 0.12 |
| 12-month follow-up | 34 (57.6) | 31 (49.2) | 1.36 (0.66 to 2.77) | 0.40 |
Each GEE model included a group indicator, time, the baseline and the interaction between intervention and time.
CI, confidence interval; DCS, Decisional Conflict Scale; DMC, Decision-Making Confidence; SD, standard deviation; SPIRIT, Sharing Patient's Illness Representations to Increase Trust.
Bereavement
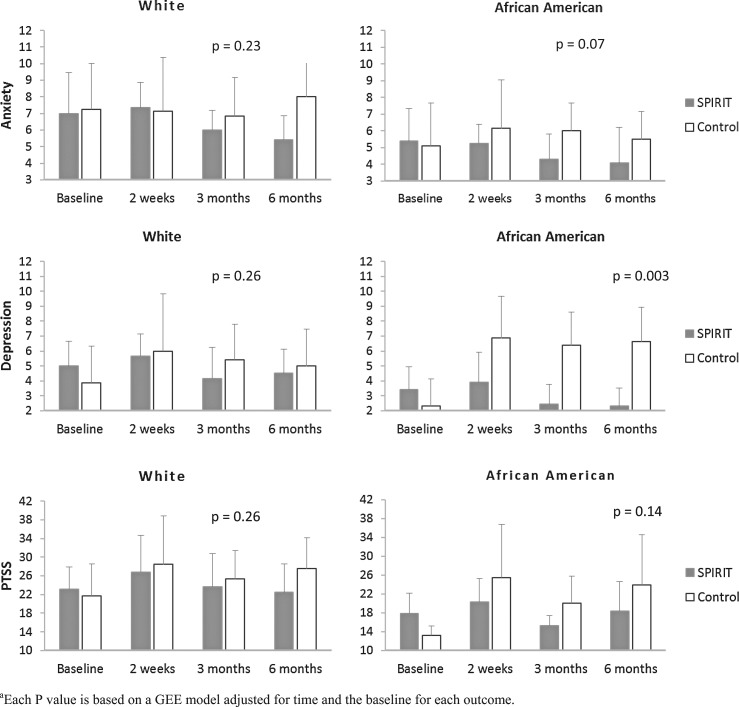
Figure 1 presents the intervention effects on anxiety and depressive symptoms and post-traumatic symptom scores by race after adjusting for time and the baseline value. At 2 weeks post-death, both SPIRIT and control groups for both races had a slight increase in these symptoms. After adjusting for time and the baseline value, there was a significant intervention effect on reducing depressive symptoms for African Americans (β = −3.49 [95% CI, −5.82 to −1.17]; p = 0.003).
FIG. 1.
Intervention effects on bereavement outcomes by race. Each p value is based on a generalized estimating equation (GEE) model adjusted for time and the baseline for each outcome. PTSS, Post-Traumatic Symptoms Scale.
Potential covariates associated with outcomes
We examined the bivariate relationships between the baseline characteristics that differed between African Americans and whites (described above) and study outcomes. Only spiritual well-being (FACIT-Sp) and comorbidity (CCI) were significantly associated with preparation for end-of-life decision making. No surrogate baseline characteristics were associated with surrogates' post-death bereavement outcomes.
Table 3 presents the relationships of FACIT subscales and CCI with preparation for end-of-life decision making after adjusting for intervention group, time, the interaction between intervention group and time, and the baseline value of each outcome. One spiritual well-being subscale, FACIT-meaning, was inversely associated with dyad congruence and the composite, but only for African Americans; a 1 SD ( = 2.8) increase in this score was associated with 25% reduction in the odds of the dyad being congruent and 34% reduction in the odds of having a better composite outcome. CCI was positively associated with dyad congruence, surrogate decision-making confidence (β = 0.04 [95% CI, 0.01 to 0.08]; p = 0.026), and the composite, but only for African Americans; a 1 SD ( = 1.7) increase in CCI was associated with 36% increase in the odds of the dyad being congruent and 46% increase in the odds of a better composite outcome.
