Abstract
Nasopharyngeal carcinoma (NPC) is a highly invasive malignancy with cervical lymphopathy as the initial presentation. Epithelial-mesenchymal transition (EMT), a process by which epithelial cells lose cell-cell adhesion and gain migratory and invasive properties, has a pivotal role in metastasis. Forkhead box C1 (FoxC1), a member of the forkhead family of transcription factors, induces EMT and has a critical role in metastasis of multiple human cancers. However, the role of FoxC1 in the progression of NPC has remained elusive. The present study revealed that the expression of FoxC1 was markedly elevated in NPC tissues compared with that in chronically inflamed nasopharyngeal tissues and was closely correlated with vimentin, fibronectin and N-cadherin expression as indicated by immunohisto-chemical assays. In addition, high FoxC1 expression was positively associated with lymph node metastasis, distant metastasis and an advanced clinical stage in patients with NPC. Furthermore, FoxC1 expression was high in NPC cell lines while being low in an immortalized normal nasopharyngeal epithelial cell line. In vitro, knockdown of FoxC1 in the CNE2 human NPC cell line by small interfering RNA downregulated vimentin, fibronectin and N-cadherin expression and reduced the migratory and invasive capacity of CNE2 cells. In conclusion, the present study indicated that FoxC1 has a pivotal role in EMT through the upregulation of vimentin, fibronectin and N-cadherin expression. Thus, FoxC1 may be a potential therapeutic target in NPC.
Keywords: forkhead box C1, epithelial-mesenchymal transition nasopharyngeal carcinoma, metastasis
Introduction
Nasopharyngeal carcinoma (NPC) is an endemic disease and a significant health problem in southern China and south-eastern Asia (1,2). The etiology of NPC includes virological, genetic and environmental factors (3). NPC is radiation-sensitive and chemo-sensitive (4); however for patients who develop local recurrence, there is no efficient systemic remedy. Distant metastasis is the leading cause of mortality of advanced NPC patients (4,5). Epithelial-mesenchymal transition (EMT), a process by which epithelial cells lose epithelial markers and gain mesenchymal markers, endows cancer cells with migratory and invasive properties to initialize metastasis (6–8). In NPC, amongst other cancer types, the EMT was reported to be a key event involved in invasion and metastasis (9).
Forkhead box C1 (FoxC1), a member of the forkhead transcription factor family, was reported to be a regulator of the EMT (10). It is well known that FoxC1 has an important role in embryonic and ocular development (11,12). Recently, accumulating evidence showed that FoxC1 was overexpressed and correlated with metastasis and poor prognosis in several cancer types, including breast cancer, hepatocellular carcinoma, pancreatic ductal adenocarcinoma, Hodgkin lymphoma and lung cancer (13–17). Indeed, FoxC1 induced EMT cells by downregulating E-cadherin to promote cell migration and aggressiveness in breast cancer and hepatocelluar carcinoma (10,18–20).
To date, no studies have investigated the clinicopathological significance of FoxC1 and its role in the EMT in NPC. The present study examined NPC tissues and NPC cell lines as well as chronically inflamed nasopharyngeal tissue specimens and an immortalized normal nasopharyngeal epithelial cell line for the expression of FoxC1. In addition, a correlation study was performed to assess the association of FoxC1 with clinicopathological characteristics and the expression of mesenchymal markers in NPC. Furthermore, the role of FoxC1's role in the EMT of NPC was investigated in vitro.
Materials and methods
Tissue specimens
All NPC and chronically inflamed nasopharyngeal tissue specimens were collected from the Affiliated Hospital of Guilin Medical University (Guilin, China) between May 2011, and February 2013. The study protocol was approved by the research ethics committee of the Affiliated Hospital of Guilin Medical University (Guilin, China) and written informed consent was obtained from each patient. All samples were pathologically re-assessed by two pathologists, and the percentage of tumor cells was ≥70% in all NPC specimens. None of the patients had received radiotherapy or chemotherapy prior to biopsy sampling (21). 93 NPC tissue specimens with complete clinical data and 33 NP specimens were collected for constructing tissue microarrays and subjected to further study. The clinicopathological characteristics of the patients are listed in Table I. Clinical staging was performed according to the tumor-nodes-metastasis (TNM) classification system of the International Union Against Cancer staging system (22).
Table I.
