Abstract
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory lung disease characterized by progressive and only partially reversible symptoms. Worldwide, the incidence of COPD presents a disturbing continuous increase. Anxiety and depression are remarkably common in COPD patients, but the evidence about optimal approaches for managing psychological comorbidities in COPD remains unclear and largely speculative. Pharmacological treatment based on selective serotonin reuptake inhibitors has almost replaced tricyclic antidepressants. The main psychological intervention is cognitive behavioral therapy. Of particular interest are pulmonary rehabilitation programs, which can reduce anxiety and depressive symptoms in these patients. Although the literature on treating anxiety and depression in patients with COPD is limited, we believe that it points to the implementation of personalized strategies to address their psychopathological comorbidities.
Keywords: COPD, anxiety, depression, pharmacological treatment, psychotherapy
Video abstract
Introduction
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines chronic obstructive pulmonary disease (COPD) as a disease state characterized by exposure to noxious agents resulting in airflow limitation that is not fully reversible, causing shortness of breath and significant systemic effects.1 This definition covers a spectrum of respiratory diseases, and includes both the clinical diagnosis of chronic bronchitis and the pathological diagnosis of emphysema.2 In clinical practice, COPD is defined by characteristically diminished air flow in lung function tests. Spirometry is required to make the diagnosis and staging in this clinical context;3 the presence of a postbroncho-dilator forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) <0.70 confirms the presence of persistent airflow limitation and thus of COPD. Unlike asthma, the limitation is practically irreversible and usually worsens gradually over time.4 This worsening is causally related to an abnormal inflammatory response of the lungs to inhaled harmful particles or gases, attributed – usually – to smoking.5
COPD is a leading cause of morbidity and mortality worldwide and results in an economic and social burden that is both substantial and increasing.6 COPD prevalence, morbidity, and mortality vary across countries and across different groups within countries. The Global Burden of Disease Study estimated that COPD will become the fourth leading cause of death and the seventh leading cause of disability-adjusted life year(s) lost worldwide by 2030.7 The death rate associated with COPD has doubled in the past 30 years,8 implying that the health-care system failed to address the problem.9
Comorbidity studies10–12 from Western and developing countries, inpatient and outpatient population, and younger and elderly patients reveal a substantial over-representation of anxiety and depression in COPD, from significant symptoms to full diagnostic mental disorders,13 according to Diagnostic and Statistical Manual of Mental Disorders-4th edition (DSM-IV) and International Classification of Diseases, 10th Revision (ICD-10) taxonomic systems. Prevalence rates of both anxiety and depression in patients with COPD vary widely depending on the population surveyed and the measurement tools. Also, the overlap between symptoms of COPD disease and symptoms of anxiety and depression may contribute to the variations in prevalence figures, especially because questionnaires designed to screen for anxiety and depression include a large number of somatic complaints (poor sleeping pattern, anorexia, breathlessness, and fatigue).14
Anxiety in COPD patients is often associated with clinical depression, and studies indicate that depressed COPD patients have a seven-fold risk to suffer from comorbid clinical anxiety compared to nondepressed COPD patients.11,15 There is an overlap in existing symptomatology between the two disorders, with fatigue, weight changes, sleep disturbance, agitation, irritability, and difficulty in concentrating appearing as common symptoms.16
In outpatients with COPD, studies indicate rates of depression varying from 7% to 80% and that of anxiety from 2% to 80%.14–26 Prevalence of generalized anxiety disorder (GAD) ranges from 10% to 33%27,28 and of panic attacks or panic disorder (PD) from 8% to 67%.28 In stable COPD, the prevalence of clinical depression ranges from 10% to 42% and that of anxiety between 10% and 19%.29 In a systematic review30 that focused on patients with severe COPD disease, the prevalence of depression ranged from 37% to 71% and that of anxiety from 50% to 75%, figures comparable to or higher than prevalence rates in other advanced diseases such as cancer, HIV, heart disease, and renal disease.
Comorbid psychological impairments in COPD patients predict increased functional impairment,15,31 disability17 and morbidity,32,33 lower quality of life,34,35 and decreased adherence to the treatment.36,37 A systematic review and a meta-analysis have shown that depression and anxiety increase the risk of hospitalization for COPD patients.9,38 Also, patients with comorbidity spend twice as long time in hospitals and have increased mortality rates.39–42
Accordingly, recent consensus statements and guidelines on optimal care for COPD patients emphasize the need for assessment and adequate treatment of persisting anxiety and depressive symptoms in these patients. Despite the high prevalence and considerable negative impact of coexisting psychopathology in COPD, the evidence about optimal approaches for managing depression and anxiety remains unclear and largely speculative.
The objectives of this paper are to provide an overview of the prevalence, impact, and pathophysiology associated with anxiety and depression in patients with COPD and to review studies on pharmacological and nonpharmacological interventions, in an effort to highlight current knowledge and identify needs for future research.
Anxiety in patients with COPD
Anxiety disorder is a generalized term for a variety of abnormal and pathological fear and anxiety states, including GAD, PD, agoraphobia, obsessive–compulsive disorder, phobic disorders, and traumatic stress disorders. Anxiety disorders are defined using established diagnostic criteria, eg, current versions of DSM43 or ICD44 criteria, while anxiety symptoms are assessed using formal psychological instruments, eg, Hamilton Anxiety Rating Scale,45 Beck Anxiety Inventory,46 and State–Trait Anxiety Inventory.47 GAD and PD occur at a higher rate in patients with COPD compared with the general population.48 Symptoms of anxiety are manifested in a variety of ways, including physiological signs of arousal, such as tachycardia, sweating, and dyspnea. Anxiety in patients with COPD is intimately linked with the fear of acute dyspnea attacks and essentially with the sense of suffocation and the fear of death.49–51
The prevalence of anxiety-related disorders in COPD is associated with reduced functional ability and rehospitalizations.52 Common mechanisms for explaining this high association include factors related to smoking and dyspnea. Smoking is widely acknowledged as the most important environmental risk factor for the development of COPD,53 and high levels of anxiety have been identified as a risk factor for the initiation of smoking.54,55 Thus people who develop COPD as a consequence of smoking probably experienced higher levels of anxiety than the general population prior to developing the disease, and moreover, these individuals may have a greater tendency to addiction since nicotine withdrawal is associated with greater symptoms of anxiety.56–58
Evidence also suggests pathophysiologic relationships among dyspnea, hyperventilation, and anxiety.49 Physiological research has demonstrated both that respiratory rate is increased by anxiety and that the resulting rapid, shallow breathing pattern markedly worsens dyspnea in COPD.59,60 The key common physiological factors in COPD are increased ventilatory load, reduced ventilatory capacity, and increased neural respiratory drive, hyperinflation, and neuromechanical dissociation, leading to an efferent–afferent mismatch, which is fundamental to the origin of dyspnea.61 When the sense of heightened effort increases beyond a certain threshold and/or the dissociation between neural drive and the mechanical response reaches a critical level (which likely varies between individuals), it will generate a strong emotional reaction (ie, fear, distress, and anxiety) in the individual, which in turn will precipitate conditioned behavioral (avoidance) responses.62,63 These strategies help to attenuate neuromechanical dissociation and to allay anxiety. In some patients these compensations are not possible, and the affective response can quickly escalate to overt panic and overwhelming feelings of lack of control.64 Extreme fear and foreboding will, in turn, trigger patterned ventilatory and circulatory responses (via sympathetic nervous system activation) that can further amplify respiratory discomfort. The vicious cycle of breathlessness and anxiety conceptualized as “dyspnea–anxiety–dyspnea cycle” relationship suggests patients’ emotional response to breathlessness exacerbates their perception of breathlessness.65 This cycle can be illustrated by the cognitive behavioral model of dyspnea, hyperventilation, and anxiety.49 This positive feedback cycle states that individuals may misinterpret physical sensations such as dyspnea, leading to anxiety, further autonomic arousal, and increased dyspnea.66,67
Other theories proposed to explain the overlap of anxiety and panic attack symptoms with COPD are the hyperventilation model and the carbon dioxide hypersensitivity model. Hyperventilation in excess of metabolic need leads to a decrease in pCO2, causing a respiratory alkalosis that leads to vasoconstriction and typical panic symptoms such as light-headedness, numbness, tingling sensations, and shortness of breath, in healthy individuals.60 In COPD patients, increased frequency of breathing predisposes to dynamic hyperinflation, due to the slow time constant for lung deflation. Hyperinflation increases the elastic load, work, and effort of breathing, reduces inspiratory reserve capacities, and exacerbates dyspnea.68 In patients with severe COPD, chronic hypoventilation induces hypercapnia.60 An increase in pCO2 levels has been shown to activate medullary chemoreceptors, which elicits a panic response by activating noradrenergic neurons in the locus ceruleus.95 Lactate acid, formed because of hypoxia is also linked to panic attacks, and evidence suggests that patients with both COPD and anxiety are hypersensitive to lactic acid and hyperventilation.49 In other words, the pathogenesis of panic may be related to respiratory physiology by several mechanisms: the anxiogenic effects of hyperventilation, the catastrophic misinterpretation of respiratory symptoms, and/or a neurobiologic sensitivity to CO2, lactate, or other signals of suffocation. Consequently, there is a reason to believe that chronic pulmonary disease constitutes a risk factor for the development of panic anxiety related to repeated experiences with dyspnea and life threatening exacerbations of pulmonary dysfunction, repeated episodes of hypercapnia or hyperventilation, the use of anxiogenic medications, and the stress of coping with chronic disease.69
Anxiety symptoms may distract patients from self-management of disease exacerbations.70 Even a low intensity dyspnea attack is able to trigger panic anxiety which in turn heightens the sensation of dyspnea and sense of suffocation, thus creating a vicious cycle that forces many patients to restrict their daily activities.70–72 Patients with COPD usually describe their understanding of acute dyspnea as an experience inextricably related to anxiety and emotional functioning. As a result, this comorbidity leads to significant decrease in functional capacity, including phobic avoidance of activity because of anticipatory anxiety, further deconditioning, and misuse of anxiogenic medications73 (β2 agonists, theophylline, and oral corticosteroids).
Recognition of the presence of this pathophysiological mechanism provides a more comprehensive assessment of the additional functional impairment experienced by the patient even if biological parameters and laboratory results are insufficient to justify the compromised ability to perform physical functions.15,21,52 Sense of loss of control over the disease itself and loss of mastery74,75 over their ability to engage in personal and social activities engenders frustration and anxious feelings.
It is important to note that dyspnea at rest or on exertion does not correlate with the magnitude of anxiety-related symptoms, and furthermore, the magnitude of decrease in dyspnea with pharmacotherapy or exercise training is not associated with the reduction in anxiety-related symptoms, this indicates that there are other factors contributing to this relationship.76 Additionally, although patients with panic report more catastrophic misinterpretations of bodily symptoms, they do not differ from patients without panic on measures of physical functioning, disease severity, shortness of breath, or psychological distress. Thus, it has been suggested that panic symptoms may reflect a cognitive interpretation of pulmonary symptoms rather than objective pulmonary status.66
Studies indicate that anxiety and depression were not correlated with COPD severity77 (as determined by FEV1% of predicted), and it is reported that dyspnea ratings were influenced by anxiety and depressive symptoms, whereas the physiological state scarcely influenced the anxiety and depressive symptomatology.78 A possible explanation is that patients construe disease seriousness subjectively, which contributes to the development of the levels of anxiety and depressive symptoms.14
Depression in patients with COPD
Today, the ICD-1044 and DSM-V79 criteria for depression are the most common diagnostic tools. Different subtypes of depression have been defined, and the clinical course of depression is acknowledged to be variable with patients moving in and out the diagnostic subtypes over time. When it comes to depression in patients with severe somatic illness, the validity of DSM criteria may to a certain degree be questioned because it is difficult to decide when somatic symptoms are secondary to depression, or when they are secondary to somatic illness.80 Severity of depression is determined by the number and level of symptoms, as well as the degree of functional impairment. Patients with COPD may have a spectrum of symptom severity ranging from short-term depressive symptoms or adjustment disorder with depressed mood to dysthymia up to major depression.
In a cluster of studies that have compared depressive disorders across various chronic illnesses, COPD patients suffer from depression with greater frequency and greater chronicity of mood symptoms.81–84 Also, few studies10,52 have reported that approximately two-thirds of COPD patients with depression have moderate-to-severe depression, and in one study,85 it was reported that approximately one-fourth of COPD patients had unrecognized subclinical depression.
Depression in patients with COPD is often marked by feelings of hopelessness and pessimism, reduced sleep, decreased appetite, increased lethargy, difficulties in concentration, social withdrawal, impairment in functional abilities and performing activities of daily living, poorer self-reported health, impaired self-management of disease exacerbations, and poor health behaviors.52,70,86–91 The correlation between depressed mood and disease severity is modest;21 but depression symptoms are important correlates of perceived self-reported physical disability and poorer quality of life.85 Guilty feelings stemming from the sense of burden patients impose to their environment, in combination with the responsibility they might think they have for the occurrence of the disease, especially concerning ex-smokers, aggravates depressive symptomatology.92
According to studies, clinically significant levels of depression and anxiety were more prevalent in younger COPD patients, irrespective of clinical severity of COPD, perhaps because younger patients may find it difficult to come to terms with enforced changes in lifestyle, with this leading to increased psychological morbidity.93
Recent studies suggest that depression in patients with COPD is a heterogeneous entity with multiple contributing etiologies including genetic predisposition, environmental losses and stressors, and direct damage to the brain mediated by the physiologic effects of chronic respiratory disease.94
The genetic vulnerability plays a role in the eventual development of COPD in that adolescents and young adults who are depressed or have a history of depression are more likely to progress in their use of and dependence on nicotine.54,55,96 Smoking, COPD, and depression form a dynamic model of circular causality, with depression playing a role in the initiation and maintenance of smoking, smoking leading to the development of COPD, and COPD in turn contributing to the genesis of depression.94
Evidence suggests that the appearance of major depression or depressive symptomatology in patients suffering from a chronic disabling general medical condition is common and justified as a “reaction” to the losses imposed by the illness in both symbolic order and real grounds.97 These losses may include functional impacts98 such as inability to carry out prior occupational activities, shifted roles within the family, and social constellation, but also an insult to self-image that patients experience with the change in their general physical condition and somatic functioning.94 Losses for patients with COPD increase with the gradual deterioration of the disease. Dyspnea65,99 is the most common and disabling symptom experienced by COPD patients and is inextricably associated with feelings of despair, helplessness, and alienation, resulting in the apparent loss of interest for life and other people.
By the very nature of the disease process, COPD is associated with chronic, if often subclinical, hypoxemia. Low arterial oxygen saturation has been shown to be associated with periventricular white matter lesions,100 which are also present in elderly patients with depression.101 Several authors have investigated the relationship between chronic hypoxemia and neuropsychological function, and the consequences of chronic hypoxemia include both impaired cognitive function and depression.102,103 Most studies of hypoxemia and depression arise from the sleep apnea literature where one of the primary identified sequelae of recurrent nocturnal hypoxemia is depressed mood.104
Both depression and COPD have been associated with processes that jeopardize the microvasculature of the brain,105,106 and there is evidence for systemic inflammation and elevated biomarkers of oxidative damage.107 Although there are difficulties in quantification of inflammatory biomarkers, sTNFR-1 has shown a strong association with rates of depression in COPD patients.108 In the absence of prior comorbidity, systemic inflammation in COPD may result in depression and IL-6 appears to play a particularly important role in humans and in animal models of depression.109 A prospective cohort study indicated that the mean time elapsed between the diagnosis of COPD and the first episode of depression was 7.6 years.110 The long-term use of systemic corticosteroids has also been related to depression in COPD, but results are inconclusive.111
Although smoking, hypoxia, and inflammation have potential impact on the prevalence of depression in COPD, the strongest predictors of depression among patients with COPD are their severity of symptoms and reported quality of life.33 The advantage to recognizing the interdependent relationship of these contributing factors is the corollary recognition that effective intervention in any one of them will have a cascading, positive impact on the others. Effectively targeting depression, lost functionality, or chronic hypoxemia will decrease morbidity in that dimension, and potentially in the others as well.
Treatment
Despite high prevalence rates and deleterious impact of comorbid anxiety and depression in COPD, only a limited number of studies have addressed its management,26 accounting for the absence of recommendations regarding their treatment in the updated GOLD guidelines.1 Only pulmonary rehabilitation (PR) is suggested as treatment option (evidence A), which is also available for only a small percentage of patients.112 The National Institute for Health and Care Excellence (NICE) has published clinical guidelines for the use of stepped approaches to psychological and/or pharmacological treatment of depression in people with long-term conditions.113 In recognition of the expanding knowledge and the clinical importance of this area, we attempted to summarize existing empirical evidence based on studies implementing pharmacological and nonpharmacological interventions to reduce clinical anxiety and depression in people with COPD.
Method
A literature search was conducted for studies examining the effect of anxiolytic and antidepressant medical treatment, cognitive behavioral therapy (CBT), PR, and other complex interventions on anxiety and depressive symptoms in COPD patients, using PubMed databases. Essential keywords were “chronic obstructive pulmonary disease” OR “COPD” AND “anxiety” OR “depression” to capture the target population. Intervention search terms comprised “medication” OR “pharmacological treatment” OR “SSRIs” OR “antidepressants” OR “TCAs” OR “SNRIs” OR “mirtazapine” OR “buspirone” OR “benzodiazepines” OR “psychological interventions” OR “cognitive behavioural therapy” OR “psychotherapy” OR “pulmonary rehabilitation” OR “group therapy” OR “complex interventions” OR “relaxation” OR “health education” OR “counselling” OR “behavioural interventions” OR “alternative treatments” OR “Tai Chi” OR “yoga”.
Eligibility criteria
Studies for inclusion were required to be in the English language and meet participant, intervention, comparator, and outcome criteria,114,115 for studies of controlled comparative design. We also included nonrandomized studies such as clinical trials, crossover studies, observational studies, and relevant review articles and meta-analyses. Participants were adults (men and women of age ≥18 years), with a confirmed diagnosis of COPD as defined by the GOLD standard, who were treated for symptoms of anxiety and depression. Mode of interventions was pharmacological and nonpharmacological, and was aimed at reducing symptoms of anxiety and depression. The primary outcomes of interest were reduction in these symptoms following the administration of these interventions. The outcome was measured by changes from baseline anxiety and depression scores to posttreatment scores, employing validated psychological assessment instruments.
Quality assessment
The quality of included controlled comparative design studies was assessed by two authors independently with respect to the Critical Appraisal Skills Program checklists for risk of bias evaluation.116 The methodological quality of full-text articles was assessed employing checklists from the Scottish Intercollegiate Guidelines Network.300
Results
Electronic database searches yielded 637 records with 438 remaining after removal of duplicates. From the initial title screenings, 253 potentially relevant articles were identified and their abstracts were subsequently reviewed. Of these, 167 were excluded as they failed to meet inclusion criteria. Seventy-two studies and 14 reviews were retrieved in full text for further assessment.
Overview and effects of pharmacological and nonpharmacological interventions on anxiety and depression in COPD
Tables 1–4 outline the characteristics of pharmacological and nonpharmacological interventions reported in the included studies. The results column describes the effects of interventions in narratives, thus enabling comparisons across various studies.
Table 1.