Table 3.
Effects of Patient Spiritual Well-Being and Comorbidity on Dyad Congruence, Patient Decisional Conflict, Surrogate Decision-Making Confidence, and Composite Outcomea
| Dyad congruenceb | Patient DCS | Surrogate DMC | Composite outcomeb | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | Regression coefficient (95% CI) | Regression coefficient (95% CI) | OR (95% CI) | |||||
| Whites | African Americans | Whites | African Americans | Whites | African Americans | Whites | African Americans | |
| FACIT-meaning | 1.02 (0.92–1.13) | 0.91* (0.82–1.00) | 0.004 (−0.02–0.03) | 0.01 (−0.01–0.03) | - | - | 1.02 (0.92–1.13) | 0.88* (0.80–0.97) |
| FACIT-peace | 1.05 (0.95–1.15) | 0.95 (0.87–1.03) | −0.02 (−0.03–0.002) | 0.003 (−0.01–0.02) | - | - | 1.04 (0.95–1.14) | 0.92 (0.85–1.01) |
| FACIT-faith | 0.99 (0.88–1.12) | 0.93 (0.84–1.04) | −0.01 (−0.03–0.01) | −0.01 (−0.03–0.01) | - | - | 1.04 (0.95–1.14) | 0.93 (0.84–1.04) |
| CCI | 0.95 (0.78–1.16) | 1.21* (1.04–1.42) | −0.01 (−0.05–0.02) | 0.001 (−0.03–0.04) | −0.01 (−0.04–0.02) | 0.04* (0.01–0.08) | 0.97 (0.79–1.18) | 1.27** (1.08–1.48) |
p < 0.05; **p < 0.01.
Each generalized estimating equation (GEE) model included intervention, time, the interaction between intervention and time, the baseline, and the covariate.
Reference for dyad congruence = dyads not congruent in both scenarios; reference for composite outcome = dyads not congruent and/or surrogate DMC score <3.
CCI, Charlson Comorbidity Index; CI, confidence interval; DCS, Decisional Conflict Scale; DMC, Decision-Making Confidence; FACIT, Functional Assessment of Chronic Illness Therapy (completed by patients only); OR, odds ratio.
Discussion
SPIRIT was effective in improving preparation for end-of-life decision making and post-bereavement outcomes in African Americans. SPIRIT reduced patient decisional conflict at 6 months for whites and at 12 months for African Americans. Finally, SPIRIT reduced surrogates' bereavement depressive symptoms for African Americans. However, we did not find such effects in whites.
Data on differential effects of psychosocial and educational interventions between African Americans and whites are rare and inconsistent mainly because only a small proportion of African Americans are included in most studies.32 However, in a study of peer mentoring on AD completion and psychosocial outcomes in 208 dialysis patients (37% to 39% African Americans) a greater percentage of patients receiving peer mentoring completed an AD compared with those in the control groups,14 an effect that was significant for African Americans but not for whites. Furthermore, the intervention showed a significant increase in subjective well-being in African Americans but not in whites. These two interventions, SPIRIT and peer mentoring, might align with African Americans' culture and familial, religious, and communal frame of reference33 by including a family member in the intervention (SPIRIT) or by using a peer-led intervention.
Our study revealed that whites in the control group improved in dyad congruence over time as they simply were asked to think about the scenarios in the goals-of-care document and answer thought-provoking questions repeatedly. This phenomenon, known as assessment effects,34–36 appeared to be as effective as SPIRIT for whites. However, for African Americans, controls did not benefit from assessment effects as much; rather, SPIRIT was needed to improve dyad congruence.