Correlation between clinicopathological features and expression of FoxC1 in patients with nasopharyngeal carcinoma.
| Variable | n | FoxC1 expression
|
χ2 | P-value | |
|---|---|---|---|---|---|
| Low (n, %) | High (n, %) | ||||
| Gender | 0.003 | 0.573 | |||
| Female | 23 | 13 (56.5) | 10 (43.5) | ||
| Male | 70 | 40 (57.1) | 30 (42.9) | ||
| Age (years) | 2.155 | 0.104 | |||
| <50 | 50 | 25 (50.0) | 25 (50.0) | ||
| ≥50 | 43 | 28 (65.1) | 15 (34.9) | ||
| Histological type | 0.041 | 0.558 | |||
| DNKC | 10 | 6 (60.0) | 4 (40.0) | ||
| UDC | 83 | 47 (56.6) | 36 (43.4) | ||
| T classification | 30.233 | 0.000 | |||
| T1-T2 | 42 | 37 (88.1) | 5 (11.9) | ||
| T3-T4 | 51 | 16 (31.4) | 35 (68.6) | ||
| N classification | 6.012 | 0.012 | |||
| N0-N1 | 53 | 36 (67.9) | 17 (32.1) | ||
| N2-N3 | 40 | 17 (42.5) | 23 (57.5) | ||
| M classification | 7.091 | 0.009 | |||
| M0 | 80 | 50 (62.5) | 30 (37.5) | ||
| M1 | 13 | 3 (76.9) | 10 (23.1) | ||
| Clinical stage | 5.641 | 0.015 | |||
| I–II | 23 | 18 (78.3) | 5 (21.7) | ||
| III–IV | 70 | 35 (50.0) | 35 (50.0) | ||
DNKC, differentiated non-keratinizing carcinoma; UDC, undifferentiated carcinoma; T, tumor size; N, lymph node metastasis; M, distant metastasis; Fox, forkhead box.
Tissue microarray and immunohistochemical (IHC) analysis
NPC and chronically inflamed nasopharyngeal tissue specimens were subjected to a tissue microarray study performed by Pantomics Inc. (Richmond, VA, USA). Briefly, antigens in tissue slices were retrieved by boiling in citrate buffer (0.01 M; pH 6.0) and samples were stained with FoxC1 antibody (1:100; cat. no. ab5079; goat polyclonal; Abcam, Cambridge, MA, USA) for 1 h at room temperature. Incubation with horseradish peroxidase (HRP)-conjugated secondary antibody and visualization with diaminobenzidine (DAB) was performed using a MaxVision™ HRP-Polymer IHC kit and a DAB kit from Maxim (Fuzhou, China) according to the manufacturer's instructions (23). Staining with vimentin antibody (1:50; cat. no. sc-6260; mouse monoclonal; Santa Cruz Biotechnology, Inc, Dallas TX, USA), Fibronectin antibody (1:50; cat. no. sc-18825; mouse monoclonal; Santa Cruz Biotechnology, Inc.), N-cadherin antibody (1:100; cat. no. sc-59987; mouse monoclonal; Santa Cruz Biotechnology, Inc.), E-cadherin antibody (1:50; cat. no. sc-7870; rabbit polyclonal; Santa Cruz Biotechnology, Inc.) and β-catenin antibody (1:100; cat. no. 8478; rabbit polyclonal; Cell Signaling Technology, Danvers, MA, USA) was performed in an identical manner.
Scoring of the IHC staining was performed by two pathologists at Guilin Medical College (Guilin, China). Briefly, each sample was assessed by adding up the scores for the intensity and extent of staining. The intensity of staining was scored as follows: 0, negative; 1, weak; 2, intermediate or 3, strong. The extent of staining was scored based on the percentage of positive tumor cells: 0, <5%; 1, 6–25%; 2, 26–50%; 3, 51–75%; and 4, >76%. For vimentin, fibronectin and N-cadherin, each case was finally classified as negative and positive, while for FoxC1, E-cadherin and β-catenin, tissues were classified as low (final score, 0–3) and high (final score, 4–7) (10).
Cell line and cell culture
The human NPC cell lines 5–8F, 6–10B, CNE1 and CNE2 as well as the NP69 human immortalized nasopharyngeal epithelial cell line were obtained from the American Type Culture Collection (Manassas, VA, USA). The 5–8F cell line has a high metastatic potential, while that of the 6–10B cell line is low. The CNE1 cell line is well-differentiated, while differentiation of CNE2 cells is low. The NPC cell lines were cultured in RPMI-1640 (Gibco-BRL, Invitrogen Life Technologies, Inc., Carlsbad, CA, USA) supplemented with 10% heat-inactivated fetal bovine serum (FBS; Gibco-BRL) and 0.01% penicillin and streptomycin (Gibco-BRL). NP69 cells were cultured in keratinocyte serum-free medium (Gibco-BRL) without any supplementation. All cells were cultured at 37°C in a humidified incubator in an atmosphere containing 5% CO2.
