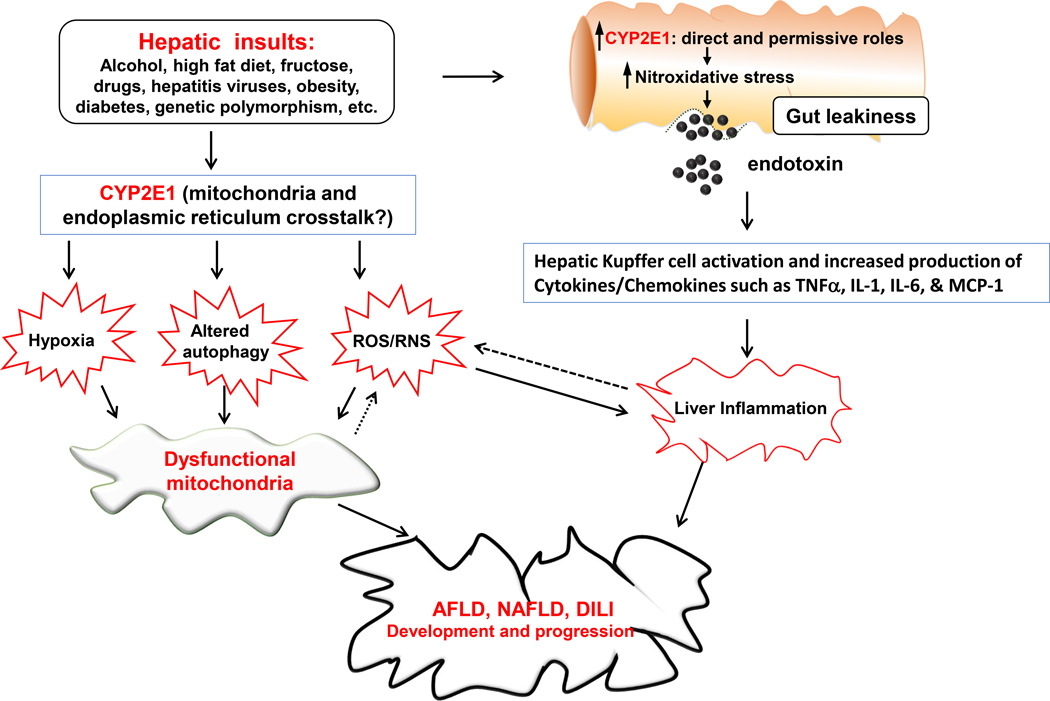
Fig. 1. Proposed mechanisms of mitochondrial dysfunction, contributing to hepatotoxicity in AFLD, NAFLD and DILI.
Various hepatic insults including alcohol (ethanol), high fat diet, fructose, drugs, hepatitis virus, obesity, diabetes, genetic polymorphism as indicated in the Figure can negatively affect the liver by promoting ER stress and mitochondria dysfunction, contributing to fat accumulation and inflammatory liver injury in AFLD, NAFLD and DILI. These negative effects are largely mediated through increased ROS/RNS production, increased hypoxia and altered autophagy by the direct and/or permissive roles of CYP2E1, as discussed in the text. These agents or conditions can also upregulate intestinal CYP2E1 and promote gut leakiness through increased nitroxidative stress, contributing to endotoxemia and more severe inflammatory liver injury via activation of Kupffer cells and the production of cytokines/chemokines, which can also increase ROS/RNS production, resulting in a viscous cycle between inflammation and oxidative stress. Ultimately, this change in the redox state combined with the increased production of ROS/RNS promote the development and progression of mitochondrial dysfunction and various hepatic diseases. Uni-directional and bi-directional arrows indicate exclusive and mutual influences, respectively.