Pharmacological treatment for anxiety and depression in COPD patients
| Source | Study design | Sample size (n) | Comparison | Measurement instruments | Results |
|---|---|---|---|---|---|
| Momtaz et al249 | Placebo-controlled | n=50 stage III and IV COPD patients with depression and/or anxiety I=25, C=25 |
Fluoxetine 20 mg for 3 months vs placebo | MADRS, HAM-A | Significant improvement in both anxiety and depression in MADRS and HAM-A scores after 3 months of treatment |
| He et al250 | RCT | n=120 patients with stable COPD with moderate or severe depression I=60, C=60 |
Sertraline hydrochloride 50 mg/d for 6 weeks vs placebo | HAMD-17, 6MWD, CAT | Patients in the sertraline hydrochloride group showed more changes in the HAMD-17 scores and CAT scores after treatment and 6MWD than in the placebo group |
| Eiser et al144 | RCT | n=28 stable outpatients with COPD stage II and III and depression (ICD-10) I=16, C=12 |
Paroxetine 20 mg vs placebo for 6 weeks, unblinded paroxetine for 3 months | HADS, BDI, MADRS, SGRQ, 6MWD | Treatment produced no significant differences, although overall improvements in depression correlated with 6MWD. Five patients developed side effects. 3 months of unblinded treatment, significantly improved depression (HADS, BDI, MADRS), and 6MWD, SGRQ scores |
| Lacasse et al147 | RCT | n=23 outpatients with COPD (average stage III), and significant depressive symptoms. 15 completed (I=8, C=7) | Paroxetine 20 mg vs placebo, for 12 weeks | GDS, SF-36, CRQ | Clinical and statistical improvement in emotional and mastery domains of CRQ. Nonsignificant improvement in GDS |
| Subbe et al156 | RCT | n=8 COPD patients, 4 with baseline anxiety | Citalopram 10–20 mg vs placebo, for 3 months and 1 week | HADS, SGRQ | Anxiety scores were not significantly reduced for the intervention as compared with placebo; however, power was very limited. SGRQ scores demonstrated a clinically relevant, but inconclusive effect, favoring placebo |
| Yohannes et al143 | Single-blinded, open study | n=57 COPD patients stage II and III and depression. I=14 agreed to fluoxetine, C=22 of those who refused treatment | Fluoxetine for 6 months, 20 mg/d | GMS and MADRS, MRADL, BPQ | 7 completed trial, 4 responded to fluoxetine treatment. 5 withdrew because of adverse side effects. 19 of those who refused treatment were still depressed |
| Smoller et al146 | Case series | n=COPD patients (severity not reported) | Sertraline (25–100 mg/d) for 4 weeks to 1 year | Not formally assessed | Clinician-reported improvement |
| Evans et al148 | RCT | n=42 physically ill elderly depressed patients completed trial, 38 with respiratory diseases I=21, C=21 | Fluoxetine vs placebo for 8 weeks, 20 mg/d | HAMD-17, ELDRS, GMS | No significant difference between groups in response rate. Trend for fluoxetine group to respond better than controls after 8 weeks (subjective report). Significantly more recovery from depression after 5 or more weeks on fluoxetine |
| Papp et al145 | Case series | n=6 consecutive COPD (severity not reported) outpatients | Sertraline titrated to 100 mg, for 6 weeks | Not formally assessed | Clinician-reported improvement |
| Singh et al154 | Crossover study | n=11 stable COPD patients, at least stage II and STAI >50 10 completed trial |
Buspirone, 30–60 mg vs placebo, for 6 weeks | STAI, 12MWD | No significant differences in either exercise or anxiety scores |
| Argyropoulou et al153 | Double-blind crossover randomized trial | n=16 COPD patients, FEV1/FVC 50.7%±15.0% | Buspirone 20 mg for 14 days | SCL-90-R, 6MWD and WRmax | Reduced anxiety and depression Increased 6MWD and WRmax |
| Ström et al139 | RCT | n=26 stable COPD patients, at least stage II. Five completed trial I=14, C=12 | Protriptyline vs placebo for 12 weeks, 10 mg/d | HADS, MACL, SIP | No improvement in depression, anxiety, or QoL scores. High rates of anticholinergic side effects |
| Borson et al137 | RCT | n=36 in patients with COPD stage II and III and comorbid depressive disorder. N=30, I=13, C=17 completed trial | Nortriptyline vs placebo for 12 weeks increased weekly until 1 mg/kg of body weight | CGI, HADS, PRAS, 12MWD, PFSI, SIP | Improvements for nortriptyline group in depression, anxiety, respiratory symptoms, physical comfort, and day-to-day functioning. No change in physiological measures |
| Sharma et al141 | Double-blind method | n=10 consecutive COPD patients (all stages) | Imipramine-diazepam combination | Not formally assessed | Helped depressed patients recover faster, but diazepam may trigger respiratory failure |
| Light et al138 | RCT | n=12 outpatients with COPD stage III and high levels of depression. n=9 completed trial | Doxepin hydrochloride vs placebo for 6 weeks | BDI, 12MWD, STAI | No significant improvements in exercise capacity or depression and anxiety scores. Increase in 12MWD correlated with improvements in depression or anxiety |
| Gordon et al140 | RCT | n=13, stable COPD outpatients stage III. n=6 completed trial | Desipramine vs placebo for 8 weeks | BDI and Zung Self-rating Depression Scale | Depression scores improved significantly after treatment with placebo and with desipramine. No effect on physiological measures |
Abbreviations: BAI, Beck anxiety inventory; BDI, Beck depression inventory; BDI-II, Beck depression inventory 1996 revision; HADS, Hospital Anxiety and Depression Scale; HAM-A, Hamilton Anxiety Rating Scale; HAMD-17, 17-item Hamilton Depression Rating Scale; MADRS, Montgomery and Asberg Depression Rating Scale; STAI, Spielberger’s state–trait anxiety inventory; GDS, Geriatric Depression Scale; GMS, geriatric mental state; CGI, Clinical Global Improvement Scale; ELDRS, Evans Liverpool Depression Rating Scale; MACL, mood adjective checklist; BPQ, Breathing Problems Questionnaire; CRQ, Chronic Respiratory Questionnaire (COPD disease-specific QoL inventory); CAT, COPD assessment test; 6MWD, 6-minute walk distance; 12MWD, 12-minute walk distance; WRmax, maximum work-rate; PFSI, Pulmonary Functional Status Instrument; PRAS, Patient-rated Anxiety Scale; MRADL, Manchester Respiratory Activities of Daily Living Questionnaire; QoL, quality of life; SGRQ, St Georges Respiratory Questionnaire; SF-36, 36-item Short Form Health Survey; SIP, sickness impact profile; RCT, randomized controlled trial; I, intervention group; C, control group; COPD, chronic obstructive pulmonary disease; ICD-10, International Classification of Diseases, 10th Revision; SCL-90-R, Hopkins Symptoms Checklist Revised; WE, wellness education; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity.
Table 2.
Cognitive behavioral therapy in COPD patients
| Source | Study design | Sample size (n) | Comparison | Measurement instruments | Results |
|---|---|---|---|---|---|
| Bove et al251 | RCT | I=33, C=33 Stage III–IV COPD outpatients with anxiety HADS-A >8 | Minimal home-based CBT psychoeducative session in combination with a telephone booster session vs usual care | HADS-A, SGRQ, CRQ-M | Ongoing – currently recruiting participants |
| Howard and Dupont252 | RCT | I=112, C=110 COPD outpatients FEV1/FVC) <0.7, MRC ≥3 with baseline anxiety and depression | Cognitive behavioral manual vs information booklets, at home over 5 weeks | HADS, CRQ-SR | At 6 months, there were significantly greater improvements in anxiety, depression, and dyspnea in the CBT intervention group |
| Jiang and He253 | RCT | I=49, C=47 Stage II–III COPD outpatients | Uncertainty management vs standard care: 4 sessions of 35 minutes, once per week over 4 weeks | SSAI, STAI, HADS-D | Compared to the control group, the intervention group showed significant improvement in anxiety, depression scores, and QoL |
| Kapella et al254 | RCT | N=23, I=9, C=9 Stage II COPD outpatients | 6 sessions of CBT-I vs WE program | POMS-D, POMS-A | Significant positive treatment-related effects of the CBT-I intervention were noted for insomnia severity, global sleep quality, wake after sleep onset, sleep efficiency, fatigue, and beliefs and attitudes about sleep. Significant positive effects were noted for depressed mood after WE program |
| Hynninen et al169 | RCT | I=25, C=26 stage II–III COPD outpatients with clinically significant anxiety and depression | CBT vs enhanced standard care: 7 sessions of 2 hours of group CBT over 7 weeks | BAI, BDI-II | CBT resulted in improvement in symptoms of anxiety and depression. The improvement was maintained at 8-month follow-up. In the control group, there was no significant change |
| Livermore et al255 | RCT | I=21, C=20 stage II–III COPD outpatients attending PR program | CBT vs routine care: 4 individualized 1-hour sessions and strategies effective for the prevention and treatment of panic disorder | HADS | Significant differences post intervention at 6-, 12-, and 18-month follow-ups, favoring the CBT group. At each follow-up, mean anxiety scores for the CBT group were in the nonclinical range, while mean scores for the routine care group were above the cutoff score |
| Lamers et al256 | RCT | I=96, C=91 COPD outpatients with mild-to-moderate major depression | Minimal psychological intervention (4 individualized 2 hours CBT and skills training) vs usual care | SCL-A, BDI | Intervention group showed lower symptoms of anxiety and depression and improved QoL measures compared to control group |
| Kunik et al257 | RCT | I=118, C=120 stage II–III COPD stable outpatients with baseline anxiety and depression | CBT vs COPD education: Intervention: 8×1 hour CBT group sessions, control: 8×1 hour COPD education sessions | BAI, BDI-II | CBT or COPD education, significantly improved QoL, anxiety, and depression over 8 weeks; the rate of change did not differ between groups. Improvements were maintained with no significant change during follow-up |
| Blumenthal et al258 | RCT | I=158, C=170 patients with end-stage lung disease awaiting lung transplantation | 12 weeks of 30-minute telephone-based CST vs UMC | BDI, STAI | Compared with UMC, CST produced lower scores on perceived stress, anxiety, depressive symptoms, and negative affect and improved scores on mental health functioning, optimism, vitality, and perceived social support |
| de Godoy et al259 | RCT | n=49 (G1=19, G2=16, G3=14) consecutive patients with COPD stage II and III. Mild-to- moderate levels of anxiety and depression | 12-week treatment. G1: PRP (physical exercise, individual psychotherapy sessions, group educational sessions, physical therapy); vs G2:PRP without physical exercise; vs G3: PRP without psychotherapy | BAI, BDI, SGRQ | G1 and G2 patients improved in anxiety and depression as well as SGRQ and exercise tolerance. G3 improved in anxiety |
| de Godoy and de Godoy260 | RCT | n=30 patients stage I–III COPD, attending PR program I=14, C=16 with baseline anxiety and depression | PR (12-week treatment program) with psychotherapy vs PR without psychotherapy | BAI, BDI | Including psychotherapy significantly reduced patients’ anxiety and depression levels but did not modify 6MWD performance |
| Kunik et al170 | RCT | I=21, C=27 from veteran hospital stage II–III stable COPD outpatients | CBT vs COPD education: 1×2-hour session of group CBT vs education session lasting 2 hours | BAI, GDS | Statistical improvement in BAI and GDS |
| Emery et al261 | RCT | N=79 (EXESM =29; ESM =25; WL =25) COPD outpatients stage III | EXESM: 37 exercise sessions, 16 education sessions, 10×1-hour stress management sessions based on CBT vs ESM: 16 education sessions, 10×1-hour stress management sessions based on CBT and WL for 10-week period | CES-D, Bradburn Affect Balance Scale; STAI, SCL- 90-R, MHLC, SIP, cognitive assessments | EXESM and WL groups showed reductions in depressive symptoms and SIP scores. EXESM showed improvements in anxiety and organized verbal processing. All groups increased mental efficiency performance |
| Eiser et al262 | Pilot study | I=10, C=8 with moderately severe, stable COPD, intervention group had significantly higher prevalence of anxiety than control group at baseline | Intervention: six 90 minutes sessions of CBT at weekly intervals vs controls: attended weekly for lung function and 6MWD for 6 weeks, but had no psychotherapy | HADS, 6MWD | Improvement in exercise tolerance in a group of ten anxious patients with severe COPD, without any change in anxiety scores |
| Coventry et al246 | Review of 7 RCT studies | N=916 patients, most had moderate-to-severe COPD, with variable psychological morbidity | CBT intervention: 30–120 minutes ×4–12 sessions group or individual face-to-face or remote | BDI, GDS, POMS-A, POMS-D, BAI, SCL-90 | The meta-analysis revealed a small beneficial effect of CBT on both anxiety and depression, neither of which was statistically significant |
| Ramsenthaler et al263 | Review of 13 RCT studies | COPD patients of all stages with mild-to-severe panic or anxiety symptoms | CBT intervention for the treatment of mild-to-severe anxiety and panic in adult patients with mild-to-severe COPD | Validated instruments of anxiety | 7 of 13 studies reported a significant impact of CBT on anxiety. Six other studies, one of which was an adequately powered RCT, failed to show an improvement in anxiety symptoms. The meta-analyses showed a small effect of CBT on anxiety |
| Baraniak and Sheffield264 | Review of 9 studies, 4 RCT | N=523 patients, most had moderate-to-severe COPD, with variable psychological morbidity | Individual or group CBT, CBT-based education, individual psychotherapy and muscle relaxation training, over a single 2-hour intervention to 12 weekly sessions vs control groups with education only, PR and exercise, weekly lab tests | Generic and disease-specific QoL and various psychological instruments | Improvement in anxiety scores was reported in 4 out of 9 studies. Four out of 7 studies reported a statistically significant improvement in depression scores. 5 studies considered QoL; findings were mixed and unclear |
| Coventry and Gellatly172 | Review of RCTs and nonrandomized trials | 3 RCTs (165 patients) and one nonrandomized controlled trial (n=8 patients), with stable and severe COPD and mild-to-moderate anxiety and depression | CBT alone or alongside exercise and/or education; comparators included WL control, standard care, exercise, education, and/or CBT | CES-D, BAI, BDI, HADS, STAI, and several measures of exercise, education, and stress management at 6, 10, and 12 weeks | There was limited evidence that CBT, when used with exercise and education, could contribute to significant reductions in anxiety and depression in patients with clinically stable and severe chronic obstructive pulmonary disease. Only one RCT (30 patients) reported a large statistically significant effect size in favor of CBT; this trial used CBT alongside education and exercise |
Abbreviations: BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; BDI-II, Beck Depression Inventory 1996 revision; HADS, Hospital Anxiety and Depression Scale; HADS-D, Hospital Anxiety and Depression Scale – Depression subscale; STAI, Spielberger’s state–trait anxiety inventory; SSAI, Spielberger’s State Anxiety Inventory; CES-D, Center for Epidemiologic Studies Depression Scale; GDS, Geriatric Depression Scale; POMS-A, Profile of Mood States Anxiety Scale; POMS-D, Profile of Mood States Depression Scale; SIP, Sickness Impact Profile; ESM, education and stress management; EXESM, exercise, education and stress management; CRQ-SR, Self-Reported Chronic Respiratory Questionnaire; RCT, randomized controlled trial; WL, waiting list; I, intervention group; C, control group, CBT-I, cognitive behavioral therapy for insomnia; G1, Group 1; G2, Group 2; G3, Group 3; COPD, chronic obstructive pulmonary disease; SCL-90-R, Hopkins Symptoms Checklist Revised; MHLC, Multidimensional Health Locus of Control inventory; 6MWD, 6-minute walk distance; PRP, pulmonary rehabilitation program; SGRQ, St Georges Respiratory Questionnaire; CST, coping skills training; UMC, usual medical care; QoL, quality of life; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; MRC, Medical Research Council; HADS-A, Hospital Anxiety and Depression Scale – Anxiety subscale; CRQ-M, Chronic Respiratory Questionnaire; SCL-A, Anxiety subscale of the Symptom Checklist-90; WE, wellness education.
Table 3.
Relaxation therapy and alternative treatments
| Source | Study design | Sample size (n) | Comparison | Measurement instruments | Results |
|---|---|---|---|---|---|
| Mkacher et al265 | RCT | I=32, C=30 COPD patients entering PRP | 6 months PRP with or without balance training 3 times a week | HADS, SGRQ, 6MWT | Anxiety decreased significantly in both groups with a greater change in the intervention group. Only the intervention group had an improved depression score at the end of 6 months. Both the intervention and PR-only group improved their QoL with a significant intergroup difference |
| Reychler et al266 | RCT | N=41 COPD patients entering PRP FEV1: 38.6%±12.5% | One session of PRP with or without ambient music | HADS, Borg scales, dyspnea VAS | Perceived exertion was not modified by ambient music, but anxiety was improved |
| Kaymaz et al267 | Nonrandomized controlled observational study | I=23, C=27 Stage III COPD patients | C = PRP 3 days a week for 8 weeks vs I = NMES 2 days a week for 10 weeks | HADS, SGRQ, MRC, ISWT, ESWT, MMT | In the I group, significant improvements were observed in the HADS scores and in all SGRQ domains except symptom domain. NMES can be used as an effective treatment strategy in PR programs for peripheral muscle training in patients with severe COPD |
| Valenza et al268 | RCT | I=23, C=23, N=46 male patients hospitalized for COPD exacerbation | 10-day controlled breathing intervention vs standard care | HADS, SGRQ, MMRC, EQ-5D | Controlled breathing exercises improve anxiety and depression in patients hospitalized for COPD exacerbation |
| Leung et al269 | RCT | N=42 COPD patients FEV1: 59%±16% | TCG: short-form Sun-style t’ai chi twice weekly for 12 weeks vs CG: usual medical care | HADS, CRQ, ISWT, ESWT, MPPB, FPI | At study completion, the ESWT time was significantly longer in the TCG than the CG. the TCG had a significant improvement in ISWT, MPPB, FPI, CRQ HADS anxiety domain |
| Santana et al270 | Prospective observational study | N=25 pre–lung transplant patients, 5 with COPD | Two-phase, 12-week IYP that included 2 hours biweekly classes | HADS, CRQ, HUI, 6MST | Changes in HADS anxiety and CRQ fatigue scores were statistically significant and changes in HUI ambulation, pain, emotion, and overall score were clinically important |
| Lord et al183 | RCT | N=24 COPD patients I=13, FEV1: 44.4%±14.4% C=11, FEV1: 63.5%±25.5% | Singing classes twice weekly for 8 weeks vs a film club for 8 weeks, once weekly | HADS, SF-36, CAT | No significant differences between groups in the response of measures of breathing control, functional exercise capacity or daily physical activity. Similar improvements in the mental component score of the SF-36 in both groups. Significant difference between the response of the physical component score favoring the singing group |
| Yeh et al180 | RCT | I=5, C=5, N=10 moderate-to-severe COPD patients | 12 weeks 1-hour class, twice weekly of tai chi plus usual care vs usual care alone | CESD, CRQ, 6MW | Significant improvement in CRQ score among the tai chi participants, compared to the usual-care group. There were nonsignificant trends toward improvement in 6MW, CESD scores |
| Lord et al182 | RCT | I=15, C=13, N=28 COPD patients FEV1: 37.2%±18.6% | 6-week course of twice- weekly singing classes vs usual care | HADS, SF-36, SGRQ, ISWT | The physical component score of the SF36 improved in the singers compared to the controls. Singers also had a significant fall in HAD anxiety score |
| Donesky-Cuenco et al181 | RCT | N=29 stable COPD patients FEV1 47.7%±15.6% | Twice-weekly 12-week yoga program vs usual- care | CESD, SSAI, FPI, SF-36, CRQ, 6MW | After the program, the subjects tolerated more activity with less dyspnea-related distress and improved their functional performance. No significant intergroup difference on CESD, SSAI scores |
| Singh et al271 | RCT | N=72 COPD patients hospitalized for COPD exacerbation | Music vs PMR. Music group listened to a self-selected music of 60–80 beats per minute for 30 minutes. PMR group practiced relaxation through a prerecorded audio of instructions of 16 muscle groups | SSAI, STAI, physiologic measures | Music and PMR are effective in reducing anxiety and dyspnea along with physiologic measures in two sessions in COPD patients hospitalized with exacerbation. However, reductions in the music group were greater compared to the PMR group |
| Lolak et al179 | RCT | N=83 COPD patients entering PRP | 8-week PR program 2 days per week with or without PMR – 25 min/wk during weeks 2–8 | HADS | The results favored the PMR group but did not reach statistical significance. Adding structured PMR training to a well-established PR program may not confer additional benefit in the further reduction of anxiety and depression in patients receiving PR |
| Bauldoff et al272 | Experimental, randomized, two- group design | I=12, C=12, N=24 moderate-to-severe COPD patients following completion of a PRP | Instructed to walk at their own pace for 20–45 minutes, 2–5 times a week, using DAS vs no DAS | HADS, ADL, 6MW, QoL | Subjects who used DAS while walking had improved functional performance and decreased perceptions of dyspnea, whereas control subjects could not maintain post- PRP gains. No significant differences were noted for the remaining variables |
| Sassi-Dambron et al220 | RCT | I=47, C=51, N=98 COPD patients FEV1: 50%±21% | 6-week techniques of PMR, breathing retraining, pacing, self- talk, and panic control vs general health education | STAI, CESD, QWB, VAS, Borg scale | A treatment program of dyspnea management strategies, PRP components, is not sufficient to produce significant improvement in dyspnea, exercise tolerance, health-related quality of well- being, anxiety, or depression |
| Gift et al273 | RCT | N=26 COPD patients stage II | 4 weeks: 4 sessions, 20 minutes PMR with prerecorded tapes vs sit quietly for 20 minutes | STAI, physiologic measures | Dyspnea, anxiety, and airway obstruction were reduced in the relaxation group while the control group remained the same or became worse |
| Volpato et al176 | Meta-analysis: 25 RCTs | I=615, C=627, N=1,426 COPD patients stage I–III | 1) Relaxation techniques; 2) PMR; 3) guided imagery; 4) distraction therapy; 5) biofeedback; 6) breathing techniques; 7) yoga; 8) Tai Chi; 9) acupressure vs control group | Validated instruments of anxiety, depression, QoL, and physiologic measures | Relaxation techniques showed minor positive effect on the value of the percentage of predicted FEV1, as well as a slight effect on levels of both the anxiety and depression. The higher effect size was found in the QoL value |
Abbreviations: HADS, Hospital Anxiety and Depression Scale; MRC, Medical Research Council; ISWT, incremental shuttle walking test; ESWT, endurance shuttle walking test; SGRQ, St Georges Respiratory Questionnaire; MMT, manual muscle testing; MMRC, Modified Medical Research Council Scale; EQ-5D, European Quality of Life Questionnaire; VAS, visual analog scale; STAI, Spielberger state–trait anxiety inventory; SSAI, Spielberger’s state anxiety inventory; CESD, Center for Epidemiologic Studies’ Depression; QWB, quality of well-being scale; ADL, activities of daily living; 6MW, 6-minute walk distance; HUI, Health Utilities Index; 6MST, 6 minute walk test; SF-36, Medical Outcomes Study Short-Form 36; FPI, Functional Performance Inventory; CAT, COPD assessment test score; MPPB, modified physical performance battery test; I, intervention group; C, control group; PMR, progressive muscle relaxation; QoL, quality of life; TCG, t’ai chi group; CG, control group; DAS, distractive auditory stimuli; CRQ, Chronic Respiratory Questionnaire; IYP, Iyengar yoga program; NMES, neuromuscular electrical stimulation; 6MWT, 6-minutes walking test.