FoxC1 knockdown in CNE2 cells by RNA interference
The human FoxC1 small interfering (si)RNA (cat. no. sc-43766) and control siRNA-A (cat. no. sc-37007) were purchased from Santa Cruz Biotechnology, Inc. At 24 h prior to transfection, CNE2 cells were plated at a density of 5×104 cells/well in a six-well plate. When the cells reached 50% confluency, they were transfected with 200 pmol (80 µM) siRNA using Lipofectamine 2000 (Invitrogen Life Technologies, Inc) according to the manufacturer's instructions. The groups transfected with FoxC1 siRNA and control siRNA were named as siFoxC1 and siNC, respectively. After 6 h of incubation, the cells were washed three times with phosphate-buffered saline (PBS) and the medium was replaced with RPMI-1640 supplemented with 10% FBS. After incubation for 48 h, cells were subjected to western blot analysis and cell motility assays.
Western blot analysis
Western blot analyses were performed using standard methods. In brief, cell pallets were lysed in radioimmunoprecipitation assay (RIPA) buffer (Beyotime Institute of Biotechnology, Haimen, China) with 1 mM phenylmethanesulfonyl fluoride (Solarbio, Beijing, China). The cell lysate was centrifuged at 10,000 × g for 10 min at 4°C and the supernatant was transferred to a fresh micro-centrifuge tube. Protein concentration was determined by the Bicinchoninic Acid Protein Assay Reagent kit (cat. no. 23225; Pierce Biotechnology, Inc., Rockford, IL, USA) and 20 µg protein was loaded per lane. The proteins were separated by 10% SDS-PAGE and electrotransferred onto a 0.45-µm poly-vinylidene difluoride membrane (Merck-Millipore, Billerica, MA, USA). The membrane was blocked with 5% nonfat milk in 20 mM Tris-HCl, 150 mM NaCl and 0.1% Tween-20 (pH 7.5) (TBST; Sigma-Aldrich) for 1.5 h and incubated with the respective primary antibodies overnight at 4°C. The dilution of FoxC1 antibody (cat. no. 8758; rabbit polyclonal; Cell Signaling Technology), vimentin antibody (cat. no. sc-6260; mouse monoclonal; Santa Cruz Biotechnology, Inc.), fibronectin antibody (cat. no. sc-18825; mouse monoclonal; Santa Cruz Biotechnology, Inc.), N-cadherin antibody (cat. no. sc-59987; mouse monoclonal; Santa Cruz Biotechnology, Inc.), E-cadherin antibody (cat. no. sc-7870; rabbit polyclonal; Santa Cruz Biotechnology, Inc.), β-catenin antibody (cat. no. 8478; rabbit polyclonal; Cell Signaling Technology) and β-actin antibody (cat. no. sc-47778; mouse monoclonal; Santa Cruz Biotechnology, Inc.) was 1:1,000. Subsequently, the membranes were washed three times with TBST and incubated with HRP-conjugated secondary antibodies goat anti-rabbit IgG (1:5,000; cat. no. ZDR-5306; ZsBio, Beijing, China) and goat anti-mouse IgG (1:5,000; cat. no. ZDR-5307; ZsBio) at room temperature for 1.5 h. The bands were visualized using an ECL Plus Western Blot kit (cat. no. sc-2048; Western Blotting Luminol Reagent; Santa Cruz Biotechnology, Inc.). The ChemiDoc™ XRS+ system (Bio-Rad Laboratories, Inc, Hercules, CA, USA) and X-OMAT BT film (Carestream Health, Inc, Rochester, NY, USA) were used to capture images of the blots. The intensity of the bands was quantified by densitometry and normalized to that of β-actin (23). The gray values of all bands were measured using Image-pro Plus 6.0 software (Media Cybernetics, Rockville, MD, USA).
In vitro migration and invasion assays
An 8-µm pore size Transwell insert (BD Biosciences, Franklin Lakes, NJ, USA) was used to assess the migratory and invasive ability of cells. At 48 h after transfection, 5×104 CNE2 cells in serum-free RPMI-1640 were seeded into the upper chamber, which was lined with a non-coated membrane, for Transwell migration assays. For invasion assays, Transwell chambers were washed with serum-free medium and 200 mg/ml Matrigel (BD Biosciences) was added to the polycarbonate membrane and dried overnight under sterile conditions. Subsequently, 1×105 cells were seeded in the upper chamber. These inserts were inserted in a 24-well plate with 500 µl RPMI-1640 containing 10% FBS. After incubation for 24 h, the cells on the upper side of the basement membrane were removed with a sterile cotton swab, and the cells that invaded to the lower side of the basement membrane were stained with Giemsa (Sigma-Aldrich). The cells which transgressed through the Transwell polycarbonate membrane were counted under a microscope (BX51; Olympus, Tokyo, Japan). Six random high-power fields were selected for each sample, and the experiment was repeated three times. Results were expressed as mean values of triplicate assays for each experimental condition.