The CCI was positively associated and the FACIT-meaning subscale inversely associated with the preparedness outcomes among African Americans but not whites. The explanation for the positive association between CCI and dyad congruence might be that the patient's illness severity is visible to both patient and surrogate, thereby leading to congruence within the dyad. In contrast, the degree to which African American patients find purpose in life despite their severe illness may not be visible and may be too personal to share with the surrogate. This lack of visibility and lack of sharing might in turn lead the surrogate to misunderstand the patient's end-of-life preferences contributing to dyad incongruence. The literature consistently suggests the importance of spirituality in end-of-life decision making for many African Americans.9,37–46 Our study may offer additional data on the relationships between spiritual well-being and outcomes of ACP for African Americans, but further research is warranted.
Studies of bereaved family members of dialysis patients are rare, making it difficult to interpret why African American surrogates benefited from SPIRIT to a greater extent than did white surrogates. Although racial differences in depressive symptomatology have been reported,47,48 literature on racial differences in depression following the death of a loved one is limited, and no studies have compared African Americans with whites with respect to the impact of an ACP intervention on bereaved family members. One study has shown that African American caregivers of relatives with Alzheimer's disease reported greater perceived loss than did whites when a relative died.49 Similarly, our control group data reveal that depressive symptom scores in African American surrogates increased post-bereavement, supporting the adverse impact of the death of a loved one on African American surrogates. In contrast, in the SPIRIT group depressive symptom scores in African American surrogates decreased.
Although we found significant effects of SPIRIT in African Americans but not in whites, the original study was not powered to formally test the interaction between SPIRIT and race and to estimate racial effects. Thus, our analytic approach was exploratory. We used the self-identified race/ethnicity category for the analysis, which may be limited to capture the complex ethnic identity. Also, the original study was conducted in a single region in the United States and the data may not be generalizable to other regions or other individuals with similar characteristics. Nonetheless, our findings suggest that SPIRIT, an ACP intervention, is effective in improving preparation for end-of-life decision making and post-bereavement outcomes in African Americans.
Acknowledgments
This study was supported by a grant from the National Institutes of Health (R01NR011464) to M.S. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.U.S. Renal Data System. USRDS 2014 Annual Data Report: Epidemiology of Kidney Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2014 [Google Scholar]
- 2.Goff SL, Eneanya ND, Feinberg R, et al. : Advance care planning: A qualitative study of dialysis patients and families. Clin J Am Soc Nephrol 2015;10:390–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davison SN: Facilitating advance care planning for patients with end-stage renal disease: The patient perspectives. Clin J Am Soc Nephrol 2006;1:1023–1028 [DOI] [PubMed] [Google Scholar]
- 4.Davison SN, Jhangri GS, Holley JL, Moss AH: Nephrologists' reported preparedness for end-of-life decision-making. Clin J Am Soc Nephrol 2006;1:1256–1262 [DOI] [PubMed] [Google Scholar]
- 5.Renal Physicians Association: Shared Decision-making in the Appropriate Initiation of and Withdrawal from Dialysis: Clinical Practice Guideline, 2e. Renal Physicians Association, Rockville, MD, 2010 [Google Scholar]
- 6.Schell JO, Green JA, Tulsky JA, Arnold RM: Communication skills training for dialysis decision-making and end-of-life care in nephrology. Clin J Am Soc Nephrol 2013;8:675–680 [DOI] [PubMed] [Google Scholar]
- 7.Luckett T, Sellars M, Tieman J, et al. : Advance care planning for adults with CKD: A systematic integrative review. Am J Kidney Dis 2014;63:761–770 [DOI] [PubMed] [Google Scholar]