Table 4.
Comprehensive PR in COPD patients
| Source | Study design | Sample size (n) | Intervention | Measurement instruments | Results |
|---|---|---|---|---|---|
| Luk et al274 | Prospective cohort study | n=83 patients with COPD who had completed PR, FEV1 mean: 46% | Assessment after 22 months following an 8-week PRP | HADS, CRQ, ISWT | ISWT gain was lost at the long-term reassessment. In CRQ, only the domains of dyspnea and fatigue remained statistically significant, and improvements in HADS scores persisted at the long-term reassessment but were not statistically significant |
| Sciriha et al275 | Prospective observational study | n=60 COPD patients stage I–IV with MRC grade 2 or above | PRP for 12 weeks 2 hours sessions, twice-weekly | HADS, SGRQ, 6MWT, Borg scale, CAT | Anxiety scoring decreased significantly by 12 weeks, while the depression rating improved by 8 weeks. No significant changes on anxiety ratings for stage III–IV COPD participants as opposed to the milder group of patients who had significant changes after 3 weeks. Participants with an MRC 2–3 had significant changes in depression ratings after 12 weeks of PRP |
| Grosbois et al276 | Retrospective observational study | n=211 patients with COPD FEV1 mean: 41.5%±17.7% | Home-based PR individually managed once a week for 8 weeks unsupervised on the other days of the week | HADS, 6MST, VSRQ | 6MST was significantly improved after completion of the program, at 6 and 12 months. HADS and VSRQ scores improved after PR, and this improvement persisted at 6 and 12 months |
| Boutou et al196 | Prospective observational study | n=787 COPD outpatients stage I–IV from 8 PR centers | PRP over 8–12 weeks with two supervised sessions and one or more unsupervised home exercise sessions each week | HAD-A, HAD-D, CRDQ, CAT, 6MWT, ISWT | Significant improvements in 6MWT or ISWT distance. Anxiety and depression scores fell post PR. QoL also improved with significant fall in CAT scores while CRDQ scores increased. Patients who completed PR were significantly older with less severe airflow obstruction, lower anxiety and depression scores, less dyspnea and better HRQoL |
| da Costa et al277 | Prospective observational study | n=125 COPD patients FEV1 mean: 43.18%±18.79% | PRP of 3 weekly sessions of 60 minutes duration for 12 weeks, a total of 36 sessions | BAI, BDI, SGRQ | Significant decreases in anxiety and depression scores and improvements in QoL were observed. Weak correlations were observed when correlating the BAI to the SGRQ |
| Jácome and Marque224 | Quasiexperimental study | n=26 COPD patients FEV1 mean: 83.8%±6.4% | 12-week PR program 3 sessions/week, 60 minutes each, with exercise training and psychoeducation | DASS, SGRQ, 6MWT, MMRC, TUG | Significant improvements were observed on 6MWT, MMRC, TUG and SGRQ total scores. No significant improvement in the SGRQ impact score and DASS scores |
| Tselebis et al278 | Prospective observational study | n=101 stage I–IV COPD patients | PRP for a period of 3 months, with three sessions per week, each lasting 50 minutes | STAI, BDI | Significant decreases in anxiety and depression rates were observed. A statistically significant reduction in anxiety and depression was revealed at all stages of COPD |
| Bhandari et al279 | Retrospective observational study | n=366 COPD patients FEV1 mean: 47%±17% at program entry, 25% had abnormal anxiety scores and 17% had abnormal depression scores | Sixteen 3-hour sessions given twice weekly over an 8-week outpatient PR program | HADS, CRQ-SR, 6MST | Of the 366 patients, 257 completed the program and 235 completed final outcome evaluation. Among patients who completed PR, there were significant improvements on all dimensions (CRQ-SR, 6MST scores, and reduced HADS scores) |
| Hogg et al280 | Prospective observational study | n=812 stage I–IV COPD patients were assessed | 656 started PR twice or once weekly for 8 weeks | HADS, ISWT, CRQ, MRC | 441 completed. Significant improvements were seen in ISWT, CRQ-SR and HADS scores. Twice-weekly compared with once-weekly programs showed similar improvement |
| Bentsen et al281 | Prospective observational study | COPD patients assessed at baseline (T1: N=100), immediately before (T2: N=66), immediately after (T3: N=54) and 3 months after (T4: N=43) | 6-week outpatient PRP, including education, psychosocial support and training sessions | HADS, COPD self-efficacy scale, ISWT | A tendency of less anxiety and depression immediately after (T3) compared with immediately before (T2) the PR program, but the changes were not significant. Higher level of self-efficacy and better exercise capacity are suggested to relieve anxiety and depression |
| Harrison et al282 | Comparative effectiveness research | n=518 patients with COPD Patients were categorized into 3 groups based on HADS scores pre PR (“none” 0–7, “probable” 8–10 and “presence” 11–21) | PRP twice a week for 7 weeks. A “responder” was defined as achieving a change of ≥48 m on ISWT and a “completer” if attended discharge assessment for PR | HADS, ISWT, CRQ-SR | Anxiety and depression did not reduce following PR in patients with no symptoms. Patients with a “probable” or “presence” of symptoms had significant reductions. There was a difference between subgroups in change for anxiety and depression with patients scoring highest on the HADS having the greatest reductions. There was no correlation between anxiety or depression and completion of PR. Responders and nonresponders did not differ in their anxiety or depression levels |
| Bratås et al283 | Prospective cohort study | n=111 stage I–IV COPD patients measured at baseline, 4 weeks and 6-month follow up | Evaluate the short- and long-term effects of a 4-week inpatient PRP | HADS, SGRQ | SGRQ scores and depression improved between baseline and program completion. After 6 months follow up, all SGRQ and HADS scores deteriorated. No significant differences between baseline and the end of follow up were found, except for worsening HADS anxiety score |
| Von Leupoldt et al284 | Prospective observational study | n=238 COPD patients with mean FEV1% predicted =54 | 3-week outpatient PR program was performed 6 h/d for 5 d/wk | 6MWD, 6MWT, HADS, SF-36 | PR was significantly associated with improvements in 6MWD, dyspnea after the 6MWT and during activities, and increased physical and mental QoL, as well as reduced anxiety and depression |
| Pirraglia et al285 | Prospective observational study | n=81 COPD patients with mean FEV1 1.23±0.39 L | PRP twice weekly for 8 weeks | BDI, BAI, CRQ-SR | The CRQ-SR and BDI scores improved significantly. Improvement in depressive symptoms was associated with improvement in fatigue, emotion and mastery |
| Bratås et al286 | Prospective observational study | n=136 patients with mild-to- severe COPD | Inpatient PRP for 7.5 hours a day, 5 d/wk for 4 weeks | HADS, SGRQ, 6MWD, TDI | A PRP improves HRQL and exercise capacity and reduces depression in COPD patients. Patients with mild or moderate disease are more likely to achieve an improved HRQoL after rehabilitation than patients with severe or very severe disease |
| Spencer et al287 | RCT | n=59 patients with moderate COPD completed an 8-week PRP I=31, C=28 |
Supervised, outpatient- based exercise plus unsupervised home exercise vs standard care of unsupervised home exercise training following an 8-week PRP | HADS, 6MWD, SGRQ | 12 months following pulmonary rehabilitation both weekly, supervised, outpatient-based exercise plus unsupervised home exercise and standard care of unsupervised home exercise successfully maintained 6MWD, SGRQ scores in subjects with moderate COPD. No significant change from baseline to 12 months for HADS scores |
| Ozdemir et al288 | RCT | n=50 male patients with COPD stage II and III I=25, C=25 |
4-week water-based PRP for 35 minutes, three times a week (totally 12 sessions) vs only medical therapy | HADS, 6MWD, CRDQ | Water-based exercises are effective in improving QoL and anxiety level in COPD patients |
| Godoy et al289 | Prospective observational study | n=30 patients with severe and extremely severe COPD | 12-week PRP, which included 24 physical exercise sessions, 24 respiratory rehabilitation sessions, 12 psychotherapy sessions and 3 educational sessions | BAI, BDI, SGRQ, 6MWT | Pre-PRP and post-PRP values revealed a significant decrease in the levels of anxiety and depression, as well as significant improvements in the distance covered on the 6MWT and the QoL index. The benefits provided by the PRP persisted throughout the 24-month study period |
| Elçi et al290 | RTC | n=78 inpatients with severe COPD | PRP (24 sessions, 90 minutes duration) vs standard medical care | HADS, SF-36, SGRQ, 6MWD | Significant differences were observed in the 6MWD measurements at the third month, as well as in the SF-36 QoL scale, SGRQ and HADS measurements at the second and third months, irrespective of FEV1 |
| Paz-Díaz et al223 | RCT | n=24 patients with severe COPD I=10, C=14 |
8-week PR program, 3 times a week for 8 weeks | BDI, STAI, MMRC, SGRQ | After PR, there was a significant improvement in the severity of depression, a decrease in symptoms, an increase in daily living activities, and a decrease in the total score of the SGRQ. Dyspnea measured by the MRC scale was significantly better in the PR group |
| Güell et al226 | RCT | n=40 patients with severe COPD FEV1, 35%±13%, I=18, C=17 | 16 weeks of PR that included breathing retraining and exercise | MBHI, SCL-90-R, 6MWD, CRQ | PR may decrease psychosocial morbidity in COPD patients even when no specific psychological intervention is performed. Findings from this study also confirm the positive impact of PR on functional exercise capacity and HRQoL |
| Alexopoulos et al225 | Prospective observational study | n=63 patients with COPD and major depression recruited from a pulmonary rehabilitation unit | Brief inpatient PRP (median length of stay was 16 days) | Hamilton Depression Scale | Approximately 51% of subjects met criteria for response and 39% met criteria for remission. History of treatment for depression was associated with limited change in depressive symptoms, whereas social support and satisfaction with treatment were predictors of improvement. Improvement of depression may be the result of behavioral interventions rather than the use of antidepressant drugs |
| Kayahan et al291 | RCT |
I=26 PR, C= 19 Stage I–III COPD patients |
2 months PR program, for 3 days and 2 1/2 hours weekly | HAM-A, HAM-D | There was a significant decrease in HAM-A scores in the rehabilitation group. On the contrary the HAM-A scores did not change in control group. The decrease in HAM-A scores in rehabilitation group was also statistically significant compared with the control group. There was no significant difference in HAM-D scores within the two groups and also there was no significant difference between the two groups in HAM-D scores. The health status, exercise tolerance and dyspnea intensity improved significantly in the rehabilitation group compared to the control group |
| Arnardóttir et al292 | RCT | n=60 patients with COPD stage II and III I=28, FEV1: 35%±13% C=32, FEV1: 32%±10% |
PR program twice weekly (90-minute duration) for 16 weeks after randomization to interval – 3-minute intervals (I) – or continuous training (C) | HADS, SF-36, CRDQ, 12 MWD | Interval training and continuous training were equally potent in improving peak exercise capacity, functional exercise capacity, dyspnea, mental health and HRQoL in patients with moderate or severe COPD |
| Goldberg et al293 | Prospective observational study | n=45 patients with COPD stage III | 3 weeks of inpatient PRP | BDI, Hamilton Anxiety Scale, Goldberg Scale, and Modified Borg Scale | The program significantly reduced anxiety and depression, and increased positive psychological outlook in severe pulmonary disease. Perceived breathlessness on the Borg Scale was significantly reduced |
| Trappenburg et al294 | Prospective observational study | n=81 patients with COPD stage II–IV, FEV1: 40%±16% | 3 months PR program (2 hours sessions, 3 times per week) | HADS, CRDQ, PFSDQ-M, 6MWT | The effects of rehabilitation are not affected by baseline psychosocial factors. Patients with less favorable psychologic or sociodemographic conditions can also benefit from pulmonary rehabilitation |
| Garuti et al195 | Prospective observational study | n=149 COPD patients, stage II–III, after an exacerbation | Inpatient PRP twelve 3-hours daily sessions | HADS, SGRQ, 6MWD | Inpatient pulmonary rehabilitation may improve levels of anxiety and depression as well as symptoms, exercise capacity and HRQoL in moderate-to-severe COPD patients after an acute exacerbation |
| Cilione et al295 | Prospective observational study | n=132 COPD patients stage II and III recovering from an acute exacerbation | Inpatient PR program: 12 sessions (6 d/wk), lasted for 3 hours daily | HADS, SGRQ, 6MWD | 6MWD increased by 34%, HAD-anxiety decreased by 16%, HAD-depression decreased by 13% and SGRQ decreased by 11% |
| White et al296 | RCT | n=103 COPD patients stage III, n1=44, n2=49 | n1: PRP twice a week for a 2-hour session for 6 weeks vs n2: brief advice | HADS, SF-36, CRQ, shuttle walking distance | At 3 months both groups reported reduced anxiety on the Hospital Anxiety and Depression Scale and dimensions of QoL, but differences between groups were not significant. Shuttle walking distance increased significantly in the intervention group compared to controls |
| Withers et al217 | Prospective observational study | n=99 COPD patients stage III (35 had significant anxiety at screening and 18 significant depression) | 3 months PR program | HADS, shuttle walk distance | PR produced statistically significant falls in mean HADS scores, which remained significantly lowered at 6-month follow up. Patients with high anxiety levels showed significantly greater improvements in shuttle walk distance than those with low HAD scores |
| Emery et al261 | RTC | n=79 COPD outpatients stage II–III, EXESM =29, ESM =25, WL =25 | EXESM: 10-week PR with exercise, education, and stress management ESM: education and stress management; and WL: wait list control | CES-D, SCL-90-R, STAI, SIP and Physiologic Measures | Intervention participants in the PRP group, compared to the other 2 groups, reported improved endurance, reduced anxiety, and improved cognitive performance |
| Ries et al219 | RTC | n=119 stable COPD outpatients stage I–III, n1=57, n2=62 | n1:8-week PR program (twelve 4-hour sessions) vs n2: an 8-week education program (four 2-hour sessions biweekly for 8 weeks) | CES-D, Quality of Well- Being Scale and Physiologic Measures | Measures of lung function, depression, and general QoL, did not differ between groups. Differences tended to diminish after 1 year of follow-up |
| Emery et al297 | Prospective observational study | 64 PR patients with COPD FEV1/FVC <0.7 | PRP for 4 hours a day, 5 d/wk for 30 days | SCL-90-R, PGWI, neuropsychological assessment | Enhanced cognitive functioning and psychological well-being |
| Dekhuijzen et al298 | RTC | n=60 COPD outpatients stage II–III, with anxiety, depression. 3 groups of 20 patients: PR 2, TF-IMT and PR + TF-IMT | PR and PR + TF-IMT: 10-week PR program (5 d/wk for 2 hours) vs TF-IMT | SCL-90, DPI, 12 MWD, ADL | PR with or without additional TF-IMT resulted in a decrease of anxiety and depression, but there were no significant differences between the two patient groups. In the PR group, these scores were still decreased after a 1-year follow-up period. TF-IMT alone had no effects on the psychological parameters |
| Coventry and Hind216 | Review and meta- analysis: 6 RCTs | n=269 clinically stable moderate-to-severe COPD patients | Comparing PRP ≥4 weeks with up to 3 sessions/wk vs standard care (with or without education) | Standardized measures of depression and/or anxiety and generic or disease-specific HRQoL measures | PRP was significantly more effective than standard care in reducing short-term anxiety and depression. Long-term follow up data showed that gains in both psychological health status and HRQoL were not sustained at 12 months |
| Coventry et al246 | Review and meta- analysis: 30 RCTs | n=2,063 COPD patients stage II–III | Multicomponent exercise training vs relaxation techniques vs CBT vs self-management education | Standardized measures of depression and/or anxiety | Multicomponent exercise training effectively reduces symptoms of anxiety and depression in all people with COPD regardless of severity of depression or anxiety, highlighting the importance of promoting physical activity in this population |
| Wiles et al299 | Review: 12 RCTs | n=738 COPD patients stage II–III | Exercise and psychological components vs control conditions or active comparators | Standardized measures of depression and/or anxiety, QoL, dyspnea, functional exercise capacity | Results for depression, anxiety, QoL, dyspnea, functional exercise capacity favored interventions which included both exercise + psychological components compared with control conditions. Compared with active comparators results were inconsistent for depression and QoL |
Abbreviations: HADS, Hospital Anxiety and Depression Scale; ISWT, incremental shuttle walk test; HAM-D, Hamilton Depression Rating Scale; HAM-A, Hamilton Anxiety Rating Scale; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; STAI, State Trait Anxiety Inventory; MMRC, Modified Medical Research Council Scale; CRQ-SR, Chronic Respiratory Questionnaire – Self reported; CRDQ, Chronic Obstructive Disease Questionnaire; SCL-90-R, Hopkins Symptoms Checklist Revised; DASS, Depression Anxiety and Stress Scales; CES-D, Center for Epidemiologic Studies Depression Scale; PGWI, Psychological General Well-being Index; QoL, quality of life; SF-36, 36-Item Short Form Health Survey; 6MWT, 6-minutes walking test; MBHI, Millon Behavior Health Inventory; 12 MWD, 12 minutes walking distance; SGRQ, St Georges Respiratory Questionnaire; SIP, Sickness Impact Profile; TDI, Transitional Dyspnea Index; MHLC, Multidimensional Health Locus of Control inventory; 6MST, 6-minute stepper test; TUG, Timed Up and Go; VSRQ, Visual Simplified Respiratory Questionnaire; MCID, minimal clinically important difference; PFSDQ-M, Modified Pulmonary Functional Status and Dyspnea Questionnaire; MRC, Medical Research Council; ADL, Activities-in-Daily-Life; DPI, Dutch Personality Inventory; PR, pulmonary rehabilitation; TF-IMT, target-flow inspiratory muscle training; I, intervention group; C, control group; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; HRQoL, health-related QoL; CAT, COPD assessment test; HAD-D, Hospital Anxiety and Depression Scale – Depression subscale; HAD-A, Hospital Anxiety and Depression Scale – Anxiety subscale.