In vitro wound-healing assay
The wound healing assay was performed following a procedure of a previous study (24). CNE2 cells were transfected with siRNA as described above. After incubation for 48 h, the cells were trypsinized (Gibco-BRL) and plated at 5×105 cells/ml into six-well plates. After incubation overnight, line-shaped wounds in the cell monolayer were generated using a pipette tip and images were captured at 0, 24 and 48 h using and Olympus BX51 microscope (24). Experiments were performed in triplicate and repeated three times.
Statistical analysis
Values are expressed as the mean ± standard deviation. Categorical data were analyzed using the χ2 test or Fisher's exact test. Quantitative data were analyzed by using the Unpaired Student's t-test for comparing two groups and one-way analysis of variance for multiple variant analysis. P<0.05 was considered to indicate a statistically significant difference between values and all analyses were performed with using SPSS 19.0 (International Business Machines, Armonk, NY, USA).
Results
FoxC1 is upregulated in NPC tissues and cell lines and high expression of FoxC1 is associated with advanced clinicopathological characteristics
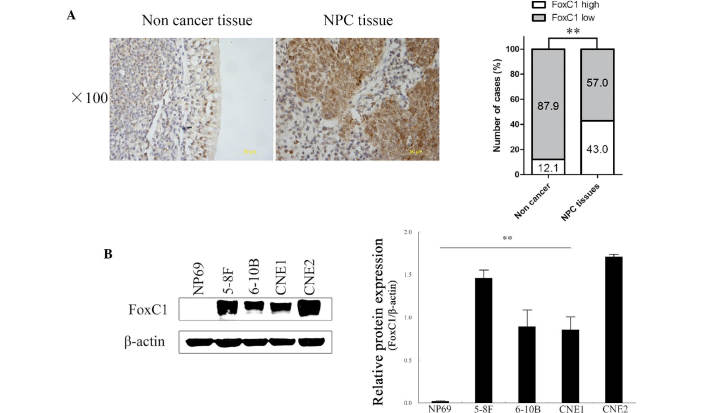
To explore the role of FoxC1 in determining clinical outcomes for NPC patients, the present study investigated the expression of FoxC1 in a tissue microarray comprising 93 NPC and 33 chronically inflamed nasopharyngeal tissue specimens. IHC analysis showed that FoxC1 was localized in the nucleus and cytoplasm. High expression of FoxC1 was observed in 40 out of 93 (43.0%) NPC tissues, but in only 4 out of 33 (12.1%) chronically inflamed nasopharyngeal tissues (P<0.01) (Fig. 1A). Western blot analysis showed that FoxC1 expression was high in NPC cell lines and low in the NP69 immortalized normal human nasopharyngeal epithelial cell line (Fig. 1B). High expression of FoxC1 was significantly correlated with tumor size, lymph node metastasis, distant metastasis and clinical stage (Table I).
Figure 1.
FoxC1 expression in NPC tissues and cell lines. (A) Immunohistochemical analysis of FoxC1 showing upregulation in NPC compared with that in chronically inflamed nasopharyngeal tissues (magnification, ×100; scale bar, 50 µm). (B) Western blot analysis showing elevated FoxC1 protein levels in NPC lines than in the immortalized nasopharyngeal epithelial cell line NP69. Values are expressed as the mean ± standard deviation. **P<0.01. Fox, forkhead box; NPC, nasopharyngeal carcinoma.
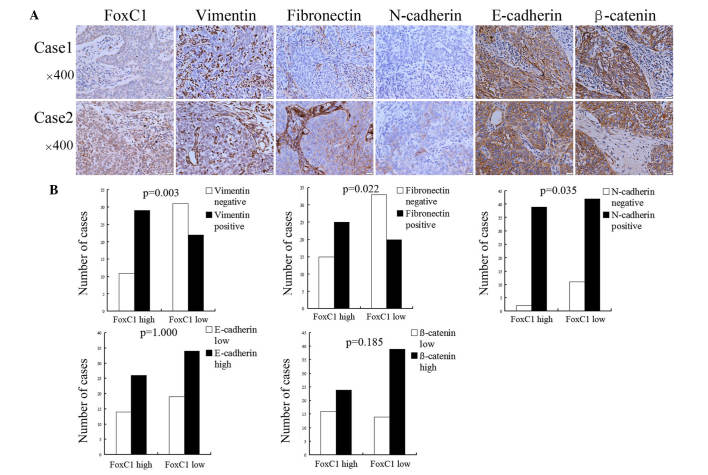
High expression of FoxC1 is positively correlated with vimentin, fibronectin and N-cadherin expression in NPC tissues
Compared to cases with low FoxC1, mesenchymal markers vimentin, fibronectin and N-cadherin were upregulated in NPC tissues with high expression of FoxC1. However, the expression levels of E-cadherin and β-catenin showed no significant difference between the high FoxC1 group and the low FoxC1 group (Fig. 2A). Among the 40 cases with high FoxC1 expression, the positive expression rate of vimentin, fibronectin and N-cadherin was 29/40 (72.5%), 25/40 (62.5%) and 39/40 (97.5%), respectively, and the high expression rate of E-cadherin and β-catenin was 26/40 (65.0%) and 24/40 (60.0%), respectively. In the specimens with low FoxC1 expression, the positive expression rate of vimentin, fibronectin and N-cadherin was 22/53 (41.5%), 20/53 (37.7%) and 42/53 (79.3%), respectively, and the high expression rate of E-cadherin and β-catenin was 34/53 (64.2%) and 39/53 (73.6%), respectively (Fig. 2B).