- 8.Hopp FP, Duffy SA: Racial variations in end-of-life care. J Am Geriatr Soc 2000;48:658–663 [DOI] [PubMed] [Google Scholar]
- 9.Karches KE, Chung GS, Arora V, Meltzer DO, et al. : Religiosity, spirituality, and end-of-life planning: A single-site survey of medical inpatients. J Pain Symptom Manage 2012;44:843–851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwak J, Haley WE: Current Research Findings on End-of-Life Decision Making Among Racially or Ethnically Diverse Groups. Gerontologist 2005;45:634–641 [DOI] [PubMed] [Google Scholar]
- 11.Pew Research Center: Views on end-of-life medical treatments. 2013. www.pewforum.org/2013/11/21/views-on-end-of-life-medical-treatments/ (Last accessedJune15, 2015)
- 12.Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Anderson NB, Bulatao RA, Cohen B. (eds). National Academies Press, Washington, D.C., 2004 [PubMed] [Google Scholar]
- 13.Pew Forum: A religious portrit of African Americans. Pew Forum on Religion & Public Life 2007;2015 [Google Scholar]
- 14.Perry E, Swartz J, Brown S, et al. : Peer mentoring: A culturally sensitive approach to end-of-life planning for long-term dialysis patients. Am J Kidney Dis 2005;46:111–119 [DOI] [PubMed] [Google Scholar]
- 15.Song MK, Ward SE, Happ MB, et al. Randomized controlled trial of SPIRIT: An effective approach to preparing African American dialysis patients and families for end-of-life. Res Nurs Health 2009;32:260–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Song MK, Donovan HD, Piraino B, et al. Effects of an intervention to improve communication about end-of-life care among African Americans with chronic kidney disease. Appl Nurs Res 2010;23:65–72 [DOI] [PubMed] [Google Scholar]
- 17.Donovan HS, Ward S. A representational approach to patient education. J Nurs Scholarsh 2001;33:211–216 [DOI] [PubMed] [Google Scholar]
- 18.Donovan HS, Ward SE, Song MK, et al. : An update on the representational approach to patient education. J Nurs Scholarsh 2007;39:259–265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Song MK, Ward SE: Making visible a theory-guided advance care planning intervention. J Nurs Scholarsh 2015;47:389–396 [DOI] [PubMed] [Google Scholar]
- 20.Song MK, Ward SE, Fine JP, et al. : Advance care planning and end-of-life decision-making in dialysis: A randomized controlled trial targeting patients and their surrogates. Am J Kidney Dis 2015;65 813–822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Charlson M, Szatrowski TP, Peterson J, Gold J: Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245–1251 [DOI] [PubMed] [Google Scholar]
- 22.Fried L, Bernardini J, Piraino B: Charlson comorbidity index as a predictor of outcomes in incident peritoneal dialysis patients. Am J Kidney Dis 2001;37:337–342 [DOI] [PubMed] [Google Scholar]
- 23.Pfeiffer E: A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975;23:433–441 [DOI] [PubMed] [Google Scholar]
- 24.Centers for Medicare and Medicaid Services: Medicare and Medicaid Programs; Conditions for Coverage for End-Stage Renal Disease Facilities; Final Rule. In: Services DoHaH, ed; April 15, 2008 [PubMed]
- 25.Song MK, Kirchhoff KT, Douglas J, Ward S, et al. : A randomized, controlled trial to improve advance care planning among patients undergoing cardiac surgery. Med Care 2005;43:1049–1053 [DOI] [PubMed] [Google Scholar]
- 26.Song MK, Ward SE, Lin FC: End-of-life decision-making confidence in surrogates of African-American dialysis patients is overly optimistic. J Palliat Med 2012;15:412–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zigmond AS, Snaith RP: The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–370 [DOI] [PubMed] [Google Scholar]
- 28.Eid J, Thayer JF, Johnsen BH: Measuring post-traumatic stress: a psychometric evaluation of symptom—and coping questionnaires based on a Norwegian sample. Scand J Psychol 1999;40:101–108 [DOI] [PubMed] [Google Scholar]
- 29.Peterman AH, Fitchett G, Brady MJ, Hernandez L, et al. : Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy—Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med 2002;24:49–58 [DOI] [PubMed] [Google Scholar]