Pharmacological treatment
Management of depression and anxiety in COPD patients starts with the correct diagnosis. Many patients suffer transitory mood symptoms during respiratory exacerbations and there is no evidence that these time-limited symptoms require specific treatment. NICE guidelines117 advise that antidepressants should not be routinely prescribed for physically ill patients with subthreshold symptoms of depression or mild-to-moderate depression. Pharmacological therapy must be considered when major depression is diagnosed to avoid its long-term effects on overall disability.17,118–120 A recent study in USA reported that less than a third of COPD patients with major depression received appropriate treatment.121 The importance of routine screening in COPD patients for depressive symptoms is considered paramount in order to initiate the most appropriate treatment (especially after acute exacerbations and when changes occur in patients’ circumstances).122
All antidepressants have similar effectiveness but mainly differ based on type and severity of side effects. Based on which chemicals in the brain they affect, the main categories are tricyclic antidepressants (TCAs), tetracyclic antidepressants, monoamine oxidase inhibitors, reversible inhibitors of monoamine oxidase, selective serotonin reuptake inhibitors (SSRIs), serotonin and noradrenaline reuptake inhibitors, noradrenergic and specific serotonergic antidepressants, norepinephrine and dopamine reuptake inhibitors, and melatonergic antidepressants.
The choice of antidepressant depends on the pattern of depression,123 and it is useful to differentiate between early- and late-onset depression,94 because there is a distinct symptom profile that necessitates diverse treatment strategies. Late-onset depression or geriatric vascular depression after COPD diagnosis, caused by physiologic changes associated with COPD that have direct effect on brain’s vasculature, is characterized by more cognitive dysfunction, physical disability, limited insight, and psychomotor retardation and necessitates support networks and protection against continuous vascular damage. Late-onset depression has been found to be more refractory to treatment with antidepressants,124,125 associated with a greater degree of patient apathy,126 and less often associated with a family history of depression.127,128 On the other hand, early-onset depression is defined as depression that develops prior to the diagnosis of COPD, often during an individual’s youth. This type of depression is often reflective of a genetic vulnerability to depression, which increases adolescents’ risk for developing addiction to nicotine and presents with more classic symptoms, but might have greater difficulty with smoking cessation.129,130
It is also necessary to consider that the prescribed medications should not cause sedation or respiratory depression in patients with chronic respiratory conditions. Plus, the ideal medication should have a low side effect profile, a short half-life with no active metabolites,8 and provoke few drug interactions, especially when considering the other already administered medications for COPD.131 The most commonly used agents in COPD are β2-adrenergic agonists and anticholinergic medication. β2-adrenergic agonists can cause dose-related prolongation of the QT interval and potassium loss. Thus coadministration with some SSRIs and TCAs that can prolong QT interval may result in additive effects and increased risk of ventricular arrhythmias. Also, the anticholinergic action of TCAs may be added to that of anticholinergic bronchodilators used in COPD. Besides pharmacodynamics, pharmacokinetic interactions should be considered, and hence medications with the lowest potential to interfere with cytochrome P450 system should be considered.132
In general, antidepressants seem to have little effect on ventilator drive, but caution should be taken while prescribing certain antidepressants (TCAs and mirtazapine) in COPD patients with hypercapnia.112,133 On the contrary, benzodiazepines may cause respiratory depression and should be avoided, especially for patients with COPD who are CO2 retainers.134,135 A recent prospective study136 evaluating the safety of benzodiazepines and opioids in patients with very severe COPD indicated that concurrent use of benzodiazepines and opioids in lower doses (<0.3 defined daily doses per day) was not associated with increased admissions or mortality, whereas higher doses (>0.3 defined daily doses per day) might increase mortality. Additionally, β-blockers are contraindicated in these patients, despite their anxiolytic effect due to their potential risk of bronchoconstriction.73 Low-potency atypical antipsychotics in very small dosages may alleviate anxiety symptoms in these patients, but should be used with caution as they can have potential neurological and cardiovascular side effects.26
Small, placebo-controlled trials of antidepressant drug therapy in patients with COPD did not demonstrate significant treatment effects, with the exception of one study, in 1992,137 which indicated high efficacy for nortriptyline in improving short-term outcomes for depression, anxiety, cognitive function, and overall disability. Other TCAs have been tested, such as doxepine,138 imipramine, and amitriptyline,139–142 with contradictory results. More recent studies143–147 have used SSRIs, the current first-line medications for the management of depression, but most suffered from methodological flaws. In few randomized, double-blind, placebo-controlled studies, sertraline,145,146 fluoxetine,143,148 citalopram,149 and paroxetine147 offered improvements in quality of life, dyspnea, and fatigue. Start-up side effects with SSRIs include gastrointestinal upset, headache, tremor, and either psychomotor activation or sedation, which is frequently problematic in COPD patients. Treatment timelines necessitate checking the tolerance of medication during 1–3 weeks, then evaluating the response during 2–4 weeks, and if there is response, it is important to complete symptom resolution and move on to continuation and then maintenance phase. In case there is none or inadequate response, augmenting strategies are advised or change of medication is required.14 Either way, it is necessary to consult a psychiatrist150 in cases of suicidal or self-injurious behavior, psychotic or bipolar depression, or other psychiatric comorbidities (eg, substance abuse, personality disorders). The presence of complex psychological issues, multimorbidity, frailty, and polypharmacy also necessitates integrated and comprehensive approach for the care of these people.151
Concerning anxiety, several studies have investigated the effectiveness of specific medications152 with contradictory results for buspirone153,154 and inconclusive results for SSRIs, even though they are better tolerated and can relieve symptoms of panic,145,146 but compliance may be poor.143 A recent Cochrane review155 on pharmacological interventions for the treatment of anxiety in COPD patients analyzed four studies and found insufficient evidence of benefit for any of medications included. Two studies using SSRIs showed a nonsignificant reduction in anxiety symptoms,144,156 while two other studies using TCA and azapirones did not show any improvement.138,154 Anticonvulsants such as gabapentin have also been prescribed for the treatment of anxiety symptoms in COPD patients.73
Some authors report143,157 that patients with COPD and psychiatric comorbidity are reluctant to take yet another medication, possibly because of stigma associated with the disease or denial, and as mentioned before, data supporting the efficacy of medication-only treatment are extremely limited.158,159
When implementing treatment strategies for COPD patients, it is important to remember that there is a greater possibility for medical comorbidities, increased risk for medication interactions, and greater physical debilitation than the community population.160 An overview of studies on pharmacological treatment for anxiety and depression in COPD patients is summarized in Table 1.
Psychotherapeutic interventions
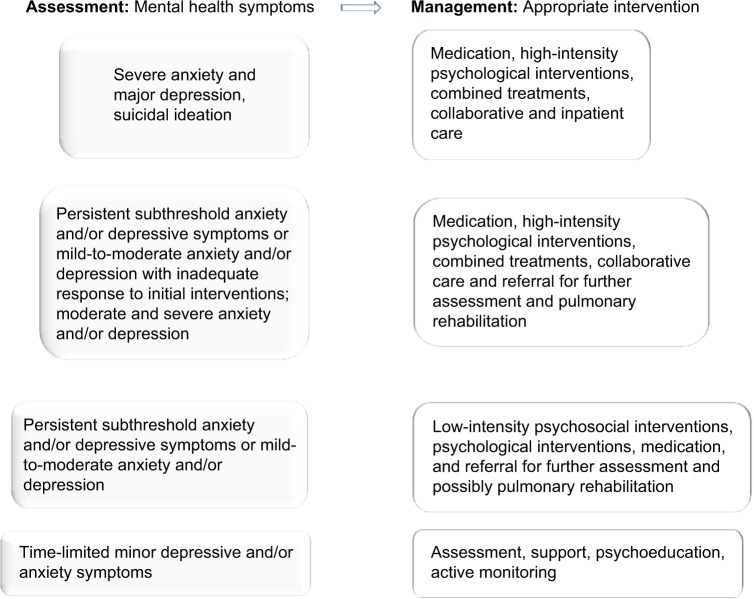
Patients prefer nondrug treatments,161 and clinical guidelines117,162 promote nonpharmacological interventions as first-line therapy for depression and anxiety in people with long-term conditions. NICE recommends use of low- (eg, self-help programs) or high-intensity (individual or group CBT) psychosocial interventions depending on the severity of mood symptoms.163 Both individual and group therapy psychological interventions are useful in promoting more adaptive coping in COPD patients.92
CBT
Evidence suggests that individualized or group CBT is the treatment of choice for addressing the maladaptive coping in the COPD patient with mental health difficulties, because of the time-limited and action-oriented nature of the intervention.164 According to this psychotherapeutic approach, emphasis is given to the effect of cognitions on mood and behavior. This model of psychotherapy assumes that maladaptive, or faulty, thinking patterns cause maladaptive behavior and “negative” emotions. Maladaptive behavior is behavior that is counterproductive or interferes with everyday living.14 The treatment focuses on changing an individual’s thoughts (cognitive patterns) in order to change his or her behavior and emotional state. Therapists attempt to make their patients aware of these distorted thinking patterns, or cognitive distortions, that fuel anxiety and depressive symptoms and change them (a process termed cognitive restructuring).14 Therapy focuses on helping patients discover alternative solutions and promote more adaptive coping styles in order to overcome adversities and effectuate operational techniques to address their problems.165–167
Mental health guidelines recommend CBT as the treatment of choice for a range of mood and anxiety disorders and as an adjunct to other treatments. Low-intensity CBT-based psychosocial interventions are recommended for people with mild-to-moderate anxiety and/or depression, whereas high-intensity psychological interventions using CBT in combination with medication is recommended for people with moderate-to-severe depression.162,163 Not all aspects of CBT may be necessary to produce a therapeutic effect. Purely behavioral interventions can be as effective as CBT for patients with depression.168
Some studies report that there is potential for psychological interventions to reduce anxiety and depression in people with COPD.169,170 A recent meta-analysis of four CBT studies for anxiety and depression in COPD patients indicated improvements in these symptoms.171 Also, based on randomized controlled trials, CBT resulted in improvement in symptoms of anxiety and depression (Table 2), especially when used with exercise and education.172
Group psychotherapy
Group psychotherapy is a financially attractive approach in response to the realities of limited resources, regardless of its theoretical orientation, because it involves fewer therapists, less therapist per person-hours, and serves more patients.
The group context and group process, if explicitly utilized within the principles of system dynamics, offers valuable healing opportunities.14 Therapeutic principles,173,174 termed “therapeutic” factors, include the experience of relief from emotional distress through the free and uninhibited expression of emotion, feeling a sense of belonging, acceptance, and validation. Within a context that reflects the individual’s perception of reality, group members share experiences and feelings and develop social skills through a modeling process.
The therapist’s interventions facilitate group activities by taking advantage of the inherent assets of the team, ensuring that it runs efficiently with appropriate boundaries being maintained.14
Relaxation therapy and alternative treatments
Relaxation therapy encompasses a range of techniques such as breathing exercises, sequential muscle relaxation, biofeedback, guided imagery, distraction therapy, hypnosis, meditation/mindfulness, and physical posture therapy.175,176 Often, some of these techniques are components of PR or are used as an adjunct to other therapies (eg, CBT).112 The purpose of this therapy is to promote psychological change by effectively managing physiological changes accompanying anxiety. In other words, regulation of the sympathetic nervous system and management of the stimulation of certain regions of the hypothalamus facilitate the relaxation response.177 In this perspective, relaxation techniques are often used to inhibit anxiety, increasing the patient’s perception of self-control or modulating his or her emotions, in order to promote the perceived well-being of the subject.
A meta-analysis of trials with relaxation-based therapies for COPD patients indicated statistically significant beneficial effects on both dyspnea and psychological well-being.178 Another recent meta-analysis on the effects of relaxation techniques, of 25 randomized controlled trials including both inpatients and outpatients with COPD, showed a minor positive effect on respiratory function as well as a slight effect on levels of both the anxiety and depression. The higher effect size was found in the quality of life value.176
Several other studies have investigated other types of relaxation approaches.179 In a pilot study, the authors argued that the introduction of Tai Chi exercises was worth exploring in patients with COPD,180 while in another study,181 Yoga exercises were performed. Singing lessons have also been used as an intervention in patients with COPD.182,183 The basic theory is that singing lessons could improve quality of life or functional status in these patients.184 Regarding these less traditional interventions, there is still lack of certainty about their applicability, their long-term effectiveness, the active component (physical or psychological), and how they can be incorporated into standard care.185 An overview of studies on relaxation therapies and alternative treatments for anxiety and depression in COPD patients is summarized in Table 3.
PR
Treatment strategies include PR, because it improves patient’s ability to participate in stress-reducing activities and increases their sense of self mastery. It also improves quality of life by increasing patients’ perception of available social supports.186 According to the American Thoracic Society and the European Respiratory Society, PR187 is an evidence-based multidisciplinary and comprehensive intervention for patients with chronic respiratory diseases who are symptomatic and often have decreased daily life activities.
The ideal patient for PR is one with functional limitations, moderate-to-severe lung disease, who is stable on standard therapy, without comorbid serious or unstable medical conditions, willing to learn about the disease, and motivated to devote time and effort necessary to benefit from a comprehensive care program.188
The interdisciplinary team of health-care professionals in PR may include physicians, nurses, respiratory and physical therapists, psychologists, and exercise specialists.151 PR programs operate by means of progressive exercise, training of respiratory function, and psychoeducation, so that patients obtain better exercise tolerance with less dyspnea. The goal is to restore the patient to the highest possible level of independent function.189 Patients are educated about their disease and learn breathing techniques to reduce air hunger and exercises to optimize oxygen use, and this in turn improves exercise tolerance. Key outcomes such as exercise capacity and overall health-related quality of life may be accurately measured.190–192
Exercise-based PR programs have been the most consistently helpful interventions for minor mood symptoms in COPD patients,193–195 but the greatest improvements in anxiety and depression are usually in those with the highest scores at baseline.196 The paradox is that patients most likely to benefit from PR appear least likely to complete it.197,198 It is important therefore to be able to identify patients with COPD who may need additional support to complete a PR program in order to broaden benefit to all.
Several mechanisms have been hypothesized to explain the effect of exercise rehabilitation on mental health symptoms. Biological mechanisms associated with exercise activity include changes in central monoamine function,199–204 enhanced hypothalamic–pituitary–adrenal axis regulation, increased release of endogenous opioids,205–207 and reduced systemic inflammation.208,209 In this way, regular physical activity may reduce depression and anxiety among patients undergoing PR. In addition, behavioral mechanisms210–215 associated with exercise activities operate synergistically to produce reductions of symptoms. Such mechanisms include active distraction from worrying thought patterns (rumination), increase of self-efficacy by providing patients with a meaningful mastery experience, and provision of daily pleasant events and regular social contact and support.
A recent systematic review216 showed that PR is beneficial in reducing anxiety and depressive symptoms, but the long-term benefit is unknown. Studies combining antidepressant pharmacotherapy or psychotherapy indicated more effective results than PR alone.217,218 Because both depression and anxiety may be manifested in physical symptoms during the course of a PR program, collaborative care is essential among all involved health-care professionals to ensure that patients’ problems are identified, evaluated, and treated.
The majority of PR programs have a primary exercise focus in order to recondition the legs and other peripheral muscles, making them more efficient as to oxygen needs, and thereby requiring relative less breathing to satisfy these oxygen requirements.219 Additionally, PR programs teach breathing control exercises to patients and educate them in recognizing an impending dyspnea attack and preventing it, or controlling it, so they lose their fear of exerting themselves.220
In PR settings, patients learn that they can have increases in activity levels and in dyspnea without perceiving that increase in dyspnea as a medical crisis. When patients experience their symptoms safely, they become desensitized by learning to distinguish between physical and emotional symptoms. Then, these patients can gradually take responsibility for the day-to-day management of their condition, with a result of improving their confidence, control, and autonomy.221
PR should be offered to all COPD patients irrespective of disease severity, since they all get improvements,222,223 from mild COPD224 to severe-to-very severe lung disease.225,226 Emphasis should be given to exercise training with respect to patients with mild-to-moderate disease, but for patients with severe-to-very severe COPD, PR programs should be tailored mostly toward dyspnea management and psychological support.227,228
In sum, the preponderance of recent evidence supports the utility of PR for reducing depression and anxiety and enhancing cognitive performance, but it is necessary to maintain the physical activity regimen to sustain the gains in physical fitness, mood, and cognitive performance, otherwise a relapse is inevitable.193 Representative studies with PR programs for COPD patients are summarized in Table 4.
Discussion and recommendations
Mental health problems in COPD remain underdiagnosed and undertreated.229 Although more than one-third of individuals with COPD experience comorbid symptoms of depression and anxiety,230 available evidence suggests that less than one-third of COPD patients with such comorbidity are receiving appropriate treatment for this.231 Every clinician caring for patients with COPD should have a high level of suspicion regarding the presence of mental health comorbidities since they are associated with poorer outcomes.230
The first step to improve practice is to achieve earlier and more accurate diagnosis. It is not clear when screening should be done232,233 and if it should be carried out with all COPD patients or just to those at higher risk of these comorbidities.29 Current screening tools for anxiety and depression in patients with COPD were primarily validated for patients with other chronic diseases.234–237 The Hospital Anxiety Depression and the Beck Depression and Anxiety Inventory scales have been recommended as the preferable choice of screening tools for anxiety and depression in patients with COPD.29 Clinicians should be aware of the somatic overlap between anxiety and/or depression and COPD.238,239
Mild-to-moderate symptoms of anxiety and/or depression should not be ignored, and treatment should be considered. High-scoring patients should be referred to a mental health specialist for a comprehensive diagnostic assessment using structured clinical interviews. It is well known that physiological, functional, and psychosocial consequences of COPD are only poorly to moderately related to each other.240 This means that a comprehensive assessment of the effects of COPD requires a battery of instruments that not only tap the disease-specific effects, but also the overall burden of the disease on everyday functioning and emotional well-being. Accurate assessment will ensure that treatment modalities are targeting the specific mental health problem taking into account individual factors, such as genetic predisposition, nicotine addiction, social support, other comorbidities, etc.