Figure 2.
High FoxC1 expression is associated with mesenchymal and epithelial markers in nasopharyngeal carcinoma. (A) Immunohistochemical staining of FoxC1 protein and mesenchymal and epithelial markers, including vimentin, fibronectin, N-cadherin, E-cadherin and β-catenin in nasopharyngeal carcinoma. In case 1, FoxC1 expression was low and the cancer cells were negative for vimentin, fibronectin and N-cadherin expression, while being highly positive for E-cadherin and β-catenin expression. In case 2, FoxC1 expression was high and tissue stained positive for vimentin, fibronectin, N-cadherin, E-cadherin and β-catenin. (B) According to statistical analysis, FoxC1 expression was positively correlated with vimentin, fibronectin and N-cadherin expression, but not with E-cadherin and β-catenin expression. Values are expressed as the mean ± standard deviation. Fox, forkhead box.
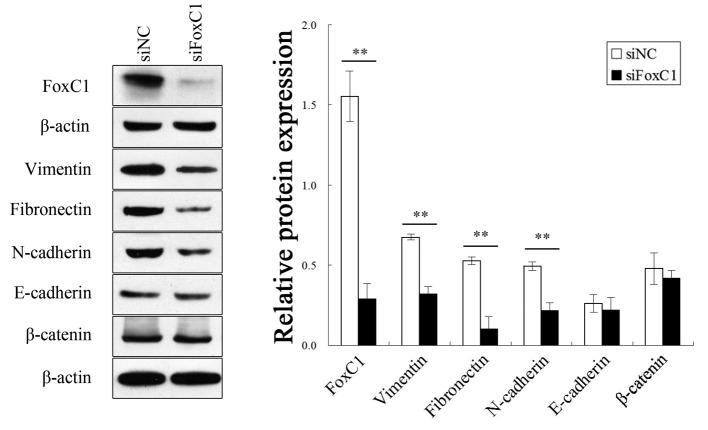
FoxC1 knockdown by siRNA decreases vimentin, fibronectin and N-cadherin expression in CNE2 cells
After FoxC1 knockdown by siRNA, the mesenchymal markers vimentin, fibronectin and N-cadherin were downregulated in CNE2 cells. However, the expression of E-cadherin and β-catenin was not significantly different between the knockdown group and the control group (Fig. 3).
Figure 3.
Mesenchymal and epithelial marker expression after FoxC1 knockdown by siRNA in CNE2 cells. Western blot analysis showed that vimentin, fibronectin and N-cadherin, but not E-cadherin and β-catenin were downregulated in CNE2 cells after FoxC1 knockdown. Values are expressed as the mean ± standard deviation. **P<0.01. Fox, forkhead box; siRNA, small interfering RNA; NC, negative control.
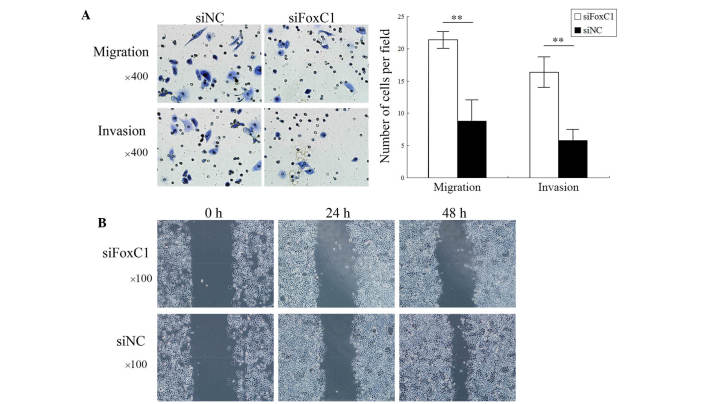
FoxC1 knockdown by siRNA reduces CNE2 cell migration and invasion in vitro
Transwell assays showed that the number of migrated and invaded CNE2 cells was significantly decreased after FoxC1 knockdown by siRNA (Fig. 4A). As shown in Fig. 4B, wound healing of the CNE2 cell layer was inhibited after FoxC1 knockdown by siRNA. These results demonstrated that the migratory and invasive capabilities of NPC cells were deceased following downregulation of FoxC1.