- 30.Bredle JM, Salsman JM, Debb SM, Arnold BJ, et al. : Spiritual well-being as a component of health-related quality of life: The Funactional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp). Religions 2011;2:77–94 [Google Scholar]
- 31.Yan J, Fine J: Estimating equations for association structures. Stat Med 2004;23:859–874 [DOI] [PubMed] [Google Scholar]
- 32.Thompson-Brenner H, Franko DL, Thompson DR, et al. : Race/ethnicity, education, and treatment parameters as moderators and predictors of outcome in binge eating disorder. J Consult Clin Psychol 2013;81:710–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baker M: Cultural differences in the use of advance directives: A review of the literature. Afr Am Res Perspect 2000;8:1–15 [Google Scholar]
- 34.Song MK, Ward SE: Assessment effects in educational and psychosocial intervention trials: An important but often-overlooked problem. Res Nurs Health 2015;38:241–247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McCambridge J, Butor-Bhavsar K, Witton J, Elbourne D: Can research assessments themselves cause bias in behaviour change trials? A systematic review of evidence from solomon 4-group studies. PLoS ONE 2011;6:e25223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McCambridge J, Kypri K: Can simply answering research questions change behaviour? Systematic review and meta analyses of brief alcohol intervention trials. PLoS ONE 2011;6:e23748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kagawa-Singer M, Blackhall LJ: Negotiating cross-cultural issues at the end of life: “You got to go where he lives.” JAMA 2001;286:2993–3001 [DOI] [PubMed] [Google Scholar]
- 38.Koffman J, Higginson IJ: Accounts of carers' satisfaction with health care at the end of life: A comparison of first generation black Caribbeans and white patients with advanced disease. Palliat Med 2001;15:337–345 [DOI] [PubMed] [Google Scholar]
- 39.Dawson G: African Americans and end of life care: yes to appropriate end of life supportive care, no to assisted suicide or euthanasia. J Natl Med Assoc 2002;94:40–43 [PMC free article] [PubMed] [Google Scholar]
- 40.Phipps E, True G, Harris D, et al. : Approaching the end of life: Attitudes, preferences, and behaviors of African-American and white patients and their family caregivers. J Clin Oncol 2003;21:549–554 [DOI] [PubMed] [Google Scholar]
- 41.Johnson KS, Elbert-Avila KI, Tulsky JA: The influence of spiritual beliefs and practices on the treatment preferences of African Americans: A review of the literature. J Am Geriatr Soc 2005;53:711–719 [DOI] [PubMed] [Google Scholar]
- 42.Mor V, Papandonatos G, Miller SC: End-of-life hospitalization for African American and non-Latino white nursing home residents: Variation by race and a facility's racial composition. J Palliat Med 2005;8:58–68 [DOI] [PubMed] [Google Scholar]
- 43.Torke AM, Garas NS, Sexson W, Branch WT: Medical care at the end of life: Views of African American patients in an urban hospital. J Palliat Med 2005;8:593–602 [DOI] [PubMed] [Google Scholar]
- 44.True G, Phipps EJ, Braitman LE, et al. : Treatment preferences and advance care planning at end of life: The role of ethnicity and spiritual coping in cancer patients. Ann Behav Med 2005;30:174–179 [DOI] [PubMed] [Google Scholar]
- 45.Wicher CP, Meeker MA: What influences African American end-of-life preferences? J Health Care Poor Underserved 2012;23:28–58 [DOI] [PubMed] [Google Scholar]
- 46.Branch WT, Jr, Torke A, Brown-Haithco RC: The importance of spirituality in African-Americans' end-of-life experience. J Gen Intern Med 2006;21:1203–1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gonzalez HM, Tarraf W, Whitfield KE, Vega WA: The epidemiology of major depression and ethnicity in the United States. J Psychiatr Res 2010;44:1043–1051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams DR, Yan Y, Jackson JS, Anderson NB: Racial differences in physical and mental health: Socio-economic status, stress and discrimination. J Health Psychol 1997;2:335–351 [DOI] [PubMed] [Google Scholar]
- 49.Owen JE, Goode KT, Haley WE: End of life care and reactions to death in African-American and white family caregivers of relatives with Alzheimer's disease. Omega (Westport) 2001;43:349–61 [DOI] [PubMed] [Google Scholar]