Identification of mental health problem should guide the choice of pharmacological, psychotherapeutic, or other suitable intervention (Figure 1). While treatment guidelines highlight the importance of recognizing and treating depression and anxiety in patients with COPD, there are few clear evidence-based pathways for the treatment of depression and anxiety. A GOLD report states that there is no evidence that anxiety and depression should be treated differently in the presence of COPD, so at this point of time guidelines are based on treatment of depression and anxiety for the general population.1
Figure 1.
Recommendations for appropriate interventions following assessment of mental health symptoms in patients with COPD.
In clinical practice, bidirectional associations between depression and/or anxiety and COPD imply the need to promote approaches that integrate physical and mental health care. The NICE has published clinical guidelines for managing depression in people with long-term conditions.113 The guidelines review the evidence for the associated service-level interventions (such as stepped care and collaborative care) and psychosocial, psychological, and pharmacological interventions.
According to reviews and meta-analysis,185,230 current evidence for treatment options to reduce anxiety and depression in patients with COPD include pharmacological treatments, CBT, PR, relaxation therapy, and personalized interventions.241,242 PR has extensive evidence supporting its benefits, and it has been shown to significantly reduce symptoms of both anxiety and depression in COPD patients.216 Although there is lack of strong evidence for the efficacy of pharmacological treatment in patients with COPD with comorbid depression and anxiety, adding a depression- or anxiety-targeted treatment to the PR program may have additive therapeutic benefits.225 Maximizing the efficiency of services is important as limited health resources allocated to PR programs mean that not every patient with COPD who might benefit has access to them.
In recent years, a model of care termed the collaborative-care model has been found to be associated with significant improvement in depression outcomes.243–245 Collaborative-care models that focus on building partnerships between mental health and other professionals to foster integration of care for people with complex morbidities present a fruitful framework for the management of mental health in COPD.29 By definition, PR is an example of a collaborative-care model. In particular, the integration of PR and psychological therapies, such as CBT, has the potential to lead to significant patient benefits.230 Contemporary research suggests that complex psychological and/or lifestyle interventions, which include a PR component, have the greatest effects on depression and anxiety in patients with COPD.246
Most people with stable COPD are managed in primary care where recognition, assessment, and initial management of anxiety and depressive symptoms can be provided.229 Tailoring mental health interventions to adapt not only to the unique needs of COPD patients but also to the current primary care setting is necessary. From the earliest consultations, we should acknowledge patients’ beliefs about their COPD and its management to better assess their likely responsiveness to treatment. We can then more effectively deliver from a menu of interventions in order to improve outcomes. Continuity of care implies that when COPD patients need hospitalization for the treatment of exacerbations, mental health issues should be more systematically addressed enhancing benefit for the many not the few.
Limitations
Including nonrandomized studies and other reviews and meta-analyses resulted in differences to varying degrees from the typical intervention review. Reporting results in narratives impeded the drawing of statistical conclusions about the interventions’ summary effect.
Future needs
Future research studies should focus on:
Identifying which components of PR are essential, its ideal length and location (hospital-based inpatient or outpatient, or community-based, home-based), the degree of supervision and intensity of training required, how long treatment effects persist, and the barriers of PR attendance and completion in real-life PR settings.
Determining the best treatment for specific COPD groups, eg, based on sex, severity of COPD, frequency of exacerbations, and type and severity of comorbid mental health problems, so the efficacy of treatments in different subgroups can be assessed.
Disentangling the contributions of exercise training, education, and CBT in a COPD population with clear inclusion and exclusion criteria for anxiety and depression severity and adequately powered RCTs.
Investigate a range of treatment options in COPD across all care settings, including comparison of different treatment options and various combinations.
Address the cost-effectiveness and feasibility of targeted treatment of anxiety and depression, of the different interventions (eg, optimal length of therapy; when to stop treatment in nonresponders; identifying predictors of success and failure).
Examine novel types of disease management interventions with respect to social and behavioral principles and models most relevant for COPD patients in order to increase their engagement and improve health outcomes.247,248
Develop properly “evidence-based” COPD care programs that proactively address mental health in order to optimize physical and mental health outcomes.
Conclusion
Patients suffering from COPD frequently experience comor-bid symptoms of anxiety and depression. Detection and recognition of these symptoms is of utmost importance as they are related to both disease progression, treatment, and rehabilitation procedures. Although the literature on treating anxiety and depression in COPD patients is limited, we believe that it points to a more multidisciplinary approach and to the implementation of personalized strategies to address both anxiety and depressive symptoms in these patients.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Global Initiative for Chronic Obstructive Lung Disease Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. [Accessed December 21, 2015]. [Updated 2015]. Available from: http://www.goldcopd.org/
- 2.National Heart Lung and Blood Institute . What is COPD? Bethesda, MD: US National Institutes of Health; [Accessed January 9, 2016]. Updated July 31, 2013. Available from: http://www.nhlbi.nih.gov/health/health-topics/topics/copd. [Google Scholar]
- 3.Zwar NA, Marks GB, Hermiz O, et al. Predictors of accuracy of diagnosis of chronic obstructive pulmonary disease in general practice. Med J Aust. 2011;195(4):168–171. doi: 10.5694/j.1326-5377.2011.tb03271.x. [DOI] [PubMed] [Google Scholar]
- 4.Nathell L, Nathell M, Malmberg P, et al. COPD diagnosis related to different guidelines and spirometry techniques. Respir Res. 2007;8(1):89. doi: 10.1186/1465-9921-8-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 6.Lopez AD, Shibuya K, Rao C, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27:397–412. doi: 10.1183/09031936.06.00025805. [DOI] [PubMed] [Google Scholar]
- 7.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edmunds M, Scudder L. Examining the relationships between COPD and anxiety and depression. Heart Lung. 2009;38:34–47. [Google Scholar]
- 9.Pooler A, Beech R. Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic review. Int J Chron Obstruct Pulmon Dis. 2014;9:315–330. doi: 10.2147/COPD.S53255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yohannes AM, Baldwin RC, Connolly MJ. Depression and anxiety in elderly outpatients with chronic obstructive pulmonary disease: prevalence, and validation of the BASDEC screening questionnaire. Int J Geriatr Psychiatry. 2000;15:1090–1096. doi: 10.1002/1099-1166(200012)15:12<1090::aid-gps249>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 11.Lacasse Y, Rousseau L, Maltais F. Prevalence of depressive symptoms and depression in patients with severe oxygen-dependent chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2001;21:80–86. doi: 10.1097/00008483-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Aghanwa HS, Erhabor GE. Specific psychiatric morbidity among patients with chronic obstructive pulmonary disease in a Nigerian general hospital. J Psychosom Res. 2001;50:179–183. doi: 10.1016/s0022-3999(00)00206-3. [DOI] [PubMed] [Google Scholar]
- 13.Hill K, Geist R, Goldstein RS. Anxiety and depression in end-stage COPD. Eur Respir J. 2008;31(3):667–677. doi: 10.1183/09031936.00125707. [DOI] [PubMed] [Google Scholar]
- 14.Tselebis A, Bratis D, Pachi A, et al. Anxiety and depression in patients with chronic obstructive pulmonary disease (COPD) In: Zirimis L, Papazoglakis A, editors. Chronic Obstructive Pulmonary Disease: New Research. New York, NY: Nova Science Publishers; 2013. pp. 15–40. [Google Scholar]
- 15.Light RW, Merrill EJ, Despars JA, et al. Prevalence of depression and anxiety in patients with COPD: relationship to functional capacity. Chest. 1985;87:35–38. doi: 10.1378/chest.87.1.35. [DOI] [PubMed] [Google Scholar]
- 16.Di Marco F, Verga M, Reggente M, et al. Anxiety and depression in COPD patients: the roles of gender and disease severity. Respir Med. 2006;100:1767–1774. doi: 10.1016/j.rmed.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 17.Katz PP, Julian LJ, Omachi TA, et al. The impact of disability on depression among individuals with COPD. Chest. 2010;137:838–845. doi: 10.1378/chest.09-1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McSweeny AJ, Grant I, Heaton RK, et al. Life quality of patients with chronic obstructive pulmonary disease. Arch Intern Med. 1982;142(3):473–478. [PubMed] [Google Scholar]
- 19.Isoaho R, Keistinen T, Laippala P, et al. Chronic obstructive pulmonary disease and symptoms related to depression in elderly persons. Psychol Rep. 1995;76:287–297. doi: 10.2466/pr0.1995.76.1.287. [DOI] [PubMed] [Google Scholar]
- 20.Borak J, Sliwinski P, Piasecki Z, et al. Psychological status of COPD patients on long term oxygen therapy. Eur Respir J. 1991;4:59–62. [PubMed] [Google Scholar]
- 21.Engstrom CP, Persson LO, Larsson S, et al. Functional status and well being in chronic obstructive pulmonary disease with regard to clinical parameters and smoking: a descriptive and comparative study. Thorax. 1996;51:825–830. doi: 10.1136/thx.51.8.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White RJ, Rudkin ST, Ashley J, et al. Outpatient pulmonary rehabilitation in severe chronic obstructive pulmonary disease. J R Coll Physicians Lond. 1997;31:541–545. [PMC free article] [PubMed] [Google Scholar]
- 23.Bosley CM, Corden ZM, Rees PJ, et al. Psychological factors associated with use of home nebulized therapy for COPD. Eur Respir J. 1996;9:2346–2350. doi: 10.1183/09031936.96.09112346. [DOI] [PubMed] [Google Scholar]
- 24.Jones PW, Baveystock CM, Littlejohns P. Relationships between general health measured with the sickness impact profile and respiratory symptoms, physiological measures, and mood in patients with chronic airflow limitation. Am Rev Respir Dis. 1989;140:1538–1543. doi: 10.1164/ajrccm/140.6.1538. [DOI] [PubMed] [Google Scholar]
- 25.Karajgi B, Rifkin A, Doddi S, et al. The prevalence of anxiety disorders in patients with chronic obstructive pulmonary disease. Am J Psychiatry. 1990;147:200–201. doi: 10.1176/ajp.147.2.200. [DOI] [PubMed] [Google Scholar]
- 26.Mikkelsen RL, Middelboe T, Pisinger C, et al. Anxiety and depression in patients with chronic obstructive pulmonary disease (COPD). A review. Nord J Psychiatry. 2004;58:65–70. doi: 10.1080/08039480310000824. [DOI] [PubMed] [Google Scholar]
- 27.Dowson CA, Kuijer RG, Mulder RT. Anxiety and self-management behaviour in chronic obstructive pulmonary disease: what has been learned? Chron Respir Dis. 2004;1:213–220. doi: 10.1191/1479972304cd032rs. [DOI] [PubMed] [Google Scholar]
- 28.Hynninen KM, Breitve MH, Wiborg AB, et al. Psychological characteristics of patients with chronic obstructive pulmonary disease: a review. J Psychosom Res. 2005;59:429–443. doi: 10.1016/j.jpsychores.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 29.Maurer J, Rebbapragada V, Borson S, et al. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008;134(4 Suppl):43S–56S. doi: 10.1378/chest.08-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31:58–69. doi: 10.1016/j.jpainsymman.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 31.Felker B, Katon W, Hedrick SC, et al. The association between depressive symptoms and health status in patients with chronic pulmonary disease. Gen Hosp Psychiatry. 2001;23:56–61. doi: 10.1016/s0163-8343(01)00127-x. [DOI] [PubMed] [Google Scholar]
- 32.Yohannes AM, Baldwin RC, Connolly MJ. Depression and anxiety in elderly patients with chronic obstructive pulmonary disease. Age Ageing. 2006;35(5):457–459. doi: 10.1093/ageing/afl011. [DOI] [PubMed] [Google Scholar]
- 33.Hanania NA, Mullerova H, Locantore NW, et al. Determinants of depression in the ECLIPSE chronic obstructive pulmonary disease cohort. Am J Respir Crit Care Med. 2011;183:604–611. doi: 10.1164/rccm.201003-0472OC. [DOI] [PubMed] [Google Scholar]
- 34.Cully JA, Graham DP, Stanley MA, et al. Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics. 2006;47:312–319. doi: 10.1176/appi.psy.47.4.312. [DOI] [PubMed] [Google Scholar]
- 35.Prigatano GP, Wright EC, Levin D. Quality of life and its predictors in patients with mild hypoxemia and chronic obstructive pulmonary disease. Arch Intern Med. 1984;144(8):1613–1619. [PubMed] [Google Scholar]
- 36.Kosmas E, Tselebis A, Bratis D, et al. The Relationship between the adherence to treatment and the psychological profile of patients with chronic obstructive pulmonary disease. Chest. 2014;145(3_MeetingAbstracts):377A. [Google Scholar]
- 37.Stapleton RD, Nielsen EL, Engelberg RA, et al. Association of depression and life-sustaining treatment preferences in patients with COPD. Chest. 2005;127:328–334. doi: 10.1378/chest.127.1.328. [DOI] [PubMed] [Google Scholar]
- 38.Laurin C, Moullec G, Bacon SL, et al. Impact of anxiety and depression on chronic obstructive pulmonary disease exacerbation risk. Am J Respir Crit Care Med. 2012;185:918–923. doi: 10.1164/rccm.201105-0939PP. [DOI] [PubMed] [Google Scholar]
- 39.Fan VS, Curtis JR, Tu SP, et al. Using quality of life to predict hospitalization and mortality in patients with obstructive lung diseases. Chest. 2002;122:429–436. doi: 10.1378/chest.122.2.429. [DOI] [PubMed] [Google Scholar]
- 40.Almagro P, Calbo E, de Echagüen AO, et al. Mortality after hospitalization for COPD. Chest. 2002;121:1441–1448. doi: 10.1378/chest.121.5.1441. [DOI] [PubMed] [Google Scholar]
- 41.Stage KB, Middelboe T, Pisinger C. Depression and chronic obstructive pulmonary disease (COPD). Impact on survival. Acta Psychiatr Scand. 2005;111(4):320–323. doi: 10.1111/j.1600-0447.2004.00497.x. [DOI] [PubMed] [Google Scholar]
- 42.Fan VS, Ramsey SD, Giardino ND, et al. Sex, depression, and risk of hospitalization and mortality in chronic obstructive pulmonary disease. Arch Intern Med. 2007;167:2345–2353. doi: 10.1001/archinte.167.21.2345. [DOI] [PubMed] [Google Scholar]
- 43.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: APA; 1994. [Google Scholar]
- 44.World Health Organization . The ICD-10 Classification of Mental and Behavioural Disorders Diagnostic Criteria for Research. Geneva, Switzerland: WHO; 1993. [Google Scholar]
- 45.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 46.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 47.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State–Trait Anxiety Inventory (Form Y) Palo Alto, CA: Consulting Psychologist’s Press; 1983. [Google Scholar]
- 48.Willgoss TG, Yohannes AM. Anxiety disorders in patients with COPD: a systematic review. Respir Care. 2013;58(5):858–866. doi: 10.4187/respcare.01862. [DOI] [PubMed] [Google Scholar]
- 49.Smoller JW, Pollack MH, Otto MW, et al. Panic anxiety, dyspnea, and respiratory disease. Theoretical and clinical considerations. Am J Respir Crit Care Med. 1996;154(1):6–17. doi: 10.1164/ajrccm.154.1.8680700. [DOI] [PubMed] [Google Scholar]
- 50.Klein DF. False suffocation alarms, spontaneous panics, and related conditions. An integrative hypothesis. Arch Gen Psychiatry. 1993;50:306–317. doi: 10.1001/archpsyc.1993.01820160076009. [DOI] [PubMed] [Google Scholar]
- 51.Dudley DL, Glaser EM, Jorgenson BN, et al. Psychosocial concomitants to rehabilitation in chronic obstructive pulmonary disease. Part 2: psychosocial treatment. Chest. 1980;77(4):544–551. doi: 10.1378/chest.77.4.544. [DOI] [PubMed] [Google Scholar]
- 52.Kim HF, Kunik ME, Molinari VA, et al. Functional impairment in COPD patients: the impact of anxiety and depression. Psychosomatics. 2000;41:465–471. doi: 10.1176/appi.psy.41.6.465. [DOI] [PubMed] [Google Scholar]
- 53.Pauwels RA, Buist AS, Calverley PMA, et al. GOLD Scientific Committee Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163:1256–1276. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 54.Patton GC, Hibbert M, Rosier MJ, et al. Is smoking associated with depression and anxiety in teenagers? Am J Public Health. 1996;86:225–230. doi: 10.2105/ajph.86.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Breslau N, Kilbey MM, Andreski P. Nicotine withdrawal symptoms and psychiatric disorders: findings from an epidemiologic study of young adults. Am J Psychiatry. 1992;149:464–469. doi: 10.1176/ajp.149.4.464. [DOI] [PubMed] [Google Scholar]
- 56.Acri JB, Grunberg N. A psychophysical task to quantify smoking cessation induced irritability: the reactive irritability scale (RIS) Addict Behav. 1992;17:587–601. doi: 10.1016/0306-4603(92)90068-7. [DOI] [PubMed] [Google Scholar]
- 57.Parrott AC. Stress modulation over the day in cigarette smokers. Addiction. 1995;90:233–244. doi: 10.1046/j.1360-0443.1995.9022339.x. [DOI] [PubMed] [Google Scholar]
- 58.Thornton A, Lee P, Fry J. Differences between smokers, ex-smokers, passive smokers and non-smokers. J Clin Epidemiol. 1994;47(10):1143–1162. doi: 10.1016/0895-4356(94)90101-5. [DOI] [PubMed] [Google Scholar]
- 59.Umezawa A. A respiratory control method based on psycho-physiological studies Proceedings of the 11th Annual Meeting of the International Society for the Advancement of Respiratory Psychophysiology (ISARP), Princeton NJ, October 17–19, 2004. Biol Psychiatry. 2006;(72):222–238. doi: 10.1016/j.biopsycho.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 60.O’Donnell D, Banzett R, Carrieri-Kohlman V, et al. Pathophysiology of dyspnea in chronic obstructive pulmonary disease: a roundtable. Proc Am Thorac Soc. 2007;4:145–168. doi: 10.1513/pats.200611-159CC. [DOI] [PubMed] [Google Scholar]
- 61.Jolley CJ, Moxham J. A physiological model of patient-reported breathlessness during daily activities in COPD. Eur Respir Rev. 2009;18(112):66–79. doi: 10.1183/09059180.00000809. [DOI] [PubMed] [Google Scholar]
- 62.Liotti M, Brannan S, Egan G, et al. Brain responses associated with consciousness of breathlessness (air hunger) Proc Natl Acad Sci U S A. 2001;98:2035–2040. doi: 10.1073/pnas.98.4.2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Evans KC, Banzett RB, Adams L, et al. BOLD fMRI identifies limbic, paralimbic, and cerebellar activation during air hunger. J Neurophysiol. 2002;88:1500–1511. doi: 10.1152/jn.2002.88.3.1500. [DOI] [PubMed] [Google Scholar]
- 64.Livermore N, Butler J, Sharpe L, McBain R, Gandevia S, McKenzie D. Panic attacks and perception of inspiratory resistive loads in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2008;178:7–12. doi: 10.1164/rccm.200711-1700OC. [DOI] [PubMed] [Google Scholar]
- 65.Bailey PH. The dyspnea–anxiety–dyspnea cycle – COPD patients’ stories of breathlessness: “It’s scary/when you can’t breathe”. Qual Health Res. 2005;14(6):760–778. doi: 10.1177/1049732304265973. [DOI] [PubMed] [Google Scholar]