Figure 4.
FoxC1 knockdown by siRNA decreases the migrative and invasive ability of CNE2 cells in vitro. (A) Giemsa staining showed that the number of migrated and invaded cells was markedly decreased following FoxC1 knockdown. (B) Wound healing assay showing that knockdown of FoxC1 by siRNA reduced the distance of migration of CNE2 cells. Values are expressed as the mean ± standard deviation. **P<0.01. Fox, forkhead box; NC, negative control; siRNA, small interfering RNA.
Discussion
The present study revealed that FoxC1 was overexpressed in NPC tissues as compared with that in chronically inflamed nasopharyngeal tissues. These results were consistent with those obtained from cell lines, which showed high FoxC1 expression, while the NP69 immortalized normal nasopharyngeal epithelial cell showed low FoxC1 expression. Furthermore, high FoxC1 expression in NPC tissues was correlated with aggressive phenotypes with large tumor size, lymph node metastasis, distant metastasis and advanced clinical stage. These results implied that FoxC1 is involved in the development and progression in NPC. In addition, knockdown of FoxC1 significantly decreased the migratory, invasive and wound healing capacities of CNE2 cells in vitro. The results from clinical samples and cultured NPC cell lines supported the notion that FoxC1 contributes to aggressive phenotypes in NPC.
The EMT is a key event involved in tumor invasiveness and metastasis and is regulated by several transcription factors during tumor progression, including Twist, Snai1, Slug, Goosecoid, zinc finger E-box binding homeobox 1 and Smad-interacting protein 1 (25). FoxC1 was recently reported to be a transcriptional factor involved in the EMT (10). In the present study, high FoxC1 was correlated with upregulated mesenchymal markers (vimentin, fibronectin and N-cadherin) but not with epithelial markers (E-cadherin and β-catenin) in NPC tissues as well as in cell lines in vitro. Furthermore, the roles of epithelial and mesenchymal markers in the motility of NPC cells were verified by FoxC1 knockdown. Following downregulation of the mesenchymal markers, the migratory and invasive capacities of CNE2 cells were inhibited in vitro.
In the process of EMT, epithelial cells lose their cell-cell adhesion abilities, while cell-extracellular matrix adhesion is enhanced (8). Fibronectin is a high-molecular weight (~440 kDa) glycoprotein, which binds to extracellular matrix components and is thereby involved in cell adhesive and migratory processes (26). Fibronectin expression was reported to be increased in lung cancer, particularly in non-small cell lung carcinoma. The adhesion of lung carcinoma cells to fibronectin enhances their tumorigenicity and confers resistance to apoptosis-inducing chemotherapeutic agents (27,28). N-cadherin is a calcium-dependent cell-cell adhesion glycoprotein, which is abundant in cancer cells and facilitates transendothelial migration (29). Vimentin is responsible for maintaining cell shape, integrity of the cytoplasm and stabilization of cytoskeletal interactions (30). Overexpression of vimentin was observed in spindle-shaped NPC cells, which are thought to be highly invasive (31). The results of the present study showed that FoxC1 expression was positively associated with the expression of fibronectin, N-cadherin and vimentin, which all contributed to the migratory and invasive properties of CNE2 cells.
E-cadherin is a component of an E-cadherin/catenin adhesion complex located to adherens junctions, which are disrupted in cancer. Downregulated E-cadherin in cancer, particularly in advanced cases, leads to the disintegration of adherent junctions, followed by release of β-catenin and its translocation to the nucleus (8). However, the present study showed that in NPC, FoxC1 was not associated with E-cadherin and β-catenin expression. In hepatocellular carcinoma cells, it was previously shown that FoxC1 transactivates the expression of Snai1, a transcriptional inhibitor of E-cadherin, (10,32,33). In human breast cancer, the expression of FoxC1 is also negatively correlated with the expression of E-cadherin and β-catenin (18). The underlying mechanism of how FoxC1 regulates E-cadherin is still required to be elucidated. The results of the present study implied that in NPC, FoxC1 is involved in the EMT by increasing cell-extracellular matrix adhesion rather than disrupting adherens junctions.
In conclusion, the present study showed that FoxC1 was overexpressed and involved in the process of EMT through upregulating fibronectin, vimentin and N-cadherin, which contributed to cell migration and invasion in human NPC. These data suggested that FoxC1 is a potential promoter of the EMT and a prospective therapeutic target in NPC.
Acknowledgments
The present study was supported by the Natural Science Foundation of Guangxi Province (grant no. 2011jjD40031).
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Fang W, Li X, Jiang Q, Liu Z, Yang H, Wang S, Xie S, Liu Q, Liu T, Huang J, et al. Transcriptional patterns, biomarkers and pathways characterizing nasopharyngeal carcinoma of Southern China. J Transl Med. 2008;6(32) doi: 10.1186/1479-5876-6-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chou J, Lin YC. Nasopharyngeal carcinoma-review of the molecular mechanisms of tumorigenesis. Head Neck. 2008;30:946–963. doi: 10.1002/hed.20833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei WI, Sham JS. Nasopharyngeal carcinoma. Lancet. 2005;365:2041–2054. doi: 10.1016/S0140-6736(05)66698-6. [DOI] [PubMed] [Google Scholar]
- 5.Wang R, Wu F, Lu H, Wei B, Feng G, Li G, Liu M, Yan H, Zhu J, Zhang Y, Hu K. Definitive intensity-modulated radiation therapy for nasopharyngeal carcinoma: Long-term outcome of a multicenter prospective study. J Cancer Res Clin Oncol. 2013;139:139–145. doi: 10.1007/s00432-012-1313-0. [DOI] [PubMed] [Google Scholar]
- 6.Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Brabletz T. EMT and MET in metastasis: Where are the cancer stem cells? Cancer Cell. 2012;22:699–701. doi: 10.1016/j.ccr.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 8.Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol. 2014;15:178–196. doi: 10.1038/nrm3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cai LM, Lyu XM, Luo WR, Cui XF, Ye YF, Yuan CC, Peng QX, Wu DH, Liu TF, Wang E, et al. EBV-miR-BART7-3p promotes the EMT and metastasis of nasopharyngeal carcinoma cells by suppressing the tumor suppressor PTEN. Oncogene. 2015;34:2156–2166. doi: 10.1038/onc.2014.341. [DOI] [PubMed] [Google Scholar]
- 10.Xia L, Huang W, Tian D, Zhu H, Qi X, Chen Z, Zhang Y, Hu H, Fan D, Nie Y, Wu K. Overexpression of forkhead box C1 promotes tumor metastasis and indicates poor prognosis in hepatocellular carcinoma. Hepatology. 2013;57:610–624. doi: 10.1002/hep.26029. [DOI] [PubMed] [Google Scholar]
- 11.Paylakhi SH, Moazzeni H, Yazdani S, Rassouli P, Arefian E, Jaberi E, Arash EH, Gilani AS, Fan JB, April C, et al. FOXC1 in human trabecular meshwork cells is involved in regulatory pathway that includes miR-204, MEIS2 and ITGβ1. Exp Eye Res. 2013;111:112–121. doi: 10.1016/j.exer.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 12.Khan AO, Aldahmesh MA, Mohamed JY, Alkuraya FS. Congenital glaucoma with acquired peripheral circumferential iris degeneration. J AAPOS. 2013;17:105–107. doi: 10.1016/j.jaapos.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Ray PS, Wang J, Qu Y, Sim MS, Shamonki J, Bagaria SP, Ye X, Liu B, Elashoff D, Hoon DS, et al. FOXC1 is a potential prognostic biomarker with functional significance in basal-like breast cancer. Cancer Res. 2010;70:3870–3876. doi: 10.1158/0008-5472.CAN-09-4120. [DOI] [PubMed] [Google Scholar]
- 14.Xu ZY, Ding SM, Zhou L, Xie HY, Chen KJ, Zhang W, Xing CY, Guo HJ, Zheng SS. FOXC1 contributes to microvascular invasion in primary hepatocellular carcinoma via regulating epithelial-mesenchymal transition. Int J Biol Sci. 2012;8:1130–1141. doi: 10.7150/ijbs.4769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang L, Gu F, Liu CY, Wang RJ, Li J, Xu JY. High level of FOXC1 expression is associated with poor prognosis in pancreatic ductal adenocarcinoma. Tumour Biol. 2013;34:853–858. doi: 10.1007/s13277-012-0617-7. [DOI] [PubMed] [Google Scholar]
- 16.Nagel S, Meyer C, Kaufmann M, Drexler HG, MacLeod RA. Deregulated FOX genes in Hodgkin lymphoma. Genes Chromosomes. Cancer. 2014;53:917–933. doi: 10.1002/gcc.22204. [DOI] [PubMed] [Google Scholar]
- 17.Wei LX, Zhou RS, Xu HF, Wang JY, Yuan MH. High expression of FOXC1 is associated with poor clinical outcome in non-small cell lung cancer patients. Tumour Biol. 2013;34:941–946. doi: 10.1007/s13277-012-0629-3. [DOI] [PubMed] [Google Scholar]