- 66.Porzelius J, Vest M, Nochomovitz M. Respiratory function, cognitions, and panic in chronic obstructive pulmonary patients. Behav Res Ther. 1992;30:75–77. doi: 10.1016/0005-7967(92)90101-l. [DOI] [PubMed] [Google Scholar]
- 67.Howard C, Hallas C, Wray J, et al. The relationship between illness perceptions and panic in chronic obstructive pulmonary disease. Behav Res Ther. 2009;47:71–76. doi: 10.1016/j.brat.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 68.McKenzie D, Butler J, Gandevia S. Respiratory muscle function and activation in chronic obstructive pulmonary disease. J Appl Physiol. 2009;107:621–629. doi: 10.1152/japplphysiol.00163.2009. [DOI] [PubMed] [Google Scholar]
- 69.Vanderpool M. Resilience: a missing link in our understanding of survival. Harv Rev Psychiatry. 2002;10:302–306. doi: 10.1080/10673220216282. [DOI] [PubMed] [Google Scholar]
- 70.Dowson CA, Town GI, Framptom C, et al. Psychopathology and illness beliefs influence COPD self-management. J Psychosom Res. 2004;56(3):333–340. doi: 10.1016/S0022-3999(03)00040-0. [DOI] [PubMed] [Google Scholar]
- 71.O’Donnell DE, Webb K, McGuire M. Controlling Breathlessness and Cough Comprehensive Management of COPD. Hamilton, ON: BC Decker; 2002. [Google Scholar]
- 72.Lustig FM, Haas A, Castillo R. Clinical and rehabilitation regime in patients with chronic obstructive pulmonary diseases. Arch Phys Med Rehabil. 1972;53:315–322. [PubMed] [Google Scholar]
- 73.Cantor L, Jacobson R. COPD: how to manage comorbid depression and anxiety. J Fam Pract. 2003;2:11. [Google Scholar]
- 74.Brown GW, Andrews B, Harris T, Adler Z, Bridge L. Social support, self esteem and depression. Psychol Med. 1986;6:238–247. doi: 10.1017/s0033291700011831. [DOI] [PubMed] [Google Scholar]
- 75.Holahan CK, Holahan CJ. Self-efficacy, social support, and depression in aging: a longitudinal analysis. J Gerontol. 1987;42(1):65–68. doi: 10.1093/geronj/42.1.65. [DOI] [PubMed] [Google Scholar]
- 76.Kaptein AA, Scharloo M, Fischer MJ, et al. Illness perceptions and COPD: an emerging field for COPD patient management. J Asthma. 2008;45:625–629. doi: 10.1080/02770900802127048. [DOI] [PubMed] [Google Scholar]
- 77.Tselebis A, Kosmas E, Bratis D, et al. Prevalence of alexithymia and its association with anxiety and depression in a sample of Greek chronic obstructive pulmonary disease (COPD) outpatients. Ann Gen Psychiatry. 2010;9:16. doi: 10.1186/1744-859X-9-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mishima M, Oku Y, Muro S, et al. Relationship between dyspnoea in daily life and psycho-physiologic state in patients with chronic obstructive pulmonary disease during long term domiciliary oxygen therapy. Intern Med. 1996;35:453–458. doi: 10.2169/internalmedicine.35.453. [DOI] [PubMed] [Google Scholar]
- 79.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: APA; 2015. [Google Scholar]
- 80.Gift AG, McCrone SH. Depression in patients with COPD. Heart Lung. 1993;22:289–297. [PubMed] [Google Scholar]
- 81.Koenig HG. Differences between depressed patients with heart failure and those with pulmonary disease. Am J Geriatr Psychiatry. 2006;14:211–219. doi: 10.1097/01.JGP.0000192495.73673.3e. [DOI] [PubMed] [Google Scholar]
- 82.Kurosawa H, Shimizu Y, Nishimatsu Y, et al. The relationship between mental disorders and physical severities in patients with acute myocardial infarction. Jpn Circ J. 1983;47(6):723–728. doi: 10.1253/jcj.47.723. [DOI] [PubMed] [Google Scholar]
- 83.Katon W, Sullivan MD. Depression and chronic medical illness. J Clin Psychiatry. 1990;51:3–11. [PubMed] [Google Scholar]
- 84.Evans DL, Staab JP, Petitto JM, et al. Depression in the medical setting: biopsychological interactions and treatment considerations. J Clin Psychiatry. 1999;60(Suppl 4):40–55. [PubMed] [Google Scholar]
- 85.Yohannes AM, Baldwin RC, Connolly MJ. Prevalence of sub-threshold depression in elderly patients with chronic obstructive pulmonary disease. Int J Geriatr Psychiatry. 2003;18:412–416. doi: 10.1002/gps.851. [DOI] [PubMed] [Google Scholar]
- 86.Emery CF, Green MR, Suh S. Neuropsychiatric function in chronic lung disease: the role of pulmonary rehabilitation. Respir Care. 2008;53(9):1208–1216. [PubMed] [Google Scholar]
- 87.Graydon JE, Ross E. Influence of symptoms, lung function, mood, and social support on level of functioning of patients with COPD. Res Nurs Health. 1995;18(6):525–533. doi: 10.1002/nur.4770180608. [DOI] [PubMed] [Google Scholar]
- 88.Weaver TE, Richmond TS, Narsavage GL. An explanatory model of functional status in chronic obstructive pulmonary disease. Nurs Res. 1997;46(1):26–31. doi: 10.1097/00006199-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 89.Johnson G, Kong DC, Thoman R. Factors associated with medication nonadherence in patients with COPD. Chest. 2005;128(5):3198–3204. doi: 10.1378/chest.128.5.3198. [DOI] [PubMed] [Google Scholar]
- 90.Leidy NK. Functional performance in people with chronic obstructive pulmonary disease. Image J Nurs Sch. 1995;27(1):23–34. doi: 10.1111/j.1547-5069.1995.tb00809.x. [DOI] [PubMed] [Google Scholar]
- 91.Wagena EJ, Kant I, Huibers MJ, et al. Psychological distress and depressed mood in employees with asthma, chronic bronchitis or emphysema: a population-based observational study on prevalence and the relationship with smoking cigarettes. Eur J Epidemiol. 2004;19(2):147–153. doi: 10.1023/b:ejep.0000017825.07470.41. [DOI] [PubMed] [Google Scholar]
- 92.Post L, Collins C. The poorly coping COPD patient: a psychotherapeutic perspective. Int J Psychiatry Med. 11(2):1981–1982. 173–182. doi: 10.2190/vuvv-2rqv-ag30-dpl1. [DOI] [PubMed] [Google Scholar]
- 93.Cleland JA, Lee AJ, Hall S. Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Fam Pract. 2007;24(3):217–223. doi: 10.1093/fampra/cmm009. [DOI] [PubMed] [Google Scholar]
- 94.Norwood RJ. A review of etiologies of depression in COPD. Int J Chron Obstruct Pulmon Dis. 2007;2(4):485–491. [PMC free article] [PubMed] [Google Scholar]
- 95.Schmidt NB, Telch MJ, Jaimez TL. Biological challenge manipulation of PCO2 levels: a test of Klein’s (1993) suffocation alarm theory of panic. J Abnorm Psychol. 1996;105(3):446–454. doi: 10.1037//0021-843x.105.3.446. [DOI] [PubMed] [Google Scholar]
- 96.Ferguson DM. Comorbidity between depressive disorders and nicotine dependence in a cohort of 16 year olds. Arch Gen Psychiatry. 1996;53:1043–1047. doi: 10.1001/archpsyc.1996.01830110081010. [DOI] [PubMed] [Google Scholar]
- 97.Agle DP, Baum GL. Psychological aspects of chronic obstructive pulmonary disease. Med Clin North Am. 1977;61(4):749–758. doi: 10.1016/s0025-7125(16)31294-9. [DOI] [PubMed] [Google Scholar]
- 98.Dunlop DD, Lyons JS, Manheim LM, et al. Arthritis and heart disease as risk factors for major depression: the role of functional limitation. Med Care. 2004;42(6):502–511. doi: 10.1097/01.mlr.0000127997.51128.81. [DOI] [PubMed] [Google Scholar]
- 99.Cooper CB. Determining the role of exercise in patients with chronic pulmonary disease. Med Sci Sports Exerc. 1995;27:147–157. [PubMed] [Google Scholar]
- 100.van Dijk EJ, Vermeer SE, de Groot JC, et al. Arterial oxygen saturation, COPD, and cerebral small vessel disease. J Neurol Neurosurg Psychiatry. 2004;75:733–736. doi: 10.1136/jnnp.2003.022012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Campbell JJ, 3rd, Coffey CE. Neuropsychiatric significance of sub-cortical hyperintensity. J Neuropsychiatry Clin Neurosci. 2001;13:261–288. doi: 10.1176/jnp.13.2.261. [DOI] [PubMed] [Google Scholar]
- 102.El-Ad B, Lavie P. Effect of sleep apnea on cognition and mood. Int Rev Psychiatry. 2005;17(4):277–282. doi: 10.1080/09540260500104508. [DOI] [PubMed] [Google Scholar]
- 103.Ozge C, Ozge A, Unal O. Cognitive and functional deterioration in patients with severe COPD. Behav Neurol. 2006;17(2):121–130. doi: 10.1155/2006/848607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Aloia MS, Arnedt JT, Davis JD, et al. Neuropsychological sequelae of obstructive sleep apnea-hypopnea syndrome: a critical review. J Int Neuropsychol Soc. 2004;10:772–785. doi: 10.1017/S1355617704105134. [DOI] [PubMed] [Google Scholar]
- 105.Figiel GS, Krishnan KR, Doraiswamy PM, et al. Subcortical hyperintensities on brain magnetic resonance imaging: a comparison between late age onset and early onset elderly depressed subjects. Neurobiol Aging. 1991;12:245–247. doi: 10.1016/0197-4580(91)90104-r. [DOI] [PubMed] [Google Scholar]
- 106.Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33:1165–1185. doi: 10.1183/09031936.00128008. [DOI] [PubMed] [Google Scholar]
- 107.Nussbaumer-Ochsner Y, Rabe KF. Systemic manifestations of COPD. Chest. 2011;139(1):165–173. doi: 10.1378/chest.10-1252. [DOI] [PubMed] [Google Scholar]
- 108.Eagan TM, Ueland T, Wagner PD, et al. Systemic inflammatory markers in COPD: results from the Bergen COPD Cohort Study. Eur Respir J. 2010;35:540–548. doi: 10.1183/09031936.00088209. [DOI] [PubMed] [Google Scholar]
- 109.Anisman H, Merali Z, Hayley S. Neurotransmitter, peptide and cytokine processes in relation to depressive disorder: comorbidity between depression and neurodegenerative disorders. Prog Neurobiol. 2008;85:1–74. doi: 10.1016/j.pneurobio.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 110.Bemt L, Schermer T, Bor H. The risk for depression comorbidity in patients with COPD. Chest. 2009;135(1):108–111. doi: 10.1378/chest.08-0965. [DOI] [PubMed] [Google Scholar]
- 111.Gift AG, Wood RM, Cahill CA. Depression, somatization and steroid use in chronic obstructive pulmonary disease. Int J Nurs Stud. 1989;26:281–286. doi: 10.1016/0020-7489(89)90009-6. [DOI] [PubMed] [Google Scholar]
- 112.Cafarella PA, Effing TW, Usmani ZA. Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: a literature review. Respirology. 2012;17(4):627–638. doi: 10.1111/j.1440-1843.2012.02148.x. [DOI] [PubMed] [Google Scholar]
- 113.National Institute for Health and Care Excellence . Depression in Adults with a Chronic Physical Health Problem. Treatment and Management. London, UK: National Institute for Health and Care Excellence; 2009. [Accessed December 21, 2015]. Available from: http://www.nice.org.uk/guidance/cg91. [Google Scholar]
- 114.da Costa Santos CM, de Mattos Pimenta CA, Nobre MR. The PICO strategy for the research question construction and evidence search. Rev Lat Am Enfermagem. 2007;15(3):508–511. doi: 10.1590/s0104-11692007000300023. [DOI] [PubMed] [Google Scholar]
- 115.O’Connor D, Green S, Higgins JPT. Defining the review question and developing criteria for including studies. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.0.0. London, UK: The Cochrane Collaboration; [Accessed December 21, 2015]. Updated February 2008. Available from: http://www.cochrane-handbook.org/ [Google Scholar]
- 116.Critical Appraisal Skills Programme Critical Appraisal Skills Programme: Making Sense Of Evidence. Secondary Critical Appraisal Skills Programme: Making Sense Of Evidence. 2013. [Accessed December 21, 2015]. Available from: http://www.casp-uk.net/
- 117.National Institute for Health and Clinical Excellence Depression. The treatment and management of depression in adults This is a partial update of NICE clinical guideline 23. NICE clinical guideline 90. Oct, 2009. [Accessed January 9, 2016]. Available from: https://www.nice.org.uk/guidance/cg90.
- 118.Yohannes AM. Management of anxiety and depression in patients with COPD. Expert Rev Respir Med. 2008;2:337–347. doi: 10.1586/17476348.2.3.337. [DOI] [PubMed] [Google Scholar]
- 119.Xu W, Collet JP, Shapiro S, et al. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med. 2008;178:913–920. doi: 10.1164/rccm.200804-619OC. [DOI] [PubMed] [Google Scholar]
- 120.Koenig HG. Predictors of depression outcomes in medical inpatients with chronic pulmonary disease. Am J Geriatr Psychiatry. 2006;14:939–948. doi: 10.1097/01.JGP.0000206380.57732.54. [DOI] [PubMed] [Google Scholar]
- 121.Kunik ME, Roundy K, Veazey C, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127:1205–1211. doi: 10.1378/chest.127.4.1205. [DOI] [PubMed] [Google Scholar]
- 122.Cicutto LC, Brooks D. Self-care approaches to managing chronic obstructive pulmonary disease: a provincial survey. Respir Med. 2006;100:1540–1546. doi: 10.1016/j.rmed.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 123.Covino NA, Dirks JF, Kinsman RA, et al. Patterns of depression in chronic illness. Psychother Psychosom. 1982;37:144–153. doi: 10.1159/000287567. [DOI] [PubMed] [Google Scholar]
- 124.Coffey CE, Figiel GS, Djang WT, et al. Leukoencephalopathy in elderly depressed patients referred for ECT. Biol Psychiatry. 1988;24:143–161. doi: 10.1016/0006-3223(88)90270-3. [DOI] [PubMed] [Google Scholar]
- 125.Hickie I, Scott E, Mitchell P, et al. Subcortical hyperintensities on magnetic resonance imaging: clinical correlates and prognostic significance in patients with severe depression. Biol Psychiatry. 1995;37:151–160. doi: 10.1016/0006-3223(94)00174-2. [DOI] [PubMed] [Google Scholar]
- 126.Krishnan KR, Hays JC, Tupler LA, et al. Clinical and phenomenological comparisons of late-onset and early-onset depression. Am J Psychiatry. 1995;152:785–788. doi: 10.1176/ajp.152.5.785. [DOI] [PubMed] [Google Scholar]
- 127.Krishnan KR, Hays JC, Blazer DG. MRI-defined vascular depression. Am J Psychiatry. 1997;154:497–501. doi: 10.1176/ajp.154.4.497. [DOI] [PubMed] [Google Scholar]
- 128.Fujikawa T, Yamawaki S, Touhouda Y. Background factors and clinical symptoms of major depression with silent cerebral infarction. Stroke. 1994;25:798–801. doi: 10.1161/01.str.25.4.798. [DOI] [PubMed] [Google Scholar]
- 129.Covey LS, Glassman AH, Stetner F. Major depression following smoking cessation. Am J Psychiatry. 1997;154(2):263–265. doi: 10.1176/ajp.154.2.263. [DOI] [PubMed] [Google Scholar]
- 130.Covey LS. Tobacco cessation among patients with depression. Prim Care. 1999;26(3):691–706. doi: 10.1016/s0095-4543(05)70124-x. [DOI] [PubMed] [Google Scholar]
- 131.Hillas G, Perlikos F, Tsiligianni I, et al. Managing comorbidities in COPD. International Journal of COPD. 2015;10:95–109. doi: 10.2147/COPD.S54473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Nelson DR. The cytochrome p450 homepage. Hum Genomics. 2009;4:59–65. doi: 10.1186/1479-7364-4-1-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Steen SN. The effects of psychotropic drugs on respiration. Pharmacol Ther B. 1976;2:717–741. doi: 10.1016/0306-039x(76)90075-1. [DOI] [PubMed] [Google Scholar]
- 134.Man GCW, Hsu K, Spoule BJ, et al. Effect of alprazolam on exercise and dyspnea in patients with chronic obstructive pulmonary disease. Chest. 1986;90:832–836. doi: 10.1378/chest.90.6.832. [DOI] [PubMed] [Google Scholar]
- 135.Halvorsen T, Martinussen PE. Benzodiazepine use in COPD: empirical evidence from Norway. Int J Chron Obstruct Pulmon Dis. 2015;10:1695–1702. doi: 10.2147/COPD.S83107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ekström MP, Bornefalk-Hermansson A, Abernethy AP, et al. Safety of benzodiazepines and opioids in very severe respiratory disease: national prospective study. BMJ. 2014;348:g445. doi: 10.1136/bmj.g445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Borson S, McDonald GJ, Gayle T, et al. Improvement in mood, physical symptoms, and function with nortriptyline for depression in patients with chronic obstructive pulmonary disease. Psychosomatics. 1992;33:190–201. doi: 10.1016/S0033-3182(92)71995-1. [DOI] [PubMed] [Google Scholar]
- 138.Light RW, Merrill EJ, Despars J, et al. Doxepin treatment of depressed patients with chronic obstructive pulmonary disease. Arch Intern Med. 1986;146:1377–1380. [PubMed] [Google Scholar]
- 139.Ström K, Boman G, Pehrsson K, et al. Effect of protriptyline, 10 mg daily, on chronic hypoxaemia in chronic obstructive pulmonary disease. Eur Respir J. 1995;8:425–429. doi: 10.1183/09031936.95.08030425. [DOI] [PubMed] [Google Scholar]
- 140.Gordon GH, Michiels TM, Mahutte CK, et al. Effect of desipra-mine on control of ventilation and depression scores in patients with severe chronic obstructive pulmonary disease. Psychiatry Res. 1985;15:25–32. doi: 10.1016/0165-1781(85)90036-8. [DOI] [PubMed] [Google Scholar]
- 141.Sharma TN, Goyal RL, Gupta PR, et al. Psychiatric disorders in COPD with special reference to the usefulness of imipramine–diazepam combination. Indian J Chest Dis Allied Sci. 1988;30:263–268. [PubMed] [Google Scholar]
- 142.Borson S, Claypoole K, McDonald GL. Depression and chronic obstructive pulmonary disease: treatment trials. Semin Clin Neuropsychiatry. 1998;3:115–130. [PubMed] [Google Scholar]
- 143.Yohannes AM, Connolly MJ, Baldwin RC. A feasibility study of antidepressant drug therapy in depressed elderly patients with chronic obstructive pulmonary disease. Int J Geriatr Psychiatry. 2001;16:451–454. doi: 10.1002/gps.461. [DOI] [PubMed] [Google Scholar]
- 144.Eiser N, Harte R, Spiros K. Effect of treating depression on quality-of-life and exercise tolerance in severe COPD. COPD. 2005;2:233–241. [PubMed] [Google Scholar]
- 145.Papp LA, Weiss JR, Greenberg HE, et al. Sertraline for chronic obstructive pulmonary disease and comorbid anxiety and mood disorders. Am J Psychiatry. 1995;152:1531. doi: 10.1176/ajp.152.10.1531a. [DOI] [PubMed] [Google Scholar]
- 146.Smoller JW, Pollack MH, Systrom D, et al. Sertraline effects on dyspnea in patients with obstructive airways disease. Psychosomatics. 1998;39:24–29. doi: 10.1016/S0033-3182(98)71377-5. [DOI] [PubMed] [Google Scholar]
- 147.Lacasse Y, Beaudoin L, Rousseau L, et al. Randomized trial of paroxetine in end-stage COPD. Monaldi Arch Chest Dis. 2004;61:140–147. doi: 10.4081/monaldi.2004.692. [DOI] [PubMed] [Google Scholar]
- 148.Evans M, Hammond M, Wilson K, et al. Placebo controlled treatment trial of depression in elderly physically ill patients. Int J Geriatr Psychiatry. 1997;12:817–824. doi: 10.1002/(sici)1099-1166(199708)12:8<817::aid-gps645>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 149.Silvertooth EJ, Doraiswamy PM, Clary GL, et al. Citalopram and quality of life in lung transplant recipients. Psychosomatics. 2004;45:171–272. doi: 10.1176/appi.psy.45.3.271. [DOI] [PubMed] [Google Scholar]
- 150.Hegerl U, Mergl R. Depression and suicidality in COPD: understandable reaction or independent disorders? Eur Respir J. 2014;44(3):734–743. doi: 10.1183/09031936.00193213. [DOI] [PubMed] [Google Scholar]
- 151.Voekel M, Voelkel NF, MacNee W. Chronic Obstructive Lung Diseases 2. Psychosocial Aspects of Chronic Obstructive Pulmonary Disease. Hamilton, ON: B.C. Decker Inc; 2008. [Google Scholar]
- 152.Brenes GA. Anxiety and chronic obstructive pulmonary disease: prevalence, impact, and treatment. Psychosom Med. 2003;65:963–970. doi: 10.1097/01.psy.0000097339.75789.81. [DOI] [PubMed] [Google Scholar]
- 153.Argyropoulou P, Patakas D, Koukou A, et al. Buspirone effect on breathlessness and exercise performance in patients with chronic obstructive pulmonary disease. Respiration. 1993;60:216–220. doi: 10.1159/000196202. [DOI] [PubMed] [Google Scholar]
- 154.Singh NP, Despars JA, Stansbury DW, et al. Effects of buspirone on anxiety levels and exercise tolerance in patients with chronic airflow obstruction and mild anxiety. Chest. 1993;103:800–804. doi: 10.1378/chest.103.3.800. [DOI] [PubMed] [Google Scholar]
- 155.Usmani ZA, Carson KV, Cheng J, et al. Pharmacological interventions for the treatment of anxiety disorders in chronic obstructive pulmonary disease (Review) Cochrane Database Syst Rev. 2011;(11):CD008483. doi: 10.1002/14651858.CD008483.pub2. [DOI] [PubMed] [Google Scholar]
- 156.Subbe C, Collier GM, Bedson E, et al. ISRCTN41544517: Pilot Study to Examine the Effect of Citalopram on Health Status, Anxiety and Depression in Patients with Chronic Obstructive Pulmonary Disease. 2004. [Accessed December 21, 2015]. Available from: www.controlled-trials.com.