- 18.Bloushtain-Qimron N, Yao J, Snyder EL, Shipitsin M, Campbell LL, Mani SA, Hu M, Chen H, Ustyansky V, Antosiewicz JE, et al. Cell type-specific DNA methylation patterns in the human breast. Proc Natl Acad Sci USA. 2008;105:14076–14081. doi: 10.1073/pnas.0805206105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taube JH, Herschkowitz JI, Komurov K, Zhou AY, Gupta S, Yang J, Hartwell K, Onder TT, Gupta PB, Evans KW, et al. Core epithelial-to-mesenchymal transition interactome gene expression signature is associated with claudin-low and meta-plastic breast cancer subtypes. Proc Natl Acad Sci USA. 2010;107:15449–15454. doi: 10.1073/pnas.1004900107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sizemore ST, Keri RA. The forkhead box transcription factor FOXC1 promotes breast cancer invasion by inducing matrix metalloprotease 7 (MMP7) expression. J Biol Chem. 2012;287:24631–24640. doi: 10.1074/jbc.M112.375865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu N, Chen NY, Cui RX, Li WF, Li Y, Wei RR, Zhang MY, Sun Y, Huang BJ, Chen M, et al. Prognostic value of a microRNA signature in nasopharyngeal carcinoma: A microRNA expression analysis. Lancet Oncol. 2012;13:633–641. doi: 10.1016/S1470-2045(12)70102-X. [DOI] [PubMed] [Google Scholar]
- 22.Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual. 7th ed. Springer; New York: 2009. [Google Scholar]
- 23.Zhang XL, Huang CX, Zhang J, Inoue A, Zeng SE, Xiao SJ. CtBP1 is involved in epithelial-mesenchymal transition and is a potential therapeutic target for hepatocellular carcinoma. Oncol Rep. 2013;30:809–814. doi: 10.3892/or.2013.2537. [DOI] [PubMed] [Google Scholar]
- 24.Thompson CC, Ashcroft FJ, Patel S, Saraga G, Vimalachandran D, Prime W, Campbell F, Dodson A, Jenkins RE, Lemoine NR, et al. Pancreatic cancer cells overexpress gelsolin family-capping proteins, which contribute to their cell motility. Gut. 2007;56:95–106. doi: 10.1136/gut.2005.083691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119:1420–1428. doi: 10.1172/JCI39104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pankov R, Yamada KM. Fibronectin at a glance. J Cell Sci. 2002;115:3861–3863. doi: 10.1242/jcs.00059. [DOI] [PubMed] [Google Scholar]
- 27.Williams CM, Engler AJ, Slone RD, Galante LL, Schwarzbauer JE. Fibronectin expression modulates mammary epithelial cell proliferation during acinar differentiation. Cancer Res. 2008;68:3185–3192. doi: 10.1158/0008-5472.CAN-07-2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Han S, Khuri FR, Roman J. Fibronectin stimulates non-small cell lung carcinoma cell growth through activation of Akt/mammalian target of rapamycin/S6 kinase and inactivation of LKB1/AMP-activated protein kinase signal pathways. Cancer Res. 2006;66:315–323. doi: 10.1158/0008-5472.CAN-05-2367. [DOI] [PubMed] [Google Scholar]
- 29.Ramis-Conde I, Chaplain MA, Anderson AR, Drasdo D. Multi-scale modelling of cancer cell intravasation: The role of cadherins in metastasis. Phys Biol. 2009;6(016008) doi: 10.1088/1478-3975/6/1/016008. [DOI] [PubMed] [Google Scholar]
- 30.Ogrodnik M, Salmonowicz H, Brown R, Turkowska J, Średniawa W, Pattabiraman S, Amen T, Abraham AC, Eichler N, Lyakhovetsky R, Kaganovich D. Dynamic JUNQ inclusion bodies are asymmetrically inherited in mammalian cell lines through the asymmetric partitioning of vimentin. Proc Natl Acad Sci USA. 2014;111:8049–8054. doi: 10.1073/pnas.1324035111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang W, Li X, Zhang W, Li W, Yi M, Yang J, Zeng Z, Colvin Wanshura LE, McCarthy JB, Fan S, et al. Oxidored-nitro domain containing protein 1 (NOR1) expression suppresses slug/vimentin but not snail in nasopharyngeal carcinoma: Inhibition of EMT in vitro and in vivo in mice. Cancer Lett. 2014;348:109–118. doi: 10.1016/j.canlet.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 32.Cano A, Pérez-Moreno MA, Rodrigo I, Locascio A, Blanco MJ, del Barrio MG, Portillo F, Nieto MA. The transcription factor snail controls epithelial-mesenchymal transitions by repressing E-cadherin expression. Nat Cell Biol. 2000;2:76–83. doi: 10.1038/35000025. [DOI] [PubMed] [Google Scholar]
- 33.Batlle E, Sancho E, Franci C, Domínguez D, Monfar M, Baulida J, García De Herreros A. The transcription factor snail is a repressor of E-cadherin gene expression in epithelial tumour cells. Nat Cell Biol. 2000;2:84–89. doi: 10.1038/35000034. [DOI] [PubMed] [Google Scholar]