- 157.Yohannes AM, Connolly MJ. Do antidepressants work in patients with chronic obstructive pulmonary disease with comorbid depression? Expert Rev Respir Med. 2011;5(6):727–729. doi: 10.1586/ers.11.70. [DOI] [PubMed] [Google Scholar]
- 158.Wilson I. Depression in the patient with COPD. Int J Chron Obstruct Pulmon Dis. 2006;1(1):61–64. doi: 10.2147/copd.2006.1.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Yohannes AM, Alexopoulos GS. Pharmacologic treatment of depression in older patients with COPD: impact on the course of the disease and health outcomes. Drugs Aging. 2014;31(7):483–492. doi: 10.1007/s40266-014-0186-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bourbeau J, Nault D, Borycki E. Comprehensive Management of Chronic Obstructive Pulmonary Disease. Hamilton, ON: B.C. Decker Inc; 2002. [Google Scholar]
- 161.McHugh RK, Whitton SW, Peckham AD, et al. Patient preference for psychological vs pharmacologic treatment of psychiatric disorders: a meta-analytic review. J Clin Psychiatry. 2013;74(6):595–602. doi: 10.4088/JCP.12r07757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.National Institute for Health and Clinical Excellence . NICE Clinical Guideline 22 Anxiety (Amended): Management of Anxiety (Panic Disorder, With or Without Agoraphobia, and Generalized Anxiety Disorder) in Adults in Primary, Secondary or Community Care. London, UK: National Institute for Health and Clinical Excellence; 2007. [Accessed January 9, 2016]. Available from: https://www.nice.org.uk/guidance/cg22. [Google Scholar]
- 163.National Institute for Health and Clinical Excellence . CG91 Depression with a Chronic Physical Health Problem: NICE Guideline. London, UK: National Collaborating Centre for Mental Health; 2009. [Accessed January 9, 2016]. Available from: https://www.nice.org.uk/guidance/cg91. [Google Scholar]
- 164.Beck AT, Rush AJ, Shaw BF, et al. Cognitive Therapy for Depression. New York, NY: Guildford Press; 1979. [Google Scholar]
- 165.Heslop K, De Soyza A, Baker CR, Stenton C, Burns GP. Using individualized cognitive behavioral therapy as a treatment for people with COPD. Nurs Times. 2009;105:14–17. [PubMed] [Google Scholar]
- 166.Kraus CA, Kunik ME, Stanley MA. Use of cognitive behavioral therapy in late-life psychiatric disorders. Geriatrics. 2007;62:21–26. [PubMed] [Google Scholar]
- 167.Lightner E. Effect of individual cognitive behavioral therapy on depression and anxiety in older adults with chronic obstructive pulmonary disease: a feasibility study. Psychology Dissertations. 2010. [Accessed December 21, 2015]. Paper 81. Available from: http://digitalcommons.pcom.edu/psychology_dissertations/81.
- 168.Ekers D, Richards D, Gilbody S. A meta-analysis of randomized trials of behavioural treatment of depression. Psychol Med. 2008;38:611–623. doi: 10.1017/S0033291707001614. [DOI] [PubMed] [Google Scholar]
- 169.Hynninen M, Bjerke N, Pallesen S, et al. A randomized controlled trial of cognitive behavioral therapy for anxiety and depression in COPD. Respir Med. 2010;104:986–994. doi: 10.1016/j.rmed.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 170.Kunik ME, Braun U, Stanley MA, et al. One session cognitive behavioural therapy for elderly patients with chronic obstructive pulmonary disease. Psychol Med. 2001;31:717–723. doi: 10.1017/s0033291701003890. [DOI] [PubMed] [Google Scholar]
- 171.Smith SMS, Sonego S, Ketcheson L, et al. A review of the effectiveness of psychological interventions used for anxiety and depression in chronic obstructive pulmonary disease. BMJ Open Respir Res. 2014;1:e000042. doi: 10.1136/bmjresp-2014-000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Coventry PA, Gellatly JL. Improving outcomes for COPD patients with mild-to-moderate anxiety and depression: a systematic review of cognitive behavioural therapy. Br J Health Psychol. 2008;13:381–400. doi: 10.1348/135910707X203723. [DOI] [PubMed] [Google Scholar]
- 173.Yalom ID, Leszcz M. The Theory and Practice of Group Psychotherapy. 5th ed. New York, NY: Basic Books; 2005. p. XII. [Google Scholar]
- 174.Butler T, Fuhriman A. Curative factors in group therapy: a review of the recent literature. Small Group Res. 1983;14:131–142. [Google Scholar]
- 175.Vickers A, Zollman C. ABC of complementary medicine. Hypnosis and relaxation therapies. BMJ. 1999;319:1346–1349. doi: 10.1136/bmj.319.7221.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Volpato E, Banfi P, Roger SM, et al. Relaxation techniques for people with chronic obstructive pulmonary disease: a systematic review and a meta-analysis. Evid Based Complement Alternat Med. 2015;2015:628365. doi: 10.1155/2015/628365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Benson H, Beary JF, Carol MP. The relaxation response. Psychiatry. 1974;37:37–46. doi: 10.1080/00332747.1974.11023785. [DOI] [PubMed] [Google Scholar]
- 178.Devine EC, Pearcy J. Meta-analysis of the effects of psychoeducational care in adults with chronic obstructive pulmonary disease. Patient Educ Couns. 1996;29:167–178. doi: 10.1016/0738-3991(96)00862-2. [DOI] [PubMed] [Google Scholar]
- 179.Lolak S, Connors GL, Sheridan MJ, et al. Effects of progressive muscle relaxation training on anxiety and depression in patients enrolled in an outpatient pulmonary rehabilitation program. Psychother Psychosom. 2008;77:119–125. doi: 10.1159/000112889. [DOI] [PubMed] [Google Scholar]
- 180.Yeh GY, Roberts DH, Wayne PM, et al. Tai chi exercise for patients with chronic obstructive pulmonary disease: a pilot study. Respir Care. 2010;55:1475–1482. [PMC free article] [PubMed] [Google Scholar]
- 181.Donesky-Cuenco D, Nguyen HQ, Paul S, et al. Yoga therapy decreases dyspnea-related distress and improves functional performance in people with chronic obstructive pulmonary disease: a pilot study. J Altern Complement Med. 2009;15:225–234. doi: 10.1089/acm.2008.0389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Lord VM, Cave P, Hume VJ, et al. Singing teaching as a therapy for chronic respiratory disease – a randomised controlled trial and qualitative evaluation. BMC Pulm Med. 2010;10:41. doi: 10.1186/1471-2466-10-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lord VM, Hume VJ, Kelly JL, et al. Singing classes for chronic obstructive pulmonary disease: a randomized controlled trial. BMC Pulm Med. 2012;12:69. doi: 10.1186/1471-2466-12-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Bonilha AG, Onofre F, Vieira ML, et al. Effects of singing classes on pulmonary function and quality of life of COPD patients. Int J Chron Obstruct Pulmon Dis. 2009;4:1–8. [PMC free article] [PubMed] [Google Scholar]
- 185.Pumar MI, Gray CR, Walsh JR, et al. Anxiety and depression – important psychological comorbidities of COPD. J Thorac Dis. 2014;6(11):1615–1631. doi: 10.3978/j.issn.2072-1439.2014.09.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Nici L, Donner C, Wouters E, et al. ATS/ERS Pulmonary Rehabilitation Writing Committee American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173:1390–1414. doi: 10.1164/rccm.200508-1211ST. [DOI] [PubMed] [Google Scholar]
- 187.Richard Z. The nonpharmacologic treatment of chronic obstructive pulmonary disease. Advances in our understanding of pulmonary rehabilitation. Proc Am Thorac Soc. 2007;4(7):549–553. doi: 10.1513/pats.200701-015FM. [DOI] [PubMed] [Google Scholar]
- 188.Stockley RA. Chronic Obstructive Pulmonary Disease. Oxford, UK: Blackwell Publishing Ltd; 2007. [Google Scholar]
- 189.Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):1011–1027. doi: 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 190.Goldstein RS, Gort EH, Stubbing D, et al. Randomised controlled trial of respiratory rehabilitation. Lancet. 1994;344:1394–1397. doi: 10.1016/s0140-6736(94)90568-1. [DOI] [PubMed] [Google Scholar]
- 191.Griffiths TL, Burr ML, Campbell IA, et al. Results at 1 year of outpatient multidisciplinary pulmonary rehabilitation: a randomised controlled trial. Lancet. 2000;355:362–368. doi: 10.1016/s0140-6736(99)07042-7. [DOI] [PubMed] [Google Scholar]
- 192.Mota S, Güell R, Barreiro E, et al. Clinical outcomes of expiratory muscle training in severe COPD patients. Respir Med. 2007;101(3):516–524. doi: 10.1016/j.rmed.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 193.Emery CF, Shermer RL, Hauck ER, et al. Cognitive and psychological outcomes of exercise in a 1-year follow-up study of patients with chronic obstructive pulmonary disease. Health Psychol. 2003;22:598–604. doi: 10.1037/0278-6133.22.6.598. [DOI] [PubMed] [Google Scholar]
- 194.Kozora E, Tran ZV, Make B. Neurobehavioral improvement after brief rehabilitation in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2002;22:426–430. doi: 10.1097/00008483-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 195.Garuti G, Cilione C, Dell’Orso D, et al. Impact of comprehensive pulmonary rehabilitation on anxiety and depression in hospitalized COPD patients. Monaldi Arch Chest Dis. 2003;59:56–61. [PubMed] [Google Scholar]
- 196.Boutou AK, Tanner RJ, Lord VM, et al. An evaluation of factors associated with completion and benefit from pulmonary rehabilitation in COPD. BMJ Open Respir Res. 2014;1:e000051. doi: 10.1136/bmjresp-2014-000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Fischer MJ, Scharloo M, Abbink JJ, et al. Participation and drop-out in pulmonary rehabilitation: a qualitative analysis of the patient’s perspective. Clin Rehabil. 2007;21:212–221. doi: 10.1177/0269215506070783. [DOI] [PubMed] [Google Scholar]
- 198.Robertson N. Running up that hill: how pulmonary rehabilitation can be enhanced by understanding patient perceptions of their condition. Chron Respir Dis. 2010;7(4):203–205. doi: 10.1177/1479972310389343. [DOI] [PubMed] [Google Scholar]
- 199.Dishman RK. Brain monoamines, exercise, and behavioral stress: animal models. Med Sci Sports Exerc. 1997;29(1):63–74. doi: 10.1097/00005768-199701000-00010. [DOI] [PubMed] [Google Scholar]
- 200.Ransford CP. A role for amines in the antidepressant effect of exercise: a review. Med Sci Sports Exerc. 1982;14(1):1–10. doi: 10.1249/00005768-198201000-00001. [DOI] [PubMed] [Google Scholar]
- 201.Dunn AL, Reigle TG, Youngstedt SD, et al. Brain norepinephrine and metabolites after treadmill training and wheel running in rats. Med Sci Sports Exerc. 1996;28(2):204–209. doi: 10.1097/00005768-199602000-00008. [DOI] [PubMed] [Google Scholar]
- 202.Jacobs BL. Serotonin, motor activity and depression-related disorders. Am Sci. 1994;82:456–463. [Google Scholar]
- 203.Chaouloff F. Effects of acute exercise on central serotonergic systems. Med Sci Sports Exerc. 1997;29(1):58–62. doi: 10.1097/00005768-199701000-00009. [DOI] [PubMed] [Google Scholar]
- 204.Raglin JS, Morgan WP. Influence of exercise and quiet rest on state anxiety and blood pressure. Med Sci Sports Exerc. 1981;19(5):456–463. [PubMed] [Google Scholar]
- 205.Carr DB, Bullen BA, Skrinar GS, et al. Physical conditioning facilitates the exercise-induced secretion of beta-endorphin and beta-lipotropin in women. N Engl J Med. 1981;305(10):597–617. doi: 10.1056/NEJM198109033051006. [DOI] [PubMed] [Google Scholar]
- 206.Farrell PA, Gates WK, Maksud MG, et al. Increases in plasma beta-endorphin/beta-lipotropin immunoreactivity after treadmill running in humans. J Appl Physiol Respir Environ Exerc Physiol. 1982;52(5):1245–1249. doi: 10.1152/jappl.1982.52.5.1245. [DOI] [PubMed] [Google Scholar]
- 207.Gambert SR, Hagen TC, Garthwaite TL. Exercise and the endogenous opioids. N Engl J Med. 1981;305:1590–1591. doi: 10.1056/NEJM198112243052619. [DOI] [PubMed] [Google Scholar]
- 208.Pitsavos C, Chrysohoou C, Panagiotakos DB, et al. Association of leisure-time physical activity on inflammation markers (C-reactive protein, white cell blood count, serum amyloid A, and fibrinogen) in healthy subjects (from the ATTICA study) Am J Cardiol. 2003;91(3):368–370. doi: 10.1016/s0002-9149(02)03175-2. [DOI] [PubMed] [Google Scholar]
- 209.Church TS, Barlow CE, Earnest CP, et al. Associations between cardiorespiratory fitness and C-reactive protein in men. Arterioscler Thomb Vasc Biol. 2002;22(11):1869–1876. doi: 10.1161/01.atv.0000036611.77940.f8. [DOI] [PubMed] [Google Scholar]
- 210.Morrow J, Nolen-Hoeksema S. Effects of response to depression on the remediation of depressive affect. J Pers Soc Psychol. 1990;58(3):519–527. doi: 10.1037//0022-3514.58.3.519. [DOI] [PubMed] [Google Scholar]
- 211.Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta earthquake. J Pers Soc Psychol. 1991;61(1):115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- 212.McAuley E, Jerome GJ, Marquez DX, et al. Exercise self-efficacy in older adults: social, affective, and behavioral influences. Ann Behav Med. 2003;25(1):1–7. doi: 10.1207/S15324796ABM2501_01. [DOI] [PubMed] [Google Scholar]
- 213.Craft LL. Exercise and clinical depression: examining two psychological mechanisms. Psychol Sport Exerc. 2003;6:151–171. [Google Scholar]
- 214.Lewinsohn PM, Gotlib IH. Behavioral theory and treatment of depression. In: Beckham EE, Leber WR, editors. Handbook of Depression. 2nd ed. New York, NY: Guildford Press; 1995. pp. 352–375. [Google Scholar]
- 215.Bartoholomew JB, Ciccolo JT. Exercise, depression, and cognition. In: Spirduso WW, Poon LW, Chodzko-Zajko W, editors. Exercise and Its Mediating Effects on Cognition. Vol. 2. Champaign, IL: Human Kinetics; 2008. pp. 33–46. [Google Scholar]
- 216.Coventry PA, Hind D. Comprehensive pulmonary rehabilitation for anxiety and depression in adults with chronic obstructive pulmonary disease: systematic review and meta-analysis. J Psychosom Res. 2007;63:551–565. doi: 10.1016/j.jpsychores.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 217.Withers NJ, Rudkin ST, White RJ. Anxiety and Depression in Sever Chronic Obstructive Pulmonary Disease: The Effects of Pulmonary Rehabilitation. Bristol, UK: Department of Medicine, Frenchay Hospital; 1999. [DOI] [PubMed] [Google Scholar]
- 218.Alexopoulos GS, Kiosses DN, Sirey JA, et al. Untangling therapeutic ingredients of a personalized intervention for patients with depression and severe COPD. Am J Geriatr Psychiatry. 2014;22(11):1316–1324. doi: 10.1016/j.jagp.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Ries AL, Kaplan RM, Limberg TM, et al. Effects of pulmonary rehabilitation on physiologic and psychosocial outcomes in patients with chronic obstructive pulmonary disease. Ann Intern Med. 1995;122:823–832. doi: 10.7326/0003-4819-122-11-199506010-00003. [DOI] [PubMed] [Google Scholar]
- 220.Sassi-Dambron DE, Eakin EG, Ries AL, et al. Treatment of dyspnea in COPD: a controlled clinical trial of dyspnea management strategies. Chest. 1995;107:724–729. doi: 10.1378/chest.107.3.724. [DOI] [PubMed] [Google Scholar]
- 221.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 222.Pantou I, Harikiopoulou M, Bratis D, et al. The impact of rehabilitation-induced symptomatic, functional and psychological outcomes on health-related quality of life. European Respiratory Society, Annual Congress. September 2–6, 2006, Munich, Germany. European Respiratory Journal. 2006;28(suppl 5) Published in. [Google Scholar]
- 223.Paz-Dıaz H, Montes de Oca M, Lopez JM, et al. Pulmonary rehabilitation improves depression, anxiety, dyspnea and health status in patients with COPD. Am J Phys Med Rehabil. 2006;86(1):30–35. doi: 10.1097/phm.0b013e31802b8eca. [DOI] [PubMed] [Google Scholar]
- 224.Jácome C, Marque A. Impact of pulmonary rehabilitation in subjects with mild COPD. Respir Care. 2014;59(10):1577–1582. doi: 10.4187/respcare.03091. [DOI] [PubMed] [Google Scholar]
- 225.Alexopoulos GS, Sirey JA, Raue PJ, et al. Outcomes of depressed patients undergoing inpatient pulmonary rehabilitation. Am J Geriatr Psychiatry. 2006;14:466–475. doi: 10.1097/01.JGP.0000199381.98971.d1. [DOI] [PubMed] [Google Scholar]
- 226.Guell R, Resqueti V, Sangenis M, et al. Impact of pulmonary rehabilitation on psychosocial morbidity in patients with severe COPD. Chest. 2006;129:899–904. doi: 10.1378/chest.129.4.899. [DOI] [PubMed] [Google Scholar]
- 227.Kosmas E, Tselebis A, Bratis D, et al. Impact of pulmonary rehabilitation on anxiety and depression in patients with COPD; European Respiratory Society, Annual Congress; Berlin, Germany: 2008. [Google Scholar]
- 228.Pantou I, Harikiopoulou M, Mpletsa M, et al. Does the severity of chronic obstructive pulmonary disease reflect on the outcomes of pulmonary rehabilitation?. European Respiratory Society, Annual Congress; Stockholm: 2007. [Google Scholar]
- 229.Mignogna J, Cully JA. Depression and anxiety in patients with COPD: a focus on psychological treatments in ambulatory care settings. Curr Respir Med Rev. 2012;8:137–144. [Google Scholar]
- 230.Panagioti M, Scott C, Blakemor A, et al. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:1289–1306. doi: 10.2147/COPD.S72073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Yohannes AM, Alexopoulos GS. Depression and anxiety in patients with COPD. Eur Respir Rev. 2014;23(133):345–349. doi: 10.1183/09059180.00007813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.U.S. Preventive Services Task Force Screening for depression: recommendations and rationale. Ann Intern Med. 2002;136:760–764. doi: 10.7326/0003-4819-136-10-200205210-00012. [DOI] [PubMed] [Google Scholar]
- 233.Gilbody S, House AO, Sheldon TA. Screening and case finding instruments for depression. Cochrane Database Syst Rev. 2005;(4):CD002792. doi: 10.1002/14651858.CD002792.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Cavanaugh S, Clark DC, Gibbons RD. Diagnosing depression in the hospitalized medically ill. Psychosomatics. 1983;24:809–815. doi: 10.1016/S0033-3182(83)73151-8. [DOI] [PubMed] [Google Scholar]
- 235.Bukberg J, Penman D, Holland JC. Depression in hospitalized cancer patients. Psychosom Med. 1984;46:199–212. doi: 10.1097/00006842-198405000-00002. [DOI] [PubMed] [Google Scholar]
- 236.Endicott J. Measurement of depression in patients with cancer. Cancer. 1984;53:2243–2249. doi: 10.1002/cncr.1984.53.s10.2243. [DOI] [PubMed] [Google Scholar]
- 237.Yates WR, Mitchell J, Rush AJ, et al. Clinical features of depressed outpatients with and without co-occurring general medical conditions in STAR*D. Gen Hosp Psychiatry. 2004;26:421–429. doi: 10.1016/j.genhosppsych.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 238.Yohannes AM, Willgoss TG, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry. 2010;25:1209–1221. doi: 10.1002/gps.2463. [DOI] [PubMed] [Google Scholar]
- 239.Simon GE, Von Korff M. Medical co-morbidity and validity of DSM-IV depression criteria. Psychol Med. 2006;36:27–36. doi: 10.1017/S0033291705006136. [DOI] [PubMed] [Google Scholar]
- 240.Engstrom CP, Persson LO, Larsso S, et al. Health-related quality of life in COPD: why both disease-specific and generic measures should be used. Eur Respir J. 2001;18:69–76. doi: 10.1183/09031936.01.00044901. [DOI] [PubMed] [Google Scholar]
- 241.Alexopoulos GS, Raue PJ, Sirey JA, Arean PA. Developing an intervention for depressed, chronically medically ill elders: a model from COPD. Int J Geriatr Psychiatry. 2008;23(5):447–453. doi: 10.1002/gps.1925. [DOI] [PubMed] [Google Scholar]
- 242.Alexopoulos GS, Kiosses DN, Sirey JA, et al. Personalised intervention for people with depression and severe COPD. Br J Psychiatry. 2013;202(3):235–236. doi: 10.1192/bjp.bp.112.120139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Gilbody S, Bower P, Fletcher J, et al. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med. 2006;166:2314–2321. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- 244.Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525. doi: 10.1002/14651858.CD006525.pub2. [DOI] [PubMed] [Google Scholar]
- 245.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Coventry PA, Bower P, Keywort C, et al. The effect of complex interventions on depression and anxiety in chronic obstructive pulmonary disease: systematic review and meta-analysis. PLoS One. 2013;8(4):e60532. doi: 10.1371/journal.pone.0060532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Clark NM, Dodge JA, Partridge MR, et al. Focusing on outcomes: making the most of COPD interventions. Int J Chron Obstruct Pulmon Dis. 2009;4:61–77. [PMC free article] [PubMed] [Google Scholar]
- 248.Almagro P, Castro A. Helping COPD patients change health behavior in order to improve their quality of life. Int J Chron Obstruct Pulmon Dis. 2013;8:335–345. doi: 10.2147/COPD.S34211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Momtaz OM, Rabei SM, Tawfike NR, et al. Effect of treatment of depression and anxiety on physiological state of severe COPD patients. Egypt J Chest Dis Tuberc. 2015;64:29–34. [Google Scholar]
- 250.He Y, Zheng Y, Xu C, et al. Sertraline hydrochloride treatment for patients with stable chronic obstructive pulmonary disease complicated with depression: a randomized controlled trial. Clin Respir J. 2014 Oct 13; doi: 10.1111/crj.12219. Epub. [DOI] [PubMed] [Google Scholar]
- 251.Bove DG, Overgaard D, Lomborg K, et al. Efficacy of a minimal home-based psychoeducative intervention versus usual care for managing anxiety and dyspnoea in patients with severe chronic obstructive pulmonary disease: a randomised controlled trial protocol. BMJ Open. 2015;5:e008031. doi: 10.1136/bmjopen-2015-008031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Howard C, Dupont S. The COPD breathlessness manual’: a randomised controlled trial to test a cognitive-behavioural manual versus information booklets on health service use, mood and health status, in patients with chronic obstructive pulmonary disease. NPJ Prim Care Respir Med. 2014;24:14076. doi: 10.1038/npjpcrm.2014.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Jiang X, He G. Effects of an uncertainty management intervention on uncertainty, anxiety, depression, and quality of life of chronic obstructive pulmonary disease outpatients. Res Nurs Health. 2012;35(4):409–418. doi: 10.1002/nur.21483. [DOI] [PubMed] [Google Scholar]
- 254.Kapella MC, Herdegen JJ, Perlis ML, et al. Cognitive behavioral therapy for insomnia comorbid with COPD is feasible with preliminary evidence of positive sleep and fatigue effects. Int J Chron Obstruct Pulmon Dis. 2011;6:625–635. doi: 10.2147/COPD.S24858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Livermore N, Sharpe L, McKenzie D. Prevention of panic attacks and panic disorder in COPD. Eur Respir J. 2010;35:557–563. doi: 10.1183/09031936.00060309. [DOI] [PubMed] [Google Scholar]
- 256.Lamers F, Jonkers CC, Bosma H, et al. Improving quality of life in depressed COPD patients: effectiveness of a minimal psychological intervention. COPD. 2010;7(5):315–322. doi: 10.3109/15412555.2010.510156. [DOI] [PubMed] [Google Scholar]
- 257.Kunik ME, Veazey C, Cully JA, et al. COPD education and cognitive behavioral therapy group treatment for clinically significant symptoms of depression and anxiety in COPD patients; a randomized controlled trial. Psychol Med. 2008;37:1–12. doi: 10.1017/S0033291707001687. [DOI] [PubMed] [Google Scholar]
- 258.Blumenthal JA, Babyak MA, Keefe FJ, et al. Telephone-based coping skills training for patients awaiting lung transplantation. J Consult Clin Psychol. 2006;74(3):535–544. doi: 10.1037/0022-006X.74.3.535. [DOI] [PubMed] [Google Scholar]
- 259.de Godoy DV, de Godoy RF, Becker Júnior B, et al. The effect of psychotherapy provided as part of a pulmonary rehabilitation program for the treatment of patients with chronic obstructive pulmonary disease. J Bras Pneumol. 2005;31:499–505. [Google Scholar]
- 260.de Godoy DV, de Godoy RF. A randomized controlled trial of the effect of psychotherapy on anxiety and depression in chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2003;84:1154–1157. doi: 10.1016/s0003-9993(03)00239-9. [DOI] [PubMed] [Google Scholar]
- 261.Emery CF, Schein RL, Hauck ER, et al. Psychological and cognitive outcomes of a randomized trial of exercise among patients with chronic obstructive pulmonary disease. Health Psychol. 1998;17(3):232–240. doi: 10.1037//0278-6133.17.3.232. [DOI] [PubMed] [Google Scholar]
- 262.Eiser N, West C, Evans S, et al. Effects of psychotherapy in moderately severe COPD: a pilot study. Eur Respir J. 1997;10:1581–1584. doi: 10.1183/09031936.97.10071581. [DOI] [PubMed] [Google Scholar]
- 263.Ramsenthaler C, Siegert RJ, Weatherall M, et al. Cognitive behavioural therapy (CBT) for panic and anxiety in chronic obstructive pulmonary disease – a systematic review. Palliat Med. 2012;26(6):1. [Google Scholar]
- 264.Baraniak A, Sheffield D. The efficacy of psychologically based interventions to improve anxiety, depression and quality of life in COPD: a systematic review and meta-analysis. Patient Educ Couns. 2011;83(1):29–36. doi: 10.1016/j.pec.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 265.Mkacher W, Mekki M, Chaieb F, et al. Balance training in pulmonary rehabilitation: effects on psychosocial outcomes. J Cardiopulm Rehabil Prev. 2015;35(4):278–285. doi: 10.1097/HCR.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 266.Reychler G, Mottart F2, Boland M, et al. Influence of ambient music on perceived exertion during a pulmonary rehabilitation session: a randomized crossover study. Respir Care. 2015;60(5):711–717. doi: 10.4187/respcare.03671. [DOI] [PubMed] [Google Scholar]
- 267.Kaymaz D, Ergün P, Demirci E, et al. Comparison of the effects of neuromuscular electrical stimulation and endurance training in patients with severe chronic obstructive pulmonary disease. Tuberk Toraks. 2015;63(1):1–7. doi: 10.5578/tt.8493. [DOI] [PubMed] [Google Scholar]
- 268.Valenza MC, Valenza-Pena G, Torres-Sanchez I, et al. Effectiveness of controlled breathing techniques on anxiety and depression in hospitalized patients with COPD: a randomized clinical trial. Respir Care. 2014;59(2):209–215. doi: 10.4187/respcare.02565. [DOI] [PubMed] [Google Scholar]
- 269.Leung RWM, McKeough ZJ, Peters MJ, et al. Short-form Sun-style t’ai chi as an exercise training modality in people with COPD. Eur Respir J. 2013;41(5):1051–1057. doi: 10.1183/09031936.00036912. [DOI] [PubMed] [Google Scholar]
- 270.Santana MJ, S-Parrilla J, Mirus J, et al. An assessment of the effects of Iyengar yoga practice on the health-related quality of life of patients with chronic respiratory diseases: a pilot study. Can Respir J. 2013;20(2):e17–e23. doi: 10.1155/2013/265406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Singh VP, Rao V, Prem V, Sahoo RC, Keshav Pai K. Comparison of the effectiveness of music and progressive muscle relaxation for anxiety in COPD – a randomized controlled pilot study. Chron Respir Dis. 2009;6(4):209–216. doi: 10.1177/1479972309346754. [DOI] [PubMed] [Google Scholar]
- 272.Bauldoff GS, Hoffman LA, Zullo TG, et al. Exercise maintenance following pulmonary rehabilitation: effect of distractive stimuli. Chest. 2002;122(3):948–954. doi: 10.1378/chest.122.3.948. [DOI] [PubMed] [Google Scholar]
- 273.Gift AG, Moore T, Soeken K. Relaxation to reduce dyspnea and anxiety in COPD patients. Nurs Res. 1992;41:242–246. [PubMed] [Google Scholar]
- 274.Luk EK, Khan F, Irving L. Maintaining gains following pulmonary rehabilitation. Lung. 2015;193(5):709–715. doi: 10.1007/s00408-015-9751-5. [DOI] [PubMed] [Google Scholar]
- 275.Sciriha A, Lungaro-Mifsud S, Scerri J, et al. Pulmonary rehabilitation in chronic obstructive pulmonary disease: outcomes in a 12 week programme. Eur J Physiother. 2015;17(4):1–9. [Google Scholar]
- 276.Grosbois JM, Gicquello A, Langlois C, et al. Long-term evaluation of home-based pulmonary rehabilitation in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:2037–2044. doi: 10.2147/COPD.S90534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.da Costa CC, de Azeredo LC, Colombo C, et al. Effect of a Pulmonary Rehabilitation Program on the levels of anxiety and depression and on the quality of life of patients with chronic obstructive pulmonary disease. Rev Port Pneumol. 2014;20(6):299–304. doi: 10.1016/j.rppneu.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 278.Tselebis A, Bratis D, Pachi A, et al. A pulmonary rehabilitation program reduces levels of anxiety and depression in COPD patients. Multidiscip Respir Med. 2013;8(1):41. doi: 10.1186/2049-6958-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Bhandari NJ, Jain T, Marolda C, et al. Comprehensive pulmonary rehabilitation results in clinically meaningful improvements in anxiety and depression in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2013;33(2):123–127. doi: 10.1097/HCR.0b013e31828254d4. [DOI] [PubMed] [Google Scholar]
- 280.Hogg L, Garrod R, Thornton H, et al. Effectiveness, attendance, and completion of an integrated, system-wide pulmonary rehabilitation service for COPD: prospective observational study. COPD. 2012;9(5):546–554. doi: 10.3109/15412555.2012.707258. [DOI] [PubMed] [Google Scholar]
- 281.Bentsen SB, Wentzel-Larsen T, Henriksen AH, et al. Anxiety and depression following pulmonary rehabilitation. Scand J Caring Sci. 2013;27(3):541–550. doi: 10.1111/j.1471-6712.2012.01064.x. [DOI] [PubMed] [Google Scholar]
- 282.Harrison SL, Greening NJ, Williams JE, et al. Have we underestimated the efficacy of pulmonary rehabilitation in improving mood? Respir Med. 2012;106(6):838–844. doi: 10.1016/j.rmed.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 283.Bratås O, Espnes GA, Rannestad T, et al. Relapse of health related quality of life and psychological health in patients with chronic obstructive pulmonary disease 6 months after rehabilitation. Scand J Caring Sci. 2012;26(2):219–227. doi: 10.1111/j.1471-6712.2011.00921.x. [DOI] [PubMed] [Google Scholar]
- 284.von Leupoldt A, Taube K, Lehmann K, et al. The impact of anxiety and depression on outcomes of pulmonary rehabilitation in patients with COPD. Chest. 2011;140(3):730–736. doi: 10.1378/chest.10-2917. [DOI] [PubMed] [Google Scholar]
- 285.Pirraglia PA, Casserly B, Velasco R, et al. Association of change in depression and anxiety symptoms with functional outcomes in pulmonary rehabilitation patients. J Psychosom Res. 2011;71(1):45–49. doi: 10.1016/j.jpsychores.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 286.Bratås O, Espnes GA, Rannestad T, et al. Pulmonary rehabilitation reduces depression and enhances health-related quality of life in COPD patients – especially in patients with mild or moderate disease. Chron Respir Dis. 2010;7(4):229–237. doi: 10.1177/1479972310374343. [DOI] [PubMed] [Google Scholar]
- 287.Spencer LM, Alison JA, McKeough ZJ. Do supervised weekly exercise programs maintain functional exercise capacity and quality of life, twelve months after pulmonary rehabilitation in COPD? BMC Pulm Med. 2007;7:7. doi: 10.1186/1471-2466-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Ozdemir EP, Solak O, Fidan F, et al. The effect of water-based pulmonary rehabilitation on anxiety and quality of life in chronic pulmonary obstructive disease patients. Turk Klin J Med Sci. 2010;30(3):880–887. [Google Scholar]
- 289.Godoy RF, Teixeira PJ, Becker Júnior B, et al. Long-term repercussions of a pulmonary rehabilitation program on the indices of anxiety, depression, quality of life and physical performance in patients with COPD. J Bras Pneumol. 2009;35(2):129–136. doi: 10.1590/s1806-37132009000200005. [DOI] [PubMed] [Google Scholar]
- 290.Elçi A, Börekçi S, Ovayolu N, et al. The efficacy and applicability of a pulmonary rehabilitation programme for patients with COPD in a secondary-care community hospital. Respirology. 2008;13(5):703–707. doi: 10.1111/j.1440-1843.2008.01327.x. [DOI] [PubMed] [Google Scholar]
- 291.Kayahan B, Karapolat H, Atýntoprak E, et al. Psychological outcomes of an outpatient pulmonary rehabilitation program in patients with chronic obstructive pulmonary disease. Respir Med. 2006;100(6):1050–1057. doi: 10.1016/j.rmed.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 292.Arnardóttir RH, Boman G, Larsson K, et al. Interval training compared with continuous training in patients with COPD. Respir Med. 2007;101(6):1196–204. doi: 10.1016/j.rmed.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 293.Goldberg R, Hillberg R, Reinecker L, et al. Evaluation of patients with severe pulmonary disease before and after pulmonary rehabilitation. Disabil Rehabil. 2004;26(11):641–648. doi: 10.1080/09638280410001663120. [DOI] [PubMed] [Google Scholar]
- 294.Trappenburg JC, Troosters T, Spruit MA, et al. Psychosocial conditions do not affect short-term outcome of multidisciplinary rehabilitation in chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2005;86(9):1788–1792. doi: 10.1016/j.apmr.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 295.Cilione C, Lorenzi C, Dell Orso D, et al. Predictors of change in exercise capacity after comprehensive COPD inpatient rehabilitation. Med Sci Monit. 2002;8(11):CR740–CR745. [PubMed] [Google Scholar]
- 296.White RJ, Rudkin ST, Harrison ST, et al. Pulmonary rehabilitation compared with brief advice given for severe chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2002;22:338–344. doi: 10.1097/00008483-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 297.Emery CF, Leatherman NE, Burker EJ, et al. Psychological outcomes of a pulmonary rehabilitation program. Chest. 1991;100:613–617. doi: 10.1378/chest.100.3.613. [DOI] [PubMed] [Google Scholar]
- 298.Dekhuijzen PN, Beek MM, Folgering HT, et al. Psychological changes during pulmonary rehabilitation and target-flow inspiratory muscle training in COPD patients with a ventilatory limitation during exercise. Int J Rehabil Res. 1990;13(2):109–117. doi: 10.1097/00004356-199006000-00002. [DOI] [PubMed] [Google Scholar]
- 299.Wiles L, Cafarella P, Williams MT. Exercise training combined with psychological interventions for people with chronic obstructive pulmonary disease. Respirology. 2015;20(1):46–55. doi: 10.1111/resp.12419. [DOI] [PubMed] [Google Scholar]
- 300.Scottish Intercollegiate Guidelines Network Critical Appraisal: Notes and Checklists. Secondary Critical Appraisal: Notes and Checklists. 2014. [Accessed December 21, 2015]. Available from: http://www.sign.ac.uk/methodology/checklists